Abstract
Background
Pediatric asthma has been identified by regulators, clinicians, clinical trial sponsors, and caregivers as an area in need of novel fit-for-purpose clinical outcome assessments (COAs) developed in accordance with the U.S. Food and Drug Administration’s (FDA’s) regulatory guidance for evaluating clinical benefit in treatment trials. To address this gap, the Patient-Reported Outcome (PRO) Consortium’s Pediatric Asthma Working Group has continued development of 2 COAs to assess asthma signs and symptoms in pediatric asthma clinical trials to support efficacy endpoints: a PRO measure, the Pediatric Asthma Diary—Child (PAD-C) for children 8–11 years old (y.o.) and an observer-reported outcome measure, the Pediatric Asthma Diary-Observer (PAD—O) for caregivers of children 4–11 y.o. This qualitative research aimed to generate evidence regarding the content validity of the PAD-C and PAD-O.
Methods
Semi-structured combined concept elicitation and cognitive interviews were conducted with a diverse sample of U.S. participants (15 children 8–11 y.o. and 30 caregivers of children 4–11 y.o.). All children had clinician-diagnosed mild to severe asthma. Interviews explored the experience of pediatric asthma and assessed the understanding and relevance of both measures. Interviews were conducted across 3 iterative rounds to allow for modifications.
Results
Concept elicitation findings demonstrated that the core sign/symptom and impact concepts assessed in the PAD-C (cough, hard to breathe, out of breath, wheezing, chest tightness, and nighttime awakenings/symptoms) and PAD-O (cough, difficulty breathing, short of breath, wheezing, and nighttime awakenings/signs) correspond to those most frequently reported by participants; concept saturation was achieved. All PAD-C and PAD-O instructions and core items were well understood and considered relevant by most participants. Feedback from participants, the Pediatric Asthma Working Group, advisory panel, and FDA supported modifications to the measures, including addition of 1 new item to both measures and removal of 1 caregiver item.
Conclusions
Findings provide strong support for the content validity of both measures. The cross-sectional measurement properties of both measures and their user experience and feasibility in electronic format will be assessed in a future quantitative pilot study with qualitative exit interviews, intended to support the reliability, construct validity, final content, and, ultimately, FDA qualification of the measures.
Plain English summary
Pediatric asthma is one of the most common chronic diseases in children. However, there are problems of underdiagnosis, poor disease management, and undertreatment for many pediatric asthma patients, pressuring healthcare systems worldwide. Evaluating asthma symptoms is an important part of the development of treatments for pediatric asthma. However, there are few clinical outcome assessments (COAs) developed in line with regulatory guidance to directly assess symptom severity and evaluate the benefit of new treatments in children with asthma. In this study, we continued the development of the Pediatric Asthma Diary—Child (PAD-C) and the Pediatric Asthma Diary—Observer (PAD-O), according to regulatory guidance, to assess asthma signs and symptoms in children 4 through 11 years old and address this unmet need. The study aimed to explore the experience of pediatric asthma and assess how well-understood and relevant the measures are. Three rounds of qualitative interviews were conducted with 15 children 8 through 11 years old and 30 caregivers of children 4 through 11 years old with asthma. Results show that both measures are well-understood and assess the relevant and important aspects of pediatric asthma reported by children and caregivers. Findings provide evidence supporting the PAD-C and PAD-O as measures of symptom severity and their future use in pediatric asthma treatment trials. Further research is underway to evaluate their measurement properties and assess the user experience and feasibility of electronic completion, to ultimately support the PAD-C and PAD-O in an ongoing COA qualification process by the United States Food and Drug Administration.
Similar content being viewed by others
Background
As a chronic inflammatory disease of the airways, pediatric asthma is characterized by recurrent episodes of shortness of breath, wheeze, chest tightness, and cough. These episodes are typically associated with expiratory airflow limitation that may resolve spontaneously or in response to medication [1]. Pediatric asthma is recognized as the most common chronic disease in children [2, 3]; however, prevalence is increasing globally and issues of underdiagnosis, poor disease management, and undertreatment continue to persist [4]. As a result, pediatric asthma remains a critical area of unmet need and poses a substantial global burden on healthcare systems [5].
International guidelines issued by the Global Initiative for Asthma (GINA) state that the long-term goals of asthma management are to achieve good symptom control and to minimize future risk of exacerbations, persistent airflow limitation, and side effects of treatment [1]. The achievement of good symptom control necessitates the assessment of asthma symptoms; however, there are poor correlations between objective measures of asthma severity typically used in clinical trials (e.g., forced expiratory volume in 1 s and peak expiratory flow) and patients’ self-reported experience [6,7,8]. The assessment of asthma symptoms is a critical component in the development of treatments for pediatric asthma and to ease the burden on children and their families. Therefore, to ensure the patient perspective of asthma is accurately represented and assessed in clinical research, there is a need for novel clinical outcome assessments (COAs) to directly assess symptom severity and evaluate clinical benefit in pediatric asthma populations [9, 10].
