Abstract
Background
No available studies demonstrate validity and meaningful change thresholds of Work Productivity and Activity Impairment (WPAI) questionnaire in patients with migraine. In this post-hoc analysis, we assessed reliability, validity, responsiveness, and meaningful within-patient change from baseline to Month 3 for Work Productivity and Activity Impairment (WPAI) domain scores in patients with episodic migraine (EM) or chronic migraine (CM).
Method
The Phase 3, multicenter, randomized, double-blind, placebo-controlled CONQUER study (NCT03559257, N = 462) enrolled patients with EM or CM who failed two to four categories of prior preventive medication in past ten years. The analyses were performed for WPAI domain scores (absenteeism, presenteeism, overall work productivity, and non-work-related activity impairment). Migraine Specific Quality of Life Questionnaire version 2.1 (MSQv2.1) domain scores (Role Function-Restrictive [RFR] and Role Function-Preventive [RFP]), and monthly migraine headache days were used as anchors. Responder criteria were changes from baseline to Month 3 for each of these anchors and were defined as: increase in MSQ-RFR by ≥ 25.71 points and MSQ-RFP by ≥ 20.00 points and a 50% reduction in monthly migraine headache days. Assessments were performed for overall population, and patients with EM or CM. The meaningful change threshold was determined based on Youden index, Phi coefficient and sensitivity.
Results
Of 462 randomized patients, 444 who completed WPAI questionnaire were included in post-hoc analysis. Test–retest reliability over 3 months in a stable subgroup revealed moderate correlations for non-work-related Activity Impairment (ICC = 0.446) presenteeism (ICC = 0.438) and a fair correlation for overall work productivity loss (ICC = 0.360). At baseline, all correlations between WPAI domain scores and continuous anchor variables exceeded recommended threshold of ≥ 0.30, except for WPAI domain scores with number of monthly migraine headache days. Patients achieving pre-specified responsiveness thresholds for monthly migraine headache days, and MSQ-RFP, MSQ-RFR from baseline to Month 3 (responders) showed significant improvements in WPAI domain scores compared with non-responders (P < 0.001). The meaningful change thresholds of -20 (% unit) were identified for WPAI domain scores.
Conclusion
In conclusion, WPAI has sufficient validity, reliability, responsiveness, and appropriate interpretation standards to assess the impact of EM or CM on presenteeism and overall work productivity loss and non-work-related activity impairment.
Trial registration
NCT number of CONQUER study, NCT03559257.
Similar content being viewed by others
Introduction
The global prevalence of migraine varies among studies, a recent update provides a summary estimate of 14% and shows a prevalence peak in mid-life [1,2,3,4,5]. A review addressing the impact of episodic migraine (EM) and chronic migraine (CM) on employment absenteeism and presenteeism indicated that patients with migraine lost an average of 4.4 working days and experienced reduced work productivity for an additional 11.4 days annually [6]. A reduction in work productivity has implications for people with migraine, families, employers, and society.
A recent global survey, “My Migraine Voice”, evaluated the social and economic impact of migraine in patients with ≥ 4 monthly migraine days who were receiving preventive treatment for EM or CM [7]. The findings of the survey indicated that an increase in number of migraine preventive treatment failures was associated with increased rates of absenteeism (work hours missed from total work hours), presenteeism (degree of productivity affected while working), work productivity (overall work productivity affected), and non-activity-related activity impairment (degree of productivity affected in regular unpaid activity) as measured by the Work Productivity and Activity Impairment (WPAI) instrument [7]. These cross-sectional results from “My Migraine Voice” most likely reflect confounding by indication, that is, patients with more severe disease are more likely to receive treatment.
Guidelines for clinical trials of migraine treatments recommend the use of Patient Reported Outcome (PRO) measures [8, 9]. Specifically, Guidelines of the International Headache Society (IHS) for controlled trials of preventive treatment of EM and CM suggest measuring the mean change from baseline in the WPAI questionnaire [8, 9]. The WPAI is a PRO measure that assesses the impact of health problems on work-related productivity and non-work-related activity impairment over the past 7 days [10, 11]. Meaningful change (improvement) thresholds for the WPAI may be useful for clinical interpretation of the impact of a disease on patients’ ability to work [12]. The reliability, validity, and responsiveness of WPAI in patients across various disease areas have been previously reported [13,14,15,16,17]. Additionally, content validity of WPAI is also established in previous publications and it is recommended by IHS [9, 18, 19]. Qualitative research has confirmed the conceptual importance of work productivity for people with migraine, and several real-world and population-based studies have utilized the WPAI questionnaire to assess the impact of migraine on work productivity [20,21,22,23,24,25,26,27,28]. However, to the best of our knowledge, there is no report determining the validity and meaningful change of WPAI in patients with migraine.
Recently, the CONQUER study demonstrated the efficacy and safety of galcanezumab versus placebo in patients with EM or CM who had previously failed to benefit from or tolerate two to four standard-of-care categories of migraine preventive medications [29]. Significantly greater reductions (p < 0·0001) in monthly migraine-headache days averaged across Months 1 to 3 were reported in patients treated with galcanezumab versus placebo. Furthermore, reduction in WPAI domain scores from baseline were significantly greater (p ≤ 0.0004) in the galcanezumab group compared with placebo [30]. In this post-hoc analysis of the CONQUER study, we aim to assess the reliability, validity, responsiveness, and meaningful within-patient change from baseline to Month 3 for the WPAI domain scores in patients with EM or CM.
Methods
Study design and patient population
CONQUER (NCT03559257, N = 462) was a Phase 3, multicenter, randomized, double-blind, placebo-controlled study. The details on the study design and patient population have been previously published [29]. In brief, patients meeting the International Classification of Headache Disorders, third edition (ICHD-3) [31, 32] criteria for EM or CM and who failed two to four categories of prior preventive medications in the past ten years due to lack of efficacy (after at least two months at maximum tolerated dose) or safety and tolerability reasons or both were included. Patients were required to have four or more monthly migraine-headache days and one or more monthly headache-free days on average during the three months prior to screening. Eligible patients were randomly assigned (1:1) to monthly subcutaneous injections of either galcanezumab 120 mg (loading dose 240 mg) or placebo administered by subcutaneous injection once monthly over 3-month double-blind phase. All patients received galcanezumab 120 mg during 3-month open-label phase. The study protocol was approved by the Institutional Review Board, Medical Ethics Committee, or Medical Research and Ethics Committee of the participating study sites. The study was conducted in concordance with the Declaration of Helsinki guidelines. All patients provided written informed consent before participation in CONQUER trial.
Subgroup analyses were conducted based on EM and CM status as defined in the clinical trial protocol based on the baseline monthly migraine-headache days. CM was defined as ≥ 8 migraine headache days, with ≥ 15 headache days (migraine or nonmigraine). EM was defined as not meeting the criteria for CM and having at least 4 migraine headache days.
