Abstract
Background
The construct validity and interpretation of the Patient-Reported Outcome Measurement Information System (PROMIS®) Physical Function short form 20a (PF20a) questionnaire were evaluated for patients with late-onset Pompe disease (LOPD), a rare, autosomal recessive, progressive neuromuscular disorder treatable by enzyme replacement therapy (ERT).
Methods
In the phase 3 PROPEL study, adults with LOPD underwent testing of physical functioning and had PRO measurements at baseline and at weeks 12, 26, 38, and 52 while receiving experimental or standard-of-care ERT. All patients were pooled for analyses, without comparisons between treatment groups. Associations and correlations between PROMIS PF20a scores and the 6-minute walk distance (6MWD), % predicted forced vital capacity (FVC), manual muscle test (MMT) of the lower extremities, Gait, Stairs, Gowers’ maneuver, Chair (GSGC) score, and Rasch-built Pompe-specific Activity (R-PAct) scale were evaluated by calculating regression coefficients in linear regression models and Pearson correlation coefficients (R); patients’ age, sex, race, ERT prior to study, body mass index, and study treatment were included as covariables. The minimal clinically important difference (MCID) of PROMIS PF20a was determined using distribution- and anchor-based methods.
Results
123 patients received at least 1 dose of ERT. In multivariable analyses, PROMIS PF20a scores had strong correlations with R-PAct scores (R = 0.83 at baseline and R = 0.67 when evaluating changes between baseline and 52 weeks) and moderate correlations with the 6MWD (R = 0.57 at baseline and R = 0.48 when evaluating changes between baseline and 52 weeks). Moderate correlations were also observed between PROMIS PF20a and MMT (R = 0.54), GSGC (R=-0.51), and FVC (R = 0.48) at baseline. In multivariable linear regression models, associations were significant between PROMIS PF20a and 6MWD (P = 0.0006), MMT (P = 0.0034), GSGC (P = 0.0278), and R-PAct (P < 0.0001) at baseline, between PROMIS PF20a and 6MWD (P < 0.0001), FVC (P = 0.0490), and R-PAct (P < 0.0001) when combining all measurements, and between PF20a and 6MWD (P = 0.0016) and R-PAct (P = 0.0001) when evaluating changes in scores between baseline and 52 weeks. The anchor-based and distribution-based MCID for a clinically important improvement for PROMIS PF20a were 2.4 and 4.2, respectively.
Conclusions
PROMIS PF20a has validity as an instrument both to measure and to longitudinally follow physical function in patients with LOPD.
Trial registration
ClinicalTrials.gov, NCT03729362. Registered 2 November 2018, https://www.clinicaltrials.gov/search?term=NCT03729362.
Plain English summary
Late-onset Pompe disease (LOPD) is a rare, hereditary disease. Patients with LOPD have decreased production of an enzyme, which leads to symptoms that gradually get worse, including muscle weakness and trouble breathing. Enzyme replacement therapy may slow down the disease progression. In recent years, enzyme replacement therapies have been improved. To measure the benefit of such new therapies, patients with LOPD are asked to fill in surveys about their symptoms before and during treatment, but there is no standard survey to use. In this study, we used a survey called the Patient-Reported Outcome Measurement Information System (PROMIS®) Physical Function short form 20a (PF20a) questionnaire. This questionnaire is used for various diseases and tests someone’s ability to perform daily physical activities such as getting dressed. We compared the results of this survey to other tests which evaluate a variety of functions, such as how far a patient can walk in 6 minutes, leg muscle strength, and a patient’s lung capacity. In general, we found that the score provided by the PROMIS PF20a questionnaire had moderate to strong agreement with other test scores. Furthermore, we looked at the minimum difference in PROMIS PF20a scores that a patient found a relevant difference (i.e., a relevant improvement or worsening of the disease). Patients found a difference between 2.4 and 4.2 points in the score relevant. The results from this study show that PROMIS PF20a may be used to measure symptoms and follow symptoms over time in patients with LOPD.
Similar content being viewed by others
Background
Pompe disease is a rare, autosomal recessive, metabolic disorder [1]. Due to pathogenic variants in the GAA gene, patients have an acid α-glucosidase (GAA) deficiency, leading to accumulation of glycogen in lysosomes. In late-onset Pompe disease (LOPD), patients have some residual enzyme activity (ranging from ~ 1% to 2% up to 40%), resulting in an onset of symptoms ranging from early childhood to late adulthood [2, 3]. Symptoms of LOPD are predominantly related to skeletal muscle and diaphragmatic dysfunction, causing mobility and respiratory difficulties [1]. Treatment consists of enzyme replacement therapy (ERT) to slow disease progression, supplemented by symptomatic treatment and supportive care.
Recently, advances have been made for LOPD treatment with the development of second-generation ERTs using recombinant human GAA (rhGAA), such as avalglucosidase alfa [4, 5] and cipaglucosidase alfa in combination with the small molecule stabilizer miglustat [6]. Avalglucosidase alfa received approval by the United States Food and Drug Administration in 2021 [7] and cipaglucosidase alfa with miglustat received approval by the European Medicines Agency in 2023 [8]. These rhGAAs enhance mannose-6-phosphate receptor-mediated uptake of GAA, resulting in increased clearance of the accumulated glycogen in lysosomes. While not a cure, these agents aim to improve the mobility and respiratory capacity of patients and therefore, to improve the well-being and quality of life of patients with LOPD.
