Abstract
Background
Polypharmacy is one of the most important health issues for its potential impacts on disease burden and healthcare costs. The aim of this study was to update a comprehensive picture of prevalence and trends in polypharmacy over 20 years in U.S. adults.
Methods
Participants included 55,081 adults aged ≥ 20 from the National Health and Nutrition Examination Survey, January 1, 1999, through December 31, 2018. The simultaneously use of ≥ 5 drugs in one individual was defined as polypharmacy. National prevalence and trends in polypharmacy were evaluated among U.S. adults within different demo-socioeconomic status and pre-existing diseases.
Results
From 1999–2000 to 2017–2018, the overall percentages of adults with polypharmacy remained on the rise, increasing from 8.2% (7.2–9.2%) to 17.1% (15.7–18.5%) (average annual percentage change [AAPC] = 2.9%, P = .001). The polypharmacy prevalence was considerably higher in the elderly (from 23.5% to 44.1%), in adults with heart disease (from 40.6% to 61.7%), and in adults with diabetes (from 36.3% to 57.7%). Also, we observed a greater increase rate of polypharmacy in men (AAPC = 4.1%, P < .001), in the Mexican American (AAPC = 6.3%, P < .001), and in the non-Hispanic Black (AAPC = 4.4%, P < .001).
Conclusions
From 1999–2000 to 2017–2018, the prevalence of polypharmacy is continually increasing in U.S. adults. The polypharmacy was especially higher in the older, in patients with heart disease, or diabetes. The high prevalence urges the healthcare providers and health policymakers to manage polypharmacy among specific population groups.
Similar content being viewed by others
Background
Polypharmacy is often commonly defined as the simultaneous use of five or more prescription drugs by one individual. Over the past two decades, it has been observed significant increases in overall prescription drug use and polypharmacy, probably due to large-scale policy changes caused by the introduction of new drugs, research on drug side effects and interactions, or the growing need for treatment of complications [1]. In U.S., it was reported that the prevalence of polypharmacy increased from 8.2% in 1999–2000 to 15% in 2011–2012 [1]. Furthermore, the proportion of polypharmacy among adults aged 65 and older tripled from 12.8% to 39.0% between 1988 and 2010 [2]. A recent meta-analysis reported the pooled polypharmacy prevalence was 37% among individuals over aged 19 [3]. Summarized by another review, the prevalence of polypharmacy varied from 10% to as high as nearly 90% in different populations [4]. Polypharmacy can be a major issue related to prescribed medications, which has become one of the most important but underappreciated health concerns.
Although the use of multiple medications may treat symptoms, prevent disease complications, or increase life expectancy, the majority of research suggests that polypharmacy is associated with negative clinical consequences, including nonadherence to treatment, adverse drug events (e.g., falls, fractures, renal failure), drug-drug interactions, and hospitalizations [5, 6]. Polypharmacy is also linked to increased risks of disability, cognitive decline, and even mortality [7, 8]. In addition, polypharmacy is ordinary among individuals with multimorbidity and an excess of unplanned hospitalizations is seen in those with higher levels of polypharmacy, leading to higher costs of care for individuals and health care systems [9]. Besides, health care tends to be segmented without shared records, as a result, patients with multimorbidity who visit to multiple providers might be prescribed duplicative or interacting treatments [10]. It was estimated that polypharmacy cost at least $50 billion annually from U.S. health plans in 2002, accounting for a large proportion of pharmaceutical expenditure [11].
The substantial increases in prescription medication use and polypharmacy were distinguished particularly in developed countries [12, 13]. However, current guidelines fail to provide adequate information on dosing schedules for people simultaneously using multiple medications, and it was observed that people with polypharmacy may have a higher risk of potentially inappropriate medication use in these developed countries [14]. It is important to have a better understanding of polypharmacy by taking an undated and comprehensive estimation of its prevalence and trend. By using the U.S. as a model case, the aim of this study was to update the national prevalence and trends in polypharmacy among U.S. adults with different demo-socioeconomic status and pre-existing diseases.
