Abstract
Oral appliance (OA) therapy is a promising alternative to continuous positive airway pressure (CPAP) for patients with obstructive sleep apnea (OSA). By holding the mandible in a forward position, an OA keeps the airway open and prevents collapse. The recently revised practice parameters of the American Academy of Sleep Medicine extend the indications for OA therapy, recommending that “sleep physicians consider prescription of an OA for adult patients with OSA who are intolerant of CPAP therapy or prefer alternative therapy.” This manuscript reviews the practical considerations for effective OA therapy with a discussion of three factors: patient eligibility for OA therapy, device features, and requirements for OA providers. Identification of patients who are eligible for OA therapy is a key factor because the overall success rate of OA therapy is lower than that of CPAP. Conventional predictive variables have low sensitivity and specificity; however, new tools such as drug-induced sleep endoscopy and single-night polysomnographic OA titration have been developed. Other factors to consider when determining the indications for OA include the patient’s oral health, evidence of inadequate treatment for older populations, and the risk of long-term dentofacial side effects. For the second factor, customization of OA features is a key component of treatment success, and no single OA design most effectively improves every situation. Although adjustment of the mandibular position is much more important than device selection, the adjustment procedure has not been standardized. Additionally, a pitfall that tends to be forgotten is the relationship between application of the mandibular position and device selection. Promising new technology has become commercially available in the clinical setting to provide objective adherence monitoring. Finally, the third factor is the availability of enough qualified dentists because sleep medicine is a relatively new and highly multidisciplinary field. Because OSA treatments such as CPAP and OA therapy are generally considered for continuous use, treatments should be carefully planned with attention to multiple aspects. Additionally, because OA therapy requires the cooperation of professionals with different areas of expertise, such as dentists and physicians with various specialties, everyone involved in OA therapy must understand it well.
Similar content being viewed by others
Background
Obstructive sleep apnea (OSA) is a major sleep disorder. Because of repeated complete or partial collapse of the upper airway during sleep, patients develop sleep fragmentation and oxygen desaturation. OSA is estimated to occur in approximately 24% of middle-aged men and 9% of women (Young et al. 1993).
Typical nocturnal signs and symptoms of OSA are snoring, observed apnea, waking with a sensation of choking or gasping, unexplained tachycardia, restless sleep, sweating during sleep, nocturia, bruxism, nocturnal gastroesophageal reflux, insomnia, disrupted sleep, sleep walking, and sleep terrors. Daytime symptoms of OSA include excessive daytime sleepiness, afternoon drowsiness, forgetfulness, impaired concentration and attention, personality changes, and morning headache (Cao et al. 2011). As a result, OSA increases the risk of motor vehicle accidents, cardiovascular morbidity, and all-cause mortality (Marshall et al. 2008; Young et al. 2002). Therefore, OSA requires effective, appropriate treatment to preserve overall health.
Continuous positive airway pressure (CPAP), which opens and splints the upper airway with controlled compressed air, is considered the gold standard treatment for OSA. Although CPAP is highly effective in decreasing respiratory events, low acceptance and adherence are weaknesses of this therapy (Sutherland et al. 2014a and b).
Many treatment options have been developed for patients who are not eligible for CPAP therapy, including oral appliance (OA) therapy, surgery, weight loss, exercise, nasal expiratory positive airway pressure therapy, oral pressure therapy, hypoglossal nerve stimulation, and pharmacologic treatment (Sutherland et al. 2015).
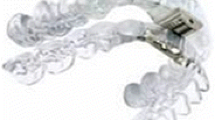
OA therapy, which holds the mandible in a forward position, works by keeping the airway open and preventing collapse. Previous imaging studies have revealed that mandibular advancement with the use of an OA enlarges the upper airway space, particularly in the lateral dimension of the velopharyngeal area (Chan et al. 2010a). Most types of OAs hold the mandible forward; therefore, they are called mandibular advancement splints, mandibular advancement devices (MADs), or prosthetic mandibular advancement. Except for the discussion about tongue-retaining devices (TRDs), the OAs in this review refer to MADs.
Recent comparisons between CPAP and OA in overnight sleep studies have shown that both treatments improve sleep-disordered breathing (SDB) (Sutherland et al. 2014a). CPAP is generally more effective than OA therapy, with a higher percentage of patients experiencing complete control of OSA. However, this greater efficacy does not necessarily translate into better health outcomes in clinical practice. The inferiority of OA therapy in reducing apneic events may be counteracted by greater treatment adherence because of more frequent nightly use of OA therapy compared with CPAP (Sutherland et al. 2014a).
The previous practice parameters of the American Academy of Sleep Medicine suggested OA therapy as a first-line treatment in patients with mild to moderate OSA and for patients with more severe OSA who fail treatment attempts with CPAP therapy (Kushida et al. 2006). In other words, first-line use of OA therapy was limited to mild to moderate OSA. The recently revised practice parameters have extended the indications for OA use, recommending that “sleep physicians consider prescription of an OA, rather than no treatment, for adult patients with OSA who are intolerant of CPAP therapy or prefer alternative therapy” (Ramar et al. 2015).
OA therapy differs from other treatment options. Patients cannot be given optimal care without crucial division of roles and collaboration between dentists and physicians with expertise in sleep medicine. In addition, OAs are generally custom-made and require delicate adjustment based on many factors, such as patients’ symptoms of OSA and oral condition. Both proper device selection and skill regarding how to adjust these devices are needed for effective treatment. This review summarizes three important components of practical, effective OA therapy: (1) eligibility of patients for OA therapy, (2) device features, and (3) requirements for OA providers.
Patient eligibility for OA therapy
Predictors of treatment success
Determining which patients are eligible for OA therapy is one key factor of successful treatment because the total success rate of OA therapy is lower than that of CPAP, and the treatment process generally requires more time and higher cost. However, although many studies have explored the subject, no standardized parameters and procedures have been established to predict the treatment response before OA fabrication. Although female sex, young age, low body mass index, small neck circumference, low baseline apnea–hypopnea index (AHI), supine-dependent OSA, and obstruction area mainly in the oropharyngeal region during sleep are reportedly associated with treatment success, none of these parameters can predict the outcome of OA treatment, either singly or combination (Chan and Cistulli 2009).