To measure clinically meaningful benefit of rhGAA, patient-reported outcomes (PROs) are used [9, 10]. Examples of PRO measurements previously used in LOPD include the Rotterdam handicap scale, the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36), the Rasch-built Pompe-specific Activity (R-PAct) scale, the Pompe Disease Symptom Scale (PDSS), and the Pompe Disease Impact Scale (PDIS), the latter 3 having been developed recently to specifically evaluate disease progression and treatment in LOPD [5, 11,12,13,14].
As PROs rely on subjective interpretation from patients, PRO measurements need to be validated to ensure they adequately measure relevant and important aspects of the disease, and that limitations of the instrument are known. The extensive recommendations from COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN), driven by an international expert panel, define terminology of measurement properties of PROs and provide guidance evaluating the methodological quality of studies on these measurement properties, recommending assessment of reliability, validity, and responsiveness of PRO measurements [15,16,17]. The International Society for Quality-of-Life Research (ISOQOL) developed minimum standards for PRO measures combining existing literature, including guidance from COSMIN and health authorities [18]. Using recommendations from ISOQOL, COSMIN, and other relevant literature, Francis et al. have subsequently developed a checklist to operationalize PRO measurements, which includes 18 scoring criteria to evaluate the conceptual model, content validity, reliability, construct validity, scoring and interpretation, respondent burden and presentation of the PRO measurement [19].
Validation of PRO measurements is particularly important in LOPD, as no gold standard of PRO measurement exists to date. In previous studies, some validation checks have been conducted to evaluate the use of R-PAct, PDIS, and PDSS in patients with LOPD [13, 14, 20]. In addition, Harfouche et al. evaluated the use of the PRO Measurement Information System (PROMIS®) in 30 patients with Pompe disease, concluding that selected PROMIS questionnaires are meaningful and address important concepts to patients with Pompe disease, including motor function and symptoms of functional disability [21]. However, this study had some limitations, including the low number of patients, open-label design with patients knowing what treatment they were receiving, and that PROMIS was measured at a single time point only. Subsequently, the PROMIS Physical Function short form 20a questionnaire (PROMIS PF20a) was included as a PRO instrument in the PROPEL phase 3 study, its patient-level data providing a key source of cross-sectional and longitudinal data to analyze the questionnaire in LOPD [6]. The PROMIS PF20a measures current self-reported capability of physical activities, including functioning of upper and lower extremities and central regions, and instrumental activities of daily living. It can be used in the adult general population and adults with chronic health conditions, in both clinical trials or clinical practice settings. The aim of this report is to show construct validity of PROMIS PF20a by comparing the scoring of this questionnaire in PROPEL to various tests for physical functioning as well as the R-PAct scale, both cross-sectionally and longitudinally, to further validate its use in LOPD. A further aim was to improve interpretation of the PROMIS PF20a score in patients with LOPD by determining the minimal clinically important difference (MCID) of PROMIS PF20a scores.
Methods
Patient selection
To evaluate the PROMIS PF20a questionnaire in LOPD, data from the PROPEL study were used [6]. PROPEL (NCT03729362) is a global, randomized, double-blind, parallel-group, phase 3 clinical trial that evaluated the efficacy and safety of cipaglucosidase alfa plus miglustat (n = 85) compared to alglucosidase alfa plus placebo (n = 38) in adult patients (age ≥ 18 years, body weight ≥ 40 kg) with confirmed LOPD. Patients were either ERT-naïve or had been treated with alglucosidase alfa for ≥ 2 years (20 mg/kg once every 2 weeks; ERT-experienced). For the analyses in this study, all patients were pooled into 1 cohort without differentiating between treatments, to make use of all available data. A comparison of PROMIS PF20a scores between treatment arms has been conducted as a key secondary endpoint of PROPEL and is described by Schoser et al. [6]. Additional details of the study protocol have been published previously [6].
Data collection
Patients’ baseline characteristics collected in PROPEL and used in the current study include age, sex, race, body mass index (BMI) and previous ERT status (naïve or experienced). Various outcome measurements were evaluated at baseline, weeks 12, 26, 38, and 52. In this study, we included the following outcomes that were measured in PROPEL:
-
PROMIS PF20a [6, 22, 23]: patients answer 20 questions on physical function, which the patient can score from unable to do (1) to being able to do without any difficulties or limitations (5). Hence, the score ranges between 20 and 100, with a higher score indicating better physical functioning.
-
6-minute walk distance (6MWD) [6, 24]: the distance (in meters) a patient can quickly walk within 6 min on a flat surface with walking shoes; walking aids (e.g., a cane, walker, or rollator) were permitted and were used consistently throughout the study, when required.
-
% predicted forced vital capacity (FVC) [6, 25]: the volume of a maximal forced expiratory effort (FVC) after maximal inspiration, while sitting, compared to the FVC for healthy adults in the National Health and Nutrition Examination Survey (NHANES) III.
-
Manual Muscle Test (MMT) of the lower extremities [6, 26]: skeletal muscle strength in the hips and knees is scored using the Medical Research Council scale (0 to 5 points, with a score of 5 indicating normal function and a score of 0 indicating no muscle movement). The final score is the sum of the score for hip flexion and abduction, and knee flexion and extension in both extremities, and therefore, ranges from 0 to 40, with a higher score indicating better muscle function.
