Abstract
Purpose
To quantify incidental thyroid pathology including malignancy on routine 18F-FDG PET-CT scans
To compare standardised uptake values (SUVmax) in thyroid malignancy subtypes
Methods and materials
This is a retrospective study of all 18F-FDG PET-CT scans (n = 6179) performed in a teaching hospital between June 2010 and May 2019. RIS database search of reports for the word “thyroid” was performed. Studies with evidence of thyroid uptake were included. Patient age and gender, primary indication for PET scan (malignant or non-malignant), thyroid result on PET (diffuse or focal tracer uptake, SUVmax), ultrasound and FNAC results were recorded.
Results
Incidental abnormal thyroid tracer uptake as a proportion of all 18F-FDG PET-CT scans was 4.37% (n = 270). Out of region patients (n = 87) whose records could not be obtained were excluded leaving a study group of n = 183. Ninety-four in this group had focal uptake, and 89 had diffuse uptake. Fifty-five patients in the focal group had undergone further investigations. Of these, 30 were thought to be benign on USS alone, and 25 patients underwent USS/FNAC. Thirteen (24%) malignancies were identified (5 papillary, 6 follicular, 1 poorly differentiated thyroid cancer, 1 metastatic malignancy). Mean SUVmax for papillary carcinoma was noted to be 8.2 g/ml, and follicular carcinoma was 12.6 g/ml.
Conclusion
Incidental abnormal thyroid 18F-FDG PET-CT uptake in PET-CT scans of 4.37% is in keeping with the known limited literature. Rather similar number of patients was noted in the focal and diffuse tracer uptake categories in the final study group. Around quarter of the focal lesions were identified to be malignant, implying focal lesions should always be further investigated.
Similar content being viewed by others
Introduction
The increasing role of PET-CT in oncological and non-oncological conditions has resulted in an increased detection of PET-CT incidentalomas, commonly involving the thyroid gland (The Royal College of radiologists, 2012; Delivanis & Castro, 2018; Vassiliadi & Tsagarakis, 2011).
The tracer 18F-FDGFootnote 1 used in PET-CT can incidentally accumulate in the thyroid gland, either diffusely or focally. Incidental focal 18F-FDG uptake within the thyroid gland has previously been found to occur in 1.2–4.3% of all PET-CT scans in patients scanned for an alternative indication (Kao et al., 2012; Soelberg et al., 2012; Cohen et al., 2001; Kang et al., 2003; Chen et al., 2005; Chen et al., 2009; Ho et al., 2011). Patients with focal uptake within the thyroid gland are at a higher risk of malignancy, with studies reporting between 26 and 50% (Kao et al., 2012; Soelberg et al., 2012; Cohen et al., 2001; Chen et al., 2005; Chen et al., 2009; Kim et al., 2005; Chu et al., 2006; Bae et al., 2009). Figures 1 and 2 are two patients in our institution scanned for an alternative indication who subsequently were found to have thyroid malignancy. Further investigation of focal 18F-FDG uptake with ultrasound and FNACFootnote 2 is recommended because of this increased risk of malignancy (Pencharz et al., 2018; Haugen et al., 2015; Hoang et al., 2015).
Fifty-three-year-old female with a diagnosis of Hodgkin’s lymphoma underwent PET-CT scan to monitor her response to chemotherapy. PET coronal (a) and axial (b) images show focus of increased tracer uptake in the left lobe of the thyroid. Image c shows fused axial PET-CT image showing the same abnormality (SUV max 11.1g/ml). FNAC biopsy showed this to be papillary thyroid carcinoma
Seventy-nine-year-old female with a past medical history of systemic sclerosis and Raynaud’s disease. She presented with symptoms of weight loss, retrosternal chest discomfort and general cognitive decline. Prior investigations had shown a raised CRP and normal WCC in her routine blood, and an OGD showed oesophagitis only. She had a CT CAP and PET-CT to investigate for possibility of an organ tumour/large vessel vasculitis. Image a shows axial CT with a large left-sided thyroid mass. Image b is a fused axial PET-CT scan showing 33 mm × 36 mm metabolically active lesion (SUV max 10.3 g/ml) which occupies much of the left lobe of the thyroid gland and is responsible for tracheal deviation to the right. FNAC confirmed follicular carcinoma
PET-CT can deduce semi-quantitative evaluations of glucose metabolism in tissues by measuring standardised uptake value (SUVmax) (Chu et al., 2014). The role of SUVmax in thyroid malignancy is debated as studies have produced conflicting results, and, although reasonable to suggest that malignancy is associated with a higher SUVmax value (Kumar et al., 2013), some studies have shown no correlation (Eloy et al., 2009; Are et al., 2007).