Methods
Study population
Data for this study were obtained from National Health and Nutrition Examination Survey (NHANES), a study conducted in all 50 states and the District of Columbia by using a complex multi-stage probability sampling method to investigate the health status of the U.S. population. NHANES collected participants’ demographic information, dietary data, examination data, lifestyles, health conditions and biochemical indexes by self-administrated questionnaires, physical examinations, and laboratory tests. All survey participants were eligible.
Data are publicly available at https://www.cdc.gov/nchs/nhanes/index.htm. NHANES has been approved by the Institutional Review Board of the National Center for Health Statistics. All participants have signed informed consent forms.
In this study, ten cycles of 1999–2000, 2001–2002, 2003–2004, 2005–2006, 2007–2008, 2009–2010, 2011–2012, 2013–2014, 2015–2016, and 2017–2018 were included, with a total of 101,316 individuals. We excluded those younger than 20 years, as well as those with incomplete information on polypharmacy. Finally, 55,081 individuals were included in this analysis.
Assessment of polypharmacy
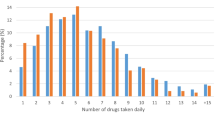
During the household interview, participants were asked about if they needed any prescriptions by the question: “Have you taken any prescription medicines in the past month?”. Individuals who answered “yes” were asked to show the drug containers for all products used. Meanwhile, the interviewer recorded the number and names of prescription medicines reported.
Statistical analysis
The prevalence of polypharmacy, defined as simultaneous use of 5 or more drugs, was calculated within every 2-year cycle in NHANES. Survey-weighted regression models were used to estimate the rate of polypharmacy. Since the observed trends might be affected by changes in the age-distribution of the whole population, we also conducted age-adjusted analyses to show the age-standardized polypharmacy rate according to the US 2000 Standard Population (based on 5-year age groups, up to 80 years+). Joinpoint analyses were used to identify points of inflection and calculate the average annual percentage change (AAPC) before and after the inflection points [15].
Subgroup analyses were also conducted to reveal the potential heterogeneity in population with different demo-socioeconomic status and pre-existing diseases. We stratified participants by sex (men and women), age (20–39 years, 40–64 years and ≥ 65 years), race (Mexican American, other Hispanic, non-Hispanic White, non-Hispanic Black, and other race—including Multi-Racial), education (high school or below, and college or above), and income (indicated by family income-to-poverty ratio [PIR], where PIR ≤ 1.0 was regarded as poverty). In addition, we also investigated the polypharmacy in participants with specific category of diseases. The self-administrated questionnaires in NHANES provide a broad range of health conditions via in-home personal interviews, including hypertension, high-cholesterol (hypercholesterolemia), diabetes, heart disease (congestive heart failure, coronary heart disease, angina/angina pectoris, or heart attack), respiratory disease (asthma, emphysema, or chronic bronchitis), and cancer. For example, in terms of cancer, participants were asked by the survey questions of “Have you ever been told by a doctor or other health professional that you had had cancer or a malignancy of any kind?”. All analyses were conducted by SAS 9.4 (TS Level 1M6).
Results
Table 1 shows the prevalence of the participants with polypharmacy in all years, year of 1999–2000, and year of 2017–2018, stratified by population characteristics. During the overall period, a higher prevalence of polypharmacy was observed in women, in the elderly, in the Non-Hispanic White, in adults with education level at high school or below, in adults with heart disease. Similar patterns were observed in the year of 1999–2000 and 2017–2018.