-
Gait, Stairs, Gowers’ maneuver, Chair (GSGC) score [6, 27]: the patient walks 10 m (gait), climbs 4 stairs, performs the Gowers’ maneuver (begin lying down on the floor, then rise from the floor to a standing position), and stands up from a chair. Each item is scored from 1 (normal function) to 7 (gait: confined to wheelchair; stairs: unable to climb stairs; Gowers’ maneuver: unable to rise) or 6 (chair: unable to get up from chair) and therefore, ranges from 4 to 27, with a lower score indicating better physical functioning.
-
R-PAct [13]: patients answer a questionnaire of 18 questions to quantify the effect of Pompe disease on their daily activities and social participation. Three answers are possible: 0 = no; 1 = yes, but with difficulty; 2 = yes, without difficulty. Hence, the score ranges from 0 to 36, with a higher score indicating fewer limitations in activities and social participation.
-
Subject’s global impression of change (SGIC) in overall physical well-being [6, 28,29,30]: the patients answer this question using a 7-point rating scale, with answers ‘1 = very much worse’, ‘2 = worse’, ‘3 = somewhat worse’, ‘4 = no change’, ‘5 = somewhat improved’, ‘6 = improved’, and ‘7 = very much improved’.
Evaluation of the PROMIS PF20a questionnaire
To analyze construct validity of the PROMIS PF20a questionnaire, correlation and associations were evaluated between PROMIS PF20a and 6MWD, % predicted FVC, MMT of the lower extremities, GSGC, and R-PAct scores, at baseline, combining all measurements (baseline, weeks 12, 26, 38, and 52), and for changes of scores between baseline and 52 weeks.
Additionally, interpretation of changes in PRO measurements was assessed by determining what represented an MCID in PROMIS PF20a. The MCID has previously been defined as “the smallest difference in score in the domain of interest which patients perceive as beneficial and which would mandate, in the absence of troublesome side effects and excessive cost, a change in the patient’s management” [31, 32]. A distribution-based and anchor-based MCID was calculated. In the anchor-based approach, an external measure is used as an anchor, which has established cut-offs to define clinically meaningful improvement and correlates with the measure for which a MCID will be derived. The SGIC in overall physical well-being was selected as an anchor, as it directly asked patients participating in PROPEL whether they had observed a meaningful benefit (or worsening) in the first year after initiating treatment.
Statistical analyses
For descriptive statistics, categorical variables were summarized by frequency (number of patients) and percentage. Continuous variables were summarized using mean, standard deviation (SD), median, and range.
To evaluate associations between scoring of the PROMIS PF20a and functional measures (6MWD, % predicted FVC, MMT of the lower extremities, and GSGC) or R-PAct, multivariable (adjusted) linear regression models were applied with PROMIS PF20a as the dependent and the respective other measure as independent variable. The models adjusted for age (continuous), sex (categorical: male, female), race (categorical: White, Asian, other), previous ERT status (categorical: naïve, experienced), BMI (continuous), and study treatment (categorical: cipaglucosidase alfa plus miglustat, alglucosidase alfa plus placebo). Regression coefficients (B) including their 95% confidence intervals and p-values were calculated. Additionally, mixed-effects linear regression models, which adjusted for repeated measures at baseline, weeks 12, 26, 38, and 52 within individuals were applied. To evaluate correlations, scatterplots including regression lines were drawn, and the Pearson correlation coefficient (R) was calculated, both for baseline scores and changes in scores after one year of treatment (difference between scores in week 0 and week 52). A Pearson correlation coefficient ≤|0.19| (absolute values, i.e., R between -0.19 and 0.19) was considered very weak correlation, a coefficient ≥|0.20| to ≤|0.39| (i.e., -0.39 to -0.20 or 0.20 to 0.39) a weak correlation, a coefficient ≥|0.40| to ≤|0.59| a moderate correlation, a coefficient ≥|0.60| to ≤|0.79| a strong correlation, and a coefficient ≥|0.80| a very strong correlation [33]. In the main analyses, Pearson correlation coefficients were adjusted for abovementioned covariables; sensitivity analyses excluded these variables from the models (unadjusted models).
The distribution-based MCID was calculated by taking 1/3 of the SD of the PROMIS PF20a scores at baseline of all PROPEL patients [34,35,36]. The anchor-based MCID for improvement and deterioration were defined as the mean change from baseline in PROMIS PF20a scores in patients who had reported that their overall physical well-being had somewhat improved (SGIC score = 5) or somewhat worsened (SGIC score = 3) at week 52, respectively [31]. As a sensitivity analysis, the MCID was defined as the mean change in PROMIS PF20a scores in patients who had reported that their overall physical well-being remained stable (SGIC score = 4).
All statistical analyses were conducted using SAS (version 9.4 TS1M4).
