Abstract
Background
Medical three-dimensional (3D) printing has demonstrated utility and value in anatomic models for vascular conditions. A writing group composed of the Radiological Society of North America (RSNA) Special Interest Group on 3D Printing (3DPSIG) provides appropriateness recommendations for vascular 3D printing indications.
Methods
A structured literature search was conducted to identify all relevant articles using 3D printing technology associated with vascular indications. Each study was vetted by the authors and strength of evidence was assessed according to published appropriateness ratings.
Results
Evidence-based recommendations for when 3D printing is appropriate are provided for the following areas: aneurysm, dissection, extremity vascular disease, other arterial diseases, acute venous thromboembolic disease, venous disorders, lymphedema, congenital vascular malformations, vascular trauma, vascular tumors, visceral vasculature for surgical planning, dialysis access, vascular research/development and modeling, and other vasculopathy. Recommendations are provided in accordance with strength of evidence of publications corresponding to each vascular condition combined with expert opinion from members of the 3DPSIG.
Conclusion
This consensus appropriateness ratings document, created by the members of the 3DPSIG, provides an updated reference for clinical standards of 3D printing for the care of patients with vascular conditions.
Similar content being viewed by others
Background
In 2018, the Radiological Society of North America (RSNA) Special Interest Group on Three-Dimensional Printing (3DPSIG) published appropriateness ratings for medical 3D printing and appropriateness for certain clinical scenarios including congenital heart disease, craniomaxillofacial pathologies, genitourinary pathologies, musculoskeletal pathologies, vascular pathologies, and breast pathologies [1]. Since then, there has been an expansion in the use of 3D printing to plan for vascular intervention, as well as more clinical reports. The purpose of this document is to update the clinical indications for 3D printing of vascular pathologies, and then vet, vote, and publish recommendations on their appropriateness.
Methods
The 3DPSIG identified clinical situations for 3D printing of vascular conditions, and then provided recommendations for when 3D printing is considered usually appropriate, maybe appropriate, and rarely appropriate [2]. Strength of evidence was determined by literature review. The 3DPSIG Guidelines Chairperson managed the ratings of this document via a vote among 3DPSIG members. The results of the ratings follow the established 1–9 format (with 9 being the most appropriate):
-
1–3, red, rarely appropriate: There is a lack of a clear benefit or experience that shows an advantage over usual practice.
-
4–6, yellow, may be appropriate: There may be times when there is an advantage, but the data is lacking, or the benefits have not been fully defined.
-
7–9, green, usually appropriate: Data and experience shows an advantage to 3D printing as a method to represent and/or extend the value of data contained in the medical imaging examination.
Clinical scenarios were organized using standard categories of patients with vascular conditions [3]. A major treatise in vascular interventions served as a guide for search terms (Appendix 1), to ensure an exhaustive search [4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122]. Afterwards, an English language PubMed literature search through January 2022 and an appropriateness ratings document using standard categories for assessment were created. The supporting evidence was obtained through structured PubMed searches. From each search result, the relevant articles written in English were curated by consensus between physicians with expertise in 3D printing and vascular pathologies. Publications were deemed ineligible if they solely focused on bioprinting, virtual or augmented reality, or were review articles without new patient data. Neurovascular pathologies were excluded. All final included literature [4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122] and recommendations of this section were vetted and approved by vote of 3DPSIG members virtually at the July 20, 2022 3DPSIG Appropriateness Committee Meeting. Afterwards, the ratings and associated literature were posted on the 3DPSIG’s members-only online forum and comments could be made by 3DPSIG members for a 2-week period. All included studies were graded with a strength of evidence assessment, using as a methodology the assignment used by the American College of Radiology [2]. The paper represents the findings and conclusions of the 3DPSIG and does not represent an endorsement by the Radiological Society of North America (RSNA).
Results
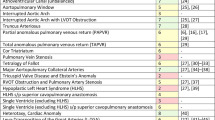
Table 1 provides evidence-based appropriateness ratings, supplemented by expert opinion when there was a paucity of peer-review data, to define and support the use of 3D printing for patients undergoing vascular intervention. The citations included in forming the appropriateness recommendations and the strength of evidence assessment are presented in Appendices 1 and 2 respectively.