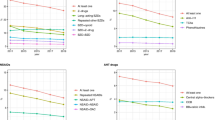
From 1999–2000 to 2017–2018, the overall percentages of adults with polypharmacy remained on the rise, increasing from 8.2% (95% CI 7.2 to 9.2) to 17.1% (95% CI 15.7 to 18.5) (AAPC = 2.9%, P = 0.001, Fig. 1). This pattern remained unchanged with age-adjustment model (Additional file 1: Fig. S2). Furthermore, similar trends were observed in subgroup analyses. In the sex-stratified analysis, the prevalence of polypharmacy was consistently higher in women than in men. From 1999–2000 to 2017–2018, the prevalence of polypharmacy increased from 10.4% (95% CI 9.0 to 11.8) to 17.8% (95% CI 15.8 to 19.8) and increased from 5.8% (95% CI 4.8 to 6.8) to 16.3% (95% CI 14.1 to 18.5) in women and men, respectively (Fig. 2A). However, the AAPC was relatively higher in men (4.1%, P < 0.001) than that in women (2.4%, P = 0.006). In the age-stratified analysis, the polypharmacy prevalence was consistently higher in participants aged 65 years and older than that in the 40–64 years group and simultaneously higher than in the 20–39 years group. Between 1999–2000 and 2017–2018, the prevalence increased from 23.5% (95% CI 20.6 to 26.4) to 44.1% (95% CI 40.4 to 47.8) in the 65 years and older group, while it increased from 10.4% (95% CI 8.6 to 12.2) to 15.8% (95% CI 13.4 to 18.2) and from 0.7% (95% CI 0.1 to 1.3) to 3.4% (95% CI 2.2 to 4.6) in the 40–64 years and 20–39 years groups, respectively (Fig. 2B). The AAPCs ranged between 2.1 to 2.9 and did not differ much across age groups. In the race-stratified analysis, the non-Hispanic White consistently had the highest prevalence during the observation period, rising from 9.2% (95% CI 8.0 to 10.4) to 20.0% (95% CI 17.8 to 22.2). This was followed by the non-Hispanic Black, which increased from 7.3% (95% CI 5.7 to 8.9) to 16.2% (95% CI 14.2 to 18.2). Mexican Americans had the lowest prevalence rate, with the prevalence rising from 2.6% (95% CI 1.8 to 3.4) to 8.7% (95% CI 6.5 to 10.9) (Fig. 2C). However, the AAPCs were higher in the Mexican American (6.3%, P < 0.001) and in the non-Hispanic Black (4.4%, P < 0.001) than that in other races.
Grouped by different levels of education, the prevalence of polypharmacy was consistently higher in adults with low education (high school or below) than in those with high education (college or above). Among adults with education at the high school level or below, the polypharmacy prevalence increased from 10.0% (95% CI 8.6 to 11.4) to 18.9% (95% CI 16.7 to 21.1) from 1999–2000 to 2017–2018, while among those with education at the university level or above it increased from 6.4% (95% CI 5.2 to 7.6) to 15.9% (95% CI 13.9 to 17.9) (Fig. 3A). As for the level of poverty, there was no apparent difference in polypharmacy prevalence between populations below or above the poverty level (Fig. 3B).
In addition, according to participants self-reporting whether they had a certain disease diagnosed by a doctor, we divided the participants into six groups by suffering from hypertension, high-cholesterol, diabetes, heart disease, respiratory diseases, and cancer. From 1999–2000 to 2017–2018, it was observed that patients with heart disease had the highest prevalence of polypharmacy, rising from 40.6% (95% CI 34.5 to 46.7) to 61.7% (95% CI 55.2 to 68.2). The prevalence of polypharmacy was also considerably high among adults with diabetes, which rose from 36.3% (95% CI 30.2 to 42.4) to 57.7% (95% CI 52.4 to 63.0). The polypharmacy prevalence among those with high-cholesterol and respiratory diseases was relatively low. Among adults with respiratory diseases, the prevalence increased from 17.7% (95% CI 14.4 to 21.0) to 28.2% (95% CI 24.5 to 31.9) (Fig. 4). The AAPCs ranged between 1.2% (heart disease) to 2.7% (cancer).
Discussion
From 1999–2000 to 2017–2018, there was an overall increasing trend in the prevalence of polypharmacy in U.S. adults, from 8.2% to 17.1%, with an AAPC of 2.9%. The polypharmacy prevalence was considerably higher in the elderly, in adults with heart disease, and in adults with diabetes. Also, we observed a greater increase rate of polypharmacy in men, in the Mexican American, and in the non-Hispanic Black.