Results
In total, 125 patients were randomized in PROPEL, and 123 patients were dosed with cipaglucosidase alfa plus miglustat (n = 85) or alglucosidase alfa plus placebo (n = 38). Mean age of these 123 patients was 47 years (SD 13 years), patients had a mean BMI of 25 kg/m2 (SD 6 kg/m2), 55% of the patients were female, most patients (85%) were White and 77% had previously received ERT (Supplementary Table 1). In the outcomes analyses, 1 patient was excluded as the patient deliberately underperformed at baseline to gain entry into the study [6]. Results from outcomes measuring physical function and PROs in the PROPEL study are summarized in Table 1. At baseline, having pooled patients from both treatment groups into 1 cohort, the mean PROMIS PF20a score was 67 (SD 12, n = 121), patients walked a mean distance of 356 m (SD 114 m, n = 122) in the 6MWD test, had a % predicted FVC of 70 (SD 20, n = 122), and scored on average 28 (SD 6, n = 118), 15 (SD 5, n = 106), and 20 (SD 6, n = 102) on the MMT of lower extremities, GSGC, and R-PAct scores, respectively. After 52 weeks, the mean PROMIS PF20a, MMT of lower extremities, GSGC, and R-PAct scores changed to 69 (SD 14, n = 121), 29 (SD 6, n = 114), 14 (SD 5, n = 102), and 21 (SD 7, n = 102), respectively; patients walked a mean distance of 372 m (SD 127, n = 122) in the 6MWD test, and had a % predicted FVC of 69 (SD 20, n = 121).
In univariable linear regression models, PROMIS PF20a scores were significantly associated with all other outcome measures (Table 2), both at baseline (P ≤ 0.0004) and when combining all measurements (P ≤ 0.0023). As expected, associations were negative between PROMIS PF20a and GSGC scores, but positive for all other outcomes, as a higher GSGC score indicates worse physical functioning while in all other outcomes a higher score indicates better functioning. PROMIS PF20a scores were also significantly associated with 6MWD (B = 0.09, 95% CI 0.05 to 0.12; per 1-meter increment in the 6MWD test) and R-PAct (B = 1.07, 95% CI 0.65 to 1.50; per 1-point increment) when evaluating changes in scores between baseline and 52 weeks.
Adjusting for age, sex, race, previous ERT status, BMI, and study treatment in multivariable analyses, directionality of associations remained the same. In these multivariable linear regression analyses, baseline PROMIS PF20a scores were significantly associated to baseline 6MWD (B = 0.04, 95% CI 0.02 to 0.07; per 1-meter increment in the 6MWD test), MMT scores of the lower extremities (B = 0.67, 95% CI 0.23 to 1.11; per 1-point increment), GSGC scores (B=-0.78, 95% CI -1.47 to -0.09; per 1-point increment), and R-PAct scores (B = 1.72, 95% CI 1.36 to 2.08; per 1-point increment), but not to the baseline % predicted FVC (B = 0.10, 95% CI -0.04 to 0.24; per 1% increment in predicted FVC). Changes in PROMIS PF20a scores between baseline and 52 weeks were significantly associated with changes in the 6MWD (B = 0.08, 95% CI 0.03 to 0.12) and R-PAct scores (B = 1.03, 95% CI 0.52 to 1.53). Combining measurements at all timepoints in a multivariable, mixed-effects, linear regression model, associations were significant between PROMIS PF20a scores and the 6MWD (B = 0.05, 95% CI 0.03 to 0.06), R-PAct scores (B = 1.23, 95% CI 1.04 to 1.41), and % predicted FVC (B = 0.08, 95% CI 0.00 to 0.17, P = 0.049). In summary, these results indicated that PROMIS PF20a scores were associated with other physical function measures, particularly with R-PAct scores and the 6MWD.
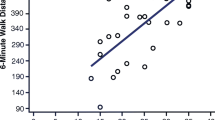
These results were further confirmed by evaluating correlations between PROMIS PF20a and other outcome measures using Pearson’s correlation coefficients (Fig. 1 and Supplementary Fig. 1). In multivariable analyses, a very strong correlation was observed between PROMIS PF20a and R-PAct scores (R = 0.832), and moderate correlations were observed between PROMIS PF20a and 6MWD (R = 0.568), MMT of the lower extremities (R = 0.540), GSGC (R=-0.508), and % predicted FVC (R = 0.483) at baseline (Fig. 1A). When evaluating changes between baseline and 52 weeks, the correlation between PROMIS PF20a and R-PAct remained strong (R = 0.671) and the correlation between PROMIS PF20a and 6MWD remained moderate (R = 0.475), whereas the correlations between PROMIS PF20a and GSGC (R=-0.394), MMT of the lower extremities (R = 0.360), and % predicted FVC (R = 0.355) were moderate (Fig. 1B).
Correlation between PROMIS Physical Function short form 20a scores and other outcome measures, adjusted model. P-values are determined by multivariable linear regression. 6MWD: 6-minute walk distance; FVC: forced vital capacity; GSGC: gait, stairs, Gowers’ maneuver, chair; MMT: manual muscle test; N: number of patients; R: Pearson’s correlation coefficient; R-PAct: Rasch-built Pompe-specific Activity scale
In the final analyses, the MCID was determined. The SD of PROMIS PF20a scores at baseline was 12.5, thus, the distribution-based MCID was established at 4.2. Using this cutoff, 28% (N = 34) of patients in PROPEL reported an improvement in PROMIS PF20a score after 1 year at or above the MCID (≥ 4.2), and 20% (N = 24) were considered to have a clinically important worsening of symptoms (i.e., their PROMIS PF20a scores after 1 year was equal to or below -4.2).
