Abstract
Background
Current therapeutic agents, including nifurtimox and benznidazole, are not sufficiently effective in the chronic phase of Trypanosoma cruzi infection and are accompanied by various side effects. In this study, 120 kinds of extracts from medicinal herbs used for Kampo formulations and 94 kinds of compounds isolated from medicinal herbs for Kampo formulations were screened for anti-T. cruzi activity in vitro and in vivo.
Methods
As an experimental method, a recombinant protozoan cloned strain expressing luciferase, namely Luc2-Tulahuen, was used in the experiments. The in vitro anti-T. cruzi activity on epimastigote, trypomastigote, and amastigote forms was assessed by measuring luminescence intensity after treatment with the Kampo extracts or compounds. In addition, the cytotoxicity of compounds was tested using mouse and human feeder cell lines. The in vivo anti-T. cruzi activity was measured by a murine acute infection model using intraperitoneal injection of trypomastigotes followed by live bioluminescence imaging.
Results
As a result, three protoberberine-type alkaloids, namely coptisine chloride, dehydrocorydaline nitrate, and palmatine chloride, showed strong anti-T. cruzi activities with low cytotoxicity. The IC50 values of these compounds differed depending on the side chain, and the most effective compound, coptisine chloride, showed a significant effect in the acute infection model.
Conclusions
For these reasons, coptisine chloride is a hit compound that can be a potential candidate for anti-Chagas disease drugs. In addition, it was expected that there would be room for further improvement by modifying the side chains of the basic skeleton.
Similar content being viewed by others
Background
Chagas disease, caused by a protozoan parasite Trypanosoma cruzi (T. cruzi), is a debilitating illness that affects from 6 to 7 million [1, 2] people mostly in Latin America. The disease is now expanding to non-endemic areas due to human migration [3]. The disease can be categorized into two distinct phases namely: an acute phase and a chronic phase. Acute phase is defined by high parasitemia, fever and lymphadenopathy and is usually resolved within 4–8 weeks [4]. Chronic phase begins after the acute phase and stays asymptomatic for decades (indeterminate phase) until clinical manifestation of the disease developed [3]. About 30–40% of chronically infected individuals develop typical clinical complications which involve cardiac and or gastrointestinal lesions [5].
Chemotherapeutics that are currently used for treatment of the disease are nifurtimox and benznidazole that have been used since 1960 [6, 7]. These drugs have been reported to show limited therapeutic activity against the infection [1] and have low compliance among patients due to the toxic side effects [8]. Still there is no vaccine for Chagas disease currently [9]. Thus, the lack of an efficient drug treatment requires the development of new anti-T. cruzi compound that has improved tolerability, safety, lower toxicity and improved efficacy on both phases of the disease [10].
Traditional Chinese medicine has more than 2000-year history and its standardization has been developed over a long period of time [11]. However, Kampo is a traditional treatment system originated from Chinese medicine was developed in Japan [12, 13]. In general, Kampo herbs are supposed to have a rich resource of active components [14, 15].
In this study, 120 kinds of extracts from medicinal herbs used for Kampo formulations and 94 kinds of compounds isolated from medicinal herbs for Kampo formulations which have been well quality controlled and maintained by Japanese leading research institute, Institute of Natural Medicine, University of Toyama, were screened for their anti-T. cruzi activity in vitro. We have confirmed that the protoberberine-type alkaloids with isoquinoline skeleton, which are the major active components of several plant extracts, showed a significant anti-T. cruzi activity in vitro as well as in vivo.
Methods
Kampo extracts and compounds
The Kampo extracts and compounds library was provided by the Institute of Natural Medicine (The University of Toyama, Toyama, Japan). The library contains 120 kinds of extracts from medicinal herbs used for Kampo formulations and 94 kinds of compounds isolated from medicinal herbs for Kampo formulations (Additional file 1: Table S1, S2, Figs. 1, 2). Ultra-pure water generated by Milli-Q (Merck KGaA, Darmstadt, Germany) was the solvent for all herbal extracts and the concentration was adjusted by dry weight of the extract. Compounds were preserved at a concentration of 10 mM dissolved in dimethyl sulfoxide (DMSO; Wako Pure Chemicals Industrial Ltd, Japan). For more extensive experiments, coptisine chloride was purchased from Toronto Research Chemicals (Canada), and benznidazole was purchased from Sigma-Aldrich (USA). For in vivo administration solvent, 10 mg/ml solution in 7% Tween-80 (Sigma-Aldrich, USA), 3% ethanol (v/v) (Wako Pure Chemicals Industrial Ltd, Japan) and 90% (v/v) Milli-Q water [16] was prepared.
