Abstract
Background
Patient reported outcomes (PROs) are being used frequently in clinical practice. PROs often serve several purposes, such as increasing patient involvement, assessing health status, and monitoring and improving the quality-of-care at an aggregated level. However, the lack of representative PRO-data may have implications for all these purposes. This study aims to assess the association of non-administration of (not sending an electronic invite to PRO) and non-response to (not responding to PRO) electronically administered PROs with social inequality in a primary healthcare cancer rehabilitation setting. Furthermore, it examines whether the workflows surrounding PRO have an impact on non-administration and non-response.
Methods
This is a cross sectional study using routinely collected data from electronic health records and registers including cancer survivors (CSs) over 18 years booked for an initial consultation in a primary healthcare cancer rehabilitation setting using PROs for systematic health status assessment. During the study period two different PRO platforms were used, each associated with different workflows. Non-administration and non-response rates were calculated for sociodemographic characteristics for each PRO platform. Crude and adjusted odds ratios were calculated using univariate and multivariate logistic regression.
Results
In total, 1868 (platform 1) and 1446 (platform 2) CSCSs were booked for an initial consultation. Of these, 233 (12.5%) (platform 1) and 283 (19.6%) (platform 2) were not sent a PRO (non-administration). Among those who received a PRO, 157 (9.6%) on platform 1 and 140 (12.0%) on platform 2 did not respond (non-response). Non-administration of and non-response to PROs were significantly associated with lower socioeconomic status. Moreover, the workflows surrounding PROs seem to have an impact on non-inclusion in and non-response to PROs.
Conclusions
Non-administration of and non-response to PROs in clinical practice is associated with determinants of social inequality. Clinical workflows and the PRO platforms used may potentially worsen this inequality. It is important to consider these implications when using PROs at both the individual and aggregated levels. A key aspect of implementing PROs in clinical practice is the ongoing focus on representativeness, including a focus on monitoring PRO administration and response.
Similar content being viewed by others
Background
Patient reported outcome (PRO) questionnaires are increasingly used in routine clinical practice for long term conditions, including cancer [1,2,3,4]. On the individual level, PROs have the potential to increase patient-centred care by providing the patient’s perspective and facilitating dialogue in consultations by identifying and focusing on the patient’s current health status [5,6,7,8,9,10,11]. On the aggregated level, PRO-data may be used for quality monitoring and improvement in clinical practice as well as research purposes [12, 13]. In the field of oncology, most studies on the use of PROs have been performed in hospital settings in relation to patients undergoing active treatment, whereas knowledge about routine use in other settings is scarce [2].
One challenge of using PRO questionnaires in clinical practice is the potential to exacerbate existing health inequalities. The integration of PROs into routine clinical care may face challenges arising from a variety of factors concerning both patients and healthcare professionals [9, 14, 15]. The organization of PRO data collection, including aspects such as incorporation into existing clinical workflows or the design of the PRO collection system, can impact patient participation in PRO assessments [3, 16]. Studies have shown that non-response is higher in men, persons with higher ages, ethnic minorities, individuals with lower socioeconomic status, and persons living alone [17,18,19,20,21]. The same pattern is seen for the use of electronically administered PROs [20]. Lower socioeconomic status has been associated with lower health literacy, or eHealth literacy [22, 23], and the use of PROs or electronic PROs may exclude populations not able to fill out or finish questionnaires due to low health literacy. Also, cognitive impairments or language barriers may hinder participation in PROs [24, 25]. A lack of representative PRO data not only excludes some populations from the individual benefits of using PROs but also introduces bias in the data used to evaluate clinical care and thus a risk of making decisions about health service innovations that only benefit certain populations. It is therefore important that healthcare organisations have awareness of the availability and accessibility of services to accommodate patients with different strengths and limitations, i.e., organisational health literacy responsiveness [26, 27]. Most studies report on response rates for PRO, whereas studies focusing on administration or distribution rates are few [28].
The objective of this study was to assess whether non-administration of (i.e., not sending an invite to PRO) and non-response to (i.e., not responding to PRO) electronically administered PROs were associated with social inequality in health among cancer survivors referred to rehabilitation in primary healthcare cancer rehabilitation. Additionally, the study aimed to determine whether the workflows surrounding PRO and the PRO platform impacted non-administration and non-response.
Methods
Study design
The study is cross sectional using routinely collected data from electronic health records.