Secondary objectives of the CONQUER study, among others, were to compare galcanezumab with placebo on changes in disability and quality of life using PRO measures. The objectives of this post-hoc analyses were to assess the reliability, validity, responsiveness and determine meaningful within-patient change thresholds for the WPAI domain scores.
Study measures
The WPAI-Specific Health Problem version 2 is a six-item questionnaire, with a recall period of past seven days. The WPAI questionnaire was collected at the baseline and at the Month 3 visit during double-blind period to assess past one week WPAI score. The instrument includes questions on employment status, hours missed from work due to the specific health problem (i.e. migraine), hours missed from work for other reasons, hours worked, the degree that migraine affected productivity while working, and the degree that migraine affected other daily activities [33]. Based on the responses to the six items, four scores for absenteeism, presenteeism, overall work productivity, and non-work-related activity impairment were derived as indicated in the Statistical Analysis section. The percentages were calculated as amount of time lost in each domain divided by the amount of time in each domain.
Details on calculation of WPAI scores are provided in Additional file 1. All WPAI scores were presented as percentage units across this paper.
The Migraine Specific Quality of Life Questionnaire version 2.1 (MSQv2.1) is a self-administered disease specific quality of life questionnaire [34]. The recall period for MSQ is the past 4 weeks. The MSQ score data was collected at baseline and month 3 visit during double-blind phase. The instrument consists of 14 items that assess 3 domains: (1) Role Function-Restrictive (RFR); (2) Role Function-Preventive (RFP); and (3) Emotional Function. This study focused only on MSQ RFR and RFP domains. The MSQ domain scores range from 0 (worst functional health status) to 100 (best functional health status). Increasing scores indicate improvements in quality of life [35].
Patients enrolled in the study used an electronic daily diary to record headache features and use of acute headache medications throughout the study. The number of monthly migraine headache days (per 30-day period) was the primary measure in the CONQUER study. A migraine headache day was defined as a calendar day on which a migraine or probable migraine occurred. Migraine was defined as a headache, with or without aura, of ≥ 30 min duration with both of the following required features (A and B):
-
A.
At least 2 of the following headache characteristics: unilateral location, pulsating quality, moderate or severe pain intensity, aggravation by or causing avoidance of routine physical activity, AND
-
B.
During headache at least one of the following: nausea and/or vomiting, photophobia and phonophobia (definition adapted from IHS ICHD-3). Probable migraine headache was defined as a headache of ≥ 30 min duration, with or without aura, but missing one of the migraine features in the IHS ICHD-3 definition [32].
In calculating the number of migraine headache days for each period, if the period was not equal to 30 days, the number of migraine headache days was adjusted by multiplying the number of migraine headache days by (30/x) where ‘x’ was the total number of non-missing diary days in the period assuming that the proportion of days with migraine is the same for days with missing and non-missing electronic patient-reported outcomes (ePRO). If more than half ePRO diary days are missing, monthly migraine headache days for that 1-month period were considered missing. Additional patient-reported data were recorded directly by the patient on an electronic tablet at the time of clinic visits.
MSQ-RFR, MSQ-RFP, and monthly migraine headache days were selected as independent anchors for this study. We have not included the Patient Global Impression of Severity (PGI-S) and Migraine Disability Assessment (MIDAS) as anchors because of lower Youden index observed in the analysis for both anchors, (Youden index < 0.25) and bimodal trends in the Youden index plots. Established responder criteria consisted of changes from baseline to Month 3 for each of these anchors, and were defined as: an improvement in MSQ-RFR by ≥ 25.71 points, an improvement in MSQ-RFP by ≥ 20.00 points [36], a 50% reduction in monthly migraine headache days.[37], while the non-responder were defined as: a < 25.71 points improvement or stay the same or worsening on MSQ-RFR score, a < 20 improvement or stay the same or worsening on the MSQ-RFP score [33], a < 50% reduction in monthly migraine headache days [9, 34, 38]. Patients who did not meet the responder criteria were defined as non-responders for each of the anchors. Responder and non-responder status was separately defined for each anchor.
Statistical analysis
A statistical analysis plan was developed prior to the execution of this post-hoc analysis. In this post-hoc analysis, reliability, validity, responsiveness (ability to detect change), and meaningful within-patient change in WPAI score were assessed before the use of the 3 anchor-based responder definitions indicated above. WPAI absenteeism, presenteeism, overall work productivity, and non-work-related activity impairment scores are calculated from the responses of the 6 items of the WPAI (employment status, hours missed from work due to migraine, hours missed from work for other reasons, hours actually worked, degree migraine affected productivity while working and degree migraine affected productivity in regular unpaid activities) as impairment percentages [33]. Higher numbers indicate greater impairment and less productivity (i.e., worse outcomes). Calculations are completed for individuals who responded that they were employed (Additional file 1). WPAI scores were presented as percentage. Assessments were performed for the overall population, and patients with EM or CM. Descriptive statistics (including mean, standard deviation, and floor and ceiling effects) were used to determine the distribution of scores for WPAI. As the scores and changes from baseline to Month 3 for WPAI absenteeism, and correlations between WPAI absenteeism and selected anchor of monthly migraine headache days were very low in the patient population, it was determined during the initial stage of this analysis that it was not appropriate to evaluate responsiveness for this measure alone (i.e. without accounting for presenteeism). Therefore, the analyses were performed for three WPAI domain scores- presenteeism, overall work productivity loss (absenteeism plus presenteeism), and non-work-related activity impairment using the selected anchors (MSQ-RFR, MSQ-RFP, and monthly migraine headache days).
The methods for anchor selection included evaluating Spearman’s correlation analyses to test hypotheses about relationships between outcome variables at baseline (overall, and EM/CM subpopulations). Correlations between outcomes were determined using the non-parametric Spearman’s rank correlation coefficient (Rho) because the data is not assumed to be normally distributed. Multiple outcomes were evaluated, and heat maps were created by plotting Spearman’s Rank Correlation Coefficients (Rho) between these outcomes and the WPAI. Absolute value of Rho > 0.90 to ≤ 1.00 indicated very high correlation, ≥ 0.70 to ≤ 0.90 indicated high correlation, ≥ 0.60 to < 0.70 indicated moderate high correlation, ≥ 0.50 to < 0.6 indicated moderate correlation, ≥ 0.40 to < 0.50 indicated moderate low correlation, ≥ 0.30 to < 0.40 indicated low correlation, and 0.00 to ≤ 0.30 indicated negligible correlation. These methods resulted in the selected anchors, as the other outcomes had weaker associations and were not suitable anchors, such as the MSQ Emotional Domain [39, 40].