Mammalian control and host cell lines
Newborn mouse heart fibroblast cells (NMH cells) were obtained from Bio-Resource Center, Institute of Tropical Medicine (NEKKEN), Nagasaki University. HuH28 (derived from 37-year-old female) cells [17] were maintained at Chulabhorn International College of Medicine, Thammasat University, Thailand.
Parasites
We used a laboratory strain of T. cruzi which luciferase gene was transfected and integrated named Luc2-Tulahuen originally donated by Professor Takeshi Nara at Iryo Sosei University [18], and were obtained from the bio-resource center at the institute of tropical medicine (NEKKEN) funded by National Bio-resource Project (NBRP) Japan. Epimastigote form of T. cruzi was cultured in liver infusion tryptose (LIT) medium (Liver Infusion Broth (BD 226920), Tryptose (BD 211713), Becton Dickinson, USA) supplemented with 10% fetal bovine serum (FBS) (Gibco, USA), washed human red blood cells (Japan Red Cross Blood Center) and 500 mg/ml of G418 (Thermo Fisher Scientific, USA) at 26 °C until parasites reach to logarithmic stage. T. cruzi epimastigotes partially transformed to metacyclic forms were transferred to confluent NMH cells maintained in minimal essential medium (MEM) (Wako Pure Chemicals Industrial Ltd, Japan) supplemented with 10% newborn calf serum (Thermo Fisher Scientific, USA) at 37 °C and 5% CO2 as described elsewhere [19]. After 48 h incubation, free parasites outside the host cells were washed out and fresh complete MEM was added.
In vitro anti-T. cruzi (trypomastigotes and amastigotes) assay
Luc2-Tulahuen trypomastigotes (3 × 104/well) and NMH cells (5 × 104/well) were mixed into a 96-well white plate. Test samples and controls were added and incubated with the cells for 72 h. NP-40 (Wako Pure Chemicals Industrial Ltd, Japan) was used as the positive control, and a solvent in which the drug was dissolved as a negative. After 72 h of incubation, 100 μl of luciferin solution containing 0.6% NP-40 (Piccagene) (Toyo Ink Group, Japan) was added. Luminescence intensity was measured by a plate reader (ARVO MX 1420) (Measurement time: 1 s) [20].
In vitro anti-T. cruzi (intracellular amastigotes) assay
The intracellular amastigotes assay was described by Alonso-Padilla et al. [21]. Briefly, 6 × 106 trypomastigotes and 3 × 106 host cells (NMH cells) are seeded in a 25 cm2 flask in serum-free media (MEM + 1% newborn calf serum) to enhance the intracellular infection. After 24 h incubation, the cells were washed twice with phosphate buffered saline (PBS), then replaced by MEM + 10% newborn calf serum and incubated for another 24 h. Infected cells were detached by trypsinization. Infected host fibroblast cells (5 × 104/well) were seeded into a 96-well plate. Test samples and the controls were added to the mixture and incubated for 72 h. Luminescence intensity was measured by a plate reader and the Piccagene (Measurement time: 1 s) [22, 23].
In vitro assay for anti-epimastigote form of T. cruzi activity
Luc2-Tulahuen epimastigotes (2 × 105/well) were dispensed into 96-well plate. After 72 h incubation, luminescence intensity was measured by adding lysis buffer with luciferin as substrate (PicaGene Luminescence Kit, Fuji Film Wako chemicals, Japan) (Measurement time: 1 s) [24].
The IC50 was calculated using the following equation:
where A is the lowest concentration at which the percentage inhibition exceeds 50%, B is the highest concentration at which percentage inhibition is less than 50%, and C and D are the percentage inhibition of the sample at concentrations B and A, respectively.
Evaluation of cytotoxicity and measurement of 50% injury concentration
NMH cells or HuH28 cells (1 × 104/well) of 100 μl aliquots were seeded on a 96-well black plate. Test samples were added and incubated for 72 h. NP-40 was added as a positive control (100% cytotoxicity) and a solvent in which the samples were dissolved as a negative control (0% cytotoxicity). Then 10 μl of alamarBlue reagent (10%, Funakoshi Co., Tokyo, Japan) for mitochondria staining was added and incubated for another 4 h. The fluorescence intensity (544 nm/590 nm) was measured with a plate reader (measurement time: 0.1 s).