Symptoms of asthma are most appropriately assessed using patient-reported outcome (PRO) measures, since only persons with asthma can feel and self-report on many symptoms. However, as young children (i.e., ≤ 7 years old [y.o.]) may not be able to reliably self-report symptom experience, pediatric asthma trials can involve the collection of PRO data from older children (i.e., ≥ 8 y.o.) on asthma symptoms and observer-reported outcome (ObsRO) data from parents/caregivers on observable asthma-related signs for younger children [9]. Although recent efforts to develop COAs in pediatric asthma exist [11], there is still a lack of fit-for-purpose COAs developed in accordance with United States (U.S.) Food and Drug Administration’s (FDA’s) evidentiary expectations for evaluating clinical benefit in pediatric asthma clinical trials [12]. During previous interactions between FDA and the PRO Consortium’s Asthma Working Group during qualification of the Asthma Daytime Symptom Diary (ADSD) and the Asthma Nighttime Symptom Diary (ANSD) for adolescent and adult populations [13, 14], FDA feedback noted the measurement gap in pediatric populations and requested the development of novel COAs to assess asthma symptoms in a broader range of asthma patients (i.e., < 12 y.o.) in clinical studies.
To address this, Merck Sharpe & Dohme Corporation, a member of Critical Path Institute’s (C-Path’s) PRO Consortium [15], contributed draft versions of 2 COAs for use in pediatric asthma clinical trials to assess the signs and symptoms of mild to severe persistent asthma: a PRO measure designed for completion by children 8–11 y.o. (originally named the Child Asthma Diary [CAD]); and an ObsRO measure designed for completion by parents/caregivers of children 4–11 y.o. (originally named the Observer Asthma Diary [OAD]) [16]. Initial development of the measures was informed by multiple stages of qualitative research, including a targeted literature review, input by expert scientific advisors, 3 phases of concept elicitation interviews, and 2 phases of cognitive interviews with the respective target populations. However, initial FDA feedback to Merck raised concerns regarding adequacy of the evidence for the content validity of the CAD and OAD in the planned context of use. As a result, the PRO Consortium’s Pediatric Asthma Working Group embarked on further development of the CAD and OAD, with the intention of submitting for COA qualification by FDA for the assessment of asthma sign and symptom severity in children with asthma (i.e., < 12 y.o.) in pediatric asthma clinical trials [17]. A reanalysis of Merck’s original qualitative data collected as part of the initial development of the draft CAD and OAD was conducted to address FDA’s feedback. Based on this reanalysis of the original data, the draft CAD and OAD were subsequently modified and renamed the Pediatric Asthma Diary—Child (PAD-C) and Pediatric Asthma Diary—Observer (PAD-O), respectively. FDA accepted the PAD-C and PAD-O into the Drug Development Tool (DDT) COA Qualification Program on June 13, 2017. FDA input has therefore been sought at key points throughout the development and qualification process [17] and has been outlined throughout this article where applicable.
The PAD-C and PAD-O are intended to be used to derive co-primary or secondary endpoints in pediatric asthma clinical trials to establish clinical benefit and support product-specific labeling claims. This article summarizes the qualitative research conducted to continue the development of the PAD-C and PAD-O and to generate qualitative evidence supporting their content validity in accordance with FDA regulatory guidance [10, 18, 19].
Methods
Study design
Figure 1 provides an overview of the qualitative research conducted to support the development of the PAD-C and PAD-O.
At key points throughout the process, input was obtained from the Pediatric Asthma Working Group, C-Path scientists, the advisory panel (J.K, J.H, A.E, T.W), and FDA’s Qualification Review Team. A translatability assessment was conducted on the measures following each round of interviews to ensure that any modifications to the wording used would be suitable for future translation into other languages.
Initial draft PAD-C and PAD-O
A number of changes occurred to the CAD and OAD to create the modified PAD-C and PAD-O. Prior to the study reported here, the PRO Consortium’s Pediatric Asthma Working Group and Adelphi Values made additional refinements to the PAD-C and PAD-O ahead of inclusion and testing in the qualitative interviews. Changes included rearranging and streamlining the PAD-C and PAD-O training guides and simplifying the terminology used in the instructions and item wording of each measure. This section describes the initial draft PAD-C and PAD-O tested in the Round 1 concept elicitation and cognitive interviews.
The PAD-C and PAD-O are designed to be completed twice daily and include a Morning Diary (completed once daily upon waking up to start the day) to assess nighttime awakenings and nighttime asthma symptom severity and a Bedtime Diary / Evening Diary (completed once daily before going to bed) to assess daytime symptom severity. Both measures include a Training Guide that all participants must read prior to completing the PAD-C or PAD-O to aid understanding of the diaries.
The draft PAD-C (7-item Morning Diary and 12-item Bedtime Diary) has been developed for use in children with asthma 8–11 y.o. to assess self-reported asthma symptom severity. The draft PAD-O (9-item Morning Diary and 12-item Evening Diary) has been developed for use in caregivers of children with asthma 4–11 y.o. to assess caregiver-reported asthma sign/symptom severity. When completing the PAD-O, the caregiver can also consider input from other informants (e.g., the child, siblings, teachers, babysitters, and spouses/partners) regarding observable asthma signs and symptoms.