Reliability
Test–retest reliability was assessed in a population considered to be stable. This group received placebo and had a change of one day or less in their number of migraine-headache days per month. WPAI domain scores at baseline and Months 3 were used to assess test–retest reliability. Intra-class correlation coefficients (ICC) were calculated using the two-level random-intercept-only mixed model [41].
where \(y_{ij}\) is the WPAI score for subject i and time j; the random intercepts \(\mu_{0j}\) have variance \({\upsigma }_{u0}^{2}\) and the residuals \(e_{ij}\) have variance \({\upsigma }_{e}^{2}\). The ICC is the ratio of the random intercept variance to the total variance\(:\)
The ICC values were classified as: 0.01 to 0.20 (slightly fair), 0.21 to 0.40 (fair), 0.41 to 0.60 (moderate), 0.61 to 0.80 (substantial), and 0.81 to 1.00 (almost perfect agreement) [42].
Validity
Construct validity of WPAI domain scores with MSQ-RFR, MSQ-RFP, and monthly migraine-headache days was assessed using Spearman’s correlation analyses at baseline. The Spearman’s rank correlation coefficient measures the strength and direction of association between two variables using a non-parametric correlation statistic with values ranging from -1 to + 1. We defined seven levels of correlation between outcomes based on the absolute values of Rho: 0.70–1.00 (high), 0.60–0.70 (moderate high), 0.50–0.60 (moderate), 0.40–0.50 (moderate low), 0.30–0.40 (low), 0.20–0.30 (negligible), and 0–0.20 (negligible-low).
Responsiveness
Anchor-based responder analyses were performed to assess the ability to detect change in WPAI domain scores by responder status for each of the three anchors (MSQ-RFR, MSQ-RFP, and monthly migraine-headache days). The least square mean changes from baseline to Month 3 for WPAI for both responders and non-responders for each of the anchor variables was estimated and compared. Statistically significant differences (p < 0.05) in change in WPAI domain scores between responders and non-responders of anchor variables indicated responsiveness or ability to detect change in the WPAI domain scores.
Analysis of covariance (ANCOVA) models were utilized to examine differences in the change in WPAI domain scores from baseline to Month 3 among patients in all the anchor-based responder groups; the assessment evaluates the past 7-days at both time points. The change in WPAI presenteeism, overall productivity loss, and non-work-related activity impairment was the dependent variable, while the responder group variable was included as the independent variable in the model. Baseline WPAI presenteeism, overall productivity loss, and non-work-related activity impairment was adjusted for the respective models.
Meaningful within-patient change thresholds
Anchor-based analyses were used to determine the meaningful within-patient change in WPAI domain scores. Monthly migraine headache days decreased by 50%, MSQ-RFR scores decreased by ≥ 25.71 points and MSQ-RFP scores decreased by ≤ 20 points were selected as anchors.
WPAI change score threshold was estimated by logistic regression with the selected anchor as a dependent variable and change from baseline WPAI score as an independent variable. Discriminative ability between the responder and non-responder groups were assessed using receiver-operator characteristic (ROC) curves, Youden index (YI), Phi correlations, and Concordance (C) statistics, which is the equivalent of the area-under-curve (AUC) of a ROC curve.
The YI, a frequently used summary measure in ROC analyses, measures the effectiveness of a predictive marker, and enables selection of an optimal threshold value for that marker. The YI was calculated at each level of improvement in the WPAI (c): [YI (c) = sensitivity (c) + (specificity (c) −1)]. Its value ranges from 0 through 1; higher value indicates better discriminative ability between the responders and non-responders. The optimal cut-score is identified as the point at which YI is maximal in the ROC analysis [43]. A threshold of change from baseline WPAI score was chosen so that YI was high for all anchor variables. The phi coefficient is a measure of association for two binary variables, and it was calculated at each level of improvement in the WPAI. The AUC has values that range from 0.5 to 1.0. AUC values closer to 0.5 indicated that the accuracy of model at predicting outcome is based on chance. Values from 0.7 to 0.8 indicate a good model. Values of 0.8 to 0.9 indicate excellent discrimination, and ≥ 0.9 show outstanding discrimination between responder and non-responder groups [44]. Empirical cumulative distribution function (eCDF) plots were generated to display the change scores from baseline to Month 3 by anchor responder groups and to provide supporting evidence for the optimal threshold. All analyses were conducted based on a 2-sided significance level of 0.05 and using SAS software Version 9.4 (SAS institute, Cary, NC).
Results
Baseline demographic and disease characteristics
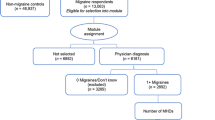
A total of 462 patients were randomized and received at least one dose of the study drug in the CONQUER study; 444 patients who completed the WPAI questionnaire for non-work-related activity impairment were included in post-hoc analyses (EM, n = 261; CM, n = 183). Of the 444 patients, overall work productivity loss data were collected from 315 patients with employment (complete data: 289; missing data: 26). Presenteeism data were collected for 315 patients (completed data: 284; missing data: 31). This analysis used complete data for measurements of WPAI at both baseline and month 3.
Baseline demographics and disease characteristics are presented in Table 1. For the overall population providing data on the WPAI, mean (SD) age was 45.9 (11.81) years, and the majority of patients (n = 381, 85.8%) were female. The WPAI absenteeism, presenteeism, overall work productivity loss, and non-work-related activity impairment scores presented as mean (SD) were 9.37 (17.85), 42.75 (23.24), 46.86 (25.69), and 50.97 (23.91), respectively. Baseline demographics and disease characteristics of employed patients were similar to those of overall patients (Table 2).
Reliability
Test–retest reliability results, estimated in stable patients treated with placebo, showed moderate correlations for WPAI presenteeism (ICC: all patients = 0.438; EM patients = 0.227; CM patients = 0.893) and WPAI non-work-related Activity Impairment (ICC: all patients = 0.446; EM patients = 0.272; CM patients = 0.653) and a fair correlation for WPAI overall work productivity loss (ICC: all patients = 0.360; EM patients = 0.158; CM patients = 0.885) [42].
Validity
At baseline, all the correlations between WPAI domain scores and continuous anchor variables exceeded the recommended threshold of ≥ 0.30, except for WPAI domain scores with the number of monthly migraine headache days in the overall population, and in patients with EM or CM. In patients with EM, the correlation between WPAI non-work-related activity impairment and MSQ-RFR was moderate-to-high (−0.606, Additional file 2: Figure S1).
Responsiveness
WPAI domain scores improved (decreased) from baseline to Month 3 (Additional file 2: Table S1). Overall, patients achieving the pre-specified responsiveness thresholds for the monthly migraine headache days, and MSQ-RFP, MSQ-RFR from baseline to Month 3 (responders) showed significant improvements in WPAI domain scores compared with non-responders (P < 0.001, Table 3). Similar results were reported in patients with EM and CM (non-responders vs non-responders, P < 0.05) (Additional file 2: Table S2A and Table S2B).
Meaningful within-patient change thresholds
The AUC for change in WPAI domain scores ranged from 0.7 to 0.8 for all the selected anchor groups, indicating “acceptable” ability of the model to differentiate between responder and non-responder groups (Additional file 2: Table S4).