The prevalence of polypharmacy has increased over the past several decades, during which several clinical guidelines such as Beers Criteria [16], the STOPP/START criteria [17], and the European Union SIMPATHY project [18] have been published for safe medication use and polypharmacy management. In this present study, we found the large increases in 1999–2003 that then plateaued, particularly for the older adults, which might be partially explained by the publication of the updated Beers list for older adults in 2003. A previous study also supported that the proportion of persons on a potentially inappropriate medication has decreased since the updated Beers criteria in 2003 [2]. Nevertheless, the highest polypharmacy was still detected in the elder population, with reported prevalence ranging from 26 to 44% [19,20,21]. Particularly, in older adults with frailty, the overall prevalence of polypharmacy and hyper-polypharmacy (the concurrent use of ten or more medications) was 59% and 22%, respectively [22]. Compared to people without polypharmacy, polypharmacy was inclined to accelerate frailty states progression, leading to adverse clinical outcomes and a higher risk of mortality in older patients with frailty [22]. Our recent study also found that polypharmacy was associated with increased risks of all-cause and cardiovascular mortality among the elderly chronic kidney disease patients [8]. In real-world clinical settings, the majority of older adults suffered from multimorbidity and polypharmacy, though the use of multiple medications may treat symptoms effectively for multimorbidity, it is crucial to explore the clinical trajectories of individuals by focusing on the dynamics and complexities of multimorbidity and polypharmacy [23, 24].
Consistent with the literature, this research found that women were more likely to have polypharmacy than men [23, 25]. This may be partially interpreted by the longer life expectancy and longer years with multimorbidity in women. Also, women are more likely to be influenced by psychiatric and social factors, leading to higher symptoms perception and health-seeking behaviors [26, 27]. However, a greater increase rate of polypharmacy in men needs further attention. In addition, previous research has established that there exist racial and ethnic disparities in prescription drug use. For example, data from the Medical Expenditure Panel Survey showed non-Hispanic whites were more likely to have access to new medications than non-Hispanic blacks and Hispanic whites [28], which was similar to our results that polypharmacy reached the highest level in non-Hispanic whites. Factors associated with racial disparities in medication use have been explored in several studies. Minorities might be less inclined to attempt new drugs, delay health-seeking behaviors, or enroll fewer health care services [29].
This present study found the highest prevalence of polypharmacy in individuals with heart disease. Heart disease is the leading cause of disability and death in the U.S., and its prevalence is still on the rise [30, 31]. Recent guidelines for the treatment of cardiovascular disease recommend the use of multiple medications to prevent complications or reduce mortality [32]. However, this is also accompanied by potential problems such as poor adherence, adverse drug reactions, hospitalizations, higher mortality burden, and substantial healthcare cost [33]. A prior study reported polypharmacy prevalence was high among people with heart failure, ranging from 17.2% to 99% [34], as well as among people with type 2 diabetes, varying from 57 to 99% [35]. Many recommendations to manage polypharmacy in people with cardiovascular diseases or diabetes have been gradually proposed in order to strike a balance between unnecessary medications and effective treatments [36, 37]. For example, patients with heart disease could have many comorbid conditions, which could be a main cause of high polypharmacy, therefore, certain particular drug class could be prioritized to treat multiple conditions [37]. Besides, new support tools have been gradually developed for patients with chronic disease to support physicians in deprescribing [38, 39].
By using nationally representative data, we provided an update prevalence and trend of polypharmacy over a 20-year period in the U.S. adults. The subgroup analyses also offered a more comprehensive picture to investigate the polypharmacy across people subgroups including sex, age, race, socioeconomic status, and pre-existing disease. Furthermore, the medication information was collected by using standard methods, and the interviewer could check the medication containers during the household interview. Data were also routinely examined for quality assurance and quality control. However, several limitations should be addressed. First, although we used sampling weights to calculate the prevalence, the non-response bias could still occur. Second, we only accessed the number of drug prescription, but the specific categories of drugs and the duration of drug use were not analyzed. Besides, data from NHANES failed to include prescriptions over the counter or herbal supplements and pro re nata (PRN) medications, potentially contributing to an underestimation of polypharmacy rates. Finally, the diseases were self-reported by participants, which might result in measurement errors and misclassification. However, previous studies have proved high validity of clinical records in NHANES [40, 41].
Conclusions
From 1999–2000 to 2017–2018, the prevalence of polypharmacy was continually increasing in U.S. adults. The polypharmacy was especially higher in the elder, in patients with heart disease, and in patients with diabetes. The high prevalence urges the healthcare providers and health policymakers to develop and implement measures targeted at polypharmacy among specific population groups, which might be of great potential significance to the delivery of appropriate and safe medication.