Optimal CPAP pressure (Sutherland et al. 2014b; Tsuiki et al. 2010), videoendoscopy (Sasao et al. 2014), drug-induced sleep endoscopy (DISE) (Vroegop et al. 2013), and remotely controlled mandibular protrusion (RCMP) assessment, which involves titration of the mandibular position during a sleep study similar to CPAP titration (Remmers et al. 2013), have recently been introduced as new indicators or tools with which to predict treatment responders and are more effective than some conventional variables. These are favorable tools in the clinical setting under the appropriate circumstances, although some require extra cost and examination.
A few studies have explained why anatomical measurement can partially predict the treatment response, although OAs are considered to enlarge the upper airway space, particularly in the lateral dimension of the velopharyngeal area (Chan et al. 2010a). Vroegop et al. (Vroegop et al. 2014) reported variations in the obstruction area in 1249 patients who underwent DISE study. That study revealed that 68.2% of patients had multiple obstructive areas. Thus, the obstruction area is not the only narrow area in the airway; the airway dynamics dramatically change during sleep.
Another current area of research interest is the attempt to define pathophysiological phenotypes of OSA. In one study (Eckert et al. 2013), four key anatomical and non-anatomical mechanisms were measured in more than 50 individuals with OSA. The passive critical closing pressure, an indicator of collapsibility of the upper airway, was measured as an anatomic factor. Non-anatomic factors included the arousal threshold, loop gain, and upper airway dilator muscle responsiveness. The study results revealed that 81% of patients had a highly collapsible airway. With respect to non-anatomic factors, 36% of patients exhibited minimal genioglossus muscle responsiveness, 37% had a low arousal threshold, and 36% had high loop gain. One or more non-anatomic pathophysiologic traits were present in 69% of patients with OSA. In addition, non-anatomic features played an important role in 56% of patients with OSA. The findings of that study indicate that non-anatomic factors are important and may be even more important than anatomic features in some patients, although a prime predisposing factor in most patients with OSA is a highly collapsible airway. A study based on this concept recently showed that OA improved upper airway collapsibility without affecting muscle function, loop gain, or the arousal threshold (Edwards et al. 2016). This suggests that patients with better passive upper airway anatomy/collapsibility and low loop gain will obtain the greatest benefit from OA therapy (Edwards et al. 2016). Gray et al. (2016) reported that non-obese patients with OSA were more likely to have a low respiratory arousal threshold and that these patients were difficult to treat with CPAP. In another study, Nerfeldt and Friberg (2016) compared adherence to and treatment effects of OA therapy between patients with two types of OSA: those with mainly respiratory arousals (“arousers”) and those with oxygen desaturations (“desaturaters”). The authors found that the 1-year adherence rate was significantly higher among arousers (85%) than desaturaters (55%), although the reduction in the AHI was similar in both groups. These results seem reasonable and can help to explain why we cannot predict the treatment response based on anatomic factors alone. Therefore, OSA phenotyping promises to be an important part of future treatment strategies.
Oral health of patients with OSA
A frequent barrier to OA therapy initiation is the patient’s dental or oral health status. Petit et al. (2002) determined the contraindication rate in 100 consecutive patients referred for suspected OSA. In that survey, 34% of patients had a contraindication to OA therapy, and another 16% required close supervision and follow-up to avoid impairment of preexisting temporomandibular joint or dental problems. This is one of the inconvenient considerations involved in treatment decisions: many patients cannot use an OA or require time to complete dental treatment before the device can be prescribed. This is especially true in older patients, who have more dental concerns than do younger patients.
Several recent studies have suggested an association between tooth loss and OSA. One questionnaire-based survey found that 40.3% of edentulous participants had a high probability of having OSA Tsuda et al. (Epub). Another cross-sectional study of community-dwelling older adults revealed a significant association between denture use and an AHI of >15 (odds ratio, 6.29; confidence interval, 1.71–23.22; P = 0.006) (Endeshaw et al. 2004). A recent national health and nutrition examination study also revealed a relationship between the risk of OSA and certain oral health variables such as tooth loss, occlusal contacts, and denture use (Sanders et al. 2016). That study revealed that chance of developing a high risk for OSA increased by 2% for each additional lost tooth among adults aged 25 to 65 years.
Another dental problem in patients undergoing OA therapy is chronic periodontitis, which is the major cause of tooth loss (Phipps and Stevens 1995). Gunaratnam et al. (2009) reported a four-times-higher prevalence of periodontitis among patients with OSA than historical controls from a national survey. A recent large, community-based, cross-sectional study revealed that the adjusted odds of severe periodontitis was 40% higher in patients with subclinical SDB, 60% higher in those with mild SDB, and 50% higher in those with moderate/severe SDB compared with the non-apneic reference (Sanders et al. 2015). The novel association between mild SDB and periodontitis was most pronounced in young adults.
Dry mouth is a common symptom among patients with sleep apnea; it is also an important indicator of oral health (Oksenberg et al. 2006; Ruhle et al. 2011; Kreivi et al. 2010). Several reports have suggested that patients with dry mouth or salivary hypofunction have significantly more caries, fewer teeth, and more pain related to denture use than patients without these symptoms (Hopcraft and Tan 2010). Salivary output reaches its lowest levels during sleep, and the mouth breathing seen in patients with OSA can worsen dryness.
Sleep bruxism is a more concerning topic than OSA among dentists because it is one of the factors that causes prosthetic damage. An occlusal splint that covers only the maxillary dental arch is frequently prescribed for sleep bruxism without the need for a sleep study. Gagnon et al. (2004) estimated the effect of occlusal splints in patients with OSA. The authors reported that the AHI increased by >50% in 5 of 10 patients and that the sleeping time with snoring increased by 40% with use of the occlusal splint. This risk of aggravation associated with occlusal splints should be generally known because sleep bruxism is frequently seen in patients with OSA (Cao et al. 2011). Some authors have reported the treatment effects of OA therapy or CPAP for sleep bruxism (Landry-Schönbeck et al. 2009; Oksenberg and Arons 2002). However, some patients with OSA who exhibit sleep bruxism have reportedly broken their OA by the grinding events in the clinical setting. Because the relationship between OSA and sleep bruxism remains unclear, it may be a confounding factor in treatment decisions.