In the overall population, an optimum meaningful change in WPAI domain scores (% unit) from baseline to Month 3 corresponding to maximum YI of all three anchors was −20.0 for presenteeism, −22.2 to −19.4 for overall work productivity loss and −30.0 to −10.0 for non-work-related activity impairment (Fig. 1). In patients with EM, optimum meaningful change was −40.0 to −20.0 for presenteeism and −22.2 to −19.3 for overall work productivity loss and −40.0 to −30.0 for non-work-related activity impairment (Fig. 2). In patients with CM, optimum meaningful change was −20.0 for presenteeism and −23.0 to −19.8 for overall work productivity loss and −20.0 to −10.0 for non-work-related activity impairment (Fig. 3).
Youden’s index for WPAI domain scores improvement at Month 3 for selected anchors (Overall population). WPAI scores are presented as % unit. Abbreviations: MHD monthly migraine headache days, MSQ Migraine-Specific Quality of Life questionnaire, RFP Role Function-Preventive, RFR Role Function-Restrictive, WPAI Work Productivity and Activity Impairment questionnaire, YI Youden index
Youden’s index for WPAI domain scores improvement at Month 3 for selected anchors (EM). WPAI scores are presented as % unit. Abbreviations: EM episodic migraine, MHD monthly migraine headache days, MSQ Migraine-Specific Quality of Life questionnaire, RFP Role Function-Preventive, RFR Role Function-Restrictive, WPAI Work Productivity and Activity Impairment questionnaire, YI Youden index
Youden’s index for WPAI domain scores improvement at Month 3 for selected anchors (CM). WPAI scores are presented as % unit. CM chronic migraine, MHD monthly migraine headache days, MSQ Migraine-Specific Quality of Life questionnaire, RFP role function-preventive, RFR role function-restrictive, WPAI Work Productivity and Activity Impairment questionnaire, YI Youden index
For the overall population, Phi coefficient was ≥ 0.24 and sensitivity ranged from 0.4 to 0.8 (Table 4). YI was the highest for cut-off points of approximately -20 unit-change from baseline in WPAI (% unit) for the anchor groups, Table 3. In patients with EM, a similar trend was followed only for WPAI presenteeism and WPAI overall work productivity loss domains (Additional file 2: Table S3A). In patients with CM, results for YI were comparable to that for overall population (Additional file 2: Table S3B). The meaningful change threshold of −20 (% unit) was chosen based on the overlapping data on Youden index, Phi coefficient and sensitivity.
The eCDF plots showed a clear separation between the curves representing anchor responder and non-responder groups by WPAI change scores (Additional file 2: Figure S2).
Using the established meaningful change threshold of −20 (% unit) for WPAI, the percentage of patients from the non-responder anchor group (no change/worsening) that were mis-classified as experiencing meaningful improvement in WPAI were between 22.2 and 37.3% for overall population, 25.7% to 44.7% for EM and 16.3% to 27.9% for CM, respectively.
Discussion
This post-hoc analyses of the CONQUER study demonstrated the reliability, validity, responsiveness, and meaningful change of the WPAI questionnaire in patients with EM or CM. These results support the validity of the WPAI as a PRO to measure the impact of EM or CM on work productivity (overall and presenteeism) and non-work-related activity impairment. The meaningful change thresholds for the WPAI domain scores may help in evaluating clinically meaningful treatment responses and may be appropriate for inclusion of WPAI in future preventive migraine clinical studies.
Test–retest reliability results showed moderate correlations for WPAI presenteeism and WPAI non-work-related activity impairment and a fair correlation for WPAI overall work productivity loss. The modest ICCs for the WPAI may reflect the relatively brief, one-week recall interval. As the number of migraine days and their severity is known to vary within person from time to time, the instability of the phenomenon being measured may contribute to modest ICCs. This may also account for the higher ICCs we observed for CM than for EM. The greater ICCs among patients with CM than patients with EM may be due to the small sample size or the shorter recall period. A longer recall period longer for patients with EM may provide a more stable measurement of reliability.
Construct validity was confirmed between WPAI domain scores and continuous anchor variables- monthly migraine headache days, MSQ-RFR, and MSQ-RFP. Using an anchor-based method, a threshold of -20-unit change in scores at Month 3 (from baseline) was found to be meaningful for the three WPAI domain scores. The identified responder thresholds were consistent across patients with EM or CM. The eCDF plots substantiated the findings of the selected meaningful change threshold. A meaningful within-patient responder threshold was defined for three of the WPAI domains (presenteeism, overall work productivity, and non-work-related activity impairment) for patients with migraine (EM or CM).
The reliability, validity, responsiveness, and meaningful change of the WPAI among patients with migraine had not been previously established. The findings of this research indicate that this instrument is appropriate for use in this population and provides a within-patient responder threshold that can be used to determine a meaningful change in presenteeism, overall work productivity and non-work-related activity impairment. This threshold can be used in future research to determine the proportion of patients that are experiencing a degree of improvement that is impactful for work and non-work activities.
In the present analyses, WPAI absenteeism sub scores alone (i.e. without accounting for presenteeism) were not considered due to a possible lack of sensitivity in patients with migraine. This may be explained by a low mean baseline score of 9.37 and smaller change from baseline of −2.83 for absenteeism versus other domains making the results less sensitive to the present analyses. These low mean absenteeism scores are not unexpected, as qualitative research has revealed that employed patients with migraine frequently ‘power-through’ work, which results in modest levels of absenteeism. When people miss enough work, they may become unemployed. Across a range of chronic pain disorders unemployment rates increase with pain severity and in the highest grades of pain unemployment rates reach 20%. Selecting for persons who are employed may in effect select against individuals with high rates of absenteeism. Presenteeism is strongly influenced by migraine [28, 33, 45]. Similar findings have been observed in a prior study, where patients with migraine were more likely to miss non-work activities (family, social, and leisure) than work [46]. Prior work has addressed the psychometric properties of the WPAI for other disease states using similar methods to the those used in the present report. This research also used anchor-based and distribution-based methods and utilized clinical trial data. However, unlike the current research, the previous research determined apriori to not estimate thresholds for absenteeism and presenteeism separately, classifying these as individual domains that should be used for descriptive purposes only [47]. Another study also used clinical trial data to evaluate the change in all four WPAI domain scores among patients with ankylosing spondylitis. However, the research evaluated WPAI responsiveness using minimum clinically important differences from two other PROs, which were quantified with standardized response mean (SRM) calculations [48]. Although, all WPAI domain scores were evaluated in patients with ankylosing spondylitis, absenteeism domains was observed to be less sensitive for identifying meaningful changes [48], similar to the present study.
Strengths of this study include the use of current methods for evaluating psychometric properties, determining meaningful within-patient change thresholds, and the PROs for the analyses were comprehensive including a quality-of-life measure and an electronic daily diary measure of MHDs.