Availability of data and materials
The data involved in this study are freely available from https://www.cdc.gov/nchs/nhanes/index.htm.
Abbreviations
- AAPC:
-
Average annual percentage change
- NHANES:
-
National Health and Nutrition Examination Survey
References
Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in prescription drug use among adults in the United States From 1999–2012. JAMA. 2015;314:1818–31.
Charlesworth CJ, Smit E, Lee DS, Alramadhan F, Odden MC. Polypharmacy among adults aged 65 years and older in the United States: 1988–2010. J Gerontol A Biol Sci Med Sci. 2015;70:989–95.
Delara M, Murray L, Jafari B, Bahji A, Goodarzi Z, Kirkham J, Chowdhury Z, Seitz DP. Prevalence and factors associated with polypharmacy: a systematic review and Meta-analysis. BMC Geriatr. 2022;22:601.
Khezrian M, McNeil CJ, Murray AD, Myint PK. An overview of prevalence, determinants and health outcomes of polypharmacy. Ther Adv Drug Saf. 2020;11:2042098620933741.
Onder G, Marengoni A. Polypharmacy. JAMA. 2017;318:1728.
Davies LE, Spiers G, Kingston A, Todd A, Adamson J, Hanratty B. Adverse outcomes of polypharmacy in older people: systematic review of reviews. J Am Med Dir Assoc. 2020;21:181–7.
Wastesson JW, Morin L, Tan ECK, Johnell K. An update on the clinical consequences of polypharmacy in older adults: a narrative review. Expert Opin Drug Saf. 2018;17:1185–96.
Wang X, Yang C, Jiang J, Hu Y, Hao Y, Dong JY. Polypharmacy, chronic kidney disease, and mortality among older adults: a prospective study of National Health and nutrition examination survey, 1999–2018. Front Public Health. 2023;11:1116583.
Rozsnyai Z, Jungo KT, Reeve E, Poortvliet RKE, Rodondi N, Gussekloo J, Streit S. What do older adults with multimorbidity and polypharmacy think about deprescribing? The LESS study—a primary care-based survey. BMC Geriatr. 2020;20:435.
Hoel RW, Giddings Connolly RM, Takahashi PY. Polypharmacy management in older patients. Mayo Clin Proc. 2021;96:242–56.
Moriarty F, Hardy C, Bennett K, Smith SM, Fahey T. Trends and interaction of polypharmacy and potentially inappropriate prescribing in primary care over 15 years in Ireland: a repeated cross-sectional study. BMJ Open. 2015;5:e008656.
Bhagavathula AS, Gebreyohannes EA, Fialova D. Prevalence of polypharmacy and risks of potentially inappropriate medication use in the older population in a developing country: a systematic review and meta-analysis. Gerontology. 2022;68:136–45.
Fialova D, Topinkova E, Gambassi G, Finne-Soveri H, Jonsson PV, Carpenter I, Schroll M, Onder G, Sorbye LW, Wagner C, Reissigova J, Bernabei R and Ad HOCPRG. Potentially inappropriate medication use among elderly home care patients in Europe. JAMA. 2005;293:1348–58.
Fialova D, Laffon B, Marinkovic V, Tasic L, Doro P, Somicronos G, Mota J, Dogan S, Brkic J, Teixeira JP, Valdiglesias V, Costa S, project EH and IS WGbgHcsfhaotECA. Medication use in older patients and age-blind approach: narrative literature review (insufficient evidence on the efficacy and safety of drugs in older age, frequent use of PIMs and polypharmacy, and underuse of highly beneficial nonpharmacological strategies). Eur J Clin Pharmacol. 2019;75:451–466.
Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK. Estimating average annual per cent change in trend analysis. Stat Med. 2009;28:3670–82.
By the American Geriatrics Society Beers Criteria Update Expert P. American Geriatrics Society 2019 Updated AGS Beers Criteria(R) for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019;67:674–694.
de Groot DA, de Vries M, Joling KJ, van Campen JP, Hugtenburg JG, van Marum RJ, Vermeulen Windsant van den Tweel AM, Elders PJ, van Hout HP. Specifying ICD9, ICPC and ATC codes for the STOPP/START criteria: a multidisciplinary consensus panel. Age Ageing. 2014;43:773–8.
