Abstract
Background
Lung cancer is the leading cause of cancer-related deaths worldwide. The combination of fluorine-18 fluorodeoxyglucose positron emission tomography (18F-FDG PET) and computed tomography (CT) has a major impact on the diagnosis, staging, treatment planning and follow-up of lung cancer patients. The maximum standardized uptake value (SUVmax) is an easily performed and most widely used semi-quantitative index for the analysis of FDG PET images and estimation of metabolic activity. This study aimed to investigate the role of PET/CT in differentiating adenocarcinoma (ADC), the most common lung cancer, from squamous cell carcinoma (SCC) by comparing FDG uptake measured as SUVmax.
Results
Between 2019 and 2022, 76 patients diagnosed with non-small cell lung cancer (NSCLC) at the Department of Pathology, Atatürk University Faculty of Medicine, with histopathologic evidence of adenocarcinoma or squamous cell carcinoma, underwent retrospective analysis using PET/CT scanning to measure PET parameters of the lesions and compare them with histopathology. Among 76 NSCLC patients included in the study, 43 (57%) were histopathologically diagnosed as ADC and 33 (43%) as SCC. SUVmax, SUVmean, metabolic tumor volume (MTV) and total lesion glycolysis (TLG) values of lesions in patients with SCC were statistically significantly higher than those in patients with ADC (p values 0.007, 0.009, 0.003 and 0.04, respectively).
Conclusions
Lung SCC has higher metabolic uptake values than ADC, and PET/CT can be used to differentiate them.
Similar content being viewed by others
Introduction
Lung cancer is the most common cancer worldwide and is responsible for most cancer-related deaths. According to the World Health Organization (WHO), lung cancer is the leading cause of cancer deaths globally (Mattiuzzi and Lippi 2019). Lung cancers are divided into two main groups: small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC). NSCLC is the most common type and accounts for approximately 80–85% of all lung cancer cases. The main histologic types of NSCLC are adenocarcinoma (ADC) and squamous cell carcinoma (SCC) (Goldstraw et al. 2007). The location within the lung is one of the differences between SCC and ADC. SCC tends to be central and may have internal cavitation, while ADC tends to be peripheral and solid (Gharraf et al. 2020). Lung adenocarcinoma is the most common type of lung cancer, accounting for about 40% of all lung cancers. It tends to arise in the periphery of the lungs as it originates from small airway epithelial cells that secrete mucus and other substances (Zappa and Mousa 2016). SCC is the second most common type of lung cancer after lung adenocarcinoma and originates from the bronchial surface epithelium. Tumor cells are characterized by a squamous appearance similar to that observed in epidermal cells. Lung SCC is more strongly linked to tobacco smoking than other forms of NSCLC. It usually arises in the center of the larger bronchi and often metastasizes to the locoregional lymph nodes early in its course, but spreads outside the thorax later than other major types of lung cancer (Sabbula et al. 2023). Early and accurate diagnosis of lung cancer is invaluable for successful treatment and good outcomes. The 5-year survival rate of small, localized stage 1 NSCLCs with surgical resection is approximately 70–90%. However, the majority of patients, 3 out of 4, are diagnosed at an advanced stage and have a poor prognosis (Goldstraw et al. 2007; Walters et al. 2013).
Positron emission tomography/computed tomography (PET/CT) with fluorodeoxyglucose (FDG) labeled with fluorine-18 (F-18), a glucose analog, is now routinely used in clinical practice for both the evaluation of lung nodules and the staging of lung cancer. Due to its high diagnostic accuracy in lung cancer, FDG PET/CT imaging is now included as a routine diagnostic modality in many clinical lung cancer guidelines (Ettinger et al. 2019; Kitajima et al. 2016). FDG PET/CT has become an important tool in the diagnosis and staging of NSCLC. The maximum standard uptake value (SUVmax) in FDG PET/CT is the ratio of activity in tissue per unit volume relative to the dose carried by body weight. SUVmax of primary tumors has been found to correlate with stage, nodal status, histological type, differentiation and tumor progression in patients with NSCLC. Furthermore, high SUVmax value has been shown to have serious effects on prognostic factor in patients with NSCLC (Shimizu et al. 2014). However, the application of treatments other than surgery in patients with FDG PET/CT positive lesions requires histopathologic confirmation (Ettinger et al. 2019). There is a 20% risk of pneumothorax during transthoracic biopsy. With FDG PET/CT imaging, it may be possible to overcome this risk in many patients with lung nodules. In addition, in the case of a malignant lesion, a possible pneumothorax may delay other procedures for diagnostic evaluation, which increases the importance of non-invasive FDG PET/CT imaging (Madsen et al. 2016).