There are certain limitations to our study. One of the limitations is that the patient population for the CONQUER clinical trial was specific to patients with migraine who had a history of two to four preventive treatment category failures. In addition, analyses were limited to people with ≥ 4 monthly migraine headache days, which may represent a more impacted sample than the general population. This higher rate of monthly migraine days may have influenced employment status and associated disability, and therefore results may not be generalizable to a sample with fewer monthly migraine days. Moderate reliability or greater was not observed for the WPAI in this patient population, perhaps because the number of headache days varies from week to week and the recall interval for the WPAI is only one week. This study included WPAI data at baseline and Month 3, hence we could not include Month 1 data for analysis. Also, there was no information from the patient perspective regarding what constitutes an important change in WPAI scores. The analysis plan evaluated reliability in a group with no change or a change of only one day over one month when the WPAI evaluated one week of that month; real within person change may have reduced the ICCs for the WPAI. Responsiveness for WPAI absenteeism was not evaluated because of very low score in the patient population. Additionally, the MSQ-RFR and MSQ-RFP as anchors used in the study to validate WPAI should be easy to interpret. Change from baseline is monthly migraine days is a widely used, included in labelling, and recommended in guidelines as a primary endpoint in preventive treatment trials [9, 38]. MSQ-RFP is a recommended secondary endpoint and is included in labelling for migraine medications [49, 50]. In addition to the lack of temporal alignment to the MHD measure used to define no change and the WPAI, the one-week recall interval itself may have had reduced ICCs because of actual variation from week to week in presenteeism and non-work-related activity impairment. Increasing the recall interval reduces temporal sampling error but may result in recall bias. Reilly et al. reported that WPAI score may be unduly influenced by the most severe disease day in that interval and suggested that use of recall period as short as 24 h may be warranted to reduce recall bias [14]. Daily measures over longer periods mitigate both temporal sampling error and recall bias but substantially increase participant burden and may induce fatigue. For a disorder such as migraine, characterized by attacks, reliability may be improved with longer sampling intervals or by averaging multiple 7-day sampling intervals.
There is uncertainty if these results can be generalized to the overall migraine population. However, results observed in patients with EM or CM were consistent. Therefore, the identified responder thresholds can be applied to migraine populations without preventive treatment failures until further research is completed to confirm (or contradict) this recommendation. Prior publications show that patients with high frequency EM (10–14 headache days/month) have similar disability to those of CM (≥ 15 headache days/month) [51, 52]. On the other hand, Ishii et al., in their study comparing chronic versus episodic migraine concluded that patients with chronic migraine (15–23 headache days/month) have significantly greater disability compared to patients with high-frequency episodic migraine (8–14 headache days/month) (median [interquartile range] MIDAS score: 55 [30–90] vs. 38 [20–58], p < 0.001) [53]. Considering patients with low frequency EM were not included in the current analysis, it is not known if responder data of patients with low frequency EM would be comparable to those with low frequency CM or not. Future efforts may compare the meaningful change thresholds from this study with other studies with a less restrictive migraine population, and an evaluation of the meaningfulness of the change via patient input would be informative. Previous studies have used 50% threshold for monthly migraine headache days in patients with CM [12], which was confirmed by in post-hoc analysis of a preventive anti-CGRP treatment for CM [54]. Data on the proportion of patients achieving the responder threshold for galcanezumab versus placebo may be considered in a future publication.
Conclusions
The results of this study demonstrated the validity of the WPAI PRO to measure the impact of EM or CM on work productivity (overall and presenteeism) and non-work-related activity impairment. The meaningful change thresholds for the WPAI domain scores may help in evaluating clinically meaningful treatment responses and may be appropriate for inclusion of WPAI in future preventive migraine clinical studies. The analysis was specific to a population with a history of multiple standard-of-care migraine preventive medication failures and moderate frequency EM or greater; however, the meaningful within-patient threshold may be applied to migraine research studies until generalizability of these findings are confirmed.
Availability of data and materials
Eli Lilly and Company provides access to all individual participant data collected during the trial, after anonymization except for pharmacokinetic or genetic data. Data are available to request six months after the indication studied has been approved in the United States and European Union and after primary publication acceptance, whichever is later. No expiration date of data requests is currently set once data are made available. Access is provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data sharing agreement. Data and documents, including the study protocol, statistical analysis plan, clinical study report, blank or annotated case report forms, will be provided in a secure data sharing environment. For details on submitting a request, see the instructions provided at www.vivli.org.
Abbreviations
- ANOVA:
-
Analysis of variance
- AUC:
-
Area under the curve
- CM:
-
Chronic migraine
- C:
-
Concordance
- eCDF:
-
Empirical cumulative distribution function
- EM:
-
Episodic migraine
- ICCs:
-
Intra-class correlation coefficients
- ICHD-3:
-
International Classification of Headache Disorders
- MSQ:
-
Migraine-Specific Quality of Life questionnaire
- N:
-
Number of patients
- n:
-
Number of patients in a subgroup
- WPAI_ova:
-
Overall work productivity loss
- PRO:
-
Patient-reported outcome
- ROC:
-
Receiver-operator characteristic
- RFP:
-
Role function preventive
- RFR:
-
Role function restrictive
- SD:
-
Standard deviation
- SE:
-
Standard error
- SRM:
-
Standardized response means
- WPAI:
-
Work Productivity and Activity Impairment
- WPAI_act:
-
WPAI non-work-related activity impairment
- WPAI_pres:
-
WPAI presenteeism
- YI:
-
Youden index
References
Victor TW, Hu X, Campbell JC, Buse DC, Lipton RB (2010) Migraine prevalence by age and sex in the United States: a life-span study. Cephalalgia 30(9):1065–1072. https://doi.org/10.1177/0333102409355601