The concentration required to reduce cell viability by 50% (CC50) was calculated using the following equation:
where A is the lowest concentration at which the cell viability exceeds 50%, B is the highest concentration at which cell viability is less than 50%, and C and D are the cell viability of the sample at concentrations B and A, respectively.
Infection of mice
Mice were housed and maintained in Nagasaki University Biomedical Research Center (12 h light/dark cycle). Female BALB/c mice from 6 to 10 weeks old (20–25 g) were used in all the experiments. Mice were obtained as wild type from SLC (Japan). In standard experiments, 5 × 103 in vitro tissue culture-derived trypomastigotes (TCTs) was intra-peritoneally (i.p.) inoculated into mouse [25,26,27]. The mice were handled according to the international guidelines and institutional guideline of Nagasaki University for the use and maintenance of experimental animals. Ethical approval for this study was obtained from the institutional ethical review board, Nagasaki University (approval number R12005).
Bioluminescence imaging for efficacy evaluation
Mice were intra-peritoneally injected with 150 mg/kg d-luciferin (SYD labs, USA), then anesthetized using 2.5% (vol/vol) gaseous isoflurane in oxygen. To measure bioluminescence, mice were placed in an IVIS Lumina II system (Caliper Life Science, USA) and images were acquired 10 min after d-luciferin administration using LivingImage 4.3 (Caliper Life Sciences, USA). Exposure time was fixed as 5 min. Anesthesia was maintained throughout the imaging process through the nose cone. Whole body luminescence was determined by drawing the region of interest (ROI) and quantifying the bioluminescence expressed as total flux (photons/second; p/s) [16, 28]. Coptisine chloride was administered intra-peritoneally (i.p.) at a dose of 30 mg/kg twice a day. Benznidazole (100 mg/kg) as a positive control and the drug solvent as a negative control were administered orally (p.o.) once a day. Drug was administered for 5 consecutive days from day 4 to 8 of infection. Measurements with IVIS Lumina II were performed at five different times: on day 3 of infection (the day before drug treatment), on day 9 of infection (the day after drug treatment was completed), on day 14, 28 and 40 of infection. To maintain fairness, different experimenters performed drug treatments and luminescence intensity measurements. At day 29, BALB/c mice were injected with cyclophosphamide (Sigma-Aldrich, USA) (200 mg/kg) as an immunosuppressant by i.p. and were followed by a maximum of 3 doses at 3 day intervals [16, 29]. The use of immunosuppressant like cyclophosphamide could help enhance the visibility of the infected lesions even after 100 dpi. In this animal study, treatment was given when the luminescence intensity was high. In addition, an immunosuppressant was administered when the difference in luminescence intensity among the three groups became small due to natural immunity of the mice.
Statistical analysis
Data were tabulated on Microsoft Excel and statistically analyzed. For statistical comparisons, ANOVA analysis was used to determine the statistical significance of difference in values from the control groups. Data were expressed as the mean ± standard error, and the results were obtained from at least three independent experiments. A p-value < 0.05 was considered statistically significant.
Results
In vitro assay
One hundred and twenty extracts and 94 compounds were screened for their cytotoxic effect on the trypomastigotes and amastigotes using a mixture culture experiment (Fig. 1), some sample were shown to exhibit more than 80% reduction of parasite signals. Those positive samples were Phellodendron bark (the bark of Phellodendron amurense Ruprecht) and Coptis rhizome (the rhizome of Coptis japonica Makino, Coptis chinensis Franchet, Coptis deltoidea C.Y. Cheng et Hsiao or Coptis teeta Wallich) from the extracts, Alison B, Alkanin, Berberin chloride, Coptisine chloride, Dehydrocorydaline nitrate, Palmatine chloride, Shikonin and Timosaponin A-III from the compounds indicated by red colored in Fig. 1.
Similar set of the Kampo library was applied to mouse fibroblast cells (NMH) and human bile duct carcinoma cell line (HuH28) to observe any cytotoxic effect on host cells as shown in Fig. 2. Within two extract samples (Phellodendron bark, Coptis rhizome) and 8 compounds samples (Alison B, Alkanin, Berberin chloride, Coptisine chloride, Dehydrocorydaline nitrate, Palmatine chloride, Shikonin, Timosaponin A-III) which showed more than 80% inhibition in the T. cruzi mixture culture (Fig. 1), only three samples (Coptisine chloride, Dehydrocorydaline nitrate, Palmatine chloride) showed relatively lower cytotoxicity (Fig. 2). Therefore, we decided to select those three positive compounds (Coptisine chloride, Dehydrocorydaline nitrate, Palmatine chloride) for further analysis. Those three compounds shared the same isoquinoline skeleton namely coptisine chloride, dehydrocorydaline nitrate, and palmatine chloride.