Discussion
Aneurysms/dissection - central
Acute aortic syndrome includes patients who symptomatically present with chest or back pain, malignant hypertension, or hemodynamic instability. The most common specific diagnoses are aortic dissection, intramural hematoma, and unstable penetrating atherosclerotic ulcers. There are three general management option: open repair, endovascular treatment, or medical management with close imaging follow up. The literature supports 3D printing for intervention. The largest body of literature focuses on the management of aneurysms [4,5,6, 11,12,13,14,15, 19, 20, 24, 31, 33, 35, 37, 39,40,41,42, 45, 48, 49, 51,52,53], especially involving the abdominal aorta. There is additional literature on aortic dissection [58, 60, 61] and penetrating atherosclerotic ulcer. [65].
Extremity Vascular Disease.
Peripheral artery disease is common and presents with claudication. Patients are worked up with noninvasive studies and then imaging, the latter of which requires 3D visualization [123, 124]. Vascular intervention includes either percutaneous therapy or bypass. However, 3D printing to date has not been significantly involved in management. There are two studies where lower extremity anatomic models were used for surgical training or post-surgical assessment of alternative access or intervention [66, 67].
Acute venous thromboembolic disease
Deep venous thrombosis and pulmonary embolism are common conditions where the diagnosis is typically confirmed by imaging. Treatment is most often medical (via anticoagulation), while some patients require more invasive therapies such as directed anticoagulation or thrombectomy. Patient-specific 3D printed anatomic models do not currently have a central role in managing most patients with these conditions. Our literature search yielded one study that demonstrated feasibility. In it, a 3D printed pulmonary arterial system was used to study flow dynamics during pulmonary angiography protocols, but the anatomic model was not used in patient care [68].
Venous disorders
Venous disorders is a general term that includes chronic venous insufficiency, phlebitis, or varicose veins that typically cause lower extremity swelling and discomfort for patients. These are often managed medically and through lifestyle modifications, but can also be treated with minimally invasive endovascular interventions, e.g. radiofrequency vein ablation. 3D printed anatomic models do not appear in the literature, apart from patient-specific 3D printed extravascular stents to treat Nutcracker Syndrome [69,70,71].
Lymphedema
Lymphedema presents with swelling, and in severe cases, restricted range of motion. Treatment is often conservative symptom management. One study developed a 3D printed lymphedema phantom for ultrasound tests, but it was not used in patient care [72].
Congenital vascular malformations
Congenital vascular malformations have great variability in their presentation. The literature supports patient-specific 3D printed anatomic models for pre-intervention planning for Kommel’s diverticulum [73], double aortic arch [75, 78], and type II Abernathy malformation [77].
Vascular trauma
Injury to local vascular structures can occur due to blunt or penetrating forces. Endovascular interventions can optimize treatment of such injury through minimally invasive approaches. At this time, no studies have been performed suggesting the utility of 3D printing in such cases.
Vascular tumor
Resection of vascular tumors can be complicated when in anatomically sensitive locations or with extensive tissue involvement of the tumor. There is a single case series that used anatomic 3D printed models to retrospectively determine surgical margins of pulmonary artery sarcoma resections [81].
Miscellaneous
Kidney failure leads to dialysis. Access via an arteriovenous fistula requires either open surgery or an endovascular approach. While there is no literature for pre-procedure patient-specific 3D printed anatomic models, one study used 3D printing for arteriovenous fistula surveillance post-operatively [82].
Vascular R&D and modeling
Research and development in vascular surgery is continuously growing, especially in 3D printing applications. There are numerous pre-clinical studies detailing the involvement of 3D printing of stents and grafts, as well as modeling of vascular structure or flow dynamics [83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117].
Vasculopathy, other
Atherosclerosis can impact vascular flow dynamics due to stenosis and impact patient outcomes. Several studies have used 3D printing to simulate these structural changes in a pre-clinical setting [118,119,120,121,122].
Inflammation of the vascular structures, or vasculitis, is a broad disease category, and 3D printed anatomic models have not been published in the management of vasculitis patients.