In this study, we aimed to investigate whether semi-quantitative parameters of FDG PET/CT correlated with the main histological types of NSCLC, ADC and SCC, in retrospectively screened NSCLC patients. In particular, we tried to analyze whether SUVmax, SUVmean, metabolic tumor volume (MTV) and total lesion glycolysis (TLG) values of FDG PET/CT differed in patients diagnosed with lung SCC and ADC.
Materials and methods
Study design
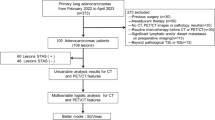
Seventy-six NSCLC cases diagnosed as adenocarcinoma and squamous cell carcinoma with pneumonectomy, lobectomy, segmentectomy and wedge resection materials in the pathology department of the university hospital, between 2019 and 2022, were included in this study. Information on age, gender, tumor histological type, tumor diameter, lymph node involvement, visceral pleural invasion status and pathological stage were obtained from the hospital automation system and the Ministry of Health e-Nabız system. H&E stained preparations of the resection materials were re-examined by two observers, and histopathologic typing was performed according to WHO 2021 criteria.
PET/CT
Patients enrolled in the study were fasted for at least 6 h. Blood glucose levels were confirmed to be less than or equal to 140 mg/dl before 18F FDG infusion. 5.5 MBq/kg 18F FDG was administered intravenously 1 h before imaging. One hour after the injection, imaging was performed from the upper thigh to the head with the patient in the supine position for 3 min per bed by Biograph 6 PET/CT (Siemens Medical Systems, Germany). Whole-body PET/CT images were evaluated by an experienced nuclear medicine specialist. Clinical staging of the patients was performed according to the TNM system of the 8th version of the American Joint Committee on Cancer/Union for International Cancer Control (AJCC/UICC). Pathologic lesion areas were drawn by the nuclear medicine specialist, and Suvmax, Suvmean, MTV and TLG values were automatically measured and recorded by Siemens VIA program for FDG uptake.
Statistical analysis
Number, percentage, mean and standard deviation were used in the evaluation of the data. Independent samples t test was used in the evaluation of normally distributed data. Mann–Whitney U and Kruskall–Wallis tests were used for data that did not show homogeneous distribution. p values of 0.05 and below were accepted as significant.
Results
A total of 76 patients, 15 (19.7%) females and 61 (80.3%) males, were included in our study. The mean age of the patients was 59 ± 9.91 years (min 26, max 78). The clinical characteristics of the patients are listed in Table 1. Excluding the incidence of ADC and SCC in women, which may be explained by their regional non-smoking habits (Cornfield et al. 2009), the parameters in Table 1 show an almost homogeneous distribution between ADC and SCC. The slides of all cases were re-evaluated by two pathologists and 43 were confirmed as ADC and 33 as SCC. In addition, tumor size, pleural invasion and tumor spread within the air spaces (STAS), which affect lung cancer stage and prognosis, were evaluated. Pleural invasion was present in 22% of our cases (17 cases), while 78% (59 cases) were negative. 41 patients had STAS, while 35 patients did not. Tumor size is an important factor in the staging of lung cancers (Rami-Porta et al. 2015). Tumor size should be given in the most accurate way because it can change the stage of the tumor. In 41 cases, the tumor size was 1–3 cm and was considered as stage 1. Twenty-seven cases were stage 2, i.e., tumor size was 3–4 cm or 1–3 cm with pleural invasion. Six cases were stage 3, and two cases were stage 4. In 14 cases, lymph node metastasis was observed, but not in 37 cases. In 25 cases there were no clear data about lymph node metastasis. Lymphovascular invasion was detected in 43 cases.