Healthy dentition is required for OA therapy, and patients with OSA are at high risk for developing the above-mentioned oral conditions. An alternative option for patients with inappropriate dentition is a TRD. A TRD features an extraoral flexible bulb and holds the tongue forward by suction. One type of TRD, the tongue-stabilizing device (TSD), is prefabricated. Because this device does not require the presence of teeth for retention, the patient’s dental condition does not need to be considered. A TSD is suggested for patients who poorly tolerate an MAD; inadequate device retention is a potential issue that reduces the effectiveness of such devices in patients with normal dentition, although objective testing of MADs and TSDs have shown similar efficacy in terms of AHI reduction (Deane et al. 2009). A TSD is never the first-line device for OA therapy; however, these prefabricated devices have advantages for patients whose dentition is not appropriate for a MAD or for patients undergoing dental treatment.
Aging
The prevalence of OSA among older patients is higher than that among middle-aged patients (Young et al. 2002). Most treatment efficacy trials have examined individuals aged <65 years. There is insufficient evidence to support the efficacy of OA therapy in older people. This population has an increased prevalence of dental disease, including missing teeth and periodontitis. The current practice parameters suggest that a clear recommendation for MAS, MAD, or TSD as first-line treatment in patients with mild to moderate SDB cannot be made because of poor evidence. The practice parameters suggest that in the case of CPAP failure, second-line treatment with a MAS, MAD, or TSD is recommended in older patients with SDB after full assessment of the dental status (Netzer et al. 2016).
Nocturia is a frequently overlooked cause of poor sleep in older patients (Bliwise et al. 2009). Nocturia is relatively common in patients with OSA, and 28% of patients reportedly take four to seven nightly trips to the bathroom (Hajduk et al. 2003). OSA has been suggested as an independent cause of frequent nocturia in older men (Guilleminault et al. 2004). In the clinical setting, some patients have reported that they discontinue CPAP use after removing the mask to go to the bathroom. Although nocturia may not be completely relieved with OSA therapy, OA therapy makes trips to the bathroom easier than does CPAP.
Side effects of OA therapy
Side effects of OA therapy are divided into two types: transient and permanent. During initiation of OA therapy, common adverse side effects include excessive salivation, mouth dryness, tooth pain, gum irritation, headaches, and temporomandibular joint discomfort. Although the reported frequencies of side effects vary greatly (Ferguson et al. 2006), symptoms are usually transient, lasting around 2 months.
When considering OA therapy as a treatment option, permanent side effects, mainly tooth movement, may be an important factor for some patients. Possible dental changes associated with OA therapy include decreased overbite (the vertical overlap of the lower teeth by the upper) and overjet (the horizontal overlap of the lower teeth by the upper), forward inclination of the lower incisors and backward inclination of the upper incisors, changes in anteroposterior occlusion, and a reduction in the number of occlusal contacts. A study of the long-term dental side effects during a decade of OA treatment revealed clinically significant and progressive changes in occlusion (Pliska et al. 2014). These side effects generally do not affect masticatory function, and many patients are unaware of any changes in their bite. Most patients concur that positive effects of OA treatment far outweigh any adverse effects related to dental changes (Marklund and Franklin 2007). However, tooth movement was found in 85.7% of patients in a 5-year analysis (Almeida et al. 2006). The possibility of occlusal change should be explained to patients, especially young patients, those with esthetic requirements, and those with narrow acceptance of occlusal change.
Tooth movement is a well-known side effect of OA therapy; however, dentofacial side effects of CPAP therapy are not yet well recognized. Cephalometric analysis of CPAP users during a 2-year period revealed significant craniofacial changes characterized by reduced maxillary and mandibular prominence and/or alteration of the relationship between the dental arches (Tsuda et al. 2010). Another research group reported a significant decrease in the number of occlusal contact points in the premolar region in patients using a CPAP device during a 2-year period (Doff et al. 2013). Patients treated with CPAP as well as those using an OA need thorough follow-up with a dental specialist experienced in the field of dental sleep medicine to ensure their oral health.
Eligibility for adjunctive therapy
OA therapy may be used as part of combination therapy or as monotherapy. Considering long-term treatment, it is important to consider each patient’s OSA characteristics and lifestyle.
Positional therapy in patients with residual supine-dependent OSA undergoing OA therapy leads to greater therapeutic efficacy than either treatment modality alone (Dieltjens et al. 2015).
El-Solh et al. 2011 suggested combined therapy comprising CPAP and an OA based on their data suggesting that the optimal CPAP pressure was reduced with combination therapy, allowing all subjects in their study to tolerate CPAP.
A recent meta-analysis comparing the efficacy of CPAP, OA therapy, exercise training, and dietary weight loss revealed that exercise training, which significantly improves daytime sleepiness, could be used as an adjunct to CPAP or OA therapy (Iftikhar et al. 2017).
CPAP is difficult to use in patients with seasonal nasal congestion, during travel, and sometimes after evacuation in case of a disaster. An OA can be used as a temporary alternative to CPAP, although its efficacy may not be adequate for routine use. The treatment plan must be determined with consideration of multiple factors.
Appliance features
Appliance design
A variety of OAs have become available on the market. Devices are characterized according to their method of retention (mandible or tongue), fabrication (preformed or custom-made), adjustability (in both the vertical and anteroposterior dimensions), allowance of jaw movement (monoblock or twin-block), and flexibility of materials (soft elastic or hard acrylic). Few studies to date have compared the efficacy of different designs. A systematic review of the efficacy of OAs according to their design suggested that no single OA design most effectively improves polysomnographic indices, and careful consideration is needed because efficacy depends on the severity of OSA as well as the OA materials, method of fabrication, and type (monoblock/twin-block) (Ahrens et al. 2011).
