Abstract
Background
The production of extended-spectrum beta-lactamases (ESBLs) among uropathogens, particularly E. coli and Klebsiella spp., poses a severe public health concern. This study explored the epidemiology of ESBL-producing E. coli and Klebsiella spp. isolated from urine samples obtained at a tertiary care children's hospital in Nepal.
Methods
A cross-sectional study was conducted from August 2016 to February 2017. A total of 745 clean catch urine samples were obtained from pediatric patients under the age of 13 and subjected to semiquantitative culture. E. coli and Klebsiella spp. were identified using standard laboratory protocols. Antibiotic susceptibility testing was performed using the Kirby-Bauer disc diffusion method, and ESBL producers were phenotypically identified using the combined disk method.
Results
Among the bacterial isolates, E. coli predominated, accounting for 139 (81.8%) positive cases. Notably, E. coli showed high susceptibility to nitrofurantoin, with 117 (84.2%) isolates being susceptible. Meanwhile, K. pneumoniae showed high susceptibility to gentamicin, with 21 (91.3%) isolates being susceptible. Of the 163 isolates of E. coli and Klebsiella spp., 62 (38.0%) were identified as multidrug-resistant (MDR), with 42 (25.8%) confirmed as phenotypic ESBL producers. Remarkably, all 41 (100%) ESBL-producing E. coli isolates were susceptible to imipenem.
Conclusions
The prevalence of ESBL producers among E. coli and K. pneumoniae isolates from pediatric patients underscores the importance of antimicrobial stewardship. Nitrofurantoin and gentamicin emerge as effective empirical treatment choices against these pathogens in children. However, the high rates of multidrug resistance and ESBL production highlight the necessity for routine surveillance, and early detection strategies to manage such infections effectively.
Similar content being viewed by others
Background
Urinary tract infections (UTIs) are a prevalent concern among children, affecting at least 3.6% of boys and 11.3% of girls by the age of 16 [1]. Notably, UTIs can progress to kidney failure, posing serious health risks to children [2]. Among the gram-negative bacteria causing UTIs, Escherichia coli (E. coli) and Klebsiella pneumoniae are predominant pathogens [1]. The rise of antimicrobial resistance (AMR) in E. coli and K. pneumoniae presents a formidable public health challenge [3]. In 2019, bacterial AMR was attributed for an estimated 1.27 million deaths globally [4]. The consequences of AMR extend beyond clinical outcomes, increasing healthcare costs by prolonging illnesses, extending hospital stays, requiring additional diagnostic tests, necessitating more intensive care, and necessitating the use of more expensive antibiotics. Novel AMR systems driven by natural genetic mutation are emerging and spreading within bacterial population, leading to an increase in multidrug-resistant (MDR) bacteria [5]. The production of beta-lactamases is a common mechanism of antimicrobial resistance, which confers resistance to beta-lactam antibiotics, including cephalosporins and carbapenems [6]. ESBLs were first reported in Germany in 1983 [7] and Nepal in 2006 [8]. Cross-resistance to other non-beta-lactam antibiotics is common in ESBL-producing bacteria, limiting therapeutic choices [9].
While the bacterial AMR profiles vary temporally and geographically, there exists a notable gap in the epidemiological understanding of ESBL-producing E. coli and Klebsiella spp. among children in Nepal. Surveillance data of this nature holds immense value for guiding evidence-based therapy and improving the management of such infections by healthcare providers. Therefore, this study aimed to elucidate the epidemiology of ESBL-producing E. coli and Klebsiella spp. in urine samples obtained from children at a tertiary care children's hospital in Nepal.
Methods
Study setting, design, and sample population
From August 2016 to February 2017, a prospective cross-sectional study was conducted at the Department of Microbiology, International Friendship Children Hospital in Kathmandu, Nepal. The study included 745 non-repetitive clean-catch midstream urine samples from pediatric patients under the age of 13 with symptoms indicative of UTI. Symptoms included urgency, dysuria, frequency, loss of bladder control, suprapubic tenderness, flank pain, costovertebral angle pain and tenderness, rigors, new or worsening fever, cloudy or foul-smelling urine, and parental reporting of similar symptoms in infants and younger children. Patients receiving antibiotic therapy or had undergone bladder catheterization within 48 h prior to sample collection were excluded. Demographic data including age, sex, and hospital ward were retrieved from hospital records.