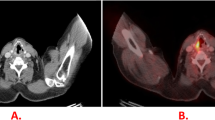
The values of PET parameters (SUVmax, SUVmean, MTV and TLG) are compared between ADC and SCC in Table 2. Statistical analysis was performed to assess whether there were significant differences in these variables. For the SUVmax, the mean value in ADC was 8.19 ± 6.57, whereas it was 13.18 ± 9.04 in SCC. The t test revealed a statistically significant difference between the two groups (t = − 2.78, p = 0.007), indicating that SUVmax values were significantly higher in SCC compared to ADC. Similarly, for the SUVmean, the mean value in ADC was 4.88 ± 3.74, and in SCC, it was 7.60 ± 5.06. The t test demonstrated a statistically significant difference (t = − 2.69, p = 0.009), suggesting that SUVmean values were significantly higher in SCC compared to ADC. For MTV, the mean value in ADC was 10.79 ± 21.11, and in SCC, it was 12.25 ± 14.64. The nonparametric Mann–Whitney U test indicated a statistically significant difference (MW-U = 430.00, p = 0.003), implying that MTV values were significantly higher in SCC compared to ADC. Lastly, for the TLG, the mean value in ADC was 77.81 ± 211.01, while in SCC, it was 150.47 ± 299.12. The Mann–Whitney U test revealed a statistically significant difference (MW-U = 522.00, p = 0.04), indicating that TLG values were significantly higher in SCC compared to ADC. In conclusion, the statistical analysis demonstrates significant differences in the parameters SUVmax, SUVmean, MTV, and TLG between the two groups. Representative pictures of ADC and SCC in Fig. 1 also show FDG uptake in SCC is higher than that in ADC. The results apparently suggest that there are statistically significant differences between the two groups being compared for each parameter, as indicated by the small p values (p < 0.05). SCC exhibits higher values for PET parameters compared to ADC.
Discussion
In this study, we analyzed the variances in semi-quantitative SUVmax, SUVmean, MTV and TLG values of FDG PET/CT between lung carcinomas diagnosed with ADC and SCC. We found significant differences between ADC and SCC. According to our study, SUVmax, SUVmean, MTV and TLG values were significantly higher in SCC patients compared to ADC patients (p values 0.007, 0.009, 0.003 and 0.04, respectively).
Early and accurate diagnosis of lung cancer subtypes is of vital importance. Although PET/CT technology, which can perform non-invasive tumor assessment for classification, staging, efficacy and prognostic evaluation, has been shown to be useful in determining the subtype of cancers in recent studies, the parameters for its use in this field have not yet matured (Sun et al. 2023). In this study, similar to recent studies (Salem et al. 2021), we found that quantitative PET/CT values were higher in SCC (Table 2).
The advantage of FDG PET/CT is that it combines the functional-metabolic information of PET with the detailed anatomical-morphologic information of CT in a single hybrid study. PET/CT has also been used to assess metabolic activity in lung cancers. Semi-quantitative PET parameters such as MTV and TLG values have previously shown promising results in providing prognostic insight for disease progression of respiratory system tumors (Jin et al. 2018).
The mRNA and protein expression of metabolic markers has been shown to be higher in squamous cell carcinomas than in adenocarcinomas, whereas adenocarcinomas are better vascularized (Goodwin et al. 2017). Adenocarcinomas have a worse disease-free survival (DFS) compared to squamous cell carcinomas based on the potential for metastasis. Adenocarcinomas have been shown to exhibit glycolysis under normoxic conditions, whereas squamous cell carcinomas are subjected to diffusion-limited hypoxia (Schuurbiers et al. 2014). Although squamous cell carcinomas have a higher FDG uptake, which is generally considered a poor prognostic factor, adenocarcinomas have a higher metastatic potential and a worse DFS (Schuurbiers et al. 2014). These findings suggest that FDG PET should be interpreted in relation to histology. FDG PET may improve the prognostic potential of the disease and its use in histology-related treatment strategies could be expanded.