Conclusion
This document updates clinical appropriateness for 3D printing for patients with vascular conditions. Adoption of common clinical standards regarding appropriate use, information and material management, and quality control are needed to ensure the greatest possible clinical benefit from 3D printing. With accruing evidence for utility and value in 3D printing, it is anticipated that this consensus appropriateness ratings document, created by the members of the 3DPSIG, will provide information that can be used for future clinical standards of 3D printing.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Chepelev L, et al. Radiological Society of North America (RSNA) 3D printing Special Interest Group (SIG): guidelines for medical 3D printing and appropriateness for clinical scenarios. 3D Print Med. 2018;4(1):11.
ACR Appropriateness Criteria. American college of radiology. [Accessed 2023 June 28]; Available from: https://www.acr.org/Clinical-Resources/ACR-Appropriateness-Criteria.
Sidawy A. In: Perler B, editor. Rutherford’s Vascular Surgery and Endovascular Therapy. Volume 9th Editionth. Elsevier; 2018. p. 2832.
Schmauss D, et al. Three-dimensional printing for perioperative planning of complex aortic arch Surgery. Ann Thorac Surg. 2014;97(6):2160–3.
Shijo T, et al. Stent grafting simulation using a three-dimensional printed model for extensive aortic arch repair combined with coarctation. Eur J Cardiothorac Surg. 2018;54(3):593–5.
Rynio P, et al. A 3D printed aortic Arch Template to facilitate decision-making regarding the Use of an Externalized Transapical Wire during thoracic endovascular Aneurysm repair. Ann Vasc Surg. 2019;54:336. e5-336 e8.
Sulaiman A, et al. In vitro non-rigid life-size model of aortic arch Aneurysm for endovascular prosthesis assessment. Eur J Cardiothorac Surg. 2008;33(1):53–7.
Izgi C, et al. External aortic Root support to prevent aortic dilatation in patients with Marfan Syndrome. J Am Coll Cardiol. 2018;72(10):1095–105.
Treasure T, et al. Personalised external aortic root support (PEARS) in Marfan Syndrome: analysis of 1–9 year outcomes by intention-to-treat in a cohort of the first 30 consecutive patients to receive a novel tissue and valve-conserving procedure, compared with the published results of aortic root replacement. Heart. 2014;100(12):969–75.
Pepper J et al. Implantation of an individually computer-designed and manufactured external support for the Marfan aortic root Multimed Man Cardiothorac Surg, 2013. 2013: p. mmt004.
Rynio P, et al. A 3-Dimensional printed aortic Arch Template to facilitate the creation of physician-modified stent-grafts. J Endovasc Ther. 2018;25(5):554–8.
Tong Y, et al. Three-Dimensional Printing to Guide the application of modified Prefenestrated Stent grafts to treat aortic Arch Disease. Ann Vasc Surg. 2020;66:152–9.
Li CS, et al. Three-Dimensional Printing-assisted fabrication of Stent Graft to reconstruct the total aortic Arch. Ann Thorac Surg. 2020;110(3):1055–9.
Tam MD, et al. Use of a 3D printed hollow aortic model to assist EVAR planning in a case with complex neck anatomy: potential of 3D printing to improve patient outcome. J Endovasc Ther. 2014;21(5):760–2.
Tam MD, et al. A pilot study assessing the impact of 3-D printed models of aortic aneurysms on management decisions in EVAR Planning. Vasc Endovascular Surg. 2016;50(1):4–9.
Hoegen P, et al. How precise are preinterventional measurements using centerline analysis applications? Objective ground truth evaluation reveals Software-specific centerline characteristics. J Endovasc Ther. 2017;24(4):584–94.
Burris NS, Hoff BA, Ross BD. Vascular deformation mapping (VDM) of thoracic aortic Aneurysm: an application for color 3D printing in aortic Disease. Ann Transl Med. 2018;6(Suppl 2):S123.
Yuan D, et al. Precise treatment of aortic Aneurysm by three-dimensional printing and simulation before endovascular intervention. Sci Rep. 2017;7(1):795.
Pakeliani D, et al. Patient-specific rehearsal feasibility before endovascular repair of ruptured abdominal aortic Aneurysm. J Endovasc Ther. 2019;26(6):871–8.