In the anchor-based approach, changes in PROMIS PF20a scores between baseline and week 52 were compared to the SGIC overall physical well-being as reported in week 52. A weak but significant correlation was observed between the two outcome measurements (R = 0.2836, P = 0.0020) in an unadjusted analysis, and therefore, the SGIC overall physical well-being was considered suitable as an anchor to determine the MCID for the PROMIS PF20a scores.
Patients reporting that their overall physical well-being remained stable (N = 45) or improved (N = 49), had on average a positive change in PROMIS PF20a scores, ranging from 2.2 (SD 10.0) for those reporting stable overall physical well-being to 8.5 (SD 11.9) for those reporting a much improved overall physical well-being (Table 3). The anchor-based MCID for improvement was established at 2.4, which corresponded to the mean change in PROMIS PF20a score for those patients reporting an improvement (score = 5) in the SGIC overall physical well-being (mean 2.4, SD 6.7). Using this cut-off, 38% (N = 46) of patients in PROPEL had a change in PROMIS PF20a score after 1 year compared to baseline equal to or larger than the MCID for improvement (≥ 2.4). The anchor-based MCID for deterioration was established at -3.4, which corresponded to the mean change in PROMIS PF20a score for those patients reporting a worsening (score = 3) in the SGIC overall physical well-being (mean -3.4, SD 7.5). Using this cut-off, 24% of LOPD patients in PROPEL had a clinically important worsening based on their change in PROMIS PF20a score at 1 year compared to baseline.
In the sensitivity analysis, the MCID was established at 2.2, which corresponded to the mean change in PROMIS PF20a score for those patients reporting a stabilization in the SGIC overall physical well-being.
Discussion
This study evaluated the construct validity and interpretation of the PROMIS PF20a questionnaire in 122 patients with LOPD, using data from the PROPEL phase 3 study [6]. PROMIS PF20a scores generally correlated well and showed statistically significant associations with the functional measures 6MWD, % predicted FVC, MMT, and GSGC, and with R-PAct, in cross-sectional assessments and to a lesser extent in longitudinal assessments. The functional measures evaluated in this study are relevant clinical measures in Pompe disease and are typically included in clinical trials to assess efficacy of treatments in LOPD. Furthermore, outcomes such as the 6MWD are considered relevant in Pompe disease by various health technology assessment bodies [37].
In our data, the PROMIS PF20a score had the strongest correlations with the R-PAct scale and 6MWD, both in cross-sectional and longitudinal measurements. This correlation between PROMIS PF20a and R-PAct scores was expected, as the questionnaires evaluate physical performance in similar domains, such as taking a shower and doing yard work [13, 22]. PROMIS PF20a scores had the weakest correlation with % predicted FVC, but nevertheless, moderate correlations were observed, and a statistically significant association was observed between the 2 outcomes when combining all longitudinal measurements in a multivariable, mixed-effects, linear regression model.
To improve our understanding of how changes in PROMIS PF20a scores should be interpreted in clinical practice, the MCID of PROMIS PF20a was estimated using both a distribution-based and an anchor-based approach, the anchor being the SGIC overall physical well-being score. This anchor was selected as it directly measures clinical improvement in physical well-being in patients and had a significant albeit weak correlation with the PROMIS PF20a score. Depending on the chosen method, derived MCIDs ranged between 2.2 and 4.2 in our study, which is in line with the MCID reported in a systematic review and meta-analysis of PROMIS measures in other populations [38].
Various checklists have been developed to operationalize tools that measure PROs, such as the validation checklist proposed by Francis et al. [19]. In the analyses presented in this manuscript, “construct validity” and “scoring and interpretation” were evaluated in LOPD (Table 4), which are considered key domains of PRO validity. Our data support expected associations with existing PRO measures and other relevant outcomes at single time points. In addition, the questionnaire can measure changes over time (construct validity). Providing the MCID will add to the interpretation of PROMIS PF20a scores and will facilitate to measure individual disease progression and/or therapy benefit in patients with LOPD.
Other characteristics on the validation checklist have been answered previously by PROMIS or other studies. The conceptual model has been described well: PROMIS PF20a measures physical function in an intended respondent population of patients with LOPD, using 2 subscales, both ranging from 0 to 5 (5 = “without any difficulty” or “not at all” to 1 = “unable to do” or “cannot do”) [22].
PROMIS questionnaires have been developed and validated by experts using rigorous methodology; the used methodology, including the use of literature searches, focus groups, and interviews, is described on the PROMIS website [39]. Previous studies have successfully tested the reliability of PROMIS physical function measures in cancer patients [40].
Construct and content validity, and reliability of PROMIS questionnaires, including physical function, has been evaluated previously in a small-scale (N = 30), cross-sectional study of patients with LOPD [21]. Our data now analyzed multiple PROMIS PF20a assessments in a larger cohort (N = 122) of patients with LOPD, allowing longitudinal evaluation of this PRO measurement questionnaire, and therefore, further validating the use of PROMIS PF20a in patients with LOPD. Our data support expected associations between PROMIS PF20a and other functional measures in the patient population. Expected differences in PROMIS PF20a between relevant known groups are corroborated by data from the PROPEL study showing that patients in the 2 treatment arms had differences in PROMIS PF20a scores (with a least square mean difference [95% confidence interval] of 1.9 [-1.5, 5.3]), which was similar to differences in other outcome measurements of physical functioning [6].