Although the usefulness of SUVmax in thyroid malignancy is questioned, a cytological diagnosis of focal thyroid FDG-PET incidentalomas is necessary considering the increased risk of malignancy.
The primary aim of our study was to quantify incidental thyroid malignancy on 18F-FDG PET-CT in patients scanned for an alternative indication. A secondary outcome was to compare mean, median, and range of SUVmax according to thyroid malignancy subtypes.
Methods and materials
This is a retrospective study of all 18F-FDG PET-CT scans performed in a large teaching hospital between June 2010 and May 2019. We performed a CRIS (CDN Radiology Information System) database search, and results were filtered to include the word “thyroid” within the scan reports. All 18F-FDG PET-CT scans in our institution are double reported by four experienced consultants, two of whom are also experienced in routine thyroid imaging. Studies with no thyroid uptake were excluded. We manually collected patient’s data including age and gender, primary indication for PET-CT scan (malignant or non-malignant), thyroid result on PET (diffuse or focal uptake of 18F-FDG), ultrasound result and result of FNAC. Total number of FNAC diagnosed as thyroid malignancy and mean SUVmax values of thyroid malignancy subtypes were collected. Those patients who had tracer uptake but were lost to follow-up were excluded.
Results
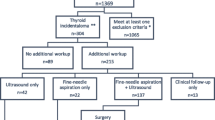
Six thousand, one-hundred and seventy-nine (n = 6179) 18F-FDG PET scans were performed during study period. Three-hundred and forty-two (n = 342) results contained the word “thyroid” of which two-hundred and seventy (n = 270) scans had increased uptake in thyroid gland. Eighty-seven (n = 87) patients were excluded (out of region patients, deaths, lost to follow-up). This left a study group of one-hundred and eighty-three (n = 183) of which one hundred and twenty-seven (n = 127) were females, and fifty-six (n = 56) were males. Ninety-four (n = 94) PET-CT scans had focal uptake, and eighty-nine (n = 89) had diffuse uptake. In our study group, those with diffuse uptake included seventy female patients (n = 70) and nineteen (n = 19) male patients. Fifty-seven females (n = 57) and thirty-seven male patients (n = 37) had focal uptake in our study group. Fifty patients in the focal group underwent further investigations. Of these, 30 were thought to be benign on USS alone and 25 patients underwent USS/FNAC, where 52% (52%, n = 13/25) were confirmed to be malignancy. Thyroid malignancy subtypes included papillary (n = 5), follicular (n = 6), metastatic malignancy (n = 1) and poorly differentiated carcinoma of the thyroid (n = 1). Patients who had a previous history of thyroid cancer with increased uptake were included in the study (n = 1). Eight (8/25) pathology result confirmed benign lesions including non-neoplastic (n = 2), follicular with Hurthle cell type changes (n = 1), and colloid nodule (n = 5). The remainder of the FNA biopsies were deemed indeterminate (n = 4/25) by the reporting pathologist giving a malignancy positive rate of 62% (13/21) within the confirmed results. Overall, 13 malignancies were identified out of the 55 patients with focal uptake who underwent further assessment (24%).
Abnormal tracer uptake in the thyroid gland incidentally as a proportion of all 18F-FDG PET-CT scans was 4.37%. Abnormal focal tracer uptake as a proportion of all 18F-FDG PET-CT scans was 2.77%. Mean SUVmax in focal malignant lesions ranged from 4 to 35.36 g/ml (Table 1) and in focal benign lesions ranged from 1.6 to 18.2 g/ml (Table 2). Mean SUVmax value for papillary carcinoma was 8.2 g/ml, and follicular carcinoma was 12.6 g/ml. Median SUVmax for papillary carcinoma was 7.4 g/ml, and follicular carcinoma was 8.2 g/ml. Given the small sample size and significant overlap in the obtained SUVmax data for the two groups, a threshold with a clinically valuable power cannot be obtained to differentiate benign and malignant tracer uptake and hence is not stated here.