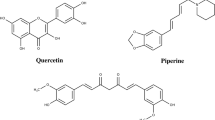
After the first screening as shown in Figs. 1 and 2 as a representative of three repeated experiments, we determined IC50 and CC50 values of the selected candidate compounds. As performed in the first in vitro screening, we used two T. cruzi-culture systems for IC50 as shown in Table 1. For this second screening, we added three more compounds, epiberberine chloride, berberrubine chloride, dl-tetrahydro coptisine to already selected compounds belonging to the same protoberberine-type alkaloids (Fig. 3, Table 1).
The reduced luminescence intensity of luciferin-expressing protozoa suggested that coptisine chloride (IC50: 4.48 μM), dehydrocorydaline nitrate (IC50: 3.47 μM) and palmatine chloride (IC50: 2.66 μM) had an antiprotozoan effect (trypomastigotes in the medium or intracellular amastigotes). It was found to be as effective as benznidazole (IC50: 2.78 μM) in activity quantification (Additional file 1: Fig. S1, Table S1).
Next, the effect on proliferative amastigotes in trypanosomes infected with NMH cells was estimated. Coptisine chloride (IC50: 4.98 μM) was the most effective as benznidazole (IC50: 4.91 μM) due to reduced luminescence intensity in luciferin-expressing protozoa (Additional file 1: Fig. S2, Table S1). On the other hand, coptisine chloride (IC50: 15.1 µM) was fourfold less effective as benznidazole (IC50: 3.78 µM) against epimastigotes (Additional file 1: Fig. S3, Table S1). Cytotoxicity to NMH cells or HuH28 cells was examined for those 6 compounds (Additional file 1: Figs S4, S5). These results indicate that there are differences in the effectiveness of the isoquinoline skeleton depending on the number of methoxy groups and side chains (Fig. 3, Table 1).
In vivo assay
After a 5-day treatment regimen with coptisine chloride (30 mg/kg bid i.p.) from day 4 to 8, the luminescence intensity was significantly reduced in the treated group compared with the untreated group. Though the luminescence intensity of the coptisine chloride group was slightly higher than that of the benznidazole group, still significant reduction was observed, as shown in Figs. 4 and 5. It was found that the luminescence intensity of the coptisine chloride-treated group was significantly reduced even after the immune suppression treatment (day 40) compared with the control group (Figs. 4, 5). Therefore, it was shown that coptisine chloride has a therapeutic effect on the acute phase in vivo model.
Luminescence intensity at different timepoints in the mice model infected with 5 × 103 trypomastigotes and treated with coptisine chloride (COP) (30 mg/kg, 2 × i.p.); positive control is benznidazole (BNZ) (100 mg/kg, 1 × p.o.); negative control is the drug solvent. Bioluminescence imaging was obtained in an IVIS Lumina II system. Data are presented as mean and standard deviation in intensity of three experiments (*p < 0.05, **p < 0.01, ***p < 0.005 when compared with vehicle). In this experiment, we excluded mice with luminescence intensity less than 1 × 107 in pre-drug measurements (Day 3)
Discussion
Chagas disease is expanding to non-endemic areas and an effective treatment is needed. Herbal compounds from traditional medicine are promising candidates for drug development, and their efficacy was demonstrated in our study.
The experimental system of mixing trypomastigotes and NMH cells confirmed the effects on trypomastigotes in the medium and amastigotes in the cells. The reduced luminescence intensity of luciferin-expressing protozoa suggested that coptisine (IC50: 4.48 μM), dehydrocorydaline (IC50: 3.47 μM) and palmatine (IC50: 2.66 μM) had an antiprotozoal effect. It was found to be as effective as benznidazole (IC50: 2.78 μM) in activity quantification (Table 1). The experiment mimics the acute phase of the disease with trypomastigotes in the blood and amastigotes in the cells [30, 32]. As a result, these compounds are thought to be effective in the acute phase. In addition, Phellodendron bark and Coptis rhizome showed more than 80% inhibition in the T. cruzi mixture culture (Fig. 1). However, these extracts also showed cytotoxicity. These consist of berberine, coptisine and palmatine. The cytotoxicity of Phellodendron bark and Coptis rhizome may be attributed to berberine.