Collection of urine samples
10–15 ml clean catch urine samples were collected using sterile, dry, wide-mouthed, and leakproof containers. For non-toilet trained children and infants, sterile foil bowls were placed beneath the genitalia, or sterile plastic bags were attached. Toilet-trained children provided clean catch voided midstream urine samples. Thorough periurethral cleaning was recommended prior to urine collection to minimize contamination. Noninvasive techniques were exclusively employed for urine collection. Equivocal samples underwent repeat testing.
Laboratory examinations of urine samples
Macroscopic examination: Urine samples were visually inspected for signs of contamination.
Quantitative culture and identification of isolates: The calibrated loop technique was used for quantitative culture, and isolates were identified as E. coli or Klebsiella spp. based on Gram's stain, cultural characteristics, and biochemical properties [10].
Antimicrobial susceptibility testing of E. coli and Klebsiella spp.
Antibiotic susceptibility testing was performed using the Kirby-Bauer disc diffusion method on Mueller–Hinton agar (MHA) (HiMedia Pvt. Ltd., India). The following antibiotic discs (HiMedia Pvt. Ltd., India) were utilized: amoxicillin (10 μg), cefixime (10 μg), cefotaxime (30 μg), cefpodoxime (30 μg), ceftazidime (30 μg), ceftriaxone (30 μg), ciprofloxacin (5 μg), cotrimoxazole (1.25/23.75 μg), gentamicin (10 μg), imipenem (10 μg), nitrofurantoin (300 μg), norfloxacin (10 μg), ofloxacin (5 μg), piperacillin (100 μg), and vancomycin (30 μg). Interpretation followed the CLSI M100-S26 guidelines, with Pseudomonas. aeruginosa ATCC 27853 and E. coli ATCC 25922 used as control strains [11]. Isolates resistant to two or more classes of antimicrobial agents were classified as multidrug-resistant (MDR).
Tests for ESBL production in E. coli and Klebsiella spp.
ESBL-producing isolates were phenotypically identified following the CLSI M100-S26 guidelines [11].
Screening of ESBL-producing strains
A zone of inhibition ≤ 25 mm for ceftriaxone, ≤ 22 mm for ceftazidime, ≤ 17 mm for cefpodoxime, and/or ≤ 27 mm for cefotaxime was indicative of confirmation of ESBL [11].
Confirmation of ESBL-producing strains
ESBL-producing isolates were phenotypically confirmed using the combined disc method. The zones of inhibition were assessed individually for the ceftazidime (30 µg) and cefotaxime (30 µg) discs, as well as in combination with clavulanic acid (10 µg), with the discs positioned 25 mm apart (center to center). Isolates showing a zone size increase of 5 mm or more around one or both of the clavulanate combined discs compared to the antibiotic alone were confirmed as ESBL producers. Control strains, K. pneumoniae ATCC 700603 and E. coli ATCC 25922 were included for reference [11].
Data management and statistical analysis
First, Microsoft Excel 2016 (Microsoft Corporation, USA) was used for data management, and then R© for Windows version 4.3.2 (R Core Team, Austria) was used for statistical analyses. Descriptive statistics were presented using percentages. The R package 'gmodels' (version 2.18.1) was utilized to generate the cross-tabulations, and the built-in R function ‘fisher.test’ was used to perform Fisher’s exact test (FET) for the test of independence. Cross-tabulations larger than 2×2 were tested using the Monte Carlo method of FET with 5,000 replicates. Odds ratios (ORs) and confidence intervals (CIs) were used to gauge the strength of the associations. Significant cross-tabulations larger than 2×2 were reparameterized into 2×2 cross-tabulations for the post hoc test. In a post hoc test, FET was utilized to identify specific significant categories. A p value of less than or equal to .05 indicated statistical significance. For inferential statistics, the traditional null hypothesis significance testing method based on the p value was employed.
Results
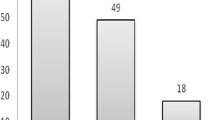
Out of the 745 samples, bacterial growth was observed in 170 (22.8%) cases. The incidence of growth was similar in samples collected from males and females. A higher proportion of samples from inpatient care settings exhibited bacterial growth, accounting for 36 (30.0%) cases. Despite the absence of a significant association between sex and bacterial growth (p value= 1, FET), a significant association was observed between patient care setting and bacterial growth (p value= .044, FET). Specifically, the odds of bacterial growth were lower among inpatients compared to outpatients (OR= 0.64). It is important to note, however, that the effect size was relatively small, and the exact strength of the association remains uncertain (95% CI 0.41-1.02) (Table 1). Notably, E. coli was the predominant bacterial isolate, accounting for 139 (81.8%) of the identified cases (Fig. 1).
