Abstract
Background
To evaluate the efficacy of PET/CT using18F-FDG (18F-fluorodeoxyglucose) as a radiotracer compared to conventional bone marrow biopsy (BMB) in detecting infiltration to bone marrow (BM) in pediatric patients with lymphoma at the time of initial diagnosis.
Methods
66 pediatric patients with lymphoma (47Hodgkin’s and 19non-Hodgkin’s lymphoma) were referred for initial staging by18F-FDG PET/CT study. All patients underwent bilateral iliac BMB and 18F-FDG PET/CT scan with no more than 2 weeks interval in-between. Follow-up for at least 6 months was used as a reference standard to compare diagnostic performance between two modalities in detecting bone marrow infiltration (BMI).
Results
Sensitivity, specificity, accuracy, as well as positive and negative predictive values of 18F-FDG PET/CT in detecting BMI were (80%, 86%, 85%, 63%, and 94%) in contrast to BMB (80%, 53%, 59%, 33%, and 90%) respectively. 18F-FDG PET/CT was concordant to BMB in 39/66 patients (59%).
Conclusion
18F-FDG PET/CT was more accurate and specific, with higher predictive values than BMB in detecting BMI during initial staging of pediatric lymphoma. In most pediatric lymphoma patients, 18F-FDG PET/CT can be used instead of BMB to determine BMI during their initial staging process.
Similar content being viewed by others
Background
Malignant lymphoma is recognized as one of the most prevalent forms of hematological malignancy worldwide (Jhanwar and Straus 2006). Lymphomas can be classified into two main categories: Hodgkin’s lymphoma (HL) and non-Hodgkin’s lymphoma (NHL). BMI is detected in around 15% of recently diagnosed cases of diffuse large B-cell subtype of NHL, with a lower occurrence rate observed in HL(Howell et al. 2002). Proper staging is crucial to optimize therapy and minimize the occurrence of severe adverse effects and toxicity (Connors 2005).
The conventional diagnostic approach for BMI has been to perform a marrow biopsy -from either of the iliac crests (Howell et al. 2002, Brusamolino et al. 2009). Nevertheless, BMB has limitations due to its aggressive nature and its ability to provide information on bone marrow involvement from only one specific location. This limitation is not informative when the BMI is scattered or patchy (Haddy et al. 1989).
Currently, 18F-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) is successfully employed for staging and monitoring of patients with NHL and HL (Almuhaideb et al. 2011; Radford et al. 2015). Multiple investigations have verified that 18F-FDG PET/CT effectively detects BMI and produces similar results to BMB(Pelosi et al. 2008). Therefore, it is assumed to have a complementary function in diagnosing BMI(Hong et al. 2012).
Therefore, the current study aimed to compare the overall diagnostic performance of 18F-FDG PET/CT and its concordance with conventional BMB in detecting BMI in the initial assessment of pediatric patients with lymphoma.
Patient and methods
All pediatric patients under the age of 18 years with pathologically confirmed Hodgkin’s or non-Hodgkin’s lymphoma (prior treatment) who underwent 18F-FDG PET/CT study and BMB for initial staging with no more than 2 weeks interval between both modalities. Patients with more than 2 weeks interval or started chemo or radiotherapy before BMB or 18F-FDG PET/CT study were eliminated.
This study was approved by the Institutional Review Board at the Faculty of Medicine, Assiut University (IRB No., 04-2022-200018) with a clinical trial number (NCT0556898).
Bone marrow biopsy
Preparation
The patient was put prone on the operation table with the posterior superior iliac crest exposed. The skin was then cleansed. The location of the biopsy was determined by palpating the iliac crest. An antiseptic solution was used to sterilize the puncture site. The area was anesthetized with local anesthetic. Then, trephine BMB was taken from the posterior iliac crest bilaterally.
BMB interpretation
After decalcification, the specimen was stained with hematoxyline and eosin and then examined for marrow infiltration by two pathologists unaware of 18F-FDG PET/CT results.
18 F-FDG PET/CT study
Preparation
Fasting for at least 4 h is required before the study. Following an FDG injection of 0.14-0.3mCi/kg (5-11MBq/Kg), the patient was placed in a warm, dark and quiet area.
Serum glucose level below 150 mg/dl was mandatory at time of radiotracer injection.