Mair A, Fernandez-Llimos F and Consortium S. Polypharmacy management programmes: the SIMPATHY Project. Eur J Hosp Pharm. 2017;24:5–6.
Page AT, Falster MO, Litchfield M, Pearson SA, Etherton-Beer C. Polypharmacy among older Australians, 2006–2017: a population-based study. Med J Aust. 2019;211:71–5.
Guthrie B, Makubate B, Hernandez-Santiago V, Dreischulte T. The rising tide of polypharmacy and drug–drug interactions: population database analysis 1995–2010. BMC Med. 2015;13:74.
Cho HJ, Chae J, Yoon SH, Kim DS. Aging and the prevalence of polypharmacy and hyper-polypharmacy among older adults in South Korea: a national retrospective study during 2010–2019. Front Pharmacol. 2022;13:866318.
Toh JJY, Zhang H, Soh YY, Zhang Z, Wu XV. Prevalence and health outcomes of polypharmacy and hyperpolypharmacy in older adults with frailty: a systematic review and meta-analysis. Ageing Res Rev. 2023;83:101811.
Vos R, Boesten J, van den Akker M. Fifteen-year trajectories of multimorbidity and polypharmacy in Dutch primary care—a longitudinal analysis of age and sex patterns. PLoS ONE. 2022;17:e0264343.
Lai SW, Liao KF, Lin CL, Lin CC, Lin CH. Longitudinal data of multimorbidity and polypharmacy in older adults in Taiwan from 2000 to 2013. Biomedicine (Taipei). 2020;10:1–4.
Rochon PA, Petrovic M, Cherubini A, Onder G, O’Mahony D, Sternberg SA, Stall NM, Gurwitz JH. Polypharmacy, inappropriate prescribing, and deprescribing in older people: through a sex and gender lens. Lancet Healthy Longev. 2021;2:e290–300.
Mauvais-Jarvis F, Bairey Merz N, Barnes PJ, Brinton RD, Carrero JJ, DeMeo DL, De Vries GJ, Epperson CN, Govindan R, Klein SL, Lonardo A, Maki PM, McCullough LD, Regitz-Zagrosek V, Regensteiner JG, Rubin JB, Sandberg K, Suzuki A. Sex and gender: modifiers of health, disease, and medicine. Lancet. 2020;396:565–82.
Gijsbers van Wijk CM, Kolk AM, van den Bosch WJ, van Hoogen HJ. Male and female morbidity in general practice: the nature of sex differences. Soc Sci Med. 1992;35:665–78.
Wang J, Noel JM, Zuckerman IH, Miller NA, Shaya FT, Mullins CD. Disparities in access to essential new prescription drugs between non-Hispanic whites, non-Hispanic blacks, and Hispanic whites. Med Care Res Rev. 2006;63:742–63.
Wallace J, Lollo A, Duchowny KA, Lavallee M, Ndumele CD. Disparities in Health Care Spending and Utilization Among Black and White Medicaid Enrollees. JAMA Health Forum. 2022;3:e221398.
Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1211–59.
Collaborators GBDCoD. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–88.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy JW, Michos ED, Miedema MD, Munoz D, Smith SC Jr, Virani SS, Williams KA Sr, Yeboah J, Ziaeian B. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:e596–646.
Tamargo J, Kjeldsen KP, Delpon E, Semb AG, Cerbai E, Dobrev D, Savarese G, Sulzgruber P, Rosano G, Borghi C, Wassman S, Torp-Pedersen CT, Agewall S, Drexel H, Baumgartner I, Lewis B, Ceconi C, Kaski JC, Niessner A. Facing the challenge of polypharmacy when prescribing for older people with cardiovascular disease. A review by the European Society of Cardiology Working Group on Cardiovascular Pharmacotherapy. Eur Heart J Cardiovasc Pharmacother. 2022;8:406–19.