The PAD-C Bedtime Diary assesses the severity of 5 core asthma symptoms (cough, hard to breathe, out of breath, wheezing, and chest tightness) and the PAD-O Evening Diary assesses the severity of 4 core observable asthma signs and symptoms (cough, difficulty breathing, shortness of breath, and wheezing). Note that chest tightness was not included within the PAD-O as it was found to not be an observable concept that can be reliably reported by caregivers in the previous qualitative research [16]. Due to difficulty with feasibility of children or caregivers reporting on the severity of individual symptoms during the night, a global assessment of nighttime asthma symptom or sign severity is included within the PAD-C Morning Diary and PAD-O Morning Diary, respectively. The morning diaries also assess presence of nighttime awakenings, which is considered a clinically relevant marker for asthma control and symptom severity [1]. The asthma sign and symptom concepts included within the PAD-C and PAD-O are assessed in terms of presence (nighttime awakenings), intensity (cough, nighttime asthma symptom severity), or frequency (cough, difficulty breathing, shortness of breath, wheezing, and chest tightness [PAD-C only]), to provide an assessment of sign and symptom severity which is widely recognized as needed to demonstrate clinical benefit in pediatric asthma treatment trials.
Additional items included in the PAD-C and PAD-O to assess other asthma-relevant measurement concepts are: difficulty falling asleep (Morning Diary), activity limitations (Bedtime Diary / Evening Diary), and rescue medication use for both rescue inhalers and nebulizers (Morning Diary and Bedtime Diary / Evening Diary). Single items designed to assess global daytime asthma symptom severity are included in the Bedtime Diary / Evening Diary only, to support analyses during measure development. In the PAD-O, items are included to capture the sources of information used by caregivers when responding to items for informational purposes only, in addition to 1 item added at FDA’s request assessing whether caregivers check on their child during the night (Morning Diary only).
Items in the PAD-C are answered using a 4- or 5-level verbal rating scales (VRS) with text descriptors for each response option paired with colored boxes of increased shading, or via “Yes/No” response options. Items in the PAD-O are answered using a 5- or 6-level VRS, or via “Yes/No/I don’t know” response options. Number entry fields are also used for the rescue inhaler and nebulizer items in both measures.
Concept elicitation and cognitive interviews
Combined semi-structured concept elicitation and cognitive interviews were conducted across 3 iterative rounds to evaluate modifications made to the PAD-C and PAD-O.
Recruitment
Forty-five participants were targeted for inclusion in the interviews, including 15 children 8–11 y.o., 15 parents/caregivers of children 4–7 y.o., and 15 parents/caregivers of children 8–11 y.o. These subgroups allowed for development and testing of the PAD-C and PAD-O in narrower age groupings to help account for developmental differences in children [9, 20]. Participants were recruited from 5 different U.S. locations (Chicago, IL; Baltimore, MD; New Orleans, LA; Pittsburgh, PA; St. Louis, MO) with the assistance of a third-party recruitment agency via referral by general practitioners, pediatricians, and respiratory specialists. Child participants were required to be 8–11 y.o., have a clinician-confirmed diagnosis of asthma as defined by national or international asthma guidelines (i.e., GINA [1], National Asthma Education and Prevention Program [NAEPP] [21]) for at least 1 year, have received/filled a prescription for asthma medication in the last year, and have experienced symptoms of asthma in the 3 weeks prior to screening. Caregivers were required to be at least 18 years of age and a parent/caregiver of a child 4–11 y.o. with a clinician-confirmed diagnosis of pediatric asthma, who had received/filled a prescription for asthma medication in the last year and had experienced signs or symptoms of asthma in the 3 weeks prior to screening.
Participants were excluded if they (or their child if a caregiver) had a diagnosis of a condition other than asthma (not including allergies or rhinitis) that affected lung function (e.g., bronchiectasis, chronic sinusitis, cystic fibrosis) or any other significant condition that would impact ability to take part in the study.
Recruitment quotas for the following characteristics were used to ensure a sociodemographically and clinically diverse sample reflective of respondents typically enrolled in pediatric asthma clinical trials: age, sex, ethnicity, race, time since diagnosis, asthma control (i.e., well-controlled and not well-controlled [22]), exacerbations, and medication use.
Interview procedure
The research was conducted in accordance with the Declaration of Helsinki and ethical approval and oversight were provided by Copernicus Group Independent Review Board (CGIRB), an independent ethical review board in the U.S. (IRB number: 20200606). All data were handled in accordance with Health Insurance Portability and Accountability Act (HIPAA) guidelines and the European General Data Protection Regulation (GDPR) for the security and privacy of health data.
All participants provided written informed consent (or parental permission and participant assent in the case of participants 8–11 y.o.) before their participation in the study. Semi-structured interviews lasting approximately 60 min were conducted by trained qualitative researchers via Microsoft Teams or by telephone. All interviews were audio recorded and transcribed verbatim.
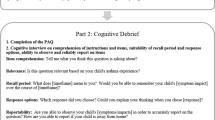
In each round, interviews included an introduction (5 min), concept elicitation (5 min), and cognitive interview (50 min) sections. A brief concept elicitation component was included at the start of the interview, to explore the experience of pediatric asthma and evaluate whether the PAD-C and PAD-O adequately assess the core symptoms reported by participants. Since comprehensive concept elicitation work was completed by Merck during initial development activities, this section was deliberately brief to allocate more time to the cognitive evaluation of the PAD-C and PAD-O. Following concept elicitation, participants were asked to complete a paper version of the PAD-C (children) or PAD-O (caregivers) using a “think aloud” method to vocalize their thoughts as they read each instruction and completed each item. In-depth cognitive interview questions were then used to explore the relevance and understanding of the diary items, instructions, response scales, and recall periods.
Analysis
A qualitative analysis plan was developed a priori to define the coding process, subgroup analyses, and presentation of results. All interview data were analyzed using qualitative analysis methods and ATLAS.ti software [23].