However, the urgent requirement from the present clinical setting in the world is to get an effective curative drug for chronic phase infection [1,2,3]. Therefore, future work will focus on testing the Kampo compounds in the chronic stage of infection.
The experimental system for intracellular amastigotes using NMH cells allowed us to confirm the effect on proliferative amastigotes in trypanosomes-infected NMH cells which mimics the chronic phase of the disease [31, 32]. Coptisine (IC50: 4.98 μM) showed comparable levels of IC50 as benznidazole (IC50: 4.91 μM) (Table 1). Although we have not yet examined in vivo chronic Chagas model, coptisine was revealed to be a possible candidate for an effective drug in the chronic phase.
As shown in Table 1, other related protoberberine-type alkaloids, dehydrocorydaline and palmatine showed strong activity in the mixture experiment with trypomastigote, amastigote and NMH, but not against intracellular amastigotes. When those three active compounds were examined for their cytotoxicity on epimastigote, they showed almost equal effectiveness of IC50 around 15–20 μM, which were less effective compared with benznidazole (3.78 μM). Therefore, coptisine is specifically more active to amastigote than to epimastigote, whereas benznidazole shows both stages active. In addition, three active protoberberine-type alkaloids showed equal cytotoxicity on the T. cruzi epimastigote cells, but the effect on the intracellular amastigote significantly increased in only coptisine which might be due to the increased permeability through host cell membrane.
Although comparison on the activities of tested compounds did not show clear structure–activity relationships, following trends were observed. The presence of methylenedioxy at rings A (at C-2 and 3) and D (C-9 and 10) and aromatization of ring C could be the key factor for the anti-Trypanosoma cruzi activity. However, the effects of the presence of methylenedioxy or methoxy groups of rings A/D were not clear. The presence of methyl group at C-13 may reduce the anti-Trypanosoma cruzi activity on the intracellular amastigote. The presence of a hydroxy group at C-9 may reduce the activity. To clarify the structure–activity relationships of the protoberberine-type alkaloids on anti-Trypanosoma cruzi activity, further studies using more diverse derivatives are required.
In animal experiments, we confirmed the equivalent parasiticidal activity of coptisine as benznidazole as evidenced by the reduction in luminescence intensity shown in Figs. 4 and 5. In addition, the relapse detected on day 40 after administration of the immunosuppressant during a period between day 30 and 39 was smaller than that in the benznidazole treatment group. This suggests that coptisine was more effective to reduce the number of parasites compared with the current standard curative protocol of benznidazole in the acute model [28]. Taken together, coptisine is a novel anti-Trypanosoma cruzi compound with an equivalent effectiveness as benznidazole when examined in vitro acute and chronic and by in vivo acute model. Our results also indicate that berberine structure with an isoquinoline skeleton might be used for more effective compounds design by the modification of side chains.
It has been reported that coptisine chloride or protoberberine-type alkaloids has various pharmaceutical effects such as anti-cancer [36, 37], anti-inflammation, and anti-diabetic as well as anti-infectious diseases [33,34,35, 38, 39]. Coptisine non-competitively inhibits DHODH in Plasmodium falciparum and showed weak inhibitory activity against human DHODH [35]. T. cruzi DHODH, which catalyzes the production of orotate, and was demonstrated to be essential for T. cruzi survival, could be one of our coptisine’s potential targets [40,41,42].
It has been reported that coptisine chloride possesses anti-cancer activity through the inhibition of PI3K/Akt/mTOR signaling and subsequent mitochondrial ROS production in the hepatocellular cancer Hep3B cells [36, 37]. T. cruzi infection has been demonstrated to stimulate host PI3K signaling in human and mice macrophages that allow intracellular parasites to grow and survive [43,44,45,46,47]. These reports suggest that inhibition of PI3K/Akt/mTOR signaling by coptisine chloride may have affected the growth and survival of intracellular parasites. Coptisine chloride has also been reported to inhibit LPS-stimulated inflammation by blocking the activation of NF-κB and MAPK in macrophages [48,49,50,51]. In coptisine chloride therapy for colitis, coptisine chloride significant suppresses mRNA expression, releases of pro-inflammatory cytokines (TNF-α, IFN-γ, IL-1β, IL-6, IL-17) and enhances the mRNA expression level of IL-10, an anti-inflammatory cytokine [52, 53].