Fabrication of a custom-made OA typically begins with the creation of dental casts of the patient’s dentition and bite registration. These chair-side steps, including initiation or adjustment of the device after laboratory work, are generally conducted by an experienced dentist. This process therefore requires time and cost. In contrast, a device molded of thermoplastic polymer materials, a so-called “boil and bite” OA, is sometimes introduced as a low-cost and easily made alternative to a custom-made appliance. The patient bites into the softened material with a roughly advanced jaw position until this configuration sets with cooling. However, thermoplastic OAs are associated with insufficient mandibular protrusion and poor retention in the patient’s mouth. A crossover study comparing the efficacy of thermoplastic and custom-made OAs showed that the post-treatment AHI was reduced only with the custom-made OA (Vanderveken et al. 2008). In addition, the thermoplastic device had a much lower rate of treatment success (60% vs 31%, respectively), and 82% of subjects preferred the customized OA at the end of the study. That study suggests that customization is a key component of treatment success. The most recent practice guideline also suggests that “a qualified dentist use a custom, titratable appliance over non-custom oral devices” (Ramar et al. 2015).
Differences in durability or the frequency of follow-up visits might influence device selection; however, data on which to base firm recommendations are lacking. One study of the side effects and technical complications of OAs during a 5-year follow-up period reported that patients made a mean of 2.5 unscheduled dental visits per year and a mean of 0.8 appliance repairs/relines per year with a dental technician (Martinez-Gomis et al. 2010). The most frequent problems among the study participants were acrylic breakage on the lateral telescopic attachment, poor retention, and the need for additional adjustments to improve comfort. Because these results may depend on the design of the device, more detailed evaluations are needed.
Titration procedure
Setting the mandibular position is critical to optimize OA therapy. It is generally thought that greater advancement is associated with a better treatment effect (Kato et al. 2000). However, a meta-regression analysis of different amounts of mandibular advancement in 13 randomized controlled trials showed that advancement amounts of >50% do not significantly influence the success rate (Bartolucci et al. 2016). Remmers et al. (2013) evaluated the ability to predict therapeutic success based on sleep studies using a remotely controlled mandibular protrusion device. The effective target protrusion position values were relatively small, with the smallest being 6% and the median being 68% of the patient’s protrusive range. Based on these reports, it seems that some patients do not need a large amount of advancement and that their devices may be over-protruding the mandible. The applied mandibular position must be balanced because too much advancement increases the risk of side effects. Although it is clearly important to achieve an optimized mandibular position for treatment success, the titration procedure is not currently standardized (Chan et al. 2010b).
One review classified the titration procedures for OAs as follows: 1) subjective titration (titration solely based on the physical limits of the patient as indicated by self-reported evolution of symptoms and physical limits), 2) objective titration (initial overnight titration of mandibular advancement during polysomnography), and 3) multiparametric titration (combination of subjective and objective findings by a single-channel device, type III portable monitoring device, and polysomnography) (Dieltjens et al. 2012).
The most popular titration procedure in the clinical setting is based on the patient’s subjective response to OA use. If a patient reports that snoring, sleepiness, or morning headache persist without side effects such as tooth pain or jaw muscle pain, the dentist advances the OA. Conversely, if the patient reports side effects, the jaw position of the OA is set back. These adjustments continue until a maximum subjective effect is achieved.
The problem associated with this titration procedure is the time-consuming steps needed and the risk of under-titration because of the absence of an objective parameter. Almeida et al. (2009) showed that subjective titration by self-reporting is often insufficient and that some patients miss the chance for successful treatment. Several subjects in their study had residual respiratory events after titration based on subjective responses; 17.4 to 30.4% of patients, depending on the definition of treatment success, could be treated with additional titration under a polysomnographic study. In the clinical setting, a follow-up sleep study is crucial to objectively verify satisfactory treatment and thus improve clinical outcomes.
Initial overnight titration may have additional benefits other than determining the titration protocol. The advantage of this type of titration is that in addition to estimating the optimal jaw position, it also predicts which patients will respond to treatment before beginning the customized OA fabrication. Because a low success rate is the biggest concern when making treatment decisions, accurate prediction of treatment responders is one of the most important issues in OA therapy. Thus, initial overnight titration is considered the most likely titration protocol to be standardized.
Several studies have estimated the accuracy and usefulness of overnight titration procedures (Table 1). One report used the appliance itself as a titration appliance (Raphaelson et al. 1998); others used a temporary appliance for the titration study and evaluated the treatment efficacy and accuracy of treatment prediction using a customized appliance with a titrated mandibular position (Remmers et al. 2013; Kuna et al. 2006; Dort et al. 2006; Tsai et al. 2004; Petelle et al. 2002; Zhou and Liu 2012).
Raphaelson et al. (1998) conducted initial overnight titration in six subjects by awakening the subjects each time the appliance was advanced. Although the authors did not report the amount of jaw advancement, they suggested that progressive jaw advancement could determine the optimal jaw position for eliminating sleep apnea and snoring.
Kuna et al. (2006) used a commercialized low-cost temporary titration appliance in their study. Although 42.9% of subjects achieved the criteria of successful treatment, such as an AHI of <10 and 50% reduction from the baseline AHI, none exhibited the same success rate with a prescribed appliance using the same jaw position estimated during the titration night. Following additional advancement, 47% of subjects achieved effective AHI reduction (AHI of <15 and 50% reduction from baseline AHI). The authors concluded that titration data cannot predict the efficacy of long-term appliance treatment.
Petelle et al. (2002) first reported a system for titration sleep studies using a hydraulic, remotely adjustable temporary appliance. Although the number of participants was small, three of seven reduced their AHI to <20 from a baseline AHI of 66.9 ± 32.4. These three patients exhibited similar results with a prescribed appliance, and two of the four patients who continued to have more than 20 obstructive events during the titration study also reduced their AHI to <20 with their prescribed appliance.