Concept saturation, defined as the point at which no new relevant or important information emerges with the collection of more data [10], was evaluated to ensure that the concepts elicited by participants during the concept elicitation portion of the interview had been fully explored. Saturation analyses were conducted for the child and caregiver samples separately by dividing participants into 3 equal groups according to the chronological order in which they were interviewed. Saturation was said to be achieved if no new concepts emerged within the final group of interviews (i.e., Round 3 interviews).
Results
Sample characteristics
A total of 45 participants were included across 3 rounds of interviews. Fifteen interviews were conducted with children 8–11 y.o. and 30 interviews were conducted with caregivers of children 4–11 y.o. All children had clinician-diagnosed mild to severe asthma.
Table 1 summarizes the sociodemographic and clinical characteristics of children participating or being represented by a caregiver in the qualitative interviews. Sociodemographic characteristics of caregivers are presented in Additional file 1: Table 1. Overall, the majority of pre-specified recruitment quotas were met or only narrowly missed, and there was good representation of characteristics in both child and caregiver samples for each age group.
Concept elicitation results
The symptoms most frequently reported by children during the concept elicitation section of the interviews correspond to the 5 core symptom concepts assessed in the PAD-C Bedtime Diary; cough, difficulty breathing, and chest tightness were reported by all child participants (n = 15/15, 100%), and shortness of breath and wheezing were reported by almost all (n = 14/15, 93.3%; see Table 2). These symptoms were elicited in each round of interviews and equally across both levels of asthma control (well-controlled and not well-controlled).
Similarly, the signs and symptoms most frequently reported by caregivers during the concept elicitation section of the interviews correspond to the 4 observable signs and symptoms assessed in the PAD-O Evening Diary; cough, difficulty breathing, and wheezing were reported by all caregivers (n = 30/30, 100%), and shortness of breath was reported by most (n = 28/30, 93.3%; see Table 2). Children and caregivers also reported other asthma symptoms including general congestion (n = 3 caregivers), tiredness (n = 3 caregivers), flushed face (n = 2 caregivers), and nasal congestion (n = 2 children).
Children and caregivers discussed how asthma impacted their/their child’s daily life. Impacts on physical activity (n = 15/15 children, 100%; n = 30/30 caregivers, 100%) and sleep (n = 15/15 children, 100%; n = 29/30 caregivers, 96.7%) were reported most frequently by children and caregivers, both of which are assessed by items in the PAD-C and PAD-O. Impacts on social functioning (n = 7/15 children, 46.7%; n = 11/30 caregivers, 36.7%), emotional wellbeing (n = 5/15 children, 33.3%; n = 12/30 caregivers, 40.0%), and school (n = 3/15 children, 20.0%; n = 1/30 caregiver, 3.3%; see Table 2) were also reported by children and caregivers. In terms of asthma treatments, all children (n = 15/15, 100%) and all but 1 caregiver (n = 29/30, 96.7%) reported the use of a rescue inhaler. Nebulizer use (n = 8/15 children, 53.3%; n = 20/30 caregivers, 66.7%) and maintenance inhaler use (n = 5/15 children, 33.3%; n = 18/30 caregivers, 60.0%) were also reported.
Concept saturation was achieved after the first 2 rounds of child interviews, by which point the majority of signs/symptoms and impact domains had been elicited. This included the core symptom concepts assessed by the PAD-C (cough, difficulty breathing, shortness of breath, wheezing, and chest tightness) and PAD-O (cough, difficulty breathing, shortness of breath, and wheezing), as well as impacts on physical activity and sleep (Additional file 1: Tables 2 and 3, respectively). Note that, nighttime awakenings were spontaneously reported for the first time in the final round of child interviews; however, nighttime awakenings were reported by 13 additional children when probed across the 3 rounds, supporting relevance of the concept to this patient population.
Cognitive interview results for the PAD-C and PAD-O
For the cognitive interviews, the Pediatric Asthma Working Group and Adelphi Values divided each of the measures into core, supplementary, and developmental items. “Core items” assess the severity of key signs, symptoms, and impacts of pediatric asthma intended for inclusion in scoring of the measure. “Supplementary items” assess other optional asthma-relevant concepts intended to supplement the measures when used in clinical trials, and “developmental items” are intended for testing purposes during development of the measures. A distinct sample of 15 participants took part in each round of cognitive interviews; 5 children completed the PAD-C and 10 caregivers completed the PAD-O in each round. Across all 3 rounds of cognitive interviews, PAD-C and PAD-O instructions and items were generally well understood and considered relevant. See Additional file 1: Figs. 1, 2, 3, 4, 5, 6, 7 and 8—for an overview of understanding and relevance across the 3 rounds of child and caregiver interviews.
The 3 iterative rounds of cognitive interviews supported refinement of the PAD-C and PAD-O, with revisions to the instructions and items implemented after each round, as summarized in Table 3 (PAD-C) and Table 4 (PAD-O). Modifications made were based on feedback from participants, the Pediatric Asthma Working Group, C-Path scientists, the advisory panel, FDA scientists, and the translatability assessments. Updates were generally applied across both measures where applicable, with the aim of promoting consistency and comprehensiveness.