Technique
PET images were acquired from the skull vertex to the middle of the thigh 60–90 min later. Simultaneous non-contrast CT scan was performed for attenuation correction and fusion with PET images to permit anatomical localization. The images were acquired on a hybrid PET/CT scanner (Biograph m CT flow; Siemens Healthineers) with 16 slice CT component. PET images were employed immediately after CT images acquisitions (5–7 bed positions) with an acquisition time of 1 to 2 min for each bed position, then reconstructed in transverse, sagittal, and coronal views using an iterative algorithm.
Interpretation
The study was examined and interpreted by experienced physicians on the manufacturer’s workstation (Synovia Siemens Healthcare).
Qualitative assessment
Any focal/multifocal lesions or diffuse heterogeneous FDG uptake in BM greater than liver reference uptake was considered abnormal. Revision of CT images for corresponding alterations was done. Diffuse homogenous BM uptake equal to or less than liver uptake was considered reactive hyperplasia and negative for BMI.
Quantitative assessment
A region of interest (ROI) was created over the iliac bone posteriorly to obtain SUV max for BM uptake (BM SUVmax). A second ROI was created over the liver (liver SUVmax) as a benchmark for uptake.
The ratio between BM SUVmax and liver SUVmax was calculated and recorded.
Data analysis and interpretation
The reference standard
To validate the results, follow-up for at least 6 months was used as a gold standard through other radiological, clinical and laboratory data in addition to follow-up 18F-FDG PET/CT to confirm or exclude BMI.
The study was considered Positive for BMI when there is abnormal BM uptake, whether focal or diffuse heterogeneous marrow uptake, greater than the liver uptake. The study was considered Negative for BMI when diffuse homogenous BM uptake is equal to or less than the liver uptake.
True positive results
If both18F-FDG PET/CT and BMB were positive and follow-up of the patient, whether clinical or radiological, was positive for BMI.
True negative results
If both18F-FDG PET/CT and BMB were negative and follow-up was negative for BMI.
False-positive results
Patients with positive or equivocal results in BMB or 18F-FDG PET/CT study yet negative for BMI in follow-up.
False-negative results
Patients with negative results in BMB or 18F-FDG PET/CT study, yet BMI proved in follow-up by further evaluation.
Equivocal Results were considered when there was unexplained diffuse homogenous marrow uptake greater than liver uptake in 18F-FDG PET/CT or inconclusive results in BMB that necessitated further investigation by immunophenotyping.
Equivocal results were considered positive in statistical analysis.
Concordant Results considered if both modalities had similar results, whether positive or negative.
Discordant Results were considered when 18F-FDG PET/CT was positive for BMI while BMB was negative and vice versa.
Statistical analysis
IBM SPSS version 26 (SPSS Inc., Chicago, IL) was used for data analysis. Qualitative variables were represented as frequencies and percentages, while quantitative data was expressed as means ± standard deviations (SD). SUVmax over the iliac bone was used to measure the uptake of BM (SUVBM). A ratio between iliac SUVmax and liver SUVmax was obtained to compare the BM uptake between positive and negative cases of BMI. The diagnostic performance indices for 18F-FDG PET/CT and BMB were generated with 95% confidence intervals for the whole study and separately for HL and NHL.
Agreement between BMB and 18F-FDG PET/CT results was calculated using Cohen’s k computation for the entire study and separately for HL and NHL.
Results
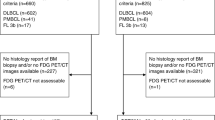
This study was conducted on 66 pediatric patients (54 male and 12 female) with recently diagnosed lymphoma (47 HL and 19 NHL). The mean age was 10 ± 3.8, median 14 (range 4–18 years). B symptoms (fever > 38 C, night sweating, and weight loss) were noted in 22 patients (33.3%); 20 cases of them had HL. Patients’ characteristics with different types of HL and NHL are shown in Table 1.
The pattern of BM uptake
Most patients, 57 out of 66 cases (86.4%), had diffuse homogenous BM uptake, while the remaining 9 patients (13.6%) had focal or heterogeneous FDG uptake, as described in Table 2.
Only 8 out of 57 patients (14%) with diffuse BM uptake were positive for BMI (5 cases with NHL and 3 with HL), while 49 of them (86%) were negative for BMI and proved to have reactive hyperplasia.
6 cases had focal uptake at multiple sites (dorsal, lumber vertebrae, pelvic bones and both femora), and only one case with a heterogeneous pattern proved positive.
The last 2 cases with unifocal BM uptake were considered negative after follow-up.