Tsai et al. (2004), Dort et al. (2006), and Remmers et al. (2013) used RCMPs in their studies. This titration system advances the mandible until obstructive respiratory events and snoring are eliminated. After the titration studies, the patients underwent another sleep study with a custom-made appliance. In the studies by Dort et al. (2006) and Remmers et al. (2013), the jaw position was estimated based on the RCMP study. In contrast, a conventional titration procedure was used by Tsai et al. (2004). Ten of 19 subjects (52.6%) in the study by Tsai et al. (2004), 16 of 33 (48.5%) in the study by Dort et al. (2006), and 58.2% in the study by Remmers et al. (2013) were treatment responders according to the definition of treatment success for each study. The positive and negative predictive values for treatment success were 90 and 89%, respectively, in the study by Tsai et al. (2004); 80 and 78%, respectively, in the study by Dort et al. (2006); and 94 and 83%, respectively, in the study by Remmers et al. (2013). Despite the high predictive rates found by Tsai et al. (2004), meaningful correlations were not found between the individual protrusion values determined by the RCMP and those at the end of the study. Remmers et al. (2013) also reported that 87.1% of their subjects were successfully treated with an estimated position; however, four subjects who were predicted to be treatment responders needed additional mandibular advancement on their fabricated final appliances.
Ferguson et al. (2006) reported that patients with mild to severe OSA have a 52% chance of controlling their sleep apnea with an OA. An overnight titration protocol seemed to result in higher treatment success rates than conventional procedures.
Zhou and Liu (2012) evaluated differences in treatment results between prescribed appliances. Titration was performed with a remote control device until a maximum reduction in the AHI was achieved. Patients received both monoblock and twin-block type appliances and underwent a sleep study to evaluate treatment efficacy. Although both appliances maintained the same jaw position based on the titration study data, the monoblock appliance reduced the AHI more than the twin-block appliance (baseline AHI, 26.4 ± 4.1; AHI with monoblock appliance, 6.6 ± 2.3; AHI with twin-block appliance, 9.9 ± 2.9). Forty-four percent of patients preferred the monoblock appliance, whereas 13% preferred the twin-block appliance.
When a single-night titration procedure is used to estimate the treatment response, RCMP studies might show acceptable results in clinical use. The limitation of this procedure is the lack of information about side effects, such as tooth or jaw pain, with long-term use. Some patients may not tolerate an OA because of excessive jaw advancement despite the fact that this achieves optimal positioning to eliminate respiratory events.
Considering the titration procedure, the difference between temporary appliances for titration and the prescribed final appliance should be mentioned. Zhou and Liu (2012) demonstrated different results with a monoblock versus twin-block appliance using the same jaw position during a single-night titration study. Similar interesting results have been reported in comparison studies of two different MADs (Geoghegan et al. 2015; Isacsson et al. 2016). Geoghegan et al. (2015) evaluated the effects of two different MADs (monoblock and twin-block) with the same bite registration as used in the study by Zhou and Liu (2012) and found that monoblock appliances reduced the AHI more than twin-block appliances. Conversely, in another study comparing monoblock and twin-block appliances, Isacsson et al. (2016) reported that both types significantly reduced the AHI and sleepiness to the same degree. Importantly, the mandible protruded an average of 3 mm more in the twin-block than monoblock appliance group. The reported average maximum protrusion in young adults is 8.0 mm (range, 2.5–13.5 mm) (Woelfel et al. 2014). To determine the optimal jaw position that controls OSA symptoms, titrations of the appliance are usually repeated by the dentist with minuscule advancements, such 0.25 to 1.00 mm. In terms of structure or mechanism, the jaw position that is applied with a monoblock appliance is identical to the bite registration if it is properly fabricated. Conversely, an adjustable or twin-block appliance allows mandibular movement including vertical opening with retroclination of the mandible. Although patients generally appreciate this flexibility, the protrusion achieved with a twin-block appliance is clearly less than the bite registration or that achieved with a monoblock appliance.
Because titration is a very sensitive procedure, bite registration and consideration of appliance characteristics are essential.
Objective adherence monitoring
Compared with CPAP, in which adherence can be objectively monitored, most adherence data for OA therapy has been limited to patients’ self-reports. This lack of objective monitoring may be a concern of sleep physicians when referring patients for OA therapy, especially patients with serious morbidities requiring strict OSA management. Commercially available objective adherence monitors have recently been developed for OA therapy, representing a great advancement in both research and clinical practice (Vanderveken et al. 2013; Inoko et al. 2009; Bonato and Bradley 2013). Vanderveken et al. (2013) estimated the safety and feasibility of a microsensor (TheraMon) with on-chip integrated readout electronics. Their study was based on the assumption that the OA therapy was being used at a measured temperature of >35 °C. No microsensor-related adverse events occurred during study period, and no statistically significant difference was found between the objective and self-reported compliance data (Vanderveken et al. 2013). Another commercially available sensor (DentiTrac) with an internal battery, internal sensors, internal memory storage, and a method to retrieve information from the data logger was also recently introduced (Bonato and Bradley 2013). Both of these adherence monitors are small enough to embed in the OA without interrupting the patient’s comfort and can be to attached to any type of OA. In the clinical setting, adherence monitors may motivate appliance use, and objective data can serve as a communication tool between the physician and dentist. Furthermore, objective data can be used for commercial drivers to prove treatment compliance for their reinstatement (Sutherland et al. 2014a).
Knowledge and skill related to dental sleep medicine among dentists
One of the roles of dentists in sleep medicine is providing OA therapy for patients with sleep apnea. The American Board of Dental Sleep Medicine (ABDSM), established in 2004, is an independent, nonprofit board of examiners that certifies dentists who treat snoring and OSA with OA therapy. Although more than 270 ABDSM diplomates are providing quality treatment for patients across the US (http://www.abdsm.org/About.aspx), more qualified dentists are needed in this field.
Difficulties have been encountered in developing educational programs in sleep medicine at academic institutions because the field is relatively new and highly multidisciplinary. In 2004, a questionnaire-based survey of 192 general dental practitioners revealed that 58% of dentists could not identify common signs and symptoms of OSA and that 55% did not know the therapeutic mechanism of OAs, despite the fact that 93% agreed that OSA constitutes a life-threatening illness (Bian 2004).
Simmons and Pullinger (2012) reported that the teaching time dedicated to sleep medicine in predoctoral dental programs in the US had increased to 3.92 h, but the authors still considered this to be insufficient. One of the authors of the present review conducted a similar survey of Japanese dental schools. Of the responding schools, 80.8% reported some educational time devoted to sleep medicine; the average was 3.8 instruction hours, which is similar to the findings in the survey by Simmons and Pullinger (2012). Most sleep medicine instruction was didactic (58.5%); only 11.5% of institutions reported a hands-on clinical laboratory experience (Tsuda et al. 2014).