Studies on this subject are limited. Similar to the results of previous studies, Schurbiers et al. and Hyun et al. showed that SCC had a higher SUV value compared to ADC as a general trend although there was no statistically significant difference in the SUV value of static PET between ADC and SCC in their study (Schuurbiers et al. 2014; Hyun et al. 2019). This may provide a theoretical basis and technical support for early, accurate and personalized treatment. The cellular reason for this may be that SCC has a higher rate of glycolysis and less vascularization compared to the high perfusion and low rate of glucose phosphorylation in ADC (Sun et al. 2023; Vriens et al. 2012). Patnaik et al.'s meta-analysis showed that higher values of SUVmax, MTV and TLG predicted a higher risk of recurrence or death in patients with surgical NSCLC. They recommended the use of FDG PET/CT to select patients at high risk of disease recurrence or death who may benefit from aggressive therapies (Patnaik et al. 2016).
The number of patients in the study is limited for a comprehensive conclusion; nevertheless, it provides important clues for a clear distinction between ADC and SCC. Moreover, our study was performed on operated patients, so the number of stage 4 patients is small, and a more comprehensive study can be performed with a similar number of patients at each stage.
Conclusions
In conclusion, 18F-FDG PET/CT imaging has a marked potential for the classification of NSCLC and differential diagnosis of subtypes and thus may help clinicians to improve the histopathologic diagnosis of lung cancer in a noninvasive manner.
Availability of data and materials
Data supporting our findings are available from the corresponding author upon reasonable request.
Abbreviations
- FDG PET:
-
Fluorine-18 fluorodeoxyglucose positron emission tomography
- SUVmax:
-
Maximum standardized uptake value
- SUVmean:
-
Mean standardized uptake value
- ADC:
-
Adenocarcinoma
- SCC:
-
Squamous cell carcinoma
- NSCLC:
-
Non-small cell lung cancer
- MTV:
-
Metabolic tumor volume
- TLG:
-
Total lesion glycolysis
References
Cornfield J, Haenszel W, Hammond EC, Lilienfeld AM, Shimkin MB, Wynder EL (2009) Smoking and lung cancer: recent evidence and a discussion of some questions*. Int J Epidemiol 38(5):1175–1191
Ettinger DS, Wood DE, Aggarwal C, Aisner DL, Akerley W, Bauman JR et al (2019) NCCN guidelines insights: non-small cell lung cancer, version 1.2020. J Natl Compr Canc Netw 17(12):1464–1472
Gharraf HS, Mehana SM, ElNagar MA (2020) Role of CT in differentiation between subtypes of lung cancer; is it possible? Egypt J Bronchol 14(1)
Goldstraw P, Crowley J, Chansky K, Giroux DJ, Groome PA, Rami-Porta R et al (2007) The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol 2(8):706–714
Goodwin J, Neugent ML, Lee SY, Choe JH, Choi H, Jenkins DMR et al (2017) The distinct metabolic phenotype of lung squamous cell carcinoma defines selective vulnerability to glycolytic inhibition. Nat Commun 8:15503
Hyun SH, Ahn MS, Koh YW, Lee SJ (2019) A machine-learning approach using PET-based radiomics to predict the histological subtypes of lung cancer. Clin Nucl Med 44(12):956–960
Jin F, Qu B, Fu Z, Zhang Y, Han A, Kong L, Yu J (2018) Prognostic value of metabolic parameters of metastatic lymph nodes on 18F-FDG PET/CT in patients with limited-stage small-cell lung cancer with lymph node involvement. Clin Lung Cancer 19(1):e101–e108
Kitajima K, Doi H, Kanda T, Yamane T, Tsujikawa T, Kaida H et al (2016) Present and future roles of FDG-PET/CT imaging in the management of lung cancer. Jpn J Radiol 34(6):387–399