Discussion
Incidental abnormal thyroid 18F-FDG uptake as a proportion of all PET-CT scans and incidence of malignancy in focal abnormal thyroid 18F-FDG uptake in our patient group are both comparable with the available limited literature (Vassiliadi & Tsagarakis, 2011; Kao et al., 2012; Soelberg et al., 2012; Cohen et al., 2001; Kang et al., 2003; Chen et al., 2005; Chen et al., 2009; Yi et al., 2005; Ho et al., 2011; Kim et al., 2005; Chu et al., 2006), reiterating the importance of detecting and investigating focal thyroid uptake on 18F-FDG PET-CT. Around a quarter of focal thyroid uptake were malignant; hence, focal lesions should be investigated further, if clinically appropriate. A significant proportion of 18F-FDG PET-CT scans are performed for known/unknown malignancy, and further assessment of incidental thyroid lesions may not be possible for many reasons. Regardless, it is important to detect thyroid lesions in all patients in order to optimise appropriate clinical decision-making.
Some of the patients who underwent USS were deemed benign sonographically despite having focal thyroid tracer uptake. It is recommended that all thyroid tracer focal uptake, if clinically appropriate, are investigated further with an ultrasound and FNAC because of the increased risk of malignancy (Bae et al., 2009; Pencharz et al., 2018; Haugen et al., 2015). Currently, we do not have agreed local guidelines for investigation of focal thyroid uptake on 18F-FDG PET-CT, but based on current recommendations and findings in this study, it would be our future practice to investigate all focal lesions to undergo FNAC where clinically necessary.
Similar number of diffuse and focal thyroid tracer uptake were found in our study, and this is important to differentiate them as they have different outcomes for patients. Abnormal thyroid tracer uptake, diffuse or focal, also appears to be more in females, and this is comparable with current literature (Stangierski et al., 2014).
Our secondary aim was to compare SUVmax across thyroid malignancy histological subtypes. Follicular carcinoma has a higher mean, median and range of SUVmax than papillary carcinoma in this study. Soelberg et al. in their meta-analysis found mean SUVmax to be 6.9 g/ml in malignant lesions (Soelberg et al., 2012), lower than our findings for both follicular and papillary carcinoma but comparable with our median SUVmax. Our sample size for each malignancy subtype is low, and mean SUVmax and median SUVmax might be affected by this, so should be interpreted cautiously.
Our study found malignancies with a wide range of SUVmax values, implying a higher mean SUVmax does not necessitate malignancy. It is debatable if SUVmax can differentiate between benign and malignant lesions, but overall it is thought that mean SUVmax is lower in benign lesions compared to malignant lesions (Soelberg et al., 2012). It is also unclear if a specific SUVmax indicates malignancy and certain cutoffs have been stipulated. In our study, we were unable to confidently identify a cutoff point for SUVmax to identify malignancy due to considerable overlap in SUVmax values in both benign and malignant focal uptake lesions. This is echoed by the results of two smaller studies, which also showed a large overlap in SUVmax value between benign and malignant lesions (Brindle et al., 2014; Agrawal et al., 2015). With the findings in this study and other studies, it is difficult to confidently use mean SUVmax value alone in differentiating between benign and malignant thyroid lesions. There is a role for SUVmax in thyroid malignancy, but a specific defined value or range cannot be accurately established in differentiating between benign or malignant lesions.
There are a few limitations to our study that we acknowledge. Our biggest limitation was that we excluded nearly a third of patients with focal thyroid tracer uptake who were lost to our follow-up. Most of those patients were referred to us initially from regional centres, and their follow-up records or results were not available for our reference. Despite this, the study still showed the prevalence of incidental thyroid uptake on 18F-FDG PET-CT. Another limitation of our study is that only a word search for “thyroid” was done in our reports, and images were not reviewed. As described earlier, all our scans are double reported within a pool of 4 experienced consultants, two of whom specialise in thyroid imaging. Most of these patients undergo scans for known malignancy, and a significant proportion of these scans are reviewed again for MDT requirements. Furthermore, there is a dedicated discrepancy meeting to identify reporting errors. We strongly believe, given the above, that the possibility of missing unreported thyroid lesions in these scans to be very low.