Finally, the domains scoring and interpretation, and respondent burden and presentation have been positively evaluated too. The questionnaire is available for public viewing [22] and has been used in patients with a high level of education and in patients with an education level below high school [40, 41]. PROMIS has created documentation explaining how to score the questionnaire and how to handle missing values. PROMIS works actively with communities to have its questionnaire translated in other languages than English, such as Spanish [41, 42]. Since the short form only contains 20 questions with 5 answering options, the time to complete this questionnaire is reasonable and comparable to R-PAct (18 questions with 3 answering options) [13], PDSS (12 questions that are answered on a scale from 0 [none] to 10 [as bad as I can imagine]), and PDIS (15 questions on mobility-related physical activities and mood in the past 24 h, with scales varying from 0 to 3 to 0 to 10) [20, 43].
Combining these findings, we consider that PROMIS PF20a has validity as a PRO measurement tool in patients with LOPD. Future studies are needed to compare PROMIS PF20a to other PRO measurement tools such as R-PAct, PDIS, and PDSS. A strength of PROMIS PF20a compared to these other tools is that PROMIS PF20a is already used in other diseases, and that the score can be computed to a T-score metric, where 50 represents the average score for the general population in the United States and 10 is one standard deviation [44]. This allows comparison of the physical function of a patient with LOPD with the average general population and patients with other diseases.
Limitations
The PROPEL study was not designed to validate PROMIS PF20a, and therefore, the analyses presented in this manuscript should be regarded as secondary, exploratory analyses. However, the advantage of using PROPEL data was that we were able to evaluate PROMIS PF20a in a reasonably-sized cohort, considering the rarity of LOPD. Another limitation of the analyses is that follow-up scores of PRO measurement tools such as PROMIS PF20a are inevitably associated with baseline scores: a greater level of disability at baseline provides more opportunity for improvement than for deterioration. In our analysis, this seems quite balanced as the MCID for improvement (2.4) was relatively similar to the MCID for worsening (3.4).
Potential limitations of the use of MCIDs have been described in detail by Copay et al. [45]. A limitation of using SGIC overall well-being as an anchor is that recall bias may have occurred when patients recalled their health state of a year ago [46, 47]. SGIC is, nevertheless, considered a useful anchor in general as it directly asks patients whether they had observed a meaningful improvement (or worsening) as compared to baseline; in our study, it is important to note that SGIC is significantly, but only weakly correlated with PROMIS PF20a change from baseline at week 52. Moreover, the distribution-based MCIDs in general are not theoretically or empirically tied to any patient-reported experience. Hence MCIDs– whether anchor or distribution-based– in this study are subject to a high degree of uncertainty and should be interpreted cautiously.
Psychometric evaluation might be needed to further support the validation of PROMIS PF20a. Furthermore, considering that LOPD is a slowly progressing disease, longer term evaluation may provide more information on the use of PROMIS PF20a to assess changes in physical function over time.
Conclusions
In patients with LOPD, PROMIS PF20a scores generally correlated well to the 6MWD, % predicted FVC, MMT of lower extremities, GSGC, and R-PAct scores when measured at various time points, and to a lesser extent when evaluating changes in functioning over time. The MCID ranged between 2.2 and 4.2 using different methodological approaches. These results and previously published data on PROMIS PF20a indicate that the questionnaire has validity and is a valuable, easy-to-use and readily available tool to measure physical function in patients with LOPD. Its use should be considered in future clinical studies of patients with LOPD and potentially in clinical practice.
Data availability
Data sharing proposals and requests for data of the PROPEL study will be reviewed on a case-by-case basis. Requests for data should be addressed to Mitchell Goldman at mgoldman@amicusrx.com. Requests will be reviewed by a medical steering committee.
