Abstract
Background
Supporting adherence to medication is an essential part of the treatment and care of patients with rheumatic and musculoskeletal diseases. The Compliance Questionnaire Rheumatology (CQR) measures adherence in rheumatic diseases through 19 items covering drug-taking behaviour to identify the reasons for adhering to treatment and the factors that contribute to suboptimal adherence. The objective of this study was to present the translation of the CQR into Danish and the face validity and reliability test.
Methods
The CQR was translated into Danish according to international guidelines, followed by a face validity test among 10 patients with rheumatoid arthritis in 2009. The test–retest reliability of the Danish CQR was evaluated in 49 patients with rheumatoid arthritis in 2020 - 2021 using the standard error of the measurement (SEM) converted into the minimally detectable change (MDC) and the intraclass correlation coefficient (ICC). Questionnaires were administered with a minimum of 10 days between assessments.
Results
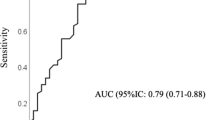
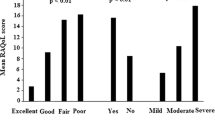
The participants in the reliability test had a mean age of 57.4 years (SD 16.1) and a mean disease duration of 1.13 years (range 2 months–2 years). The mean CQR score in the test and retest was 62.7 (confidence interval (CI) 58.8; 66.6) and 62.5 (CI 58.9; 66.1), respectively, with a SEM of 8.59 (7.16; 10.73) and an MDC of 16.83. A satisfactory test–retest reliability was confirmed by an ICC value of 0.79 (CI 0.68; 0.89).
Conclusion
The Danish CQR has satisfactory test–retest reliability in patients newly diagnosed with rheumatoid arthritis and is considered a reliable tool to measure adherence in this group.
Similar content being viewed by others
Background
Medication adherence in inflammatory arthritis has been reported to vary from 30 to 80%, despite the fact that non-adherence may cause worsening of symptoms and disease severity [1]. According to the European Alliance of Associations for Rheumatology (EULAR), adherence is the behaviour of following a prescription based on shared decision making that allows patient preferences, beliefs and necessities about medication to be considered [1]. As adherence may vary throughout the disease course and may be influenced by several factors, it should also be evaluated continuously throughout the disease course to ensure optimal care and treatment. A trustful relationship and open discussions between patients and healthcare providers is crucial to promote adherence and can be supplemented by, for example, questionnaires to measure adherence [1].
The Compliance Questionnaire Rheumatology (CQR), a validated measure specifically designed to measure drug adherence in patients with rheumatic diseases, showed a sensitivity of 98% and a specificity of 67% to identify non-adherence [2]. It has been evaluated against electronic medication event monitoring in a Dutch study that included 127 patients with rheumatoid arthritis (RA), polymyalgia rheumatica and gout [3]. Through discriminant analyses, this study found a specificity of 95% and a sensitivity of 62% in detecting good taking compliance, and the predictive value was 86% in detecting unsatisfactory taking compliance and 83% in detecting good taking compliance [3].
The CQR was translated into Danish and face-validated among 10 patients with RA in 2009 prior to a study investigating adherence to methotrexate [4]. Therefore, the aim of this article was to present data from the translation, face validity study and reliability test of the Danish CQR.
Methods
CQR
The CQR is a self-administered questionnaire [2] consisting of 19 items covering drug-taking behaviour, that is, adherence to treatment, including the reasons to adhere and the identification of factors that contribute to suboptimal adherence. The answer to each question is given on a four-point Likert scale ranging from ‘don’t agree at all’ (scored 1), ‘don’t agree’ (scored 2) and ‘agree’ (scored 3) to ‘agree very much’ (scored 4), with higher scores indicating higher adherence [3]. The CQR total score is calculated and varies from 0 (complete non-compliance) to 100 (perfect compliance) [3].