Hojo D, et al. 3D printed model-based simulation of laparoscopic Surgery for descending colon Cancer with a concomitant abdominal aortic Aneurysm. Tech Coloproctol. 2019;23(8):793–7.
Karkkainen JM, et al. Simulation of Endovascular Aortic Repair using 3D printed abdominal aortic Aneurysm model and fluid pump. Cardiovasc Intervent Radiol. 2019;42(11):1627–34.
Chung M, et al. On the optimization of low-cost FDM 3D printers for accurate replication of patient-specific abdominal aortic Aneurysm geometry. 3D Print Med. 2018;4(1):2.
Bortman J, et al. Use of 3-Dimensional Printing to create patient-specific abdominal aortic Aneurysm models for Preoperative Planning. J Cardiothorac Vasc Anesth. 2019;33(5):1442–6.
Bangeas P, Voulalas G, Ktenidis K. Rapid prototyping in aortic Surgery. Interact Cardiovasc Thorac Surg. 2016;22(4):513–4.
Polanczyk A, et al. A novel vision-based system for quantitative analysis of abdominal aortic Aneurysm deformation. Biomed Eng Online. 2019;18(1):56.
Winder RJ, et al. Abdominal aortic Aneurysm and stent graft phantom manufactured by medical rapid prototyping. J Med Eng Technol. 2002;26(2):75–8.
Coles-Black J, Bolton D, Chuen J. Accessing 3D printed vascular phantoms for Procedural Simulation. Front Surg. 2020;7:626212.
Kaschwich M, et al. Feasibility of an endovascular training and research environment with exchangeable patient specific 3D printed vascular anatomy: Simulator with exchangeable patient-specific 3D-printed vascular anatomy for endovascular training and research. Ann Anat. 2020;231:151519.
Torres IO, De Luccia N. A simulator for training in endovascular Aneurysm repair: the use of three dimensional printers. Eur J Vasc Endovasc Surg. 2017;54(2):247–53.
Wijnen N, et al. Comparison of segmentation software packages for in-hospital 3D print workflow. J Med Imaging (Bellingham). 2021;8(3):034004.
Tam MD, et al. 3D printing of an aortic Aneurysm to facilitate decision making and device selection for endovascular Aneurysm repair in complex neck anatomy. J Endovasc Ther. 2013;20(6):863–7.
Kaschwich M, et al. Accuracy evaluation of patient-specific 3D-printed aortic anatomy. Ann Anat. 2021;234:151629.
Baron V, Guevara R. Three-dimensional printing-guided fenestrated endovascular aortic Aneurysm repair using open source software and physician-modified devices. J Vasc Surg Cases Innov Tech. 2019;5(4):566–71.
Mitsuoka H, et al. Preoperative Planning for Physician-Modified endografts using a three-Dimensional Printer. Ann Vasc Dis. 2019;12(3):334–9.
Taher F, et al. The influence of prototype testing in three-dimensional aortic models on fenestrated endograft design. J Vasc Surg. 2017;65(6):1591–7.
Koleilat I, et al. Interobserver variability in physician-modified endograft planning by comparison with a three-dimensional printed aortic model. J Vasc Surg. 2016;64(6):1789–96.
Meess KM et al. 3D printed abdominal aortic Aneurysm Phantom for image guided Surgical Planning with a patient specific Fenestrated Endovascular Graft System. Proc SPIE Int Soc Opt Eng, 2017. 10138.
You JH, Kang SG, Kim BM. A novel measurement technique for the design of fenestrated stent grafts: comparison with three-dimensional aorta models. Exp Clin Cardiol. 2013;18(1):48–52.
Rhee Y, et al. Pre-sewn multi-branched aortic graft and 3D-Printing Guidance for Crawford Extent II or III Thoracoabdominal aortic Aneurysm repair. Semin Thorac Cardiovasc Surg; 2021.
Branzan D, et al. The influence of 3D printed aortic models on the evolution of Physician Modified Stent grafts for the Urgent treatment of Thoraco-abdominal and pararenal aortic pathologies. Eur J Vasc Endovasc Surg. 2021;61(3):407–12.