E. coli showed high susceptibility to nitrofurantoin (117, 84.2%) and gentamicin (105, 75.5%), however, lower susceptibility to amoxicillin (20, 14.4%). Conversely, K. pneumoniae showed high susceptibility to gentamicin (21, 91.3%), nitrofurantoin, and ciprofloxacin (both 18, 78.3%), while showing no susceptibility to amoxicillin (Fig. 2).
Of the 163 isolates of E. coli and Klebsiella spp., 62 (38.0%) were found to be MDR. Among these isolates, 71 (43.6%) tested positive during ESBL screening, yet only 42 (25.8%) of them were confirmed as ESBL producers using the combined disk method. Notably, ESBL-positive cases were predominantly observed in E. coli, while K. pneumoniae and K. oxytoca showed fewer instances. Investigation of the association between ESBL detection and the three different bacterial species revealed a statistically significant association (p value = .011, FET). Individual post hoc tests were conducted to assess specific pairs of categories. Notably, the post hoc test further revealed significant associations between the ESBL detection in both E. coli and K. pneumoniae (p value = .010, FET and p value = .009, FET, respectively), with estimated odds ratios of 9.54 and 9.04, respectively. However, effect sizes were relatively small, and the exact strength of the associations was uncertain (95% CI 1.45–405.18 and 95% CI 1.37–384.41). No significant associations were observed for K. oxytoca (p value = 1, FET). This can be attributed to the absence of ESBL producers in K. oxytoca, which complicated the statistical results due to extreme values (Table 2).
Investigation of the association between ESBL detection and MDR bacteria did not yield statistical significance (p value = 1, FET). An individual post hoc test was conducted to assess the sensitivity of the obtained p value. We specifically checked the association of ESBL detection in MDR E. coli and MDR Klebsiella spp. Despite a lack of significance at the conventional level (0.05), a potential association between MDR and ESBLs was suggested by the sharp decrease in the p value (p value = .14, FET), with an estimated odds ratio of 0.19 and a 95% CI of 0.004–1.61, indicating uncertainty about the true odds ratio (Table 2).
ESBL producers were more prevalent among females (36, 32.7%) and inpatients (12, 35.3%). Significant differences in ESBL prevalence were observed between the sexes (p value = .003, FET) (Table 3).
Among the 41 ESBL-producing E. coli isolates, all exhibited susceptibility to imipenem (41, 100.0%) and nitrofurantoin (39, 95.1%), with none exhibiting susceptibility to amoxicillin (Fig. 3). The single ESBL-producing K. pneumoniae isolate exhibited susceptibility to nitrofurantoin, gentamicin, imipenem, and meropenem.
Discussion
The management of UTIs in children is becoming increasingly complicated due to the rising prevalence of AMR among common pathogens [12]. In this study, only 18.13% of the samples yielded growth in culture, a proportion consistent with findings from other studies conducted in Nepal [13,14,15,16]. However, other studies in Nepal reported contrasting results indicating meager proportions [17, 18]. This entails a reevaluation of the existing protocols for pediatric clinical diagnosis of UTIs, focusing microbiological examinations solely on urine samples suggestive of clinical UTIs. Such an approach promises heightened sensitivity and efficacy in clinical diagnosis while conserving considerable resources and curtailing cost. The association of both E. coli and K. pneumoniae with nosocomial infections in children is a cause for, concern. These organisms normally inhabit the periurethral region as commensals. The development of UTIs occurs when these organisms gain access to and ascend within the urethra [19].
Infections caused by E. coli and Klebsiella spp. are very common in children. The presence of ESBL in these bacteria is concerning, since it elevates the risk of ESBL-producing organisms among children. In this study, a high proportion (38.0%) of the isolates were identified as MDR. Previous studies conducted in Nepal have reported even higher percentages [13, 16]. Similar results have been reported in the literature from various regions including Nepal [18], India [20], Iran [21, 22], Cambodia [23], and Turkey [24]. However, a systematic review reported lower percentages [25] potentially attributed to variations in the phenotypic detection methods of ESBL production and differences in the study population. The rise in ESBL producers in recent years may be attributed to the increased dependence on third-generation cephalosporins for treating gram-negative infections and questionable antibiotic policies. It is noteworthy that AmpC enzymes, produced by organisms such as Citrobacter, Enterobacter, and Serratia, are not inhibited by clavulanate, potentially leading to false-negative results in ESBL testing. Consequently, the prevalence of ESBL enzymes might be underestimated. Adding an AmpC inhibitor, such as cloxacillin, could enhance the detection of ESBL enzymes in these organisms [26].