For appropriate OA therapy, dentists need both technical skills to adjust the appliance and fundamental knowledge in areas such as pathophysiology, typical symptoms of OSA, sleep study interpretation, and alternate treatment options to communicate effectively with patients and sleep physicians. Sleep physicians’ specialties vary and include respirology, otolaryngology, cardiology, neurology, and psychiatry, and their treatment strategies also vary. Each of these specialists should understand this multidisciplinary situation, and dentistry should also be recognized as a specialty in sleep medicine. Current practice guidelines recommend close cooperation between sleep physicians and qualified dentists to optimize patient care (Ramar et al. 2015).
Because healthcare systems differ among countries, original treatment strategies and educational curricula should be developed to maximize the quality and cost-effectiveness of treatment according to each country’s situation. Importantly, the planning and execution of sleep medicine education in dental schools should be based not only on the dentist’s limited role, but also on the dentist’s role in general disease management within the healthcare system.
Conclusion
This manuscript reviewed practical considerations for effective OA therapy with assessment of three factors: patient eligibility for OA therapy, device features, and requirements for OA providers. Because neither CPAP nor OA therapy cures OSA, continuous use of these devices is required. Although OA therapy does not completely relieve respiratory events in all patients, the advantages and disadvantages of OA therapy differ from those of CPAP. Treatment decisions should be carefully planned with assessment of multiple factors. The three above-mentioned factors may seem to lack an inter-relationship or to be of low importance, but treatment optimization is impossible without considering all of them, especially in the clinical setting (Fig. 1). Because OA therapy requires cooperation among professionals with different areas of expertise, such as dentists and physicians of many specialties, everyone involved in therapy must understand both the benefits and drawbacks or challenges of therapy.
Abbreviations
- AHI:
-
Apnea–hypopnea index
- CPAP:
-
Continuous positive airway pressure
- MAD:
-
Mandibular advancement device
- OA:
-
Oral appliance
- OSA:
-
Obstructive sleep apnea
- RCMP:
-
Remotely controlled mandibular protrusion
- SDB:
-
Sleep-disordered breathing
- TRD:
-
Tongue-retaining device
- TSD:
-
Tongue-stabilizing device
References
Ahrens A, McGrath C, Hagg U. A systematic review of the efficacy of oral appliance design in the management of obstructive sleep apnoea. Eur J Orthod. 2011;33(3):318–24.
Almeida FR, Lowe AA, Otsuka R, et al. Long-term sequellae of oral appliance therapy in obstructive sleep apnea patients: Part 2. Study-model analysis. Am J Orthod Dentofacial Orthop. 2006;129(2):205–13. Epub 2006/02/14. (Article in eng).
Almeida FR, Parker JA, Hodges JS, et al. Effect of a titration polysomnogram on treatment success with a mandibular repositioning appliance. J Clin Sleep Med. 2009;5(3):198–204.
Bartolucci ML, Bortolotti F, Raffaelli E, et al. The effectiveness of different mandibular advancement amounts in OSA patients: a systematic review and meta-regression analysis. Sleep Breath. 2016;20(3):911–9.
Bian H. Knowledge, opinions, and clinical experience of general practice dentists toward obstructive sleep apnea and oral appliances. Sleep Breath. 2004;8(2):85–90.
Bliwise DL, Foley DJ, Vitiello MV, et al. Nocturia and disturbed sleep in the elderly. Sleep Med. 2009;10(5):540–8. Pubmed Central PMCID: 2735085.
Bonato RA, Bradley DC. Introducing a novel micro-recorder for the detection of oral appliance compliance: DentiTrac. Sleep Diagn Ther. 2013;8:12–5.
Cao M, Guilleminault C, Kushida C. Clinical features and evaluation of obstructive sleep apnea and upper airway resistance syndrome. In: Principles and practice of sleep medicine. Philadelphia: Elsevier Saunders; 2011. p. 1206–18.
Chan AS, Cistulli PA. Oral appliance treatment of obstructive sleep apnea: an update. Curr Opin Pulm Med. 2009;15(6):591–6.
Chan AS, Sutherland K, Schwab RJ, et al. The effect of mandibular advancement on upper airway structure in obstructive sleep apnoea. Thorax. 2010a;65(8):726–32.
Chan AS, Phillips CL, Cistulli PA. Obstructive sleep apnoea--an update. Intern Med J. 2010b;40(2):102–6.
Deane SA, Cistulli PA, Ng AT, et al. Comparison of mandibular advancement splint and tongue stabilizing device in obstructive sleep apnea: a randomized controlled trial. Sleep. 2009;32(5):648–53. Pubmed Central PMCID: 2675900. Epub 2009/06/02. (Article in eng).
Dieltjens M, Vanderveken OM, Heyning PH, et al. Current opinions and clinical practice in the titration of oral appliances in the treatment of sleep-disordered breathing. Sleep Med Rev. 2012;16(2):177–85.
Dieltjens M, Vroegop AV, Verbruggen AE, et al. A promising concept of combination therapy for positional obstructive sleep apnea. Sleep Breath. 2015;19(2):637–44. Pubmed Central PMCID: 4873543.
Doff MH, Finnema KJ, Hoekema A, et al. Long-term oral appliance therapy in obstructive sleep apnea syndrome: a controlled study on dental side effects. Clin Oral Investig. 2013;17(2):475–82. Pubmed Central PMCID: 3579417.
Dort LC, Hadjuk E, Remmers JE. Mandibular advancement and obstructive sleep apnoea: a method for determining effective mandibular protrusion. Eur Respir J. 2006;27(5):1003–9. Epub 2006/05/19. (Article in eng).
Eckert DJ, White DP, Jordan AS, et al. Defining phenotypic causes of obstructive sleep apnea. Identification of novel therapeutic targets. Am J Respir Crit Care Med. 2013;188(8):996–1004. Pubmed Central PMCID: 3826282.
Edwards BA, Andara C, Landry S, Sands SA, Joosten SA, Owens RL, et al. Upper-airway Collapsibility and Loop Gain Predict the Response to Oral Appliance Therapy in Patients with Obstructive Sleep Apnea. Am J Respir Crit Care Med. 2016;194(11):1413–22.