Evaluation of bone marrow infiltration
BMI was excluded in 51 patients (77.3%) and detected in 15 (22.7%) of cases: 7HL (10.6%), 8 NHL (12.1%).
Out of 15 BMI, 9 cases were detected by both BMB and 18F-FDG PET/CT.
3 cases were detected by 18F-FDGPET/CT only yet with negative BMB (the uptake in BM was focal, and the biopsy was taken from a non-active site).
3 cases were detected by BMB only with negative 18F-FDG PET/CT due to diffuse bone marrow uptake interpreted as reactive hyperplasia. Both modalities detect BMI in 12 out of 66 patients, with a detection rate of about 18%.
Concordance and discordance between 18 F-FDG PET/CT and BMB
18F-FDG PET/CT and BMB were concordant in 39 patients (59%); 9 had positive results in both modalities, and 25 had negative results. While 5 patients had equivocal (false positive) results in both modalities proved to be negative after follow-up.
Discordant Results were noticed in 27 patients (41%); 19 were true negative by 18F-FDG PET/CT with equivocal results in BMB. Another 3 cases with true positive findings in 18F-FDG PET/CT (1 case with focal BM uptake and 2 with diffuse heterogeneous uptake) yet negative BMB results (as biopsy not performed in the active sites) Fig. 1.
3 cases also had false negative results in18F-FDG PET/CT yet positive for BMI by BMB because diffuse BM uptake equal to liver uptake was interpreted as reactive hyperplasia. Taking into consideration that diffuse uptake equal to or greater than liver uptake needs further evaluation by BMB, Fig. 2.
The last 2 cases had equivocal results (FP) in 18F-FDG PET/CT; however, BMI was excluded after BMB, as described in Table 3.
Equivocal results in BMB and18F-FDG PET/CT study in relation to the final diagnosis
9 cases with diffuse homogenous BM uptake greater than liver uptake were considered equivocal by 18F-FDG PET/CT; only 3 were negative for BMI after BMB, and 6 cases still had equivocal results.
30 cases were found to be equivocal by BMB, which necessitated further evaluation by 18F-FDG PET/CT. 20 cases were negative, and 4 were positive after 18F-FDG PET/CT study, while 6 were still equivocal, as shown in Table 4.
Diagnostic performance of 18F-FDG PET/CT and BMB
18F-FDG PET/CT was more accurate (85% vs. 59%), more specific (86% vs. 53%) with higher negative and positive predictive value (94% vs. 90%), (63% vs.33%) than BMB, as illustrated in Table 5.
However, the sensitivity of both modalities was comparable to 80%. The increased sensitivity of BMB was due to bilateral iliac bone biopsy. 18F-FDG PET/CT was more sensitive, specific, and accurate in HL than NHL. The diagnostic performance of BMB is better in NHL than in HL.
Agreement between 18F-FDG PET/CT and BMB
Fair agreement (Kappa 0.33) was noticed between both modalities in patients with HL, while moderate agreement in NHL patients (kappa 0.45), Table 6.
Semi-quantitative Assessment of BMI in positive and negative cases
The difference in the mean value of BM SUVmax between cases with positive BMI and negative cases was significant (1.4 vs.1.07), with a P value of 0.11.
The difference in the mean value of the ratio between BM SUVmax and liver SUVmax was also significant (1.3 vs. 0.86), with a P value of < 0.0001, as shown in Table 7.
Impact on patient staging
15/66 cases were proved to have BMI. Upstaging by18F-FDG PET/CT from stage II and III to stage IV was noticed in 2/66 cases (3%) by detection of BMI. Upstaging from stage III to stage IV by detection of BMI in BMB in another two cases (3%). 11 /66 cases (16.6%) had stage IV by nodal and/or extra-nodal affection, and the stage was confirmed by detection of BMI by both BMB and 18F-FDG PET/CT. In the remaining 51/66 cases, the stage was confirmed by 18F-FDG PET/CT by excluding BMI.
Discussion
Evaluating BMI in lymphoma is crucial for determining the stage of the disease since its presence can advance the disease to stage IV. BMI is more frequent in pediatric NHL than in adults, 12.1% in our study (Chen et al. 2018).