Study setting
In Denmark, cancer rehabilitation is provided by municipalities in primary healthcare settings at a community level [29]. In the municipality of Copenhagen, which covers approximately 650,000 inhabitants, cancer rehabilitation is handled by the Copenhagen Centre for Cancer and Health. Rehabilitation is focussed on reaching or maintaining optimal quality of life by interventions aimed at physical, social, psychological, and cognitive function. Approximately 1200 cancer survivors (CSs) are referred yearly to the centre from hospitals (approximately 95%) or general practitioners. At the time of referral, around 58% of CSs have been diagnosed with cancer within the last 1–3 months, 24% within 4–11 months, and 18% more than a year ago. This means that many CSs are undergoing active treatment while participating in rehabilitation. Therefore, an important task for the healthcare professionals in the centre (nurses, physiotherapists, dieticians, or occupational therapists) is the assessment of the changing health status. In 2019, the centre implemented the use of electronically administered PRO in connection with the initial consultation as a tool to support systematic assessment of health status and thereby an indication of the rehabilitation needs the CS might have, to support the dialogue between the healthcare professional and CS, and for quality improvement purposes. In the present setting, it is standard practice for healthcare professionals to actively incorporate PRO into the dialogue. This emphasis on PRO utilisation has been a major focus of the management within the centre. Healthcare professionals are trained how to use the PRO platform by an internal process consultant who also facilitates exchange of experiences among the healthcare professionals about the active use of PRO during the consultation. Considering that most CSs are recently diagnosed, many may undergo emotional distress or find themselves in the initial phases of treatment, frequently encountering accompanying side effects. PRO thus serves as a snapshot of the health status of CSs who are navigating through a highly changeable period in their lives, and the relevance of their responses may vary at the time of the consultation. Therefore, a flexible approach to the active use of PRO is utilised, where, depending on the circumstances, responses may be addressed over shorter or longer periods during the consultation. The PRO used comprises 62 questions. It is a combination of validated scales and items designed specifically for health status assessment at the initial consultation. The core of the questionnaire is the 27-item Functional Assessment of Cancer Therapy-General (FACT-G) questionnaire, which measures health-related quality of life status and covers physical, social, emotional, and functional well-being [30]. These items cannot be skipped when filling out PRO. Other items cover lifestyle factors (smoking, alcohol, diet, exercise), self-rated health and cancer distress (distress thermometer), family situation, occupational situation, disease, as well as priorities and concerns. These items can be skipped when filling out PRO. On average, it takes between 10 and 20 min to answer PRO.
Workflows surrounding PRO and PRO platforms
Two different web-based PRO questionnaire platforms were used during the study period. Platform 1, a commercially available online survey platform, was used from April 2019 to February 2021. Platform 2, an online platform developed specifically for PRO use in the rehabilitation centre, was used from March 2021-August 2022. None of the platforms were integrated with the electronic health record. The workflow for PRO can be divided into four overarching steps. For both staff and patients, there are differences in several of these steps between the two platforms (Fig. 1).
Step 1: For both platforms, referred CSs were contacted by phone by a healthcare professional, and an initial consultation was booked. The CS was informed about PRO, emphasising its importance as preparation for the consultation, and that answers would be used during the consultation to help focus on the individual’s health status and accompanying needs for rehabilitation (Step 1, Fig. 1). If, during the phone call, it became evident that the CS was exempted from the secure national online digital mailbox or had difficulties accessing digital PRO, the healthcare professional suggested the possibility of answering PRO on a tablet in the centre just prior to the initial consultation.
Step 2: For platform 1, the healthcare professional informed the administration about the booked consultation, and administrative staff assigned PRO to the CS. For platform 2, the healthcare professional assigned PRO to the CS (Step 2, Fig. 1). Approximately one week prior to the booked consultation, a link to PRO was electronically sent via the secure national online digital mailbox used for communication between individuals and the public sector. The electronic mailbox is linked to a person’s civil registration number and is accessible using a digital ID authenticator app, code display or chip. For platform 1, administrative staff checked PRO response status daily for consultations the following day and sent reminders via the platform to those who had not answered. For platform 2, automatic reminders were sent if there was no answer one day prior to the consultation.
Step 3: For platform 1, a personalised link was generated. The CS logged in to their secure digital mailbox with their digital ID to access the link and was guided directly to the PRO. For Platform 2, data security was increased, and a general link was used, so the CS had to log in to the secure digital mailbox with their digital ID, access the link, and use their digital ID again to access the PRO (Step 3, Fig. 1). CSs completed the PRO at home using a smartphone, tablet, or computer. During completion, some questions were optional, but the questions from FACT-G were mandatory. CSs exempted from the national secure digital mailbox or those who found it too difficult to access had the possibility of completing the PRO on a tablet in the centre immediately prior to the consultation. In the region, the proportion of inhabitants exempted from the national digital mailbox has decreased from 6.4% in 2019 to 4.9% in 2022 [31].