Huang J, et al. 3D printing guiding stent graft fenestration: a novel technique for fenestration in endovascular Aneurysm repair. Vascular. 2017;25(4):442–6.
Coles-Black J, Barber T, Chuen J. A flexible 3D printed template to assist with Physician Modified endografts for FEVAR. Eur J Vasc Endovasc Surg. 2021;61(4):699–700.
Leotta DF, Starnes BW. Custom fenestration templates for endovascular repair of juxtarenal aortic aneurysms. J Vasc Surg. 2015;61(6):1637–41.
Marone EM, et al. A 3D-printed patient-specific model to assist decision making in endovascular treatment of thoracoabdominal aortic Aneurysm. J Cardiovasc Surg (Torino). 2018;59(2):291–3.
Starnes BW, Tatum B, Singh N. Procedural and perioperative results in patients treated with fenestrated endovascular Aneurysm repair planned by automated software in a physician-sponsored investigational device exemption trial of physician-modified endografts. J Vasc Surg. 2018;68(5):1297–307.
Crawford SA, et al. Impact of insertion technique and iliac artery anatomy on Fenestrated Endovascular Aneurysm Repair. J Endovasc Ther. 2019;26(6):797–804.
Takao H, et al. 3D Printing of Preoperative Simulation models of a splenic artery Aneurysm: Precision and Accuracy. Acad Radiol. 2017;24(5):650–3.
Itagaki MW. Using 3D printed models for planning and guidance during endovascular intervention: a technical advance. Diagn Interv Radiol. 2015;21(4):338–41.
Marone EM, et al. Robotic Treatment of Complex Splenic Artery Aneurysms with Deep Hilar Location: technical insights and Midterm results. Ann Vasc Surg. 2020;68:50–6.
Shibata E, et al. 3D-Printed visceral Aneurysm models based on CT Data for Simulations of Endovascular Embolization: evaluation of size and shape accuracy. AJR Am J Roentgenol. 2017;209(2):243–7.
Lin JC, Myers E. Three-dimensional printing for preoperative planning of renal artery Aneurysm Surgery. J Vasc Surg. 2016;64(3):810.
Li F, et al. Occlusion of an ascending aortic pseudoaneurysm with intraoperative echocardiography and a printed model. J Thorac Cardiovasc Surg. 2016;152(1):282–4.
Cuman M, et al. 3D model-guided transcatheter closure of ascending aorta pseudoaneurysm with the novel Amplatzer Trevisio intravascular delivery system. Catheter Cardiovasc Interv. 2022;99(1):140–4.
Hossien A, et al. The interactive use of Multi-dimensional modeling and 3D Printing in Preplanning of Type A Aortic Dissection. J Card Surg. 2016;31(7):441–5.
Finotello A, et al. Twelve-year follow-up post-thoracic endovascular repair in type B Aortic Dissection shown by three-dimensional Printing. Ann Vasc Surg. 2019;55:309e13–9.
Wu CA, Squelch A, Sun Z. Investigation of three-dimensional Printing materials for Printing Aorta Model replicating type B Aortic Dissection. Curr Med Imaging. 2021;17(7):843–9.
Chen D, et al. A mock circulation Loop for in vitro hemodynamic evaluation of Aorta: application in Aortic Dissection. J Endovasc Ther. 2022;29(1):132–42.
Kim WK, et al. 3D-Printing-Based Open repair of extensive thoracoabdominal aorta in severe scoliosis. Semin Thorac Cardiovasc Surg. 2019;31(1):61–3.
Wang TH, et al. Use of three dimensional-printing in the management of floating aortic thrombus due to occult Aortic Dissection: a case report. World J Clin Cases. 2021;9(7):1755–60.
Li XR, et al. Total endovascular repair of an intraoperative stent-graft deployed in the false lumen of Stanford type A Aortic Dissection: a case report. World J Clin Cases. 2020;8(5):954–62.
Zhang M, et al. Treatment of Stanford type A Aortic Dissection with triple pre-fenestration, reduced diameter, and three-dimensional-printing techniques: a case report. World J Clin Cases. 2021;9(1):183–9.