Beezer J, Al Hatrushi M, Husband A, Kurdi A, Forsyth P. Polypharmacy definition and prevalence in heart failure: a systematic review. Heart Fail Rev. 2022;27:465–92.
van Oort S, Rutters F, Warle-van Herwaarden MF, Schram MT, Stehouwer CD, Tack CJ, Abbink EJ, Wolffenbuttel BH, van der Klauw MM, DeVries JH, Siegelaar SE, Sijbrands EJ, Ozcan B, de Valk HW, Silvius B, Schroijen MA, Jazet IM, van Ballegooijen AJ, Beulens JWJ, Elders PJ, Kramers C and Diabetes Pearl from the Parelsnoer I. Characteristics associated with polypharmacy in people with type 2 diabetes: the Dutch Diabetes Pearl cohort. Diabet Med. 2021;38:e14406.
Disdier Moulder MPA, Hendricks AK, Ou NN. Towards appropriate polypharmacy in older cardiovascular patients: How many medications do I have to take? Clin Cardiol. 2020;43:137–44.
Bhatt AS, Choudhry NK. Evidence-based prescribing and polypharmacy for patients with heart failure. Ann Intern Med. 2021;174:1165–6.
Rieckert A, Reeves D, Altiner A, Drewelow E, Esmail A, Flamm M, Hann M, Johansson T, Klaassen-Mielke R, Kunnamo I, Loffler C, Piccoliori G, Sommerauer C, Trampisch US, Vogele A, Woodham A, Sonnichsen A. Use of an electronic decision support tool to reduce polypharmacy in elderly people with chronic diseases: cluster randomised controlled trial. BMJ. 2020;369:m1822.
Turk A, Wong G, Mahtani KR, Maden M, Hill R, Ranson E, Wallace E, Krska J, Mangin D, Byng R, Lasserson D, Reeve J. Optimising a person-centred approach to stopping medicines in older people with multimorbidity and polypharmacy using the DExTruS framework: a realist review. BMC Med. 2022;20:297.
Rethy L, Petito LC, Vu THT, Kershaw K, Mehta R, Shah NS, Carnethon MR, Yancy CW, Lloyd-Jones DM, Khan SS. Trends in the prevalence of self-reported heart failure by race/ethnicity and age from 2001 to 2016. JAMA Cardiol. 2020;5:1425–9.
Cheng YJ, Kanaya AM, Araneta MRG, Saydah SH, Kahn HS, Gregg EW, Fujimoto WY, Imperatore G. Prevalence of diabetes by race and ethnicity in the United States, 2011–2016. JAMA. 2019;322:2389–98.
Acknowledgements
The authors would like to thank the NHANES research group. The developers and funders of NHANES had no roles in data analysis and interpretation or manuscript writing.
Funding
This work was supported by the National key research and development program of China (grant number 2022YFC3600804 to Y. Hao); China Postdoctoral Science Foundation (grant number 2023M730113 to X. Wang).
Author information
Authors and Affiliations
Contributions
XW: Conceptualization, Formal analysis, Data curation, Writing- Original draft preparation. J-YD: Conceptualization, Formal analysis, Writing- Reviewing and Editing. KL: Data curation, Writing- Reviewing and Editing. SK: Writing- Reviewing and Editing. CT: Writing- Reviewing and Editing. YW: Writing- Reviewing and Editing. YH: Supervision, Validation, Writing- Reviewing and Editing. YH: Validation, Writing- Reviewing and Editing. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The NHANES has been approved by the Institutional Review Board of the National Center for Health Statistics. All participants have signed informed consent forms.
Consent for publication
Not applicable.
Competing interests
No potential conflicts of interest relevant to this article were reported.
Supplementary Information
Additional file 1: Fig. S1
. Results of Joinpoint trend analysis for polypharmacy among U.S. adults, 1999-2018. Fig. S2. Results of age-adjusted* Joinpoint trend analysis for polypharmacy among U.S. adults, 1999-2018. Table S1. The average annual percent change (AAPC) estimates based on Joinpoint Analyses for polypharmacy among U.S. adults, 1999-2018
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, X., Liu, K., Shirai, K. et al. Prevalence and trends of polypharmacy in U.S. adults, 1999–2018. glob health res policy 8, 25 (2023). https://doi.org/10.1186/s41256-023-00311-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41256-023-00311-4