All ESBL producers exhibited susceptibility to imipenem. A lower percentage was reported in a study in Nepal [13]. Likewise, other studies in Nepal also reported high susceptibility to imipenem [16, 18]. However, it’s important to note that imipenem, being an intravenous antibiotic, is not recommended as a first-line therapy for UTIs. Although meropenem exhibits moderate susceptibility, it falls under the same class of antibiotics as imipenem, known as carbapenems. The transfer of carbapenemase genes and ESBL genes via plasmids facilitates the rapid dissemination of carbapenemase and ESBL-producing strains. The co-production of carbapenemase and ESBL represents a significant mechanism in the evolving landscape of AMR patterns. Recent years have highlighted a substantial percentage of imipenem-resistant strains, along with co-producing ESBLs, underscoring the urgency of addressing AMR [27] Both ESBL producers and non-ESBL producers exhibited high susceptibility to nitrofurantoin, consistent with findings from studies in Nepal [16,17,18]. However, nitrofurantoin’s efficacy is compromised by enzymatic degradation, posing challenges in maintaining therapeutic concentrations within body tissues. Consequently, its use is recommended primarily for treating uncomplicated lower UTIs. Moreover, nitrofurantoin’s efficacy is limited against uropathogens other than E. coli, since Pseudomonas spp., Proteus spp., and Serratia spp. exhibit intrinsic resistance to this antibiotic [28]. Likewise, E. coli and Klebsiella spp. exhibited high susceptibility to gentamicin, with the antibiotic exhibiting moderate effectiveness against ESBL producers, consistent with findings from studies in Nepal [16, 18]. In addition, both E. coli and Klebsiella spp. exhibited moderate susceptibility to co-trimoxazole, an oral antibiotic commonly used to treat pediatric UTIs. Moreover, fluoroquinolones exhibited moderate susceptibility against E. coli and Klebsiella spp., hence they are not recommended as second-line treatments. Consistent results were reported in a study conducted in Nepal [13]. In addition, both E. coli and Klebsiella spp. exhibited moderate susceptibility to ceftriaxone and ceftazidime. However, a lower susceptibility to ceftazidime was reported in a study in Nepal [18]. Furthermore, it is recommended to consider ESBL-producing isolates as resistant to these antibiotics, regardless of the susceptibility testing results [11]. This underscores the unreliability of lower-generation cephalosporins as empiric antibiotics. In clinical practice, most children are empirically treated with antibiotics even before culture and susceptibility data are available to prevent complications [29]. The empirical use of gentamicin until the patient’s sensitivity pattern is available may be a prudent approach. Alternatively, nitrofurans remain viable first-line treatments and are cost-effective. In addition, both of these antibiotics are considered safe for pediatric use.
Among the isolates of E. coli and Klebsiella spp., 38.0% were identified as MDR, while 25.8% were found to be ESBL producers. Given the predominance of ESBL-positive E. coli strains, we tested the association between ESBL detection and three different bacterial species. Our statistical analysis revealed a significant association (p value = .011, FET). Further exploration through individual post hoc tests uncovered significant associations between ESBL detection in both E. coli and K. pneumoniae (p value = .010, FET and p value = .009, FET, respectively), with estimated odds ratios of 9.54 and 9.04, respectively. These findings indicate substantial differences in the odds of ESBL detection in both E. coli and K. pneumoniae. However, the effect sizes were relatively small, and the exact strength of the associations remained unclear (95% CI 1.45–405.18 and 95% CI 1.37–384.41). We explored the association between ESBL detection and MDR across different bacterial species. Our statistical analysis did not reveal a significant association (p value = 1, FET). To delve deeper into this relationship, we conducted an individual post hoc test focusing specifically on MDR E. coli and MDR Klebsiella spp. However, the results did not reach statistical significance at the conventional level (0.05). Nonetheless, there was a notable decrease in the p value, suggesting a potential association between MDR and ESBL detection (p value = .14, FET). The odds ratio was estimated to be 0.19 with a 95% CI of 0.004–1.61, indicating uncertainty regarding the true odds ratio. It’s important to note that while Fisher’s exact test provides insights into the overall association between categories based on aggregate counts, it does not address uncertainties or misclassification at the individual level.