Step 4: Answers to PRO were discussed with the CS at the consultation (Fig. 1, Step 4). For platform 1, administrative staff downloaded PRO answers for upcoming initial consultations, copied them into an excel sheet with colour-coding, and uploaded the excel sheet to the electronic health record so the healthcare professional could prepare for the consultation. Platform 2 was developed specifically for PRO use in the rehabilitation centre, aiming to facilitate healthcare communication around PRO in Step 4, Fig. 1. This was achieved by providing healthcare professionals with an easy overview of PRO responses for upcoming consultations, automatically generated colour-coded PRO reports, and the ability to observe changes in PRO answers over time. For both platforms, the colour coding serves as a visual tool to quickly convey the health status of the CSs based on their responses. Responses indicating severe symptoms or distress are highlighted in red, while those indicating mild or no symptoms are green.
Participants
We identified CSs over 18 years referred to cancer rehabilitation and booked for an initial consultation at the Copenhagen Centre for Cancer and Health from 1 April 2019 to 31 August 2022. If a CS had been referred and booked for a consultation more than once in the study period, the first referral was used in this study. Identified CSs were divided into two groups according to the PRO platform used at the time of referral. For each PRO platform, two populations were formed: those booked for an initial consultation (population 1a and 2a) and those who had been sent a PRO (population 1b and 2b) (Fig. 2).
Data collection
The outcomes under study were non-administration for populations 1a and 2a and non-response for populations 1b and 2b. Non-administration was defined when the CS was booked for an initial consultation, but was not sent a link to PRO. Non-response was defined when the CS had been sent a link to PRO but had not answered PRO. A response was considered valid if the CS had answered the 27 mandatory items of FACT-G. Age, sex, and educational level were selected as covariables as they have previously been shown to have an impact on the response rate [17,18,19,20]. Also, educational level is a highly contributing and robust marker for social inequality in cancer, as disease may affect other markers such as occupational status and income [32].
Data on age at referral, sex, diagnosis, administration of the PRO, and response to the PRO were retrieved from the electronic health record and the platforms used for administering the PRO. Additional sociodemographic data on individuals included in the study were obtained from registers at Statistics Denmark. The highest attained level of education was categorised according to the International Standard Classification of Education (ISCED) as low (ISCED 0–2), medium (ISCED 3–4), and high (ISCED 5–8) [33, 34]. The disposable family income level was divided in tertiles, high (~42,850–102,900€), medium (~26,800–42,800€), low (~9,000–26,750€), for each population in the study [35]. In 2020, the median disposable income level in Denmark was ~34,100€ [36]. Occupational status was categorised into employment, retirement pension (including early retirement), and social benefits (unemployment, sick leave, social security, disability pension, and education grant) [37]. Cohabitation status was categorised as ’living alone: yes’ and ’living alone: no’ [38]. Ethnicity was categorised into Danish origin, Western origin, and non-western origin, based on country of origin and parents birth or citizenship country [39, 40].
Healthcare professionals were encouraged to document it in the electronic health record if, during the telephone conversation (Step 1, Fig. 1), CSs expressed that they did not wish to receive PRO or if the healthcare professional assessed that the CS would be unable to complete PRO due to, e.g., language or cognitive barriers. To gain further insight into non-administration, an audit of the health records of those who had not received PRO was conducted. Reasons for non-administration of PRO were recorded and subsequently categorised into themes.
Statistical analysis
Sociodemographic characteristics are presented as numbers and proportions. Audit results are presented as numbers. Associations between PRO platform and non-administration rates and non-response rates in PRO were analysed by crude and multivariate logistic regression adjusting for age, sex (male or female), and education (high, medium, low). A confidence interval of 95% was used.
For each PRO platform, non-administration rates, non-response rates, and crude odds ratios were determined for each sociodemographic characteristic using logistic regression. Multivariate logistic regression adjusting for age, sex, and education was used to estimate adjusted odds ratios. The number of CSs in the individual analyses varied due to missing values for variables obtained via registers. Statistical analyses were performed using R.
Results
Participants
During the study period, 1868 (platform 1) and 1446 (platform 2) CSs were booked for an initial consultation (population 1a and 2a, respectively). Of these, 1635 (87.5%) and 1163 (80.4%) were included in PRO (population 1b and 2b, respectively) (Fig. 2). The sociodemographic characteristics of the two populations can be seen in Table 1. Across populations, most CSs were female, aged 40–64 years, had a high level of education, and were of Danish origin. The most predominant diagnoses were cancers of the breast, digestive organs, and respiratory and intrathoracic organs (Supplementary table).