Steiner TJ, Stovner LJ, Katsarava Z, Lainez JM, Lampl C, Lantéri-Minet M, Rastenyte D, Ruiz de la Torre E, Tassorelli C, Barré J, Andrée C (2014) The impact of headache in Europe: principal results of the Eurolight project. J Headache Pain 15(1):31. https://doi.org/10.1186/1129-2377-15-31
Diener HC, Ashina M, Durand-Zaleski I, Kurth T, Lantéri-Minet M, Lipton RB, Ollendorf DA, Pozo-Rosich P, Tassorelli C, Terwindt G (2021) Health technology assessment for the acute and preventive treatment of migraine: a position statement of the International Headache Society. 41(3):279–293. doi:https://doi.org/10.1177/0333102421989247
Woldeamanuel YW, Cowan RP (2017) Migraine affects 1 in 10 people worldwide featuring recent rise: a systematic review and meta-analysis of community-based studies involving 6 million participants. J Neurol Sci 372:307–315. https://doi.org/10.1016/j.jns.2016.11.071
Stovner LJ, Hagen K, Linde M, Steiner TJ (2022) The global prevalence of headache: an update, with analysis of the influences of methodological factors on prevalence estimates. J Headache Pain 23(1):34. https://doi.org/10.1186/s10194-022-01402-2
Leonardi M, Raggi A (2019) A narrative review on the burden of migraine: when the burden is the impact on people’s life. J Headache Pain 20(1):41. https://doi.org/10.1186/s10194-019-0993-0
Gibbs SN, Shah S, Deshpande CG, Bensink ME, Broder MS, Dumas PK, Buse DC, Vo P, Schwedt TJ (2020) United States patients’ perspective of living with migraine: country-specific results from the global “My Migraine Voice” survey. Headache 60(7):1351–1364. https://doi.org/10.1111/head.13829
Tassorelli C, Diener HC, Dodick DW, Silberstein SD, Lipton RB, Ashina M, Becker WJ, Ferrari MD, Goadsby PJ, Pozo-Rosich P, Wang SJ (2018) Guidelines of the International Headache Society for controlled trials of preventive treatment of chronic migraine in adults. Cephalalgia 38(5):815–832. https://doi.org/10.1177/0333102418758283
Diener HC, Tassorelli C, Dodick DW, Silberstein SD, Lipton RB, Ashina M, Becker WJ, Ferrari MD, Goadsby PJ, Pozo-Rosich P, Wang SJ, Houle TT, Hoek T, Martinelli D, Terwindt GM (2020) Guidelines of the International Headache Society for controlled trials of preventive treatment of migraine attacks in episodic migraine in adults. Cephalalgia 40(10):1026–1044. https://doi.org/10.1177/0333102420941839
Yarlas A, Maher SM, Bayliss MS, Lovley A, Cappelleri JC, DiBonaventura MD (2018) Psychometric validation of the work productivity and activity impairment questionnaire in ulcerative colitis: results from a systematic literature review. J Patient Rep Outcomes 2(1):62. doi:https://doi.org/10.1186/s41687-018-0088-8
Ford J, Nichols RM, Ye W, Tockhorn-Heidenreich A, Cotton S, Jackson J (2021) Patient-reported outcomes for migraine in the US and Europe: burden associated with multiple preventive treatment failures. Clinicoecon Outcomes Res 13:647–660. https://doi.org/10.2147/CEOR.S304158
Houts CR, Wirth RJ, McGinley JS, Cady R, Lipton RB (2020) Determining thresholds for meaningful change for the Headache Impact Test (HIT-6) total and item-specific scores in chronic migraine. Headache 60(9):2003–2013. https://doi.org/10.1111/head.13946
Bushnell DM, Reilly MC, Galani C, Martin ML, Ricci JF, Patrick DL, McBurney CR (2006) Validation of electronic data capture of the Irritable Bowel Syndrome-Quality of Life Measure, the Work Productivity and Activity Impairment Questionnaire for Irritable Bowel Syndrome and the EuroQol. Value Health 9(2):98–105. https://doi.org/10.1111/j.1524-4733.2006.00087.x
Reilly MC, Bracco A, Ricci JF, Santoro J, Stevens T (2004) The validity and accuracy of the Work Productivity and Activity Impairment questionnaire–irritable bowel syndrome version (WPAI:IBS). Aliment Pharmacol Ther 20(4):459–467. https://doi.org/10.1111/j.1365-2036.2004.02091.x
Wahlqvist P, Carlsson J, Stålhammar NO, Wiklund I (2002) Validity of a work productivity and activity impairment questionnaire for patients with symptoms of gastro-esophageal reflux disease (WPAI-GERD)–results from a cross-sectional study. Value Health 5(2):106–113. https://doi.org/10.1046/j.1524-4733.2002.52101.x
Reilly MC, Gerlier L, Brabant Y, Brown M (2008) Validity, reliability, and responsiveness of the work productivity and activity impairment questionnaire in Crohn’s disease. Clin Ther 30(2):393–404. https://doi.org/10.1016/j.clinthera.2008.02.016
Vergara M, Montserrat A, Casellas F, Villoria A, Suarez D, Maudsley M, Gallardo O, Ricart E, Calvet X (2011) A new validation of the Spanish Work Productivity and Activity Impairment Questionnaire-Crohn’s disease version. Value Health 14(6):859–861. https://doi.org/10.1016/j.jval.2011.02.1179
Lambert J, Hansen BB, Arnould B, Grataloup G, Guillemin I, Højbjerre L, Strandberg-Larsen M, Reilly MC (2014) Linguistic validation into 20 languages and content validity of the rheumatoid arthritis-specific Work Productivity and Activity Impairment questionnaire. Patient 7(2):171–176. https://doi.org/10.1007/s40271-014-0053-4
Leggett S, van der Zee-Neuen A, Boonen A, Beaton D, Bojinca M, Bosworth A, Dadoun S, Fautrel B, Hagel S, Hofstetter C, Lacaille D, Linton D, Mihai C, Petersson IF, Rogers P, Sciré C, Verstappen SM (2016) Content validity of global measures for at-work productivity in patients with rheumatic diseases: an international qualitative study. Rheumatology (Oxford) 55(8):1364–1373. https://doi.org/10.1093/rheumatology/kev435
Wong LP, Alias H, Bhoo-Pathy N, Chung I, Chong YC, Kalra S, Shah ZUBS (2020) Impact of migraine on workplace productivity and monetary loss: a study of employees in banking sector in Malaysia. J Headache Pain 21(1):68. https://doi.org/10.1186/s10194-020-01144-z
Lenz Alcayaga R, Paredes D, Hitschfeld M, Vo P, Quintana R, Carboni V (2019) PND12 work productivity and daily activities impairment (WPAI) in chilean patients with migraine: perspectives on indirect-costs drivers. Value Health Region Issues 19:S61. https://doi.org/10.1016/j.vhri.2019.08.342
Huybrechts KF, Palmsten K, Avorn J, Cohen LS, Holmes LB, Franklin JM, Mogun H, Levin R, Kowal M, Setoguchi S, Hernandez-Diaz S (2014) Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med 370(25):2397–2407. https://doi.org/10.1056/NEJMoa1312828
Lipton RB, Cohen JM, Gandhi SK, Yang R, Yeung PP, Buse DC (2020) Effect of fremanezumab on quality of life and productivity in patients with chronic migraine. Neurology 95(7):e878–e888. https://doi.org/10.1212/wnl.0000000000010000
Lipton RB, Lee L, Saikali NP, Bell J, Cohen JM (2020) Effect of headache-free days on disability, productivity, quality of life, and costs among individuals with migraine. 26(10):1344–1352. https://doi.org/10.18553/jmcp.2020.20103
Blumenfeld AM, Patel AT, Turner IM, Mullin KB, Manack Adams A, Rothrock JF (2020) Patient-reported outcomes from a 1-year, real-world, head-to-head comparison of onabotulinum toxin A and topiramate for headache prevention in adults with chronic migraine. J Prim Care Community Health 11:2150132720959936. https://doi.org/10.1177/2150132720959936
Shimizu T, Sakai F, Miyake H, Sone T, Sato M, Tanabe S, Azuma Y, Dodick DW (2021) Disability, quality of life, productivity impairment and employer costs of migraine in the workplace. J Headache Pain 22(1):29. https://doi.org/10.1186/s10194-021-01243-5