Antibiotic resistance emerges from a complex interplay of factors including ineffective antibiotic policies, poor surveillance and compliance measures, unrestricted access to antibiotics, rampant self-medication with poor adherence, suboptimal dosing practices, diagnostic errors, proliferation of low-quality counterfeit drugs, unregulated antibiotic use in agriculture, and indiscriminate antibiotic use without proper diagnosis or identification of the causative agent [30,31,32]. Antibiotic resistance patterns vary by region and time. The continual evolution of resistant strains to new antibiotics poses significant challenges in identifying effective antimicrobial drugs for treating infections caused by these pathogens. The demand for newer, more expensive drugs, coupled with pronged hospital stays, contributes to escalating healthcare costs. Since this study was confined to a single tertiary setting, further surveillance is imperative to disseminate local resistance profiles. Establishing robust surveillance systems is crucial for guiding antibiotic prescribing, mitigating resistance risks, and optimizing patient care. While empirical therapy plays a pivotal role in avoiding complications, its indiscriminate application without surveillance data can exacerbate antibiotic resistance. Considering local resistance profiles is imperative when prescribing antibiotics empirically. Such an approach will ensure the implementation of the most effective empiric (and definitive) antibiotic therapy for UTIs in children.
Phenotypic detection of ESBLs is a time-consuming and labor-intensive process, often yielding variable degrees of accuracy. Nonetheless, in routine investigations, it serves as a cost-effective alternative to molecular techniques. Understanding the prevalence of ESBLs and other antibiotic resistances in local areas can enhance physicians’ ability to make informed clinical decisions. Future studies should prioritize identifying the risk factors associated with infections caused by ESBLs and other antibiotic resistances.
Conclusions
The study highlights the commonality of ESBL production among E. coli and K. pneumoniae isolates from children in Nepal, underscoring the ongoing public health concern. The findings underscored significant resistance to commonly prescribed antibiotics among pediatric patients. Consequently, it is imperative to conduct antimicrobial susceptibility testing before initiating antibiotic therapy in children. If empirical treatment becomes necessary, nitrofurantoin and gentamicin stand out as effective and appropriate empirical choices for treating E. coli and Klebsiella spp. infections in children. Moreover, these findings underscore the urgent necessity for comprehensive antimicrobial stewardship programs to combat antibiotic resistance.
Limitations of the study
First, the study was limited to a single site over six-months with a relatively sample size. As a result, the conclusions drawn from the data may not be accurate. Conducting multicenter surveillance involving a larger sample population would bolster the reliability of the findings. Second, we were unable to comprehensively assess the associated risk factors and outcomes of UTIs in children. Third, future research should consider incorporating cohort studies to explore outcomes of antimicrobial therapy and associated risk factors. Fourth, performing antimicrobial susceptibility testing using dilution methods and assessing the minimum inhibitory concentration (MIC) would offer more precise data for monitoring drug resistance. Finally, phenotypic characterization is ineffective in determining the underlying cause of AMR in the population. We were unable to determine the genotypes of the ESBLs among the isolates due to a lack of resources. Genotyping ESBL genes would provide better insight into ESBL production among isolates in the population.
Availability of data and materials
The complete data set generated and analyzed during the study is already covered in the text. The raw data can be made available upon reasonable request to the corresponding author.
Abbreviations
- AMR:
-
Antimicrobial resistance
- ATCC:
-
American Type Culture Collection
- CFU:
-
Colony-forming units
- CLSI:
-
Clinical and Laboratory Standards Institute
- ESBL:
-
Extended-spectrum beta-lactamase
- FET:
-
Fisher’s exact test
- MDR:
-
Multidrug resistance
- MHA:
-
Mueller Hinton Agar
- UTI:
-
Urinary tract infection
References
Leung AKC, Wong AHC, Leung AAM, Hon KL. Urinary tract infection in children. Recent Pat Inflamm Allergy Drug Discov. 2019;13(1):2–18.
Morello W, La Scola C, Alberici I, Montini G. Acute pyelonephritis in children. Pediatr Nephrol. 2016;31(8):1253–65.
Mishra SK, Acharya J, Kattel HP, Koirala J, Rijal BP, Pokhrel BM. Metallo-beta-lactamase producing gram-negative bacterial isolates. J Nepal Health Res Counc. 2012;10(22):208–13.
Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet. 2022;399(10325):629–55.
World Health Organization (WHO). Antimicrobial resistance. 2021. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance. Accessed 01 Jan 2024.
Philippon A, Labia R, Jacoby G. Extended-spectrum beta-lactamases. Antimicrob Agents Chemother. 1989;33(8):1131–6.
Knothe H, Shah P, Krcmery V, Antal M, Mitsuhashi S. Transferable resistance to cefotaxime, cefoxitin, cefamandole and cefuroxime in clinical isolates of Klebsiella pneumoniae and Serratia marcescens. Infection. 1983;11(6):315–7.
Pokharel BM, Koirala J, Dahal RK, Mishra SK, Khadga PK, Tuladhar NR. Multidrug-resistant and extended-spectrum beta-lactamase (ESBL)-producing Salmonella enterica (serotypes Typhi and Paratyphi A) from blood isolates in Nepal: Surveillance of resistance and a search for newer alternatives. Int J Inf Dis. 2006;10(6):434–8.
Rudresh SM, Nagarathnamma T. Extended spectrum β-lactamase producing enterobacteriaceae & antibiotic co-resistance. Indian J Med Res. 2011;133(1):116–8.
Vandepitte J, Engbaek K, Rohner P, Piot P, Heuck CC, World Health Organization. Basic laboratory procedures in clinical bacteriology. 2nd ed. World Health Organization, Geneva; 2003.
CLSI. Performance standards for antimicrobial susceptibility testing. 26th Informational supplement M100-S26. Wayne, PA: Clinical and Laboratory Standards Institute; 2016.
Bryce A, Hay AD, Lane IF, Thornton HV, Wootton M, Costelloe C. Global prevalence of antibiotic resistance in paediatric urinary tract infections caused by Escherichia coli and association with routine use of antibiotics in primary care: systematic review and meta-analysis. BMJ. 2016;352: i939. https://doi.org/10.1136/bmj.i939.
Parajuli NP, Maharjan P, Parajuli H, Joshi G, Paudel D, Sayami S, et al. High rates of multidrug resistance among uropathogenic Escherichia coli in children and analyses of ESBL producers from Nepal. Antimicrob Resist Infect Control. 2017;6(1):9.
Rai GK, Upreti HC, Rai SK, Shah KP, Shrestha RM. Causative agents of urinary tract infections in children and their antibiotic sensitivity pattern: a hospital based study. Nepal Med Coll J (NMCJ). 2008;10(2):86–90.
Singh SD, Madhup SK. Clinical profile and antibiotics sensitivity in childhood urinary tract infection at Dhulikhel Hospital. Kathmandu Univ Med J (KUMJ). 2013;11(44):319–24.
Kayastha K, Dhungel B, Karki S, Adhikari B, Banjara MR, Rijal KR, Ghimire P. Extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella species in pediatric patients visiting international friendship children’s Hospital, Kathmandu. Nepal Infect Dis. 2020;13:1–7. https://doi.org/10.1177/1178633720909798.
Sharma KR, Bhandari P, Adhikari N, Tripathi P, Khanal S, Tiwari BR. Extended spectrum β-lactamase (ESBL) producing multi drug resistant (MDR) urinary pathogens in a children hospital from Nepal. Kathmandu Univ Med J (KUMJ). 2018;16(62):151–5.
Raya GB, Dhoubhadel BG, Shrestha D, Raya S, Laghu U, Shah A, Raya BB, Kafle R, Parry CM, Ariyoshi K. Multidrug-resistant and extended-spectrum beta-lactamase-producing uropathogens in children in Bhaktapur. Nepal Trop Med Health. 2020;48:65. https://doi.org/10.1186/s41182-020-00251-6.
McLellan LK, Hunstad DA. Urinary tract infection: pathogenesis and outlook. Trends Mol Med. 2016;22(11):946–57.
Shettigar S, Chandrashekar G, Roche R, Nayak N, Anitha K, Soans S. Bacteriological profile, antibiotic sensitivity pattern, and detection of extended-spectrum β-lactamase in the isolates of urinary tract infection from children. Indian J Child Health. 2016;3(1):27–31.
Pourakbari B, Ferdosian F, Mahmoudi S, Teymuri M, Sabouni F, Heydari H, Ashtiani MT, Mamishi S. Increase resistant rates and ESBL production between E. coli isolates causing urinary tract infection in young patients from Iran. Braz J Microbiol. 2012;2(43):766–9.