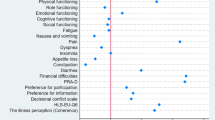
Non-administration
The non-administration rate increased from 12.5% to 19.6% with the organizational change from PRO platform 1 to 2 with non-administration being significantly more likely for platform 2 (Table 2). For both platforms, non-administration was significantly associated with lower educational levels, lower family income levels, social benefits, and being of non-western origin (Table 3). Adjusting for covariables lowered the odds ratio, but associations remained significant. For platform 1, an age of ≥75 years was significantly associated with non-administration but was no longer significant when adjusting for sex and educational level. For platform 2, ages 65–74 years and ≥75 years were significantly associated with non-administration. Adjusting for covariables increased the point estimates and exhibited odds of 2.22 to 4.58-fold respectively, for non-administration. Living alone was not associated with non-administration for either platform. An audit of reasons for non-administration documented in the health record showed that no reason had been recorded for 73 out of 233 CSs and 94 out of 283 CSs for platforms 1 and 2, respectively. The major reason for non-administration was that rehabilitation was not initiated. All CSs were contacted by phone and despite referral, rehabilitation was not initiated; therefore, no PRO was administered. Other reasons included CSs’ inability to understand Danish, technical issues such as lacking a national digital ID or IT equipment, CS reluctance to fill out PRO at the centre, CS opting out of PRO, or factors such as cognitive issues, age, impaired vision, or psychological concerns (Table 4).
Non-response
The non-response rate increased from 9.6% to 12.0% with the organisational change from PRO platform 1 to 2 (Table 2). Non-response was significantly more likely for platform 2. For each platform, non-response was significantly associated with lower educational levels, lower disposable family income levels, and retirement pension, or social benefits (Table 5). This was also the case when adjusting for covariables except for retirement pension. Higher age was associated with non-response for both platforms but only remained significant for the highest age group for platform 2 after adjustment. For platform 1, living alone was significantly associated with non-response. For platform 2, being of non-western origin was significantly associated with non-response.
Discussion
This study demonstrates that non-administration of and non-response to PROs were associated with lower socioeconomic status. Furthermore, the study found that workflows and platforms used had an impact on non-administration of and non-response to PROs. An altered workflow in connection with the implementation of platform 2 resulted in an increase in non-administration. Platform 1 was replaced by platform 2 to support the healthcare professional-CS dialogue with a better visualisation of PRO answers, comply with regulations for health records, general data protection rights (GDPR), and to increase data security. A side-effect of the increased security might have been the statistically significant increase in inequality in who responded to PROs. However, this must be balanced against the benefits in terms of improved usefulness in the consultation (e.g., automatic colour-coding, changes in responses over time) and safe storage of health record data. Although platform 1 is no longer in use, the insights gained regarding the influence of various workflows and platforms on administration and response in clinical practice are transferable. The results can inform the implementation of PRO platforms and the development of effective workflow strategies around them.
Non-administration
Most studies report on response rates in connection with the use of PRO in clinical studies with defined inclusion criteria, whereas few studies focus on the administration of PROs to patients in a pragmatic setting. In the current study, non-administration of PRO ranged from 9.6% to12.0%. In comparison, an out-patient clinic that utilizes both PRO-based and conventional follow-up determines inclusion in PRO-based follow-up through healthcare professionals’ assessment and the patients’ preferences. This clinic reports that approximately 50% of patients are included in PRO-based follow-up [41]. Another study in an outpatient clinic found administration rates of approximately 90 to95% after implementation of PROs via unmounted tablets for data collection in the waiting room immediately after patient registration [42]. In line with our findings, these studies found that the administration of PRO was significantly lower for older patients [42] and socioeconomically disadvantaged patients [41].
We found an increase in non-administration with the organisational shift from platform 1 to platform 2. This may be due to the shift in workflow that created additional demands on healthcare professionals. For example, the PRO platform was not integrated with the electronic health record, and healthcare professionals had to log in to a different platform to assign PRO to CSs. Other studies have shown that healthcare professionals’ competing clinical priorities may threaten the inclusion in PRO [15, 43, 44]. We found that, in contrast to platform 1, people over 65 years old were less likely to be included with the change to platform 2. It is possible that CSs who were not administered PROs in the current setting may also be less inclined to respond to them. The characteristics of this subpopulation were associated lower socioeconomic status which has previously been related to non-response [19, 24]. The intention was to encompass all CSs scheduled for an initial consultation in the PRO, which unfortunately was not accomplished for any of the platforms. An audit of patient records revealed that healthcare professionals recorded various reasons for non-administration. The major reason was that no rehabilitation was initiated. This is a valid reason for non-administration of PRO and indicates that the true non-administration rate may be lower. Factors such as technical barriers, language barriers, cognitive issues, age, impaired vision, or psychological concerns were also recorded. However, it was not always clear whether it was a healthcare professional assessment or the CSs choice to opt out of PRO. In palliative care, gatekeeping, where healthcare professionals shield their patients from entering studies or using PROs because of a notion that it will be too burdensome for the patient to participate due to, e.g., disease burden or cognitive impairment, is a known concern [45, 46]. Similarly, in a study implementing a digital version of the guided self-determination tool, the healthcare professionals had concerns on the patients’ behalf about age, digital skills, and cognitive function [47].