Round 1
The majority of instructions and items in the PAD-C and the PAD-O were well understood, and all core items were considered relevant by most participants. Recall period instructions for the Morning Diary and Bedtime Diary / Evening Diary were understood by most children and caregivers asked. Based on interview findings, several modifications were made to the PAD-C and PAD-O training guides and overall measures, including updates to the instructions, item wording, and response options.
Round 2
The PAD-C and PAD-O instructions and response options were understood by most participants, and all core items were understood and relevant to the majority of participants. Almost all children and caregivers understood the recall period instructions in the Morning Diary and Bedtime Diary / Evening Diary. Despite these results, further modifications were made to the PAD-C and PAD-O training guides and overall measures, including updates to the instructions (to allow for both single and multiple-observer completion [PAD-O only]), item wording, and response options.
Round 3
No changes were suggested to the PAD-C and PAD-O core items as all items and response scales were well understood and relevant to the majority of participants. Additional sections in the PAD-O Training Guide relating to single and multiple-observer completion were generally well understood, and half of the caregiver sample (n = 5/10, 50.0%) indicated that they would share completion of the PAD-O with another caregiver (e.g., another parent or grandparent), supporting retention of multiple-observer instructions. Some further modifications were made to the PAD-C and PAD-O training guides and overall measures following Round 3 interviews, including minor updates to the recall period wording within the instructions, item wording, and response scales.
Item finalization
Following completion of the 3 rounds of cognitive interviews, an item finalization meeting was held with the Pediatric Asthma Working Group to discuss findings and confirm the proposed revisions to the PAD-C and PAD-O. The evidence demonstrated that both measures provided sufficient conceptual coverage of the core symptoms in pediatric asthma, and therefore it was agreed that no additional items should be added. All items tested in the Round 3 interviews were retained for both measures, except for 1 caregiver developmental item in the Morning Diary. The revisions made were reviewed and approved by the advisory panel. Following cognitive interviews, the resulting PAD-C consisted of 8 core items, 12 supplementary items, and 1 developmental item (Fig. 2); whereas the PAD-O consisted of 7 core items, 12 supplementary items, and 2 developmental items (Fig. 3).
PAD-C draft conceptual framework. *Cough currently includes 2 items: cough frequency and cough intensity. Note: “Core Items” are intended for inclusion in the PAD-C scoring algorithm. “Supplementary Items” assess other optional asthma-relevant concepts intended to supplement the PAD-C when used in clinical trials. These items would be scored separately from the PAD-C. “Developmental Items” are intended for testing during PAD-C development.
PAD-O draft conceptual framework. *Cough currently includes 2 items: cough frequency and cough intensity. Note: “Core Items” are intended for inclusion in the PAD-O scoring algorithm. “Supplementary Items” assess other optional asthma-relevant concepts intended to supplement the PAD-O when used in clinical trials. These items would be scored separately from the PAD-O. “Developmental Items” are intended for testing during PAD-O development
Conceptual frameworks
The draft conceptual frameworks for the PAD-C and PAD-O following the 3 rounds of interviews are presented in Figs. 2 and 3, respectively. These conceptual frameworks will be finalized after the completion of a planned quantitative pilot study with qualitative exit interviews.
Discussion
Pediatric asthma has been identified by regulators and other relevant stakeholders as an area in need of novel fit-for-purpose COAs for evaluating clinical benefit in pediatric asthma treatment trials. In order to address this unmet measurement need, the PAD-C and PAD-O were accepted into FDA’s DDT COA Qualification Program [24]. The overall objective of this study was to generate qualitative evidence that the content of these measures effectively assesses the severity of the core signs and symptoms of asthma, achieved via the conduct of combined concept elicitation and cognitive interviews.
Concept elicitation
Concept elicitation findings demonstrated that the core symptom concepts assessed in the current versions of the PAD-C and PAD-O were most frequently reported by participants, providing evidence that these measures assess the most important and relevant signs and symptoms of pediatric asthma. The most frequently reported domains of impacts on daily life were physical activity and sleep impacts (including difficulty falling asleep and nighttime awakenings), both of which are assessed by items in the PAD-C and PAD-O and are considered clinically relevant concepts directly linked to asthma symptoms. The evidence confirms that no core sign or symptom concepts were missing from the PAD-C or PAD-O and the addition of further items is not needed. The findings further substantiate existing literature highlighting the widespread and considerable impact of pediatric asthma and reinforces the need for effective treatments to achieve symptom control and accurate assessments of symptom severity [5, 13, 25].
Cognitive interviews for the PAD-C and PAD-O
Across the 3 rounds of cognitive interviews, instructions and core items in the PAD-C and PAD-O were well understood and considered relevant by most participants, providing qualitative evidence to support their content validity. The iterative rounds of interviews strengthened the measures, with revisions to the instructions and items implemented and tested after each round. Several modifications were made following Round 1 interviews, including updates to item stems, response options, rescue inhaler and/or nebulizer item wording, and the addition of a new item to determine whether a child has a nebulizer for asthma treatment. Following Round 2 interviews, further updates were made to response options including updates to the cough intensity response scale on both the PAD-C and PAD-O, rescue inhaler and/or nebulizer item wording, and additional instructions were added to the PAD-O to allow for single and multiple-observer completion. Findings from Round 3 interviews supported additional changes to the rescue inhaler and/or nebulizer item wording to enhance understanding, and the item assessing whether caregivers check on their child was removed as shown in Table 4. This resulted in the current versions of the PAD-C and PAD-O at the time of publication.