BMB is an aggressive procedure that allows histopathologic analysis of a limited BM specimen obtained from posterior iliac crest. It can be painful and may result in problems like hemorrhage, infection, insufficient sample, and the need for re-biopsy. Blindly performing a unilateral iliac crest biopsy may result in a high rate of false negative bone marrow biopsies. On the other hand, 18F-FDG PET/CT is a noninvasive method that enables viewing of the entire BM in one setting (Elamir et al. 2020). This study aims to assess the role of 18F-FDG PET/CT in evaluating the infiltration to BM compared to BMB in 66 pediatric patients recently diagnosed with lymphoma.
The sensitivity of 18F-FDG PET/CT decreases when BMB is solely utilized as a reference standard (Vishnu et al. 2017). Therefore, we used follow-up findings, computed tomography (CT) changes, and/or magnetic resonance imaging (MRI) findings as a reference standard. This is a great advantage in our study characterizing it from other studies.
Diffuse BM uptake is widely debated in the majority of studies. According to most studies, diffuse uptake in the BM is linked to negative BM biopsies in cases of HL, however positive biopsies were commonly detected in cases of diffuse BM uptake in most cases of diffuse large B-cell lymphoma. This comes in agreement with our results in which the majority of patients with diffuse BM uptake, 49/57 (86%), had negative results with reactive BM hyperplasia; most of them had HL, while only 8/57 cases (14%) were positive for BMI; most of them had NHL, (Adams et al. 2014; El-Galaly et al. 2012).
A small proportion of cases in HL had a scattered pattern with BMI, as discovered by others (Salaun et al. 2009; Chiang et al. 2003).
In our study, 8 out of 15 positive cases of BMI had diffuse BM uptake. This is consistent with Cortés-Romera et al., who found that out of 9 cases with diffuse BM uptake, 4 had positive BMB findings (Cortés-Romera et al. 2014). Further study by Cerci et al. showed that 4 out of 18 NHL cases with diffuse BM uptake were positive in BMB. So, any case with diffuse BM uptake greater than or equal to liver uptake (equivocal findings) should be biopsied to establish etiology and differentiate between BMI and BM hyperplasia (Cerci et al. 2014). Also, Khan et al. reported that 5 patients with uniformly increased BM uptake were positive after biopsy (Khan et al. 2013).
We found that 6 out of 15 cases positive for BMI had focal uptake greater than liver uptake at various sites in dorsal, lumber vertebrae, pelvic bones and both femora and only 1 case with heterogenous diffuse pattern. The research conducted by Öner et al. found that widespread heterogeneous BM accumulations, which showed variations in composition, indicate a positive diagnosis for BMI (Öner et al. 2017).
Conversely, Lee et al. (Lee et al. 2012) discovered that a significant majority (90.9%) of patients with uniformly distributed increased BM activity exhibited positive BMB results in contrast to our study that showed only (14%) of patients with diffuse BM uptake were positive for BMI, while the majority had reactive BM hyperplasia.
18F-FDG PET/CT may not accurately detect minor illness with mild diffuse BM uptake, but BMB will yield positive results. In our study, diffuse BM uptake greater than liver uptake was considered equivocal results in 18F-FDG PET/CT (9 cases), necessitating further BMB to differentiate between BMI and BM reactive hyperplasia. Only 2 out of 9 equivocal cases (22.2%) in 18F-FDG PET/CT had positive BMI.
18F-FDG PET/CT can replace routine BMB when there is frank BMI like in (focal or heterogenous BM uptake), so there is no need for further BMB in these cases. Additionally, 18F-FDG PET/CT can guide the site for biopsy in cases with patchy BM infiltration to avoid false negative results. So, 18F-FDG PET/CT should be performed before BMB to detect the active site for biopsy.
Vishnu et al. examined 99 cases with DLBCL. Among these cases, 38% exhibited BMI. 24% of the total number of cases was found to have positive results for BMI when using 18F-FDG PET/CT, while only 14% had positive results when using BMB. BMB found only two cases (2%) that were not identified by 18F-FDG PET/CT, while 18F-FDG PET/CT detected 12 patients (12%) who were negative, according to BMB (Vishnu et al. 2017). This finding is comparable to our results in which 18F-FDG PET/CT detected 12 positive cases (18%), and 3 cases were negative by BMB as biopsy was not taken from the active site. The agreement between 18F-FDG PET/CT scans and also BMB yielded a concordance rate of 85 (86%) compared to 39/66 patients (59%) in our study and discordance between both modalities in 14 patients (14%) compared to 27/66 patients (41%) in our study.