El-Solh AA, Moitheennazima B, Akinnusi ME, Churder PM, Lafornara AM. Combined oral appliance and positive airway pressure therapy for obstructive sleep apnea: a pilot study. Sleep Breath. 2011;15(2):203–8.
Endeshaw YW, Katz S, Ouslander JG, et al. Association of denture use with sleep-disordered breathing among older adults. J Public Health Dent. 2004;64(3):181–3. Epub 2004/09/03. (Article in eng).
Ferguson KA, Cartwright R, Rogers R, et al. Oral appliances for snoring and obstructive sleep apnea: a review. Sleep. 2006;29(2):244–62. Epub 2006/02/24. (Article in eng).
Gagnon Y, Mayer P, Morisson F, et al. Aggravation of respiratory disturbances by the use of an occlusal splint in apneic patients: a pilot study. Int J Prosthodont. 2004;17(4):447–53. Epub 2004/09/24. (Article in eng).
Geoghegan F, Ahrens A, McGrath C, et al. An evaluation of two different mandibular advancement devices on craniofacial characteristics and upper airway dimensions of Chinese adult obstructive sleep apnea patients. Angle Orthod. 2015;85(6):962–8.
Gray E, McKenzie D, Eckert D. Obstructive Sleep Apnea Without Obesity is Common and Difficult to Treat: Evidence for a Distinct Pathophysiological Phenotype. J Clin Sleep Med. 2016;13(1):81–88.
Guilleminault C, Lin CM, Goncalves MA, et al. A prospective study of nocturia and the quality of life of elderly patients with obstructive sleep apnea or sleep onset insomnia. J Psychosom Res. 2004;56(5):511–5.
Gunaratnam K, Taylor B, Curtis B, et al. Obstructive sleep apnoea and periodontitis: a novel association? Sleep Breath. 2009;13(3):233–9. Epub 2009/02/10. (Article in eng).
Hajduk IA, Strollo Jr PJ, Jasani RR, et al. Prevalence and predictors of nocturia in obstructive sleep apnea-hypopnea syndrome--a retrospective study. Sleep. 2003;26(1):61–4.
Hopcraft MS, Tan C. Xerostomia: an update for clinicians. Aust Dent J. 2010;55(3):238–44. quiz 353.
Iftikhar IH, Bittencourt L, Youngstedt SD, Ayas N, Cistulli P, Schwab R, et al. Comparative efficacy of CPAP, MADs, exercise-training, and dietary weight loss for sleep apnea: a network meta-analysis. Sleep Med. 2017;30:7–14
Inoko Y, Yoshimura K, Kato C, et al. Efficacy and safety of temperature data loggers in measuring compliance with the use of oral appliances. Sleep Biol Rhythms. 2009;7(3):188–92.
Isacsson G, Fodor C, Sturebrand M. Obstructive sleep apnea treated with custom-made bibloc and monobloc oral appliances: a retrospective comparative study. Sleep Breath. 2017;1:93–100
Kato J, Isono S, Tanaka A, et al. Dose-dependent effects of mandibular advancement on pharyngeal mechanics and nocturnal oxygenation in patients with sleep-disordered breathing. Chest. 2000;117(4):1065–72.
Kreivi HR, Virkkula P, Lehto J, et al. Frequency of upper airway symptoms before and during continuous positive airway pressure treatment in patients with obstructive sleep apnea syndrome. Respiration. 2010;80(6):488–94.
Kuna ST, Giarraputo PC, Stanton DC, et al. Evaluation of an oral mandibular advancement titration appliance. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(5):593–603. Epub 2006/04/25. (Article in eng).
Kushida CA, Morgenthaler TI, Littner MR, et al. Practice parameters for the treatment of snoring and Obstructive Sleep Apnea with oral appliances: an update for 2005. Sleep. 2006;29(2):240–3. Epub 2006/02/24. (Article in eng).
Landry-Schönbeck A, de Grandmont P, Rompré PH, Lavigne GJ. Effect of an adjustable mandibular advancement appliance on sleep bruxism: a crossover sleep laboratory study. Int J Prosthodont. 2009;22(3);251–59.
Marklund M, Franklin KA. Long-term effects of mandibular repositioning appliances on symptoms of sleep apnoea. J Sleep Res. 2007;16(4):414–20. Epub 2007/11/27. (Article in eng).
Marshall NS, Wong KK, Liu PY, et al. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep. 2008;31(8):1079–85. Pubmed Central PMCID: 2542953.
Martinez-Gomis J, Willaert E, Nogues L, et al. Five years of sleep apnea treatment with a mandibular advancement device. Side effects and technical complications. Angle Orthod. 2010;80(1):30–6.
Nerfeldt P, Friberg D. Effectiveness of oral appliances in obstructive sleep apnea with respiratory arousals. J Clin Sleep Med. 2016;12(8):1159–65. Pubmed Central PMCID: 4957194.
Netzer NC, Ancoli-Israel S, Bliwise DL, Fulda S, Roffe C, Almeida F, et al. Principles of practice parameters for the treatment of sleep disordered breathing in the elderly and frail elderly: the consensus of the International Geriatric Sleep Medicine Task Force. Eur Respir J. 2016:ERJ-01975-2015.
Oksenberg A, Arons E. Sleep bruxism related to obstructive sleep apnea: the effect of continuous positive airway pressure. Sleep Med. 2002;3(6):513–5.
Oksenberg A, Froom P, Melamed S. Dry mouth upon awakening in obstructive sleep apnea. J Sleep Res. 2006;15(3):317–20.
Petelle B, Vincent G, Gagnadoux F, et al. One-night mandibular advancement titration for obstructive sleep apnea syndrome: a pilot study. Am J Respir Crit Care Med. 2002;165(8):1150–3. Epub 2002/04/17. (Article in eng).
Petit FX, Pepin JL, Bettega G, et al. Mandibular advancement devices: rate of contraindications in 100 consecutive obstructive sleep apnea patients. Am J Respir Crit Care Med. 2002;166(3):274–8. Epub 2002/08/03. (Article in eng).