Conclusion
Standardised approach needed for investigation of incidental 18F-FDG PET-CT focal uptake in the thyroid gland due to high prevalence of malignancy and a combination of ultrasound with FNAC is advised.
There is conflicting evidence at how to utilise SUVmax in focal thyroid tracer uptake, but its use in combination with ultrasound and histopathological findings should be sought with further bigger studies. We established that SUVmax is relatively higher in follicular carcinoma than papillary carcinoma; however, further research in large patient groups is needed.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request
Notes
18F-fluorodeoxyglucose
Fine needle aspiration with cytology
References
Agrawal K, Weaver J, Ul-Hassan F, Jeannon JP, Simo R, Carroll P, et al. Incidence and significance of incidental focal thyroid uptake on (18)F-FDG PET study in a large patient cohort: retrospective single-Centre experience in the United Kingdom. Eur Thyroid J 2015; 4:115-122. doi: https://doi.org/https://doi.org/10.1159/000431319
Are C, Hsu JF, Schoder H, Shah JP, Larson SM et al (2007) FDG-PET detected thyroid incidentalomas: need for further investigation? Ann Surg Oncol 14:239–247
Bae JS, Chae BJ, Park WC, Kim JS, Kim SH et al (2009) Incidental thyroid lesions detected by FDG-PET/CT: prevalence and risk of thyroid cancer. World J Surg Oncol 7:63
Brindle R, Mullan D, Yap BK, Gandhi A et al (2014) Thyroid incidentalomas discovered on positron emission tomography CT scanning - malignancy rate and significance of standardised uptake values. Eur J Surg Oncol 40(11):1528–1532. https://doi.org/10.1016/j.ejso.2014.05.005 Epub 2014 May 24
Chen W, Parsons M, Torigian DA, Zhuang H, Alavi A (2009) Evaluation of thyroid FDG uptake incidentally identified on FDG-PET/CT imaging. Nuclear Med Commun 30(3):240–244
Chen YK, Ding HJ, Chen KT, Chen YL, Liao AC et al (2005) Prevalence and risk of cancer of focal thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography for cancer screening in healthy subjects. Anticancer Res 25:1421–1426
Chu QD, Connor MS, Lilien DL, Johnson LW, Turnage RH et al (2006) Positron emission tomography (PET) positive thyroid incidentaloma: the risk of malignancy observed in a tertiary referral center. Am Surg 72(3):272–275
Chu Y, Zheng A, Wang F, Lin W, Yang X, Han L et al (2014) Diagnostic value of 18F-FDG-PET or PET-CT in recurrent cervical cancer: a systematic review and meta-analysis. Nuclear Med Commun 35:144–150
Cohen MS, Arslan N, Dehdashti F, Doherty GM, Lairmore TC et al (2001) Risk of malignancy in thyroid incidentalomas identified by fluorodeoxyglucose-positron emission tomography. Surgery 130:941–946
Delivanis DA, Castro MR (2018) Thyroid nodules. Humana press; Cham, Switzerland: 2017. Thyroid Incidentalomas; pp. 153–167.