Since the initiation of this research in 2016, a new electronic Pediatric Asthma Symptom Diary (ePASD) has been developed for self-completion by children 6–11 y.o., in an attempt to address the existing measurement gap in this population [11]. However, there are notable advantages of the PAD-C and PAD-O over the ePASD and other existing measures. First, the development of both a PRO measure (the PAD-C for completion by children 8–11 y.o.) and ObsRO measure (the PAD-O for completion by caregivers of children 4–11 y.o.) allows for the assessment of asthma signs and symptoms across a broader range of children with mild to severe asthma, specifically those younger than 6 y.o. Evidence from the qualitative interviews and existing literature demonstrates the importance of assessing symptom severity in children as young as 4 y.o. [1, 26], particularly as this often reflects populations included in pediatric asthma clinical trials. As such, there is a critical need for appropriate COAs with adequate evidence of being fit-for-purpose to assess asthma symptom severity in younger age groups, not purely self-reports by older children. Second, there is mixed evidence regarding the age at which a child can independently and reliably self-report, with some doubts around the appropriateness of administering PRO measures to children below the age of 8 y.o. [20, 27, 28]. The PAD-O was developed to avoid these potential issues in younger age groups, as caregivers are more likely to be optimal reporters of observable asthma signs and medication use for children under 8 y.o. [16]. The PAD-O also offers the unique ability for both single and multiple-observer completion, an addition that was supported by FDA representatives to account for a range of different caregiver and/or living situations that better reflect modern family life and allow for greater inclusivity in future pediatric asthma clinical trials. Finally, an important strength of the PAD-C and PAD-O is the pursuit of qualification as part of FDA’s DDT COA Qualification Program. Qualification ensures both measures have been developed and tested in accordance with FDA expectations and relevant guidance [10, 18, 19], including input from a diverse sample of children and caregivers from the target population with varying sociodemographic (e.g., age, sex, ethnicity, and race) and clinical characteristics (e.g., levels of asthma control, exacerbations, and medication use). This is in addition to involvement from a multidisciplinary team, COA experts, comprising representatives from 2 pharmaceutical firms, C-Path, specialist clinicians involved in the diagnosis and management of children with asthma, patient advocates, and FDA representatives.
Study limitations
Although there was good representation of different sociodemographic and clinical characteristics in the sample, some target quotas were missed. Most notably this included children on medication Step 5 and male caregivers, although, this is likely a reflection of fewer cases of more severe asthma in children and the lack of established Step 5 treatment for children 4–5 y.o. [1], and the well-documented sex differences in research participation [29, 30] and childcare responsibilities [31, 32]. Interviews were also conducted with U.S. participants only; however, the cross-cultural suitability of the PAD-C and PAD-O was explored within the translatability assessments, and full translation and cultural adaptation of the measures for other languages will be conducted in future studies.
Additionally, interviews with children 8–11 y.o. were conducted via video call or telephone. Face-to-face interviews were initially proposed as the optimal methodology to build rapport and obtain useful insights from non-verbal cues; however, this was not feasible due to the COVID-19 pandemic and associated public health restrictions when interviews were conducted between October 2020 and July 2021. Nevertheless, research has shown comparability between face-to-face and video or telephone interviews [33, 34], and additional steps were taken to mitigate against potential issues with remote interviewing (i.e., color-coding the measures) and to promote engagement throughout the child interviews (i.e., using visual aids and creative tasks).
Conclusion
The results from this qualitative study provide strong support for the content validity of the PAD-C and PAD-O for assessing severity of asthma signs and symptoms in children 4 through 11 y.o. with mild to severe pediatric asthma. The next steps in the development process include the migration of the measures to an electronic mode of data collection and the conduct of a quantitative pilot study with qualitative exit interviews. This continued research will aim to generate further evidence to confirm the cross-sectional measurement properties and evaluate the user experience and feasibility of electronic completion of the PAD-C and PAD-O to support progress towards their qualification in FDA’s COA Qualification Program.
Availability of data and material
The data described in this article are not publicly available in further detail beyond that provided in the manuscript and the extensive supplementary files.
Abbreviations
- ADSD :
-
Asthma Daytime Symptom Diary
- ANSD :
-
Asthma Nighttime Symptom Diary
- CAD:
-
Child Asthma Diary
- CGIRB:
-
Copernicus Group Independent Review Board
- COA:
-
Clinical outcome assessment
- C-Path:
-
Critical Path Institute
- DDT:
-
Drug development tool
- ePASD:
-
Electronic Pediatric Asthma Symptom Diary
- FDA:
-
U.S. Food and Drug Administration
- GDPR:
-
General Data Protection Regulation
- GINA:
-
Global Initiative for Asthma
- HIPAA:
-
Health Insurance Portability and Accountability Act
- HHS:
-
Health and Human Services
- NAEPP:
-
National Asthma Education and Prevention Program
- OAD:
-
Observer Asthma Diary
- ObsRO:
-
Observer-reported outcome
- PAD-C :
-
Pediatric Asthma Diary—Child
- PAD-O :
-
Pediatric Asthma Diary—Observer
- PRO:
-
Patient-reported outcome
- VRS:
-
Verbal rating scale
- U.S.:
-
United States
- y.o.:
-
Years old
References
Global Initiative for Asthma (2021) Global Strategy for Asthma Management and Prevention.