Phipps KR, Stevens VJ. Relative contribution of caries and periodontal disease in adult tooth loss for an HMO dental population. J Public Health Dent. 1995;55(4):250–2.
Pliska BT, Nam H, Chen H, Lowe AA, Almeida FR. Obstructive sleep apnea and mandibular advancement splints: occlusal effects and progression of changes associated with a decade of treatment. J Clin Sleep Med 2014;10(12):1285-1291 publication of the American Academy of Sleep Medicine. 2014;10(12):1285.
Ramar K, Dort LC, Katz SG, Lettieri CJ, Harrod CG, Thomas SM, et al. Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015. J Clin Sleep Med. 2015;11(7):773–827.
Raphaelson MA, Alpher EJ, Bakker KW, et al. Oral appliance therapy for obstructive sleep apnea syndrome: progressive mandibular advancement during polysomnography. Cranio. 1998;16(1):44–50. Epub 1998/03/03. (Article in eng).
Remmers J, Charkhandeh S, Grosse J, et al. Remotely controlled mandibular protrusion during sleep predicts therapeutic success with oral appliances in patients with obstructive sleep apnea. Sleep. 2013;36(10):1517–25. Pubmed Central PMCID: 3773201, 25A.
Ruhle KH, Franke KJ, Domanski U, et al. Quality of life, compliance, sleep and nasopharyngeal side effects during CPAP therapy with and without controlled heated humidification. Sleep Breath. 2011;15(3):479–85.
Sanders AE, Essick GK, Beck JD, et al. Periodontitis and sleep disordered breathing in the Hispanic community health study/study of Latinos. Sleep. 2015;38(8):1195–203. Pubmed Central PMCID: 4507724.
Sanders AE, Akinkugbe AA, Slade GD, et al. Tooth loss and obstructive sleep apnea signs and symptoms in the US population. Sleep Breath. 2016;20(3):1095–102. Pubmed Central PMCID: 4947024.
Sasao Y, Nohara K, Okuno K, et al. Videoendoscopic diagnosis for predicting the response to oral appliance therapy in severe obstructive sleep apnea. Sleep Breath. 2014;18(4):809–15.
Simmons MS, Pullinger A. Education in sleep disorders in US dental schools DDS programs. Sleep Breath. 2012;16(2):383–92. Pubmed Central PMCID: 3306848.
Sutherland K, Vanderveken OM, Tsuda H, et al. Oral appliance treatment for obstructive sleep apnea: an update. J Clin Sleep Med. 2014a;10(2):215–27. Pubmed Central PMCID: 3899326.
Sutherland K, Phillips CL, Davies A, et al. CPAP pressure for prediction of oral appliance treatment response in obstructive sleep apnea. J Clin Sleep Med. 2014b;10(9):943–9. Pubmed Central PMCID: 4153122.
Sutherland K, Cistulli PA. Recent advances in obstructive sleep apnea pathophysiology and treatment. Sleep Biol Rhythms. 2015;13(1):26–40.
Tsai WH, Vazquez JC, Oshima T, et al. Remotely controlled mandibular positioner predicts efficacy of oral appliances in sleep apnea. Am J Respir Crit Care Med. 2004;170(4):366–70. Epub 2004/04/24. (Article in eng).
Tsuda H, Almeida FR, Tsuda T, et al. Craniofacial changes after 2 years of nasal continuous positive airway pressure use in patients with obstructive sleep apnea. Chest. 2010c;138(4):870–4.
Tsuda H, Ohmaru T, Higuchi Y. Requirement for sleep medicine education in Japanese pre‐doctoral dental curriculum. Sleep Biol Rhythms. 2014;12(4):232–4.
Tsuda H, Almeida FR, Walton JN, Lowe AA. Questionnaire-based study on sleep-disordered breathing among edentulous subjects in a university oral health center. Int J Prosthodont. 2010;23(6):503–6.
Tsuiki S, Kobayashi M, Namba K, et al. Optimal positive airway pressure predicts oral appliance response to sleep apnoea. Eur Respir J. 2010;35(5):1098–105.
Vanderveken OM, Devolder A, Marklund M, et al. Comparison of a custom-made and a thermoplastic oral appliance for the treatment of mild sleep apnea. Am J Respir Crit Care Med. 2008;178(2):197–202. Epub 2007/08/04. (Article in eng).
Vanderveken OM, Dieltjens M, Wouters K, et al. Objective measurement of compliance during oral appliance therapy for sleep-disordered breathing. Thorax. 2013;68(1):91–6. Pubmed Central PMCID: 3534260.
Vroegop AV, Vanderveken OM, Dieltjens M, et al. Sleep endoscopy with simulation bite for prediction of oral appliance treatment outcome. J Sleep Res. 2013;22(3):348–55.
Vroegop AV, Vanderveken OM, Boudewyns AN, et al. Drug-induced sleep endoscopy in sleep-disordered breathing: report on 1,249 cases. Laryngoscope. 2014;124(3):797–802.
Woelfel JB, Igarashi T, Dong JK. Faculty-supervised measurements of the face and of mandibular movements on young adults. J Adv Prosthodont. 2014;6(6):483–90. Pubmed Central PMCID: 4279047.
Young T, Palta M, Dempsey J, et al. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230–5. Epub 1993/04/29. (Article in eng).
Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165(9):1217–39.
Zhou J, Liu YH. A randomised titrated crossover study comparing two oral appliances in the treatment for mild to moderate obstructive sleep apnoea/hypopnoea syndrome. J Oral Rehabil. 2012;39(12):914–22.
Acknowledgements
None.
Funding
Not applicable.
Availability of data and materials
Not applicable.
Authors’ contributions
HT interpreted the articles and was a major contributor in writing the manuscript. HT, NW, and SA read and approved the final manuscript.
Competing interests
HT and NW declare that they have no competing interest. SA has unrestricted research funding from Teijin Home Health Company and Philips Respironics Inc.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tsuda, H., Wada, N. & Ando, Si. Practical considerations for effective oral appliance use in the treatment of obstructive sleep apnea: a clinical review. Sleep Science Practice 1, 12 (2017). https://doi.org/10.1186/s41606-017-0013-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41606-017-0013-8