Madsen PH, Holdgaard PC, Christensen JB, Hoilund-Carlsen PF (2016) Clinical utility of F-18 FDG PET-CT in the initial evaluation of lung cancer. Eur J Nucl Med Mol Imaging 43(11):2084–2097
Mattiuzzi C, Lippi G (2019) Current cancer epidemiology. J Epidemiol Glob Health 9(4):217–222
Patnaik S, Liu J, Dong M, Sun X, Li W, Xing L, Yu J (2016) Prognostic value of 18F-FDG PET/CT in surgical non-small cell lung cancer: a meta-analysis. PLoS ONE 11(1):e0146195
Rami-Porta R, Bolejack V, Crowley J, Ball D, Kim J, Lyons G et al (2015) The IASLC lung cancer staging project: proposals for the revisions of the T descriptors in the forthcoming eighth edition of the TNM classification for lung cancer. J Thorac Oncol 10(7):990–1003
Sabbula BR, Gasalberti DP, Anjum F (2023) Squamous cell lung cancer. StatPearls, Treasure Island
Salem AMA, Hussein LH, Osman AM (2021) Role of FDG-PET CT in differentiating adenocarcinomas from squamous cell carcinomas of the lung. QJM Int J Med 114(Supplement_1)
Schuurbiers OCJ, Meijer TWH, Kaanders JHAM, Looijen-Salamon MG, de Geus-Oei L-F, van der Drift MA et al (2014) Glucose metabolism in NSCLC is histology-specific and diverges the prognostic potential of 18FDG-PET for adenocarcinoma and squamous cell carcinoma. J Thorac Oncol 9(10):1485–1493
Shimizu K, Maeda A, Yukawa T, Nojima Y, Saisho S, Okita R, Nakata M (2014) Difference in prognostic values of maximal standardized uptake value on fluorodeoxyglucose-positron emission tomography and cyclooxygenase-2 expression between lung adenocarcinoma and squamous cell carcinoma. World J Surg Oncol 12:343
Sun Y, Xiao L, Wang Y, Liu C, Cao L, Zhai W et al (2023) Diagnostic value of dynamic (18)F-FDG PET/CT imaging in non-small cell lung cancer and FDG hypermetabolic lymph nodes. Quant Imaging Med Surg 13(4):2556–2567
Vriens D, Disselhorst JA, Oyen WJ, de Geus-Oei LF, Visser EP (2012) Quantitative assessment of heterogeneity in tumor metabolism using FDG-PET. Int J Radiat Oncol Biol Phys 82(5):e725–e731
Walters S, Maringe C, Coleman MP, Peake MD, Butler J, Young N et al (2013) Lung cancer survival and stage at diagnosis in Australia, Canada, Denmark, Norway, Sweden and the UK: a population-based study, 2004–2007. Thorax 68(6):551–564
Zappa C, Mousa SA (2016) Non-small cell lung cancer: current treatment and future advances. Transl Lung Cancer Res 5(3):288–300
Acknowledgements
Not applicable.
Funding
Atatürk University Hospital funded the salary for the authors affiliated in Faculty of Medicine.
Author information
Authors and Affiliations
Contributions
All authors were involved in the study conception and design. AM, İK, RD, OC and SÖ were involved in acquisition of data. AM, SÇ and SÖ were involved in analysis and interpretation of the data and drafting of the manuscript and were responsible for review, editing and supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our study was approved by the ethics committee of Atatürk University Faculty of Medicine for retrospective analysis and did not require informed consent. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent for publication
Written informed consent was obtained from all the patients.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maman, A., Çiğdem, S., Kaya, İ. et al. Diagnostic value of FDG PET-CT in differentiating lung adenocarcinoma from squamous cell carcinoma. EJNMMI Rep. 8, 1 (2024). https://doi.org/10.1186/s41824-024-00187-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41824-024-00187-8