Abbreviations
- 6MWD:
-
6-minute walk distance
- BMI:
-
Body mass index
- COSMIN:
-
Consensus-based Standards for the selection of health Measurement Instruments
- ERT:
-
Enzyme replacement therapy
- FVC:
-
Forced vital capacity
- GAA:
-
Acid α-glucosidase
- GSGC:
-
Gait, stairs, Gowers’ maneuver, chair
- ISOQOL:
-
International Society for Quality-of-Life Research
- LOPD:
-
Late-onset Pompe disease
- MCID:
-
Minimal clinically important difference
- MMT:
-
Manual muscle test
- NHANES:
-
National Health and Nutrition Examination Survey
- PDIS:
-
Pompe Disease Impact Scale
- PDSS:
-
Pompe Disease Symptom Scale
- PF20a:
-
Physical Function short form 20a
- PRO:
-
Patient-reported outcome
- PROMIS:
-
Patient-Reported Outcome Measurement Information System
- rhGAA:
-
Recombinant human acid α-glucosidase
- R-PAct:
-
Rasch-built Pompe-specific Activity scale
- SD:
-
Standard deviation
- SF-36:
-
Medical Outcomes Study 36-Item Short-Form Health Survey
References
van der Ploeg AT, Reuser AJ (2008) Pompe’s disease. Lancet 372:1342–1353
American Association of Neuromuscular & Electrodiagnostic Medicine (2009) Diagnostic criteria for late-onset (childhood and adult) pompe disease. Muscle Nerve 40:149–160
Cupler EJ, Berger KI, Leshner RT et al (2012) Consensus treatment recommendations for late-onset pompe disease. Muscle Nerve 45:319–333
Diaz-Manera J, Kishnani PS, Kushlaf H et al (2021) Safety and efficacy of avalglucosidase alfa versus alglucosidase alfa in patients with late-onset pompe disease (COMET): a phase 3, randomised, multicentre trial. Lancet Neurol 20:1012–1026
Kishnani PS, Diaz-Manera J, Toscano A et al (2023) Efficacy and Safety of Avalglucosidase Alfa in Patients With Late-Onset Pompe Disease After 97 Weeks: A Phase 3 Randomized Clinical Trial. JAMA Neurol
Schoser B, Roberts M, Byrne BJ et al (2021) Safety and efficacy of cipaglucosidase alfa plus miglustat versus alglucosidase alfa plus placebo in late-onset pompe disease (PROPEL): an international, randomised, double-blind, parallel-group, phase 3 trial. Lancet Neurol 20:1027–1037
United States Food and Drug Administration (2021) Avalglucosidase Alfa-ngpt Full Prescribing Information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/761194s000lbl.pdf Accessed 18 Apr 2023
European Medicines Agency (2023) Pombiliti. https://www.ema.europa.eu/en/medicines/human/EPAR/pombiliti Accessed 06 Jun 2023
Weldring T, Smith SM (2013) Patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs). Health Serv Insights 6:61–68
United States Food and Drug Administration (2009) Guidance for Industry: Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims. https://www.fda.gov/media/77832/download Accessed 14 Apr 2023
Hagemans ML, Laforêt P, Hop WJ et al (2007) Impact of late-onset pompe disease on participation in daily life activities: evaluation of the Rotterdam Handicap Scale. Neuromuscul Disord 17:537–543
van der Ploeg AT, Clemens PR, Corzo D et al (2010) A randomized study of alglucosidase alfa in late-onset pompe’s disease. N Engl J Med 362:1396–1406
van der Beek NA, Hagemans ML, van der Ploeg AT et al (2013) The Rasch-built pompe-specific activity (R-PAct) scale. Neuromuscul Disord 23:256–264
Dimachkie MM, Kishnani PS, Ivanescu C et al (2023) Measurement Properties of 2 novel PROs, the Pompe Disease Symptom Scale and Pompe Disease Impact Scale, in the COMET Study. Neurology: Clin Pract 13:e200181
Mokkink LB, Terwee CB, Patrick DL et al (2010) The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol 63:737–745
Mokkink LB, Terwee CB, Patrick DL et al (2010) The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res 19:539–549
Mokkink LB, Terwee CB, Knol DL et al (2010) The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: a clarification of its content. BMC Med Res Methodol 10:22
Reeve BB, Wyrwich KW, Wu AW et al (2013) ISOQOL recommends minimum standards for patient-reported outcome measures used in patient-centered outcomes and comparative effectiveness research. Qual Life Res 22:1889–1905
Francis DO, McPheeters ML, Noud M et al (2016) Checklist to operationalize measurement characteristics of patient-reported outcome measures. Syst Reviews 5:129
Hamed A, Curran C, Gwaltney C et al (2019) Mobility assessment using wearable technology in patients with late-onset pompe disease. NPJ Digit Med 2:70
Harfouche M, Kishnani PS, Krusinska E et al (2020) Use of the patient-reported outcomes measurement information system (PROMIS®) to assess late-onset pompe disease severity. J Patient Rep Outcomes 4:83
Health Measures (2022) PROMIS Short Form v2.0 - Physical Function 20a. https://www.healthmeasures.net/index.php?Itemid=992 Accessed 05 May 2023
Cella D, Riley W, Stone A et al (2010) The patient-reported outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol 63:1179–1194
(2002) ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 166:111–117
The National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention (2011) Spirometry NHANES III Reference Values. https://www.cdc.gov/niosh/topics/spirometry/nhanes.html Accessed 05 May 2023
Vanhoutte EK, Faber CG, van Nes SI et al (2012) Modifying the Medical Research Council grading system through Rasch analyses. Brain 135:1639–1649
Angelini C, Semplicini C, Ravaglia S et al (2012) New motor outcome function measures in evaluation of late-onset pompe disease before and after enzyme replacement therapy. Muscle Nerve 45:831–834
Rampakakis E, Ste-Marie PA, Sampalis JS et al (2015) Real-life assessment of the validity of patient global impression of change in fibromyalgia. RMD Open 1:e000146
Dodick DW, Silberstein S, Saper J et al (2007) The impact of topiramate on health-related quality of life indicators in chronic migraine. Headache 47:1398–1408
Liu H, Tan AD, Qin R et al (2015) Comparing and validating simple measures of patient-reported Peripheral Neuropathy for Oncology clinical trials: NCCTG N0897 (Alliance) a pooled analysis of 2440 patients. SOJ Anesthesiol Pain Manag 2