Santoro G, et al. Transcatheter treatment of Complex Aortic Coarctation guided by printed 3D model. JACC Case Rep. 2021;3(6):900–4.
Ghisiawan N, et al. The use of a three-dimensional print model of an aortic arch to plan a complex percutaneous intervention in a patient with coarctation of the aorta. Cardiol Young. 2016;26(8):1568–72.
Kleszcz J, et al. Assessing a new coarctation repair simulator based on real patient’s anatomy. Cardiol Young. 2019;29(12):1517–21.
Branzan D, et al. 3-Dimensional aortic model to create a Fenestrated Stent Graft for the Urgent treatment of a paravisceral penetrating aortic Ulcer. JACC Cardiovasc Interv. 2019;12(8):793–5.
Gocer H, et al. Evaluation of 3D printing in planning, practicing, and training for endovascular lower extremity arterial interventions. Turk Gogus Kalp Damar Cerrahisi Derg. 2021;29(1):20–6.
Rynio P et al. Simulation and Training of Needle Puncture Procedure with a patient-specific 3D printed gluteal artery model. J Clin Med, 2020. 9(3).
Aldosari S, Jansen S, Sun Z. Patient-specific 3D printed pulmonary artery model with simulation of peripheral Pulmonary Embolism for developing optimal computed tomography pulmonary angiography protocols. Quant Imaging Med Surg. 2019;9(1):75–85.
Wang H, et al. A minimally invasive alternative for the treatment of nutcracker syndrome using individualized three-dimensional printed extravascular titanium stents. Chin Med J (Engl). 2019;132(12):1454–60.
He D, et al. 3D-Printed PEEK Extravascular Stent in the treatment of Nutcracker Syndrome: imaging evaluation and short-term clinical outcome. Front Bioeng Biotechnol. 2020;8:732.
Guo YT, et al. Two-year follow-up on Laparoscopic three-dimensional printed Extravascular Stent Placement for posterior nutcracker syndrome. Chin Med J (Engl). 2018;131(23):2895–6.
Chung SH, Kim KG. Design of lymphedema ultrasound phantom with 3D-printed patient-specific subcutaneous anatomy: A-mode analysis approach for early diagnosis. Phys Med. 2018;55:73–81.
Sun X, et al. Patient-specific three-dimensional printing for Kommerell’s diverticulum. Int J Cardiol. 2018;255:184–7.
Kiraly L, et al. Three-dimensional printed prototypes refine the anatomy of post-modified Norwood-1 complex aortic arch obstruction and allow presurgical simulation of the repair. Interact Cardiovasc Thorac Surg. 2016;22(2):238–40.
Arcieri L, et al. Three-dimensional printing for surgical planning of a double aortic arch case. J Card Surg. 2020;35(4):912–5.
Han Y, et al. Three-dimensional printed degradable splint in the treatment of pulmonary artery sling associated with severe bilateral bronchus stenosis. Cardiol Young. 2018;28(12):1477–80.
Chick JFB, et al. Three-Dimensional Printing facilitates successful Endovascular Closure of a type II Abernethy Malformation using an Amplatzer Atrial Septal Occluder device. Ann Vasc Surg. 2017;43:311. e15-311 e23.
Totaro P, et al. Multidisciplinary preoperative simulations to optimize surgical outcomes in a challenging case of the complete double aortic arch in the adult. J Card Surg. 2020;35(3):716–20.
Govsa F, et al. Building 3D anatomical model of coiling of the internal carotid artery derived from CT angiographic data. Eur Arch Otorhinolaryngol. 2017;274(2):1097–102.
Ye X, et al. A three-dimensional color-printed system allowing complete modeling of arteriovenous malformations for surgical simulations. J Clin Neurosci. 2020;77:134–41.
Mahajan NN, et al. A Case Series of Long-Term Surgical outcomes of Primary Pulmonary Artery Sarcomas with opportunities for 3D-Printed models in Surgical Planning. Innovations (Phila). 2021;16(1):94–100.
Colley E, et al. A methodology for non-invasive 3-D surveillance of Arteriovenous Fistulae using Freehand Ultrasound. IEEE Trans Biomed Eng. 2018;65(8):1885–91.