Eloy JA, Brett EM, Fatterpekar GM, Kostakoglu L, Som PM, Desai SC, Genden EM (2009) The significance and management of incidental [18F]fluorodeoxyglucose–positron-emission tomography uptake in the thyroid gland in patients with cancer. Am J Neuroradiol 30(7):1431–1434. https://doi.org/10.3174/ajnr.A1559
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE et al (2016) 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26:1–133. https://doi.org/. https://doi.org/10.1089/thy.2015.0020
Ho TY, Liou MJ, Lin KJ, Yen TC (2011) Prevalence and significance of thyroid uptake detected by 18F-FDG PET. Endocrine. 40(2):297–302
Hoang JK, Langer JE, Middleton WD, Wu CC, Hammers LW, Cronan JJ, et al. Managing incidental thyroid nodules detected on imaging: white paper of the ACR incidental thyroid findings committee. J Am Coll Radiol 2015; 12: 143–150. doi: https://doi. org/https://doi.org/10.1016/j.jacr.2014.09.038
Kang KW, Kim SK, Kang HS, Lee ES, Sim JS et al (2003) Prevalence and risk of cancer of focal thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography for metastasis evaluation and cancer screening in healthy subjects. J Clin Endocrinol Metabol 88:4100–4104
Kao YH, Lim SS, Ong SC, Padhy AK (2012) Thyroid incidentalomas on fluorine-18-fluorodeoxyglucose positron emission tomography-computed tomography: incidence, malignancy risk, and comparison of standardized uptake values. Cancer Assoc Radiol J 63:289–293
Kim TY, Kim WB, Ryu JS, Gong G, Hong SJ et al (2005) 18F-fluorodeoxyglucose uptake in thyroid from positron emission tomogram (PET) for evaluation in cancer patients: high prevalence of malignancy in thyroid PET incidentaloma. Laryngoscope 115:1074–1078
Kumar V, Nath K, Berman CG, Kim J, Tanvetyanon T et al (2013) Variance of SUVs for FDG-PET/CT is greater in clinical practice than under ideal study settings. Clin Nucl Med 38(3):175–182
Pencharz D, Nathan M, Wagner TL (2018) Evidence-based management of incidental focal uptake of fluorodeoxyglucose on PET-CT. Br J Radiol 91:20170774
Soelberg KK, Bonnema SJ, Brix TH, Hegedüs L (2012) Risk of malignancy in thyroid incidentalomas detected by 18F-fluorodeoxyglucose positron emission tomography: a systematic review. Thyroid 22:918–925. https://doi.org/10.1089/thy.2012.0005
Stangierski A, Woliński K, Czepczyński R, Czarnywojtek A, Lodyga M, Wyszomirska A, et al. The usefulness of standardized uptake value in differentiation between benign and malignant thyroid lesions detected incidentally in 18F-FDG PET/CT examination. PLoS One 2014; 9: e109612. doi: https://doi.org/https://doi.org/10.1371/journal.pone.0109612
The Royal College of radiologists (2012) iRefer: making the best use of clinical radiology, 7th edn. The royal college of Radiologists, London
Vassiliadi D.A., Tsagarakis S. Endocrine incidentalomas—challenges imposed by incidentally discovered lesions. National review of endocrinology, 2011; June 28th; 7:668–680. Doi: https://doi.org/10.1038/nrendo.2011.92
Yi JG, Marom EM, Munden RF, Truong MT, Macapinlac HA et al (2005) Focal uptake of fluorodeoxyglucose by the thyroid in patients undergoing initial disease staging with combined PET/CT for non–small cell lung cancer. Radiology 236:271–275
Acknowledgements
We thank NHS Tayside and PET-CT technical staff for their dedicated and enthusiastic work.
Declarations of interest
None
Research involving human participants and/or animals
This study did not involve human or animal participants.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
I confirm that each author has participated sufficiently in any submission to take public responsibility for its content, with specific roles outlined below: Dr Shea Roddy—data collection, analysis and manuscript preparation. Mr Thomas Biggans, Dr Thiru Sudarshan, Dr Avinash Kanodia—manuscript proof-reading. Dr Ahmad Raofi—data collection and manuscript proof-reading. Dr Prasad Guntur Ramkumar—data analysis, manuscript preparation and proof-reading. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interest
All authors (Dr Shea Roddy, Mr Thomas Biggans, Dr Ahmad Raofi, Dr Avinash Kanodia, Dr Thiru Sudarshan and Dr Prasad Guntur Ramkumar) have no potential conflicts of interest to declare.
Consent for publication
This was a retrospective study that did not use patient identifiers and informed consent was not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Roddy, S., Biggans, T., Raofi, A.K. et al. Prevalence of incidental thyroid malignancy on routine 18F-fluorodeoxyglucose PET-CT in a large teaching hospital. European J Hybrid Imaging 4, 21 (2020). https://doi.org/10.1186/s41824-020-00089-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41824-020-00089-5