Rezai MS, Salehifar E, Rafiei A, Langaee T, Rafati M, Shafahi K, Eslami G. Characterization of multidrug resistant extended-spectrum beta-lactamase-producing Escherichia coli among uropathogens of pediatrics in north of Iran. Biomed Res Int. 2015;2015: 309478.
Moore CE, Sona S, Poda S, Putchhat H, Kumar V, Sopheary S, Stoesser N, Bousfield R, Day N, Parry CM. Antimicrobial susceptibility of uropathogens isolated from Cambodian children. Paediatr Int Child Health. 2016;36(2):113–7.
Kizilca O, Siraneci R, Yilmaz A, Hatipoglu N, Ozturk E, Kiyak A, Ozkok D. Risk factors for community-acquired urinary tract infection caused by ESBL-producing bacteria in children. Pediatr Int. 2012;54(6):858–62.
Flokas ME, Detsis M, Alevizakos M, Mylonakis E. Prevalence of ESBL-producing Enterobacteriaceae in paediatric urinary tract infections: a systematic review and meta-analysis. J Infect. 2016;73(6):547–57.
Rawat D, Nair D. Extended-spectrum β-lactamases in gram negative bacteria. J Glob Infect Dis. 2010;2(3):263–74.
Onishi R, Shigemura K, Osawa K, Yang YM, Maeda K, Fang SB, Sung SY, Onuma K, Uda A, Miyara T, Fujisawa M. The antimicrobial resistance characteristics of imipenem-non-susceptible, imipenemase-6-producing Escherichia coli. Antibiotics. 2021;11(1):32.
Platteel TN, Beets MT, Teeuwissen HA, Doesschate TT, van de Wijgert JH, Venekamp RP, van de Pol AC. Nitrofurantoin failure in males with an uncomplicated urinary tract infection: a primary care observational cohort study. Br J Gen Pract. 2023;73(728):e204–10.
Ghorashi Z, Ghorashi S, Soltani-Ahari H, Nezami N. Demographic features and antibiotic resistance among children hospitalized for urinary tract infection in northwest Iran. Infect Drug Resist. 2011;4:171–6.
Siegel JD, Rhinehart E, Jackson M, Chiarello L. The Healthcare Infection Control Practices Advisory Committee. Management of multidrug-resistant organisms in health care settings, 2006. Am J Infect Control. 2007;35(10):S165–93.
American Society for Microbiology (ASM). Antibiotic Resistance: An Ecological Perspective on an Old Problem: This report is based on a colloquium, sponsored by the American Academy of Microbiology, convened October 12–14, 2008, at the conference center of the Fondation Mérieux in Annecy, France. 2009. https://www.ncbi.nlm.nih.gov/books/NBK559361/. Accessed 01 Jan 2024.
Dalhoff A. Global Fluoroquinolone Resistance Epidemiology and Implictions for Clinical Use. Interdiscip Perspect Infect Dis. 2012;2012: 976273.
Acknowledgements
We are grateful to the Department of Microbiology of International Friendship Children’s Hospital in Kathmandu for their kind cooperation and support.
Funding
None.
Author information
Authors and Affiliations
Contributions
SP, STK, and DS conceptualized and designed the study methodology. SP and HP collected and analyzed the data, reviewed the literature, and prepared and edited the draft of the manuscript. CA, STK, and DS supervised the entire project and edited the manuscript. DS performed the data analysis and prepared the final version of the manuscript. All the authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study utilized samples obtained during routine patient care investigations for suspected UTIs. Official permission from the hospital administration was obtained to process these samples further, adhering to the hospital's protocols. Demographic data (age, sex, hospital ward) were collected from patients, who were coded and randomized during data entry to safeguard patient privacy. Thus, the data set contained no personally identifiable information. All the research activities adhered to the principles outlined in the Declaration of Helsinki and its later amendments, ensuring ethical standards were upheld in medical research. As such, there were no specific ethical issues warranting special attention during the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pantha, S., Parajuli, H., Arjyal, C. et al. Phenotypic characterization of ESBL-producing urinary isolates of E. coli and Klebsiella spp. in a tertiary care children's hospital in Nepal. Trop Med Health 52, 20 (2024). https://doi.org/10.1186/s41182-024-00587-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41182-024-00587-3