World Health Organization (2021) Asthma. https://www.who.int/news-room/fact-sheets/detail/asthma. Accessed 11 Jan 2022
American Academy of Allergy and Asthma Immunology (2022) Childhood Asthma (Pediatric Asthma) Defined. https://www.aaaai.org/Tools-for-the-Public/Allergy,-Asthma-Immunology-Glossary/Childhood-Asthma-(Pediatric-Asthma)-Defined. Accessed 11 Jan 2022
Serebrisky D, Wiznia A (2019) Pediatric asthma: a global epidemic. Ann Glob Health 85(1):6
Ferrante G, La Grutta S (2018) The burden of pediatric asthma. Front Pediatr 6:186
Teeter JG, Bleecker ER (1998) Relationship between airway obstruction and respiratory symptoms in adult asthmatics. Chest 113(2):272–277
Ståhl E (2000) Correlation between objective measures of airway calibre and clinical symptoms in asthma: a systematic review of clinical studies. Respir Med 94(8):735–741
Davis SQ, Permutt Z, Permutt S, Naureckas ET, Bilderback AL, Rand CS, Stein BD, Krishnan JA (2009) Perception of airflow obstruction in patients hospitalized for acute asthma. Ann Allergy Asthma Immunol 102(6):455–461
Matza LS, Patrick DL, Riley AW, Alexander JJ, Rajmil L, Pleil AM, Bullinger M (2013) Pediatric patient-reported outcome instruments for research to support medical product labeling: report of the ISPOR PRO good research practices for the assessment of children and adolescents task force. Value Health 16(4):461–479
US Department of Health and Human Services Food and Drug Administration (2009) Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims.
Clark M, Romano C, Olayinka-Amao O, Whalley D, Crawford R, Pathak P, Brindicci C, Garg K, Kordy K, Everhard F (2022) Development and content validation of a self-completed, electronic Pediatric Asthma Symptom Diary. J Patient-Rep Outcomes 6(1):1–13
US Department of Health and Human Services Food and Drug Administration (2022) Patient-focused drug development: selecting, developing, or modifying fit-for-purpose clinical outcome assessments: guidance for industry, food and drug administration staff, and other stakeholders.
Gater A, Nelsen L, Fleming S, Lundy JJ, Bonner N, Hall R, Marshall C, Staunton H, Krishnan JA, Stoloff S (2016) Assessing asthma symptoms in adolescents and adults: qualitative research supporting development of the asthma daily symptom diary. Value Health 19(4):440–450
Gater A, Nelsen L, Coon CD, Eremenco S, O’Quinn S, Khan AH, Eckert L, Staunton H, Bonner N, Hall R (2022) Asthma daytime symptom diary (ADSD) and asthma nighttime symptom diary (ANSD): measurement properties of novel patient-reported symptom measures. J Allergy Clin Immunol Pract 10(5):1249–1259
Coons S, Kothari S, Monz B, Burke L (2011) The patient-reported outcome (PRO) consortium: filling measurement gaps for PRO end points to support labeling claims. Clin Pharmacol Ther 90(5):743–748
Nelsen L, Currie B, Norquist J, Peter S, Vernon M (2014) Pediatric asthma symptoms: assessments by subjects and caregivers. Value Health 17(3):A179
US Department of Health and Human Services Food and Drug Administration (2020) Qualification process for drug development tools: guidance for industry and FDA staff.
US Department of Health and Human Services Food and Drug Administration (2022) Patient-focused drug development: methods to identify what is important to patients: guidance for industry, food and drug administration staff, and other stakeholders.
US Department of Health and Human Services Food and Drug Administration (2020) Patient-focused drug development: collecting comprehensive and representative input: guidance for industry, food and drug administration staff, and other stakeholders.
Nathan PC, Furlong W, Barr RD (2004) Challenges to the measurement of health-related quality of life in children receiving cancer therapy. Pediatr Blood Cancer 43(3):215–223. https://doi.org/10.1002/pbc.20096
National Asthma Education and Prevention Program (2007) Expert panel report 3 (EPR-3): guidelines for the diagnosis and management of asthma-summary report 2007. J Allergy Clin Immunol 120(5 Suppl):S94–S138
Liu AH, Zeiger R, Sorkness C, Mahr T, Ostrom N, Burgess S, Rosenzweig JC, Manjunath R (2007) Development and cross-sectional validation of the childhood asthma control test. J Allergy Clin Immunol 119(4):817–825
ATLAS.ti.Scientific Software Development GmbH B, Germany (2018) Atlas.ti.software version 8.
US Department of Health and Human Services Food and Drug Administration (2021) Clinical Outcome Assessment (COA) Qualification Program: Frequently Asked Questions. https://www.fda.gov/drugs/clinical-outcome-assessment-coa-qualification-program/clinical-outcome-assessment-coa-qualification-program-frequently-asked-questions#HowCDERPrioritizesSubmissions.