Translation and face validity test of the CQR into Danish
The CQR was translated and face-validated into Danish among patients with RA in a study, which was conducted in 2009 [4]. After the Dutch authors of the original publications gave their approval, the instrument was translated into Danish according to the International Quality of Life Assessment method, which involves forward and backward translations by independent translators and a face validity test [5]. The instrument was tested among 10 patients with RA from the Department of Rheumatology at Aarhus University Hospital for relevance and face validity. The testing was conducted using cognitive interviewing principles, which involved the use of the ‘think aloud’ technique and verbal probing during the interview process [6, 7]. During the test, the patients were asked to express their immediate impressions of the questionnaire, and the single items, and they were instructed to go through the questionnaire and provide feedback along the way, specifically, they were asked about the layout, the response format, relevance and phrasing. Questions such as ‘What comes into your mind when you read this?’, ‘What did you notice when answering this question?‘ or ‘Did you find it easy or difficult to answer this question?‘ were asked during the interview. The feedback from this test did not lead to substantial corrections, as none of the interviewees had problems understanding the questionnaire and all the patients found the content of the questionnaire relevant. Figure 1 presents an overview of the translation and face validity test.
Reliability test
For the reliability test, adult patients (> 18 years) newly diagnosed with RA (< 2 years) according to the American College of Rheumatology/European League Against Rheumatism 2010 (ACR/EULAR 2010) criteria [8] and with sufficient skills to read and understand Danish were recruited from a rheumatology outpatient clinic at Aarhus University Hospital, Denmark.
Reliability refers to the degree to which the measurement is free from measurement error, that is, the measurement properties: internal consistency, reliability and measurement error [9]. This study used test–retest to evaluate the extent to which the CQR scores changed over time. Thus, the questionnaire was evaluated with a minimum of 10 days between assessments to reduce the risk of the recollection of answers. The questionnaire was sent to the participants at baseline, followed by a new questionnaire (retest) 10 days later. The questionnaires were administered through Research Electronic Data Capture, REDCap, a secure web application for online surveys and databases hosted at Aarhus University [10, 11]. Both questionnaires were completed at home.
Statistical analysis
Descriptive statistics were calculated for the following variables: age, gender, disease duration, laboratory variables, medical treatment and time between test and retest. Scatters of the differences between the test and retest were plotted against the means to indicate whether the differences were related to the CQR score. The differences between test and retest were calculated, and the systematic differences were assessed using a paired t-test. The differences were plotted against the means of the two measurements using Bland–Altman plots, with 95% confidence intervals (CI) and 95% limits of agreement (LOA). Absolute measurement errors were estimated by calculating the standard error of the measurement (SEM) and converted into minimally detectable change (MDC) (MDC = 1.96 × √2 × SEM). The MDC defines the smallest within-person change that can be interpreted as a ‘real’ change above the measurement error [12]. The intraclass correlation coefficient (ICC) model 2.1, with a corresponding 95% CI, was used to assess reliability. The ICC can range from 0.0 to 1.0, and according to recommendations, an ICC exceeding ≥ 0.70 is considered sufficient reliability for the evaluation of individual patients [13]. As the analysis was based on the complete responses to both questionnaires, no missing items were handled. STATA version 17 [14] was used in the statistical analysis.
Results
Data for the reliability test were collected from October 2020 to March 2021. We invited 71 patients to take part in the study, and of the 56 patients who completed the first test, 49 also completed the questionnaire at retest. Thus, non-responders included 15 patients and 7 patients missed retest. The response rate was 69%. No statistical difference was found between the included patients and the non-responders or patients who missed the retest regarding age, sex, positive rheumatoid factor, positive cyclic citrullinated peptide or methotrexate treatment (p > 0.05). Table 1 shows the participant characteristics, and Fig. 2 provides an overview of the inclusion. The mean duration between test and retest was 12.8 days (SD 3.93), and the mean CQR score was 62.69 (58.76; 66.63) by baseline (test) and 62.51 (58.91; 66.12) by retest. Thus, no statistical difference in the mean CQR score was found between test and retest (p = 0.88 using paired t-test). We found satisfactory test–retest reliability and no systematic bias between measurements, with an ICC value of 0.79 (CI 0.68; 0.89), SEM of 8.59 (7.16; 10.73) and MDC of 16.83 (Table 2). Figure 3 shows a scatter plot of the differences between the test and retest against the mean CQR score.