In a study done by Elamir Y et al., 18F-FDG PET/CT had a better sensitivity of 95.6% in identifying BMI compared to 46.7% in BMB, while both modalities exhibited excellent specificity (98% vs. 100%). 18F-FDG PET/CT scans were more accurate than BMB (97.2% vs. 83.4%) (Elamir et al. 2020).
The findings of our study demonstrated that 18F-FDG PET/CT was more accurate (85% vs. 59%) and more specific (86% vs. 53%) than BMB. However, the sensitivity of both modalities was comparable (80%). The increased sensitivity of BMB was due to the technique used with bilateral iliac bone marrow biopsy instead of conventional unilateral biopsy to decrease the false negative results.
These results contradict the meta-analysis conducted by Pakos et al. (Pakos et al. 2005), which involved 587 patients. The findings from the 18F-FDG PET/CT studies did not demonstrate a strong agreement with those of BMB in diagnosing BMI. The 18F-FDG PET/CT demonstrated a sensitivity of 51% (95% CI, 38–64%) and a specificity of 91% (95% CI, 85–95%). Only the BMB was utilized as the benchmark; hence, 18F-FDG PET/CT was not suggested as a substitute for the regular BMB in this research.
In the current study, 18F-FDG PET/CT tends to be more sensitive, specific, and accurate in HL than in NHL. However, the diagnostic performance of BMB is better in NHL than in HL. These results are consistent with those reported by Kandeel et al., who revealed that 18F-FDG PET/CT demonstrated better diagnostic accuracy than BMB in detecting BMI in patients with HL (Kandeel et al. 2020). .
Our research yielded fair agreement (Kappa 0.33) between both modalities in patients with HL while moderate agreement in NHL patients (kappa 0.45). These results could be due to the low number of cases with NHL in our study. Our findings agree with the research conducted by Cistaro et al., who similarly observed fair agreement between both modalities in pediatric patients with HL (kappa was 0.398) with p-value < 0.001, (Cistaro et al. 2018).
Ann Arbor criteria classify the disease as stage IV based on hematogenous dissemination rather than direct extension, with BMI as a determining factor for this upgrade. Upstaging of 2/66cases (3%)from stage II and III to stage IV with change in management by 18F-FDG PET/CT through detection of BMI and in further 11/66 cases with stage IV by nodal and/or extra-nodal affection, the stage was confirmed by detection of BMI in 18F-FDG PET/CT. These findings were consistent with those of Berthet et al., who investigated the impact of both modalities on determining disease stage and change in management. In 11/133 patients (< 10%), 18F-FDG PET/CT led to upstaging to stage IV and modifications in treatment approach in 4 patients (3.0%) (Berthet et al. 2013). A study conducted by Khan et al. reported comparable findings (Khan et al. 2013).
The utilization of both modalities is complementary in evaluating BMI (Kand et al. 2010). When lesions appear outside the typical regions for iliac BMB, 18F-FDGPET/CT can be used to determine the biopsy location based on metabolically active sites. Several studies indicate that performing regular BMB is essential when 18F-FDG PET/CT scan shows a negative result. This is because 18F-FDG PET/CT scans may not always detect early or limited infiltration of the bone marrow, which can be identified through BMB (Cortés-Romera et al. 2014).In our study we concluded that 18F-FDG PET/CT should be done before BMB and may substitute BMB in positive cases with focal or patchy BM uptake and in negative cases. However, BMB is complementary to 18F-FDG PET/CT in equivocal cases with unexplained diffuse homogenous BM uptake greater than liver uptake to differentiate between BMI and reactive hyperplasia.
Limitations
We incorporated a heterogeneous group of patients with HL and NHL. The current sample size in different subtypes of HL and NHL was insufficient to assess the diagnostic performance of 18F-FDG PET/CT and BMB in detecting BMI in each subtype separately. Therefore, a bigger sample size is required in future research to assess each subtype separately.
Conclusions
18F-FDG PET/CT detects BMI during the initial staging of pediatric lymphoma more accurately than routine BMB. 18F-FDG PET/CT should be performed before BMB to detect the active site for biopsy in cases with focal/patchy BM infiltration to avoid false negative results.
In certain equivocal cases with unexplained diffuse BM uptake, BMB is required as a complementary method to differentiate between BMI and BM reactive hyperplasia.
18F-FDG PET/CT has high concordance to BMB, so there is no need for further BMB to exclude BMI after a negative 18F-FDG PET/CT study.