Lipton RB, Nelson AM, Nicholson RA, Zagar A, Kim Y, Pascual J, Evers S, Hirata K, Pearlman EM (2021) Migraine Diagnosis, Disability, and Work Productivity Impact in Migraine: Results of the OVERCOME (International) Study. Available via https://ihs-headache.org/wp-content/uploads/2021/11/P0441_IHS2021_LIPTON__OVERCOME_INTL_BURDEN_MIGRAINE.pdf. Accessed 05 May 2022
Estave PM, Beeghly S, Anderson R, Margol C, Shakir M, George G, Berger A, O’Connell N, Burch R, Haas N, Powers SW, Seng E, Buse DC, Lipton RB, Wells RE (2021) Learning the full impact of migraine through patient voices: a qualitative study. Headache 61(7):1004–1020. https://doi.org/10.1111/head.14151
Mulleners WM, Kim BK, Láinez MJA, Lanteri-Minet M, Pozo-Rosich P, Wang S, Tockhorn-Heidenreich A, Aurora SK, Nichols RM, Yunes-Medina L, Detke HC (2020) Safety and efficacy of galcanezumab in patients for whom previous migraine preventive medication from two to four categories had failed (CONQUER): a multicentre, randomised, double-blind, placebo-controlled, phase 3b trial. Lancet Neurol 19(10):814–825. https://doi.org/10.1016/s1474-4422(20)30279-9
Garcia-Azorin D, Ford J, Buse D, Hand A, Wietecha L, Detke H (2020) Changes in work productivity and interictal burden: results from a randomized, double-blind, placebo-controlled clinical trial evaluating galcanezumab in adults with treatment-resistant migraine (CONQUER) (700). 94(15 Supplement):700
Kimmel MC, Cox E, Schiller C, Gettes E, Meltzer-Brody S (2018) Pharmacologic treatment of perinatal depression. Obstet Gynecol Clin North Am 45(3):419–440. https://doi.org/10.1016/j.ogc.2018.04.007
IHS (2017) The International Classification of Headache Disorders 3rd Edition. Available via https://ichd-3.org/1-migraine/. Accessed 05 May 2022
Reilly MC, Zbrozek AS, Dukes EM (1993) The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics 4(5):353–365. https://doi.org/10.2165/00019053-199304050-00006
Jhingran P, Osterhaus JT, Miller DW, Lee JT, Kirchdoerfer L (1998) Development and validation of the Migraine-Specific Quality of Life Questionnaire. Headache 38(4):295–302. https://doi.org/10.1046/j.1526-4610.1998.3804295.x
Jhingran P, Davis SM, LaVange LM, Miller DW, Helms RW (1998) MSQ: migraine-specific quality-of-life questionnaire. further investigation of the factor structure. PharmacoEconomics 13(6):707–717. https://doi.org/10.2165/00019053-199813060-00007
Speck RM, Yu R, Ford JH, Ayer DW, Bhandari R, Wyrwich KW (2021) Psychometric validation and meaningful within-patient change of the Migraine-Specific Quality of Life questionnaire version 2.1 electronic patient-reported outcome in patients with episodic and chronic migraine. Headache 61(3):511–526. https://doi.org/10.1111/head.14031
Silberstein S, Tfelt-Hansen P, Dodick DW, Limmroth V, Lipton RB, Pascual J, Wang SJ (2008) Guidelines for controlled trials of prophylactic treatment of chronic migraine in adults. Cephalalgia 28(5):484–495. https://doi.org/10.1111/j.1468-2982.2008.01555.x
McGinley JS, Houts CR, Nishida TK, Buse DC, Lipton RB, Goadsby PJ, Dodick DW, Wirth RJ (2021) Systematic review of outcomes and endpoints in preventive migraine clinical trials. Headache 61(2):253–262. https://doi.org/10.1111/head.14069
Cole JC, Lin P, Rupnow MF (2007) Validation of the Migraine-Specific Quality of Life Questionnaire version 2.1 (MSQ v. 2.1) for patients undergoing prophylactic migraine treatment. Qual Life Res 16(7):1231–1237. https://doi.org/10.1007/s11136-007-9217-1
Bagley CL, Rendas-Baum R, Maglinte GA, Yang M, Varon SF, Lee J, Kosinski M (2012) Validating migraine-specific quality of life questionnaire v21 in episodic and chronic migraine. Headache 52(3):409–421. https://doi.org/10.1111/j.1526-4610.2011.01997.x
Deyo RA, Diehr P, Patrick DL (1991) Reproducibility and responsiveness of health status measures: statistics and strategies for evaluation. Control Clin Trials 12(4 Suppl):142s-s158. https://doi.org/10.1016/s0197-2456(05)80019-4
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174
Schisterman EF, Perkins NJ, Liu A, Bondell H (2005) Optimal cut-point and its corresponding Youden Index to discriminate individuals using pooled blood samples. Epidemiology 16(1):73–81. https://doi.org/10.1097/01.ede.0000147512.81966.ba
Forgue ST, Patterson BE, Bedding AW, Payne CD, Phillips DL, Wrishko RE, Mitchell MI (2006) Tadalafil pharmacokinetics in healthy subjects. Br J Clin Pharmacol 61(3):280–288. https://doi.org/10.1111/j.1365-2125.2005.02553.x
Von Korff M, Ormel J, Keefe FJ, Dworkin SF (1992) Grading the severity of chronic pain. Pain 50(2):133–149. https://doi.org/10.1016/0304-3959(92)90154-4
Stewart WF, Lipton RB, Kolodner KB, Sawyer J, Lee C, Liberman JN (2000) Validity of the migraine disability assessment (MIDAS) score in comparison to a diary-based measure in a population sample of migraine sufferers. Pain 88(1):41–52. https://doi.org/10.1016/s0304-3959(00)00305-5
Wu JJ, Lin C, Sun L, Goldblum O, Zbrozek A, Burge R, Augustin M, Feldman SR (2019) Minimal clinically important difference (MCID) for work productivity and activity impairment (WPAI) questionnaire in psoriasis patients. 33(2):318–24. https://doi.org/10.1111/jdv.15098
Qulipta (atogepant) Prescribing Information. Available on https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/215206Orig1s000lbl.pdf. Accessed on 17 Oct 2022
Emgality (galcanezumab) Prescribing Information. Available on https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/761063s004lbl.pdf. Accessed on 17 Oct 2022
Reilly MC, Gooch KL, Wong RL, Kupper H, van der Heijde D (2010) Validity, reliability and responsiveness of the Work Productivity and Activity Impairment Questionnaire in ankylosing spondylitis. Rheumatology 49(4):812–819. https://doi.org/10.1093/rheumatology/kep457
Chalmer MA, Hansen TF, Lebedeva ER, Dodick DW, Lipton RB, Olesen J (2020) Proposed new diagnostic criteria for chronic migraine. Cephalalgia 40(4):399–406. https://doi.org/10.1177/0333102419877171
Torres-Ferrús M, Quintana M, Fernandez-Morales J, Alvarez-Sabin J, Pozo-Rosich P (2017) When does chronic migraine strike? A clinical comparison of migraine according to the headache days suffered per month. Cephalalgia 37(2):104–113. https://doi.org/10.1177/0333102416636055
Ishii R, Schwedt TJ, Dumkrieger G, Lalvani N, Craven A, Goadsby PJ, Lipton RB, Olesen J, Silberstein SD, Burish MJ, Dodick DW (2021) Chronic versus episodic migraine: the 15-day threshold does not adequately reflect substantial differences in disability across the full spectrum of headache frequency. Headache 61(7):992–1003. https://doi.org/10.1111/head.14154
Brandes JL, Diener HC, Dolezil D, Freeman MC, McAllister PJ, Winner P, Klatt J, Cheng S, Zhang F, Wen S, Ritter S, Lenz RA, Miko DD (2020) The spectrum of response to erenumab in patients with chronic migraine and subgroup analysis of patients achieving ≥50%, ≥75%, and 100% response. Cephalalgia 40(1):28–38. https://doi.org/10.1177/0333102419894559
Acknowledgements
The authors would like to thank the investigators for conduct of CONQUER study. The author would also like to thank Rahul Nikam and Karan Sharma, employees of Eli Lilly and Company for providing writing assistance.