Non-response
For both platforms, non-response was associated with indicators of lower socioeconomic status such as educational level, family income level, and occupational status. This is in line with findings from other studies [17,18,19,20,21]. In the current study, electronic PRO platforms were used. Some studies have shown that response rates were higher for manual PROs compared to electronic PRO platforms [17, 18, 21], while others have found only minor differences [48, 49]. The use of electronic PRO platforms may be an issue for persons of higher age, lower educational level, or ethnic minorities [17], although a Danish study showed only minor socioeconomic differences between non-respondents of paper- or web-based PROs [21]. This study allows us to compare non-response between two different electronic platforms. Notably, the non-response rate increased from 12.5% for platform 1 to 19.6% for platform 2. This can possibly be attributed to the increased complexity for CSs using platform 2, which was designed to comply with regulations for patient records. In this case, CSs had to first log on to their personal digital mailbox to access the link to the platform and then use their digital ID to access the PRO platform. Interestingly, for platform 2, we observed that CSs of non-western origin were less likely to respond than for platform 1. An increased non-response rate could also be caused by a decreased attention to information about PRO in Step 1, Fig. 1. The lack of utilisation of electronically administered PROs could be due to various barriers, including technical issues and usability problems with the PRO platform, concerns about data security, and the inability to use PROs due to health issues, cognitive limitations, or language barriers [14, 28].
Implications for multipurpose use of PROs in clinical practice
When utilising PROs in a primary healthcare cancer rehabilitation setting, it becomes crucial to contemplate populations that are either not included or unresponsive to PROs. On an individual level, these populations are at risk of not undergoing a systematic health status assessment, and the benefits of preparing for their consultation with a healthcare professional by answering questions related to their health status. Previous studies have shown that systematic health status assessment via patient self-assessment reveals more symptoms than open-ended questions in consultations [11, 50]. On an aggregated level, it remains pivotal to take these populations into account while devising new service innovations based on PRO data. Furthermore, when comparing PRO data across sectors or institutions, it is imperative to consider workflows surrounding PRO and the PRO platform, as this could significantly influence both the quantity and the demographics of those who respond. Various PRO platforms are used in different settings. Both administrators and healthcare professionals should be aware that switching platforms has implications for PRO.
Limitations
Overall, compared to other studies, the non-administration and non-response rates are low [18, 51]. Denmark is one of the most digitised countries in Europe [52], and the digital mailbox system is not comparable to many other countries. However, we believe the insights gained on how different workflows and platforms impact administration and response in clinical practice is transferable to other populations. The present study has a cross-sectional design, and we cannot establish a direct cause-effect relationship. There could be multiple causes to differences over time, and we have only looked at some of the major structural differences between the two platforms. In the rehabilitation centre, PROs are used at the initial consultation, at follow-up consultations, and at the completion consultation. We focused on the non-administration of and non-response to PRO at the initial consultation, as PRO administration is systematic and PRO as a dialogue tool is highly accepted among healthcare professionals. However, this aspect is still a work in progress for follow-up and completion consultations. Future studies should focus on adherence to PRO over time. A previous study showed that there is inequality in both referral to rehabilitation and attendance in rehabilitation [32]. Thus, the findings may not be representative of the broader cancer population. Another important limitation is the aspect of time, and effects of external factors. The two platforms were implemented sequentially, and although the implementation period for both platforms is included in the study, the study period for platform 1 includes timepoints during the Covid-19 pandemic where shutdowns and restrictions increased inequality in access to healthcare for various chronic conditions [53]. In the statistical analyses, age was grouped into 18–39 years, 40–64 years, 65–74 years, and ≥75 years. This grouping was chosen because it makes sense in our clinical setting. However, this may not be generalisable to other settings. In general, CSs under 40 years of age are defined as young adult cancer survivors and may have different rehabilitation needs than older cancer survivors [54]. In Denmark, CSs under the age of 67 are likely to be on the labour market and, as such, may have different rehabilitation needs than age-retired CSs. Over the age of 65, citizens in the municipality of Copenhagen are entitled to various home-based interventions. CSs over the age of 75 are less inclined to take up rehabilitation after referral to the centre, and when they take up rehabilitation they do not participate in as many interventions as other age groups. The audit results should only be seen as an indication of the reasons for non-administration. Reasons for non-administration were only recorded in two-thirds of audited health records, and it was not always clear whether it was the CS’s or the healthcare professional’s choice to opt out of PRO.