Kabirian F, et al. Nitric oxide-releasing vascular grafts: a therapeutic strategy to promote angiogenic activity and endothelium regeneration. Acta Biomater. 2019;92:82–91.
Martin NK, et al. Fused deposition modelling for the development of drug loaded cardiovascular prosthesis. Int J Pharm. 2021;595:120243.
Basile S, et al. Optimization of FDM 3D printing process parameters to produce haemodialysis curcumin-loaded vascular grafts. Drug Deliv Transl Res; 2021.
Girsowicz E, et al. Evaluation of Nitinol Stents using a 3-Dimensional printed superficial femoral artery model: a preliminary study. Ann Vasc Surg. 2016;33:1–10.
Kim T, Lee YG. Shape transformable bifurcated stents. Sci Rep. 2018;8(1):13911.
Wu Z et al. Radial Compressive Property and the Proof-of-Concept Study for Realizing Self-expansion of 3D Printing Polylactic Acid Vascular Stents with Negative Poisson’s Ratio Structure. Mater (Basel), 2018. 11(8).
Kim D, Kim T, Lee YG. 4D printed bifurcated stents with Kirigami-inspired structures. J Vis Exp, 2019(149).
Guerra AJ et al. 3D-Printed PCL/PLA Composite stents: towards a New Solution to Cardiovascular problems. Mater (Basel), 2018. 11(9).
Misra SK et al. 3D-Printed Multidrug-Eluting Stent from Graphene-Nanoplatelet-Doped Biodegradable Polymer Composite. Adv Healthc Mater, 2017. 6(11).
Zhang Y, et al. Mechanical properties and degradation of drug eluted bioresorbable vascular scaffolds prepared by three-dimensional printing technology. J Biomater Sci Polym Ed. 2019;30(7):547–60.
Singh J, et al. Biological and mechanical characterization of biodegradable carbonyl iron powder/polycaprolactone composite material fabricated using three-dimensional printing for cardiovascular stent application. Proc Inst Mech Eng H. 2020;234(9):975–87.
Farzin A, et al. 3D-Printed Sugar-based stents facilitating vascular anastomosis. Adv Healthc Mater. 2018;7(24):e1800702.
Lei Y, et al. A new process for customized patient-specific aortic stent graft using 3D printing technique. Med Eng Phys. 2020;77:80–7.
Zhou Y, et al. 4D Printing of shape memory vascular stent based on betaCD-g-Polycaprolactone. Macromol Rapid Commun. 2021;42(14):e2100176.
Gallagher MB, et al. Steady Flow in a patient-averaged Inferior Vena Cava-Part I: particle image Velocimetry measurements at Rest and Exercise conditions. Cardiovasc Eng Technol. 2018;9(4):641–53.
Craven BA, Aycock KI, Manning KB. Steady Flow in a patient-averaged Inferior Vena Cava-Part II: computational Fluid Dynamics Verification and Validation. Cardiovasc Eng Technol. 2018;9(4):654–73.
Yunker BE, et al. The design and fabrication of two portal vein flow phantoms by different methods. Med Phys. 2014;41(2):023701.
Lai SS, et al. Design of anthropomorphic flow phantoms based on rapid prototyping of compliant vessel geometries. Ultrasound Med Biol. 2013;39(9):1654–64.
Chi QZ et al. A Brush-Spin-Coating Method for Fabricating In Vitro Patient-Specific Vascular Models by Coupling 3D-Printing Cardiovasc Eng Technol, 2021. 12(2): p. 200–214.
de Zelicourt D, et al. Single-step stereolithography of complex anatomical models for optical flow measurements. J Biomech Eng. 2005;127(1):204–7.
Pekkan K, et al. Physics-driven CFD modeling of complex anatomical cardiovascular flows-a TCPC case study. Ann Biomed Eng. 2005;33(3):284–300.
Harrison GJ, et al. Closure technique after carotid endarterectomy influences local hemodynamics. J Vasc Surg. 2014;60(2):418–27.
Huang Zhang P, et al. The mechanics of spiral flow: enhanced washout and transport. Artif Organs. 2019;43(12):1144–53.