Discussion
We found that the Danish CQR is a reliable tool for measuring adherence among patients newly diagnosed with RA. To strengthen reliability and in accordance with the Consensus-based Standards for the selection of health Measurement Instruments (COSMIN) guidelines [15], we designed a study with two independent measurements and an appropriate time interval of 10 days to prevent recall of answers. Furthermore, the test conditions were similar for the measurements, as both questionnaires were administered electronically and completed at home, without the influence of healthcare providers [15]. According to the guidelines, reliability measured by ICC should exceed ≥ 0.70 as a minimum [13]. We found an ICC of 0.79, which is considered sufficient and indicates a low degree of systematic error in the measurement. The MDC showed that at least 16.83 points were needed to detect a ‘real’ change in the total CQR score.
The limitations of this study could be related to the population. There is a risk that the patients were not stable in the interim period of the measurements, as we included patients newly diagnosed with RA (< 2 years). Thus, disease activity could be more likely to vary within this group, as some could have achieved remission and others could be in high disease activity. Therefore, this instrument is expected to perform better among prevalent cases due to its more stable context. However, we expected a short interval of 10 days between assessments to reduce the risk of disease fluctuations in individuals. Additionally, it should be taken into consideration that there may be differences in adherence between incident and prevalent subjects. Often, adherence tends to be lower among incident users as discontinuation rates are highest in the initial stages of treatment [16]. For example, van den Bemt et al. highlights that patients are more likely to adhere to treatment when they believe it is effective and the benefits outweigh the risks [17]. Patients with early RA commonly experience side-effects of medications such as Methotrexate, and it takes a considerable amount of time before an effect is observed. This could potentially lead to discontinuation or non-adherence to treatment compared to prevalent patients, who have experienced the beneficial effects of the treatment.
The CQR was developed more than 20 years ago and validated against electronic event monitoring as the ‘gold standard’. This has recently been criticised as a one-dimensional validation that leaves no justification for the use of the weighted sum of items. However, the CQR is a user-friendly instrument, frequently used within rheumatology which enables comparison to other studies. Further, we have earlier shown, that high scores of CQR is associated with a high perception of necessity towards the drug, as indicated by the beliefs about medication questionnaire, among RA patients who are incident users of MTX [4]. To some extent, this finding may support the alignment between the CQR and the theoretical construct of adherence.
Another limitation could be that seven patients missed the retest, which reduced the sample from 56 to 49 patients. Although the response rate of both questionnaires was satisfactory (69%) and loss to follow-up was low, the study could have benefited from an extended sample, as the COSMIN guidelines state that 50–99 patients are considered adequate for test–retest reliability [15].
Conclusion
The Danish CQR has satisfactory test–retest reliability in patients newly diagnosed with RA and is thus considered a reliable tool to measure adherence in this group.
Data Availability
The Danish version of the CQR, and data on the statistical analysis are available upon request from the corresponding author.
Abbreviations
- ACR:
-
American College of Rheumatology
- CQR:
-
Compliance Questionnaire Rheumatology
- COSMIN:
-
Consensus-based Standards for the selection of health Measurement Instruments
- CI:
-
Confidence interval
- EULAR:
-
European Alliance of Associations for Rheumatology
- ICC:
-
Intraclass correlation coefficient
- LOA:
-
Limits of agreement
- MDC:
-
Minimally detectable change
- RA:
-
Rheumatoid arthritis
- SEM:
-
Standard error of the measurement
- SD:
-
Standard deviation
References
Ritschl V, Stamm TA, Aletaha D, Bijlsma JWJ, Böhm P, Dragoi RG et al. 2020 EULAR points to consider for the prevention, screening, assessment and management of non-adherence to treatment in people with rheumatic and Musculoskeletal Diseases for use in clinical practice. Ann Rheum Dis. 2021(80).