Jaeschke R, Singer J, Guyatt GH (1989) Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials 10:407–415
Rai SK, Yazdany J, Fortin PR et al (2015) Approaches for estimating minimal clinically important differences in systemic lupus erythematosus. Arthritis Res Ther 17:143
The BMJ (2023) Resources for readers: 11. Correlation and regression https://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one/11-correlation-and-regression Accessed 19 Jun 2023
Ousmen A, Touraine C, Deliu N et al (2018) Distribution- and anchor-based methods to determine the minimally important difference on patient-reported outcome questionnaires in oncology: a structured review. Health Qual Life Outcomes 16:228
Mouelhi Y, Jouve E, Castelli C et al (2020) How is the minimal clinically important difference established in health-related quality of life instruments? Review of anchors and methods. Health Qual Life Outcomes 18:136
Health, USDo, Human Services FDACfDE, Research et al (2006) Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes 4:79
Raza S, Keyzor I, Shohet S et al (2022) POSA283 Differential Appraisal of Functional Outcome measures by Health Technology Assessment (HTA) agencies when reviewing therapies for Rare muscular, skeletal and neurodegenerative disorders. Value in Health 25:S175
Terwee CB, Peipert JD, Chapman R et al (2021) Minimal important change (MIC): a conceptual clarification and systematic review of MIC estimates of PROMIS measures. Qual Life Res 30:2729–2754
Health Measures (2022) PROMIS - Measure Development & Research. https://www.healthmeasures.net/explore-measurement-systems/promis/measure-development-research Accessed 11 May 2023
Jensen RE, Potosky AL, Reeve BB et al (2015) Validation of the PROMIS physical function measures in a diverse US population-based cohort of cancer patients. Qual Life Res 24:2333–2344
Paz SH, Spritzer KL, Morales LS et al (2013) Age-related Differential Item Functioning for the Patient-Reported Outcomes Information System (PROMIS®) Physical Functioning Items. Prim Health Care 3
Health Measures (2022) PROMIS - Available Translations. https://www.healthmeasures.net/explore-measurement-systems/promis/intro-to-promis/available-translations Accessed 11 May 2023
Toscano A, Van der Ploeg AT, Berger KI et al (2022) Avalglucosidase Alfa improves symptoms and functioning in late-onset pompe Disease patients vs Alglucosidase Alfa: post-hoc analyses of patient-reported outcomes from COMET Trial. International Society for Pharmacoeconomics and Outcomes Research (ISPOR)-EU, Vienna, Austria
Nagaraja V, Mara C, Khanna PP et al (2018) Establishing clinical severity for PROMIS(®) measures in adult patients with rheumatic diseases. Qual Life Res 27:755–764
Copay AG, Subach BR, Glassman SD et al (2007) Understanding the minimum clinically important difference: a review of concepts and methods. Spine J 7:541–546
Knox SA, King MT (2009) Validation and calibration of the SF-36 health transition question against an external criterion of clinical change in health status. Qual Life Res 18:637–645
Norman GR, Stratford P, Regehr G (1997) Methodological problems in the retrospective computation of responsiveness to change: the lesson of Cronbach. J Clin Epidemiol 50:869–879
Acknowledgements
Professional medical writing support was provided by Dr. Michel D. Wissing, Certara.
Funding
This study was funded by Amicus Therapeutics.
Author information
Authors and Affiliations
Contributions
SiS, SR, and IK contributed to study conceptualization. SR and NH contributed to methodology. AK and HJ contributed to data curation and formal analysis. PK, AH, NH, SR, ShSD, IK, JC, and SiS contributed to data interpretation. NH wrote the first draft of the manuscript; all authors participated in writing, review, and editing of the manuscript. All authors had final responsibility for the decision to submit this manuscript for publication and have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study used data from the PROPEL phase 3 study. PROPEL was designed and monitored in accordance with the ethical principles of Good Clinical Practice guidelines and the Declaration of Helsinki. The clinical study protocol was reviewed and approved by the appropriate independent ethics committee or institutional review board at each study site. All participants provided written informed consent before participating in the study.
Consent for publication
Not applicable.
Competing interests
SiS, IK, JC, and ShSD are employees of and hold stock in Amicus Therapeutics. SR is a former employee of Amicus Therapeutics. NH, AK, and HJ are employees of Certara; Certara is a paid consultant to Amicus Therapeutics. PK has received research/grant support from Amicus Therapeutics and Sanofi Genzyme; has received consulting fees and honoraria from Amicus Therapeutics, Sanofi Genzyme, Maze Therapeutics, Bayer and Asklepios Biopharmaceutical, Inc. (AskBio); is a member of the Pompe and Gaucher Disease Registry Advisory Board for Sanofi Genzyme, Pompe Disease Advisory Board for Amicus Therapeutics, and Advisory Board for Baebies; has equity with Maze Therapeutics and has held equity in Asklepios Biopharmaceuticals, and may receive milestone payments related to that equity in the future. AH received honorariums for consulting activities from Sanofi-Aventis, Amicus, and Avrobio, and grants for research projects from Sanofi-Aventis.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1:
Supplementary data
Supplementary Material 2:
Plain language summary
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kishnani, P.S., Shohet, S., Raza, S. et al. Validation of the Patient-Reported Outcomes Measurement Information System (PROMIS®) physical function questionnaire in late-onset Pompe disease using PROPEL phase 3 data. J Patient Rep Outcomes 8, 13 (2024). https://doi.org/10.1186/s41687-024-00686-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41687-024-00686-z