Kaschwich M, et al. Development of an ultrasound-capable phantom with patient-specific 3D-printed vascular anatomy to simulate peripheral endovascular interventions. Ann Anat. 2020;232:151563.
Lashkarinia SS, et al. Computational pre-surgical planning of arterial Patch Reconstruction: Parametric limits and in Vitro Validation. Ann Biomed Eng. 2018;46(9):1292–308.
Ruedinger KL, Medero R, Roldan-Alzate A. Fabrication of low-cost patient-specific vascular models for particle image Velocimetry. Cardiovasc Eng Technol. 2019;10(3):500–7.
Boutsianis E, et al. CFD and PTV steady flow investigation in an anatomically accurate abdominal aortic Aneurysm. J Biomech Eng. 2009;131(1):011008.
Deng L, et al. Computational numerical analysis of different cannulation methods during cardiopulmonary bypass of type A Aortic Dissection model based on computational fluid dynamics. Ann Transl Med. 2021;9(8):667.
de Ruiz S, et al. A methodology for developing anisotropic AAA phantoms via additive manufacturing. J Biomech. 2017;57:161–6.
Anton R, et al. Experimental and computational investigation of the patient-specific abdominal aortic Aneurysm pressure field. Comput Methods Biomech Biomed Engin. 2015;18(9):981–92.
Mix DS, et al. Detecting Regional stiffness changes in aortic aneurysmal geometries using pressure-normalized strain. Ultrasound Med Biol. 2017;43(10):2372–94.
Cloonan AJ, et al. 3D-Printed tissue-mimicking phantoms for medical imaging and computational validation applications. 3D Print Addit Manuf. 2014;1(1):14–23.
Lermusiaux P, et al. Aortic Aneurysm: construction of a life-size model by rapid prototyping. Ann Vasc Surg. 2001;15(2):131–5.
Berry E, et al. Flexible tubular replicas of abdominal aortic aneurysms. Proc Inst Mech Eng H. 2002;216(3):211–4.
Chi Q-Z, et al. A brush-spin-coating method for fabricating in Vitro patient-specific vascular models by coupling 3D-Printing. Cardiovasc Eng Technol Vol. 2021;12(2):200–14. https://doi.org/10.1007/s13239-020-00504-9.
Hakansson A, et al. Patient specific biomodel of the whole aorta - the importance of calcified plaque removal. Vasa. 2011;40(6):453–9.
Menon NV, et al. Recapitulating atherogenic flow disturbances and vascular inflammation in a perfusable 3D stenosis model. Biofabrication. 2020;12(4):045009.
Wen CY, et al. Investigation of pulsatile flowfield in healthy thoracic aorta models. Ann Biomed Eng. 2010;38(2):391–402.
Carvalho V et al. 3D printed biomodels for Flow visualization in Stenotic vessels: an Experimental and Numerical Study. Micromachines (Basel), 2020. 11(6).
Chang D, et al. Three-Dimensional Printing for Procedure Rehearsal/Simulation/Planning in Interventional Radiology. Tech Vasc Interv Radiol. 2019;22(1):14–20.
Mitsouras D, et al. Medical 3D Printing for the Radiologist. Radiographics. 2015;35(7):1965–88.
Mitsouras D, et al. RadioGraphics Update: medical 3D Printing for the Radiologist. Radiographics. 2020;40(4):E21–3.
Funding
No funding sources to declare for this study.
Author information
Authors and Affiliations
Contributions
Every author listed above has been involved in design, data collection, interpretation, as well as manuscript drafting and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests related to this work. Competing Interests not related to this work:
NW: In-kind research support: Stratasys; Employee: GE Healthcare.
FR: Healthcare Advisory Committee member: Canon Medical Systems Corporation; Consultant: Imagia-Canexia Health, KA Imaging.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lee, J., Chadalavada, S.C., Ghodadra, A. et al. Clinical situations for which 3D Printing is considered an appropriate representation or extension of data contained in a medical imaging examination: vascular conditions. 3D Print Med 9, 34 (2023). https://doi.org/10.1186/s41205-023-00196-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41205-023-00196-6