de Klerk E, van der Heijde D, van der Tempel H, van der Linden S. Development of a questionnaire to investigate patient compliance with antirheumatic drug therapy. J Rheumatol. 1999;26(12):2635–41.
de Klerk E, van der Heijde D, Landewé R, van der Tempel H, van der Linden S. The compliance-questionnaire-rheumatology compared with electronic medication event monitoring: a validation study. J Rheumatol. 2003;30(11):2469–75.
de Thurah A, Nørgaard M, Harder I, Stengaard-Pedersen K. Compliance with methotrexate treatment in patients with rheumatoid arthritis: influence of patients’ beliefs about the medicine. A prospective cohort study. Rheumatol Int. 2010;30(11):1441–8.
Bullinger M, Alonso J, Apolone G, Leplège A, Sullivan M, Wood-Dauphinee S, et al. Translating health status questionnaires and evaluating their quality: the IQOLA Project approach. International Quality of Life Assessment. J Clin Epidemiol. 1998;51(11):913–23.
Beatty PC, Willis GB. Research Synthesis: the practice of cognitive interviewing. Pub Opin Q. 2007;71(2):287–311.
Collins D. Pretesting survey instruments: an overview of cognitive methods. Qual Life Res. 2003;12(3):229–38.
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO 3, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62(9):2569–81.
Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res. 2010;19(4):539–49.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42.
Prinsen CAC, Mokkink LB, Bouter LM, Alonso J, Patrick DL, de Vet HCW, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27(5):1147–57.
16.1 S, StataCorp. Stata Statistical Software: release 16. College Station. TX: StataCorp LLC; 2019.
Mokkink LB, Prinsen CAC, Patrick DL, Alonso J, Bouter LM, de Vet HCW, Terwee CB. Cosmin Study Design Checklist for Patient-reported outcome measurement instruments. 2019 [Available from: https://link.springer.com/content/pdf/10.1007/s00296-020-04641-1.pdf.
Strom BKSHS, editor. Textbook of Pharmacoepidemiology. 3rd ed. John Wiley & Sons Ltd; 2022. pp. 355–67. Studies of Medication Adherence.
van den Bemt BJ, Zwikker HE, van den Ende CH. Medication adherence in patients with rheumatoid arthritis: a critical appraisal of the existing literature. Expert Rev Clin Immunol. 2012;8(4):337–51.
Acknowledgements
We are grateful to the patients who participated in this study and to Anne Kjær Nielsen, nurse in the Department of Rheumatology, for her assistance in the data collection. We would also like to thank the internal research foundation at Aarhus University Hospital and TrygFonden for supporting this study.
Funding
This study was supported by an internal research foundation at Aarhus University Hospital in Denmark and TrygFonden, Denmark. The foundations had no role in the design of the study and data collection, in the analysis and interpretation of data, in writing the manuscript or in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Both authors contributed to the study’s conception and design. Data collection was performed by a study nurse under the supervision of the authors. The analysis was conducted by ATH. The first draft of the manuscript was written by LRK, in close collaboration with ATH, who critically revised the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This reliability test is part of a major project approved by the Central Denmark Region as data responsible (no. 1-16-02-52-19). This study was performed in accordance with the principles of the Declaration of Helsinki, and according to Danish Law and the Central Denmark Region Committee of Health Research Ethics, this study did not require ethical approval. Permission to use the CQR was obtained before this study. Eligible participants were informed verbally by a study nurse following an e-mail with a link to the questionnaire. Eligible participants were informed about the voluntariness of participation and the possibility of withdrawing at any time without consequences for their care and treatment. Furthermore, their confidentiality and anonymity were ensured. Informed consent was obtained by responding to the questionnaire.
Consent for publication
Not applicable.
Competing interests
The authors, Line Raunsbæk Knudsen and Annette de Thurah, declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Knudsen, L.R., de Thurah, A. Face validity and reliability test of the Danish version of the compliance questionnaire rheumatology in patients with early rheumatoid arthritis. BMC Rheumatol 7, 38 (2023). https://doi.org/10.1186/s41927-023-00364-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41927-023-00364-5