Funding
The study was sponsored by Eli Lilly and Company.
Author information
Authors and Affiliations
Contributions
J.H.F., D.W.A., and W.Y. conceived and designed the study. X.M. and W.Y. acquired the data. X.M., W.Y., D.W.A., J.H.F., S.B., D.C.B., and R.B.L. analyzed and interpreted the data. J.H.F., X.M., W.Y., D.W.A., D.C.B., and R.B.L. provided technical direction in the preparation of the manuscript. All authors critically revised the manuscript, approved the final version for publication, and agreed to be accountable for the author's own contributions and ensured that questions related to the accuracy or integrity of any part of the work are resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Institutional Review Board, Medical Ethics Committee or Medical Research, and Ethics Committee of the participating study sites. The study was conducted in concordance with the Declaration of Helsinki guidelines. All patients provided written informed consent before study participation.
Consent for publication
All the authors have provided their consent for publication.
Competing interests
WY, and DWA are employees and minor stockholders of Eli Lilly and Company. JHF is a former employee of Eli Lilly and Company and was associated with Eli Lilly till the time of manuscript submission. Her current affiliation is Agios. XM is an employee of Tech Data Services Company and performs contracted work for Eli Lilly and Company. SB was an employee of Eli Lilly and Company during the conduct of the study. DCB has received research support from Amgen, the Food and Drug Administration and the National Headache Foundation, and is a consultant to Allergan, Amgen, Eli Lilly, Lundbeck and Teva. She is a section editor for Current Pain and Headache Reports. RBL has received funding from Alder Biopharmaceuticals, Allergan, American Academy of Neurology (other activities), American Headache Society, Amgen, Autonomic Technologies (speaking and teaching), Avanir Pharmaceuticals, Biohaven Pharmaceuticals, Boston Scientific, Dr. Reddy's Laboratories, ElectroCore, Eli Lilly and Company, eNeura Therapeutics, GlaxoSmithKline, Headache (other activities) (personal fees), Informa (speaking and teaching), Merck & Co, Inc., Migraine Research Foundation, National Headache Foundation, Neurology (board membership) (serves on editorial board), National Institute on Aging (other activities), National Institute of Neurological Disorders and Stroke (other activities), Novartis (speaking and teaching) (other activities) (personal fees), Pernix, Teva Pharmaceuticals, Vedanta, and Wolff's Headache 7th and 8th Edition, Oxford University Press, 2009.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. WPAI Questions and Score.
Additional file 2. Table S1
. Change from baseline to Month 3 in WPAI domain scores. Table S2. Change in WPAI domain scores from baseline to Month 3 for responders and non-responders (EM). Table S3. Change in WPAI domain scores from baseline to Month 3 for responders and non-responders (CM). Table S4. ROC analyses for change in WPAI domain scores from baseline to Month 3 (EM). Table S5. ROC analyses for change in WPAI domain scores from baseline to Month 3 (CM). Table S6. Logistic regression of improvement in anchors on change from baseline to month 3 in WPAI domain scores. Figure S1. Spearman correlations of baseline WPAI domain scores with MSQ, and monthly migraine headache days. A Correlation of WPAI Scores with MSQ_RFP, MSQ_RFR, and Migraine Headache Days—All Patients. B Correlation of WPAI Scores with MSQ_RFP, MSQ_RFR, and Migraine Headache Days—EM Patients. C Correlation of WPAI Scores with MSQ_RFP, MSQ_RFR, and Migraine Headache Days—CM Patients. Figure S2. Cumulative distribution function plots for change in WPAI from Baseline to Month 3. A WPAI presenteeism and improvement of MSQ-RFP domain—Overall. B WPAI presenteeism and improvement of MSQ-RFP domain—EM. C WPAI presenteeism and improvement of MSQ-RFP domain—CM. D WPAI presenteeism and improvement of MSQ-RFR domain—Overall. E WPAI presenteeism and improvement of MSQ-RFR domain—EM. F WPAI presenteeism and improvement of MSQ-RFR domain—CM. G WPAI presenteeism and improvement of monthly headache days 50%—Overall. H WPAI presenteeism and improvement of monthly headache days 50%—EM. I WPAI presenteeism and improvement of monthly headache days 50%—CM. J WPAI overall work productivity loss and improvement of migraine headache days 50%—Overall. K WPAI overall work productivity loss and improvement of migraine headache days 50%—EM. L WPAI overall work productivity loss and improvement of migraine headache days 50%—CM. M WPAI overall work productivity loss and improvement of MSQ-RFR—Overall. N WPAI overall work productivity loss and improvement of MSQ-RFR—EM. O WPAI overall work productivity loss and improvement of MSQ-RFR—CM. P WPAI overall work productivity loss and improvement of MSQ-RFP—Overall. Q WPAI overall work productivity loss and improvement of MSQ-RFP—CM. R WPAI non-work-related activity impairment and improvement of migraine headache days-50%—Overall. S WPAI non-work-related activity impairment and improvement of migraine headache days-50%—EM. T WPAI non-work-related activity impairment and improvement of migraine headache days-50%—CM.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ford, J.H., Ye, W., Ayer, D.W. et al. Validation and meaningful within-patient change in work productivity and activity impairment questionnaire (WPAI) for episodic or chronic migraine. J Patient Rep Outcomes 7, 34 (2023). https://doi.org/10.1186/s41687-023-00552-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41687-023-00552-4