Conclusion
To our knowledge, this is the first study that examines participation in PRO in a primary healthcare setting and across two different electronic PRO platforms. The present findings underpin the impact clinical workflows surrounding PROs as well as the PRO platforms used have on how many and who participates in PRO. It is therefore important to have a continuous focus on organisational health literacy responsiveness and implement changes that support the inclusion of diverse CS groups in PRO, such as, getting rid of inappropriate workflows and introducing PROs in other languages, as well as a continuous focus on how healthcare professionals communicate about PRO with CSs. A focus on continuous monitoring of the administration of and response to PROs is also important when working with PROs in clinical practice. This is to be aware of the impact of changing workflows or new platforms and the implications this might have on the individual level, and when comparing PRO answers across institutions and sectors.
Data availability
The data that support the findings of this study are available from Statistics Denmark and the Health and Care Administration of the Municipality of Copenhagen, but restrictions apply to the availability of these data, which were used under approval from the regional ethics committee for the current study, and so are not publicly available.
Abbreviations
- PROs:
-
Patient reported outcomes
- CS:
-
Cancer survivor
- ISCED:
-
International Standard Classification of Education
- FACT-G:
-
Functional Assessment of Cancer Therapy - General
References
LeBlanc TW, Abernethy AP (2017) Patient-reported outcomes in cancer care — hearing the patient voice at greater volume. Nat Rev Clin Oncol 14:763–772
Lehmann J, Rothmund M, Riedl D, et al (2021) Clinical outcome assessment in cancer rehabilitation and the central role of patient-reported outcomes. Cancers (Basel) 14:84
Basch E, Barbera L, Kerrigan CL, et al (2018) Implementation of patient-reported outcomes in routine medical care. Am Soc Clin Oncol Educ Book 38:122–134
Howell D, Molloy S, Wilkinson K, et al (2015) Patient-reported outcomes in routine cancer clinical practice: a scoping review of use, impact on health outcomes, and implementation factors. Ann Oncol 26:1846–1858
Greenhalgh J, Gooding K, Gibbons E, et al (2018) How do patient reported outcome measures (PROMs) support clinician-patient communication and patient care? A realist synthesis. J Patient Rep Outcomes 2:42
Kotronoulas G, Kearney N, Maguire R, et al (2014) What is the value of the routine use of patient-reported outcome measures toward improvement of patient outcomes, processes of care, and health service outcomes in cancer care? A systematic review of controlled trials. JCO 32:1480–1501
Velikova G, Booth L, Smith AB, et al (2004) Measuring quality of life in routine oncology practice improves communication and patient well-being: a randomized controlled trial. J Clin Oncol 22:714–724
Berry DL, Blumenstein BA, Halpenny B, et al (2011) Enhancing patient-provider communication with the electronic self-report assessment for cancer: a randomized trial. J Clin Oncol 29:1029–1035
Koczwara B, Knowles R, Beatty L, et al (2023) Implementing a web-based system of screening for symptoms and needs using patient-reported outcomes in people with cancer. Support Care Cancer 31:69
Payne A, Horne A, Bayman N, et al (2023) Patient and clinician-reported experiences of using electronic patient reported outcome measures (ePROMs) as part of routine cancer care. J Patient Rep Outcomes 7:42
Strömgren AS, Groenvold M, Sorensen A, et al (2001) Symptom recognition in advanced cancer. A comparison of nursing records against patient self-rating. Acta Anaesthesiol Scand 45:1080–1085
Lavallee DC, Chenok KE, Love RM, et al (2016) Incorporating patient-reported outcomes into health care to engage patients and enhance care. Health Aff (Millwood) 35:575–582
Eriksen J, Bygholm A, Bertelsen P (2020) The purpose of Patient-Reported Outcome (PRO) post its digitalization and integration into clinical practice: an interdisciplinary redefinition resembling PROs theoretical and practical evolvement. Appl Sci 10:7507
Nielsen AS, Kidholm K, Kayser L (2020) Patients’ reasons for non-use of digital patient-reported outcome concepts: a scoping review. Health Informatics J 26:2811–2833