Nunes C, Pereira AM, Morais-Almeida M (2017) Asthma costs and social impact. Asthma Res Pract 3(1):1. https://doi.org/10.1186/s40733-016-0029-3
Centers for Disease Control and Prevention (2018) Asthma in children. https://www.cdc.gov/vitalsigns/childhood-asthma/index.html. 2022
Raat H, Mohangoo AD, Grootenhuis MA (2006) Pediatric health-related quality of life questionnaires in clinical trials. Curr Opin Allergy Clin Immunol 6(3):180–185. https://doi.org/10.1097/01.all.0000225157.67897.c2
Bevans KB, Riley AW, Moon J, Forrest CB (2010) Conceptual and methodological advances in child-reported outcomes measurement. Expert Rev Pharmacoecon Outcomes Res 10(4):385–396. https://doi.org/10.1586/erp.10.52
Armstrong BK, White E, Saracci R (1992) Principles of exposure measurement in epidemiology. Oxford University Press. New York, NY
Patel MX, Doku V, Tennakoon L (2003) Challenges in recruitment of research participants. Adv Psychiatr Treat 9(3):229–238
Hill EM, Hill MA (1990) Gender differences in child care and work: an interdisciplinary perspective. J Behav Econ 19(1):81–101
García-Mainar I, Molina JA, Montuenga VM (2011) Gender differences in childcare: time allocation in five European countries. Fem Econ 17(1):119–150
Mazar I, Lamoureux R, Ojo O, Kevane G, Banderas B, Stokes J, Shields A (2015) Telephone versus face-to-face interviews for patient-reported outcome instrument development. Value Health 18(7):A718
Gray LM, Wong-Wylie G, Rempel GR, Cook K (2020) Expanding qualitative research interviewing strategies: zoom video communications. Qual Rep 25(5):1292–1301
Acknowledgements
Linda Nelsen, an employee of GSK, and Maggie Tabberer, an employee of GSK at the time this research was conducted, provided input and guidance at key stages throughout the research on behalf of the Patient-Reported Outcome Consortium’s Pediatric Asthma Working Group. Maria Mattera, employee of Critical Path Institute and member of the Patient-Reported Outcome Consortium’s Pediatric Asthma Working Group, also provided input at key stages of the research. Asha Lehane, employee at Adelphi Values, contributed to the data analysis and interpretation. Lucy Morgan, employee at Adelphi Values at time of research, contributed to the conception or design of the study, conducted participant interviews and contributed to the data analysis or interpretation. Dr. Jerry Krishnan, a specialist clinician involved in the diagnosis and management of children with asthma, provided expert clinical input at key stages of the research. We thank the members of the U.S. Food and Drug Administration’s Qualification Review Team and other FDA scientists for their feedback during the development of the PAD-C and PAD-O.
Funding
This qualitative study was funded by the U.S. Food and Drug Administration under the Broad Agency Announcement contract 7540119C10135.
Author information
Authors and Affiliations
Consortia
Contributions
RA, RW-H, and HB contributed to the conception or design of the study; contributed to the data analysis or interpretation; and were major contributors in writing and/or revising the manuscript. AJ, AL, and FW contributed to the conception or design of the study; conducted participant interviews; contributed substantially to the data analysis or interpretation; and were major contributors in writing and/or revising the manuscript. SJC, SE, CT, ET, and VHS were major contributors to the conception or design of the study, the data analyses strategy and interpretation, and writing and/or revising the manuscript. JH, AE, and TW provided expert input to the conception or design of the study, as well as the data analyses or interpretation. All authors provided critical review and final approval of the publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval and oversight were provided by Copernicus Group Independent Review Board (CGIRB), an independent ethical review board in the U.S. (IRB tracking number: 20200606). All caregiver participants provided informed consent and parental permission (if applicable), and all child participants provided informed assent before participating in any study activities.
Consent for publication
Dissemination of findings including via publication was included in the consent and parental permission forms signed by caregivers.
Competing interests
Sonya Eremenco and Stephen Joel Coons are employees of Critical Path Institute, which is the copyright holder for the PAD-C and PAD-O on behalf of the PRO Consortium. Rob Arbuckle, Rebecca Williams-Hall, Helena Bradley, Amy Jones, Aoife Lydon, and Frances White are employees of Adelphi Values, a health outcomes agency commissioned to conduct research by companies in the pharmaceuticals industry. Adelphi Values received funding from Critical Path Institute to conduct the research summarized in this article. Claire Trennery was an employee of GSK when the research was completed and is now employed by Adelphi Values. Vivian H Shih was an employee of AstraZeneca when the research was conducted and is now employed by Insmed. Erin Tomaszewski is an employee of AstraZeneca. Dr. John Haughney was a consultant of Adelphi Values on behalf of Critical Path Institute as a scientific advisor and received a fee for his involvement. Amanda Eisen and Tonya Winders were consultants of Adelphi Values on behalf of Critical Path Institute as patient advocacy/caregiver representatives and received a fee for their involvement. Tonya Winders is a paid speaker and advisor to AstraZeneca, Amgen, GSK, Sanofi/Regeneron and Novartis. The authors declare that there are no other competing interests. Critical Path Institute is supported by the Food and Drug Administration (FDA) of the Department of Health and Human Services (HHS) and is 55% funded by the FDA/HHS, totaling $17,612,250, and 45% funded by non-government source(s), totaling $14,203,111. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement by, FDA/HHS or the U.S. Government.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Supplementary materials including tables and figures.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bradley, H., Trennery, C., Jones, A.M. et al. Assessing asthma symptoms in children: qualitative research supporting the development of the Pediatric Asthma Diary—Child (PAD-C) and Pediatric Asthma Diary—Observer (PAD-O). J Patient Rep Outcomes 7, 104 (2023). https://doi.org/10.1186/s41687-023-00639-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41687-023-00639-y