Data availability
All data used in this study can be made available on request.
Abbreviations
- PL:
-
Pediatric lymphoma
- HL:
-
Hodgkin’s lymphoma
- NHL:
-
Non-Hodgkin’s lymphoma
- BM:
-
Bone marrow
- BMB:
-
Bone marrow biopsy
- BMI:
-
Bone marrow infiltration
- PET/CT:
-
Positron emission tomography/computed tomography
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
References
Adams HJ, Kwee TC, de Keizer B, Fijnheer R, de Klerk JM, Nievelstein RA (2014) FDG PET/CT for the detection of bone marrow involvement in diffuse large B-cell lymphoma: systematic review and meta-analysis. Eur J Nucl Med Mol Imaging 41:565–574
Almuhaideb A, Papathanasiou N, Bomanji J (2011) 18F-FDG PET/CT imaging in oncology. Ann Saudi Med 31(1):3–13
Berthet L, Cochet A, Kanoun S, Berriolo-Riedinger A, Humbert O, Toubeau M et al (2013) In newly diagnosed diffuse large B-cell lymphoma, determination of bone marrow involvement with 18F-FDG PET/CT provides better diagnostic performance and prognostic stratification than does biopsy. J Nucl Med 54(8):1244–1250
Brusamolino E, Bacigalupo A, Barosi G, Biti G, Gobbi PG, Levis A et al (2009) Classical Hodgkin’s lymphoma in adults: guidelines of the Italian Society of Hematology, the Italian Society of Experimental Hematology, and the Italian Group for Bone Marrow transplantation on initial work-up, management, and follow-up. Haematologica 94(4):550
Cerci JJ, Györke T, Fanti S, Paez D, Meneghetti JC, Redondo F et al (2014) Combined PET and biopsy evidence of marrow involvement improves prognostic prediction in diffuse large B-cell lymphoma. J Nucl Med 55(10):1591–1597
Chen S, Wang S, He K, Ma C, Fu H, Wang H (2018) PET/CT predicts bone marrow involvement in paediatric non-hodgkin lymphoma and may preclude the need for bone marrow biopsy in selected patients. Eur Radiol 28:2942–2950
Chiang SB, Rebenstock A, Guan L, Alavi A, Zhuang H (2003) Diffuse bone marrow involvement of Hodgkin lymphoma mimics hematopoietic cytokine-mediated FDG uptake on FDG PET imaging. Clin Nucl Med 28(8):674–676
Cistaro A, Cassalia L, Ferrara C, Quartuccio N, Evangelista L, Bianchi M et al (2018) Italian multicenter study on accuracy of 18F-FDG PET/CT in assessing bone marrow involvement in pediatric Hodgkin lymphoma. Clin Lymphoma Myeloma Leuk 18(6):e267–e73
Connors JM (2005) State-of-the-art therapeutics: Hodgkin’s lymphoma. J Clin Oncol 23(26):6400–6408
Cortés-Romera M, Sabaté-Llobera A, Mercadal-Vilchez S, Climent-Esteller F, Serrano-Maestro A, Gámez-Cenzano C et al (2014) Bone marrow evaluation in initial staging of Lymphoma: 18: F-FDG PET/CT Versus Bone Marrow Biopsy. Clin Nucl Med 39(1):e46–e52
El-Galaly TC, d’Amore F, Mylam KJ, de Nully Brown P, Bøgsted M, Bukh A et al (2012) Routine bone marrow biopsy has little or no therapeutic consequence for positron emission tomography/computed tomography–staged treatment-naive patients with Hodgkin lymphoma. J Clin Oncol 30(36):4508–4514
Elamir Y, Elazab M, Owis AS, Elsayed HF (2020) PET/CT and bone marrow biopsy (BMB) in evaluating bone marrow in lymphoma. Egypt J Radiol Nuclear Med 51(1):1–15
Haddy TB, Parker RI, Magrath IT (1989) Bone marrow involvement in young patients with Non-hodgkin’s lymphoma: the importance of multiple bone marrow samples for accurate staging. Med Pediatr Oncol 17(5–6):418–423
Hong J, Lee Y, Park Y, Kim SG, Hwang KH, Park SH et al (2012) Role of FDG-PET/CT in detecting lymphomatous bone marrow involvement in patients with newly diagnosed diffuse large B-cell lymphoma. Ann Hematol 91:687–695
Howell SJ, Grey M, Chang J, Morgenstern GR, Cowan RA, Deakin DP et al (2002) The value of bone marrow examination in the staging of Hodgkin’s lymphoma: a review of 955 cases seen in a regional cancer centre. Br J Haematol 119(2):408–411