Nic Giolla Easpaig B, Tran Y, Bierbaum M, et al (2020) What are the attitudes of health professionals regarding patient reported outcome measures (PROMs) in oncology practice? A mixed-method synthesis of the qualitative evidence. BMC Health Serv Res 20:102
Ho A, Purdie C, Tirosh O, et al (2019) Improving the response rate of patient-reported outcome measures in an Australian tertiary metropolitan hospital. Patient Relat Outcome Meas 10:217–226
Pugh SL, Rodgers JP, Yeager KA, et al (2020) Characteristics of participation in patient-reported outcomes and electronic data capture components of NRG oncology clinical trials. Int J Radiat Oncol Biol Phys 108:950–959
Neve OM, van Benthem PPG, Stiggelbout AM, et al (2021) Response rate of patient reported outcomes: the delivery method matters. BMC Med Res Methodol 21:220
Hutchings A, Neuburger J, Grosse Frie K, et al (2012) Factors associated with non-response in routine use of patient reported outcome measures after elective surgery in England. Health Qual Life Outcomes 10:34
Hyland CJ, Guo R, Dhawan R, et al (2022) Implementing patient-reported outcomes in routine clinical care for diverse and underrepresented patients in the United States. J Patient Rep Outcomes 6:20
Ebert JF, Huibers L, Christensen B, et al (2018) Paper- or web-based questionnaire invitations as a method for data collection: cross-sectional comparative study of differences in response rate, completeness of data, and financial cost. J Med Internet Res 20:e24
Neter E, Brainin E (2012) eHealth literacy: extending the digital divide to the realm of health information. J Med Internet Res 14:e19
Rossen S, Kayser L, Vibe-Petersen J, et al (2019) Technology in exercise-based cancer rehabilitation: a cross-sectional study of receptiveness and readiness for e-Health utilization in Danish cancer rehabilitation. Acta Oncol 1–9
Kroll T, Wyke S, Jahagirdar D, et al (2014) If patient-reported outcome measures are considered key health-care quality indicators, who is excluded from participation? Health Expect 17:605–607
Egholm CL, Jensen S, Wandel A, et al (2023) The implementation of the 2017 national policy on patient-reported outcomes in Denmark: an overview of developments after six years. Health Policy 130:104755
Meggetto E, Kent F, Ward B, et al (2020) Factors influencing implementation of organizational health literacy: a realist review. J Health Organ Manag (ahead-of-print. Epub ahead of print). https://doi.org/10.1108/JHOM-06-2019-0167
Trezona A, Dodson S, Osborne RH (2017) Development of the organisational health literacy responsiveness (Org-HLR) framework in collaboration with health and social services professionals. BMC Health Serv Res 17:513
Sisodia RC, Dankers C, Orav J, et al (2020) Factors associated with increased collection of patient-reported outcomes within a large health care system. JAMA Netw Open 3:e202764
Vrangbæk K (2020) Denmark, International health care system profiles. https://www.commonwealthfund.org/international-health-policy-center/countries/denmark. Accessed 28 June 2023
FACT-G. FACIT Group. https://www.facit.org/measures/FACT-G. Accessed 25 Sep 2023
Statistik om Digital Post. https://digst.dk/it-loesninger/digital-post/om-loesningen/tal-og-statistik/. Accessed 8 Feb 2024
Oksbjerg Dalton S, Halgren Olsen M, Moustsen IR, et al (2019) Socioeconomic position, referral and attendance to rehabilitation after a cancer diagnosis: a population-based study in Copenhagen, Denmark 2010-2015. Acta Oncol 58:730–736
HFAUDD. https://www.dst.dk/da/TilSalg/Forskningsservice/Dokumentation/hoejkvalitetsvariable/hoejst-fuldfoerte-uddannelse/hfaudd. Accessed 19 June 2023
International Standard Classification of Education (ISCED), https://ec.europa.eu/eurostat/statistics-explained/index.php?title=International_Standard_Classification_of_Education_(ISCED). Accessed 19 June 2023
TIMES variabel - FAMAEKVIVADISP_13, https://www.dst.dk/da/Statistik/dokumentation/Times/personindkomst/famaekvivadisp-13. Accessed 19 June 2023
Statistics Denmark, https://m.statbank.dk/?lang=en. Accessed 30 Aug 2023
SOCIO13, https://www.dst.dk/da/TilSalg/Forskningsservice/Dokumentation/hoejkvalitetsvariable/personers-tilknytning-til-arbejdsmarkedet-set-over-hele-aaret–akm-/socio13. Accessed 19 June 2023
FAMILIE_TYPE, https://www.dst.dk/da/TilSalg/Forskningsservice/Dokumentation/hoejkvalitetsvariable/familier/familie-type. Accessed 19 June 2023
OPR_LAND, https://www.dst.dk/da/TilSalg/Forskningsservice/Dokumentation/hoejkvalitetsvariable/udlaendinge/opr-land. Accessed 19 June 2023