Jhanwar YS, Straus DJ (2006) The role of PET in lymphoma. J Nucl Med 47(8):1326–1334
Kand P, Tiwari B, Basu S, Asopa R, Nayak U (2010) Exploring the role of FDG-PET in the assessment of bone marrow involvement in lymphoma patients as interpreted by qualitative and semi-quantitative disease metabolic activity parameter. Indian J Cancer 47(4):380–384
Kandeel AA, Hussein M, Zidan L, Younis J, Edesa W, Alsayed Y (2020) Diagnostic performance of 18F-2-fluoro-2-deoxy-D-glucose PET/computerized tomography in identifying bone marrow infiltration in new patients with diffuse large B-cell lymphoma and Hodgkin lymphoma. Nucl Med Commun 41(3):269–279
Khan AB, Barrington SF, Mikhaeel NG, Hunt AA, Cameron L, Morris T et al (2013) PET-CT staging of DLBCL accurately identifies and provides new insight into the clinical significance of bone marrow involvement. Blood J Am Soc Hematol 122(1):61–67
Lee Y, Hwang KH, Hong J, Park J, Lee JH, Ahn JY et al (2012) Usefulness of 18 F-FDG PET/CT for the evaluation of bone marrow involvement in patients with high-Grade Non-hodgkin’s lymphoma. Nuclear Med Mol Imaging 46:269–277
Öner AO, Budak ES, Aydın F, Salim O, Yücel OK, Akkaya B et al (2017) Efficacy of 18F-2-fluoro-2-deoxy-D-glucose positron emission tomography/computerized tomography for bone marrow infiltration assessment in the initial staging of lymphoma. Mol Imaging Radionucl Therapy 26(2):69
Pakos EE, Fotopoulos AD, Ioannidis JP (2005) 18F-FDG PET for evaluation of bone marrow infiltration in staging of lymphoma: a meta-analysis. J Nucl Med 46(6):958–963
Pelosi E, Penna D, Deandreis D, Chiappella A, Skanjeti A, Vitolo U et al (2008) FDG-PET in the detection of bone marrow disease in Hodgkin’s disease and aggressive non-hodgkin’s lymphoma and its impact on clinical management. QJ Nucl Med Mol Imaging 52(1):9
Radford J, Illidge T, Counsell N, Hancock B, Pettengell R, Johnson P et al (2015) Results of a trial of PET-directed therapy for early-stage Hodgkin’s lymphoma. N Engl J Med 372(17):1598–1607
Salaun PY, Gastinne T, Bodet-Milin C, Campion L, Cambefort P, Moreau A et al (2009) Analysis of 18 F-FDG PET diffuse bone marrow uptake and splenic uptake in staging of Hodgkin’s lymphoma: a reflection of disease infiltration or just inflammation? Eur J Nucl Med Mol Imaging 36:1813–1821
Vishnu P, Wingerson A, Lee M, Mandelson MT, Aboulafia DM (2017) Utility of bone marrow biopsy and aspirate for staging of diffuse large B cell lymphoma in the era of positron emission tomography with 2-deoxy-2-[fluorine-18] fluoro-deoxyglucose integrated with computed tomography. Clin Lymphoma Myeloma Leuk 17(10):631–636
Acknowledgements
Not applicable.
Funding
No funds were received for this study.
Author information
Authors and Affiliations
Contributions
NB contributed to the study concept and design, data acquisition, data analysis, interpretation of study results, and substantial manuscript revision. SS and MK were involved in the study concept and design, data acquisition. TZ contributed to the substantial revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study was approved by the local Medical Ethics Committee (IRB No. 04-2022-200018) in the Faculty of Medicine, Assiut University. All procedures followed the 1964 Helsinki Declaration’s ethical guidelines and recent modifications.
Consent for publication
Written informed consent was obtained from the child’s parents in this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bashank, N., Sharef, S., Mohran, T.Z. et al. 18F-FDG PET/CT versus bone marrow biopsy in detecting bone marrow infiltration in initial staging of pediatric lymphoma. EJNMMI Rep. 8, 8 (2024). https://doi.org/10.1186/s41824-024-00200-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41824-024-00200-0