IE_TYPE, https://www.dst.dk/da/TilSalg/Forskningsservice/Dokumentation/hoejkvalitetsvariable/udlaendinge/ie-type. Accessed 19 June 2023
Schougaard LMV, de Thurah A, Christensen J, et al (2020) Sociodemographic, personal, and disease-related determinants of referral to patient-reported outcome-based follow-up of remote outpatients: a prospective cohort study. Qual Life Res 29:1335–1347
Papuga MO, Dasilva C, McIntyre A, et al (2018) Large-scale clinical implementation of PROMIS computer adaptive testing with direct incorporation into the electronic medical record. Health Syst (Basingstoke) 7:1–12
Mejdahl CT, Schougaard LMV, Hjollund NH, et al (2018) Exploring organisational mechanisms in PRO-based follow-up in routine outpatient care - an interpretive description of the clinician perspective. BMC Health Serv Res 18:546
Nguyen H, Butow P, Dhillon H, et al (2020) Using patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs) in routine head and neck cancer care: what do health professionals perceive as barriers and facilitators? J Med Imaging Radiat Oncol 64:704–710
Bausewein C, Simon ST, Benalia H, et al (2011) Implementing patient reported outcome measures (PROMs) in palliative care–users’ cry for help. Health Qual Life Outcomes 9:27
Head BA, Schapmire TJ, Zheng Y (2017) Telehealth in palliative care: a systematic review of patient-reported outcomes. J Hosp Palliat Nurs 19:130–139
Olesen ML, Rossen S, Jørgensen R, et al (2023) Usefulness of a digitally assisted person-centered care intervention: qualitative study of patients’ and nurses’ experiences in a long-term perspective. JMIR Nurs 6:e46673
Hohwü L, Lyshol H, Gissler M, et al (2013) Web-based versus traditional paper questionnaires: a mixed-mode survey with a Nordic perspective. J Med Internet Res 15:e173
Horevoorts NJ, Vissers PA, Mols F, et al (2015) Response rates for patient-reported outcomes using web-based versus paper questionnaires: comparison of two invitational methods in older colorectal cancer patients. J Med Internet Res 17:e111
Homsi J, Walsh D, Rivera N, et al (2006) Symptom evaluation in palliative medicine: patient report vs systematic assessment. Support Care Cancer 14:444–453
Richards HS, Blazeby JM, Portal A, et al (2020) A real-time electronic symptom monitoring system for patients after discharge following surgery: a pilot study in cancer-related surgery. BMC Cancer 20:543
The Digital Economy and Society Index (DESI)| Shaping Europe’s digital future, https://digital-strategy.ec.europa.eu/en/policies/desi. Accessed 7 Feb 2024
Pandemien forstærkede uligheden i sundhedsvæsenet, https://www.rkkp.dk/nyheder/pandemien-forstarkede-uligheden-i-sundhedsvasenet/. Accessed 30 Aug 2023
Andersen NH, Christiansen JA, la Cour K, et al (2022) Differences in functioning between young adults with cancer and older age groups: a cross-sectional study. European J Cancer Care 31 (Epub ahead of print). https://doi.org/10.1111/ecc.13660
Acknowledgements
The authors wish to thank Charlotte Juel Pihl for auditing health records to identify reasons for non-administration and Pia Juul Bjertrup for categorising these reasons. Special thanks are also extended to Karen Trier for her valuable input on workflows relevant to each platform at the time, and to Carina Wedell Andersen for her assistance in refining the figures.
Funding
The implementation of PRO and the development of PRO platform 2 in the Copenhagen Centre for Cancer and Health was supported through a grant from The Danish Health Authority and with funds from the Health and Care Administration of the Municipality of Copenhagen. None of the funding bodies had any role in the study design, collection, analysis, or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study. SR acquired and analysed the data and drafted the manuscript. All authors read, revised, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The use of data from patient records was approved by the ethical committee of the Capital Region Nr. R-22060676.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rossen, S., Sandager, M., Hofland, D. et al. Are all cancer survivors included when using electronically administered patient reported outcomes in primary healthcare cancer rehabilitation? A cross-sectional study. J Patient Rep Outcomes 8, 67 (2024). https://doi.org/10.1186/s41687-024-00753-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41687-024-00753-5