T. cruzi infection could stimulate both protective and pathogenic host immune responses through natural or adaptive immunological pathways [54,55,56,57,58,59]. Although we did not see any significant adverse events during in vivo experiment, previously reported immune inhibitory effects of coptisine should be carefully observed.
When considering drug development, the target product profile (TPP) is important, and oral administration is preferable for aiming a therapeutic drug for chronic Chagas disease that may need at least 2 weeks regimen. However, it is known that the oral bioavailability of coptisine chloride is low [60]. It is necessary to investigate whether these problems can be solved by improving the side chain or enclosing the compound to improve the blood concentration.
In the present study, we identified a series of protoberberine-type alkaloids as strong candidate anti-Trypanosoma cruzi medicine using in vitro and in vivo models. Among them, coptisine was expected to be the most effective candidate compound.
The model mouse used this time has poor persistence of luminescence intensity, and it is considered difficult to measure in the chronic phase. However, it may be possible to measure the chronic phase using new recombinant protozoa. In this study, we found that compounds identified in vitro are also effective in vivo. Since chronic Chagas treatment is a typical neglected tropical disease unmet needs [61, 62], further development must be facilitated.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- IC50:
-
Half-maximal inhibitory concentration
- DMSO:
-
Dimethyl sulfoxide
- NMH:
-
Newborn mouse heart fibroblast
- IP:
-
Intraperitoneal injection
- PO:
-
Per OS
- PBS:
-
Phosphate buffered saline
- NP40:
-
Nonyl phenoxypolyethoxylethanol 40
- LIT:
-
Liver infusion tryptose
- FBS:
-
Fetal bovine serum
- NBCS:
-
Newborn calf serum
- MEM:
-
Minimum essential medium
- TCTs:
-
Tissue culture-derived trypomastigotes
- BNZ:
-
Benznidazole
- COP:
-
Coptisine chloride
References
World Health Organization. Chagas diseases in Latin America: an epidemiological update based on 2010 estimates. Wkly Epidemiol Rec. 2015;90(6):33–44.
World Health Organization 2021, ‘Chagas disease (American trypanosomiasis)’, viewed 20 of January 2021, http://www.who.int/chagas/disease/en/.
Lewis MD, Fortes Francisco A, Taylor MC, Burrell-Saward H, McLatchie AP, Miles MA, Kelly JM. Bioluminescence imaging of chronic Trypanosoma cruzi infections reveals tissue-specific parasite dynamics and heart disease in the absence of locally persistent infection. Cell Microbiol. 2014;16(9):1285–300.
Hyland KV, Asfaw SH, Olson CL, Daniels MD, Engmana DM. Bioluminescent imaging of Trypanosoma cruzi infection. Int J Parasitol. 2008;38(12):1391–400.
Machado FS, Dutra WO, Esper L, Gollob KJ, Teixeira MM, Factor SM, Weiss LM, Nagajyothi F, Tanowitz HB, Garg NJ. Current understanding of immunity to Trypanosoma cruzi infection and pathogenesis of Chagas disease. Semin Immunopathol. 2012;34(6):753–70.
Schmunis GA, Yadon ZE. Chagas disease: a Latin American health problem becoming a world health problem. Acta Trop. 2010;115(1–2):14–21.
Moraes CB, Giardini MA, Kim H, Franco CH, Araujo-Junior AM, Schenkman S, Chatelain E, Freitas-Junior LH. Nitroheterocyclic compounds are more efficacious than CYP51 inhibitors against Trypanosoma cruzi: implications for Chagas disease drug discovery and development. Sci Rep. 2014;4:4703.
Palmeiro-Roldán R, Fonseca-Berzal C, Gómez-Barrio A, Arán VJ, Escario JA, Torrado-Durán S, Torrado-Santiago S. Development of novel benznidazole formulations: physicochemical characterization and in vivo evaluation on parasitemia reduction in Chagas disease. Int J Pharm. 2014;472(1–2):110–7.
Díaz-Chiguer DL, Márquez-Navarro A, Nogueda-Torres B, de la Luz G, León-Ávila J-V, Hernández-Campos A. In vitro and in vivo trypanocidal activity of some benzimidazole derivatives against two strains of Trypanosoma cruzi. Acta trop. 2012;122(1):108–12.
Lascano F, Bournissen FG, Altcheh J. Review of pharmacological options for the treatment of Chagas disease. Br J Clin Pharmacol. 2022;88(2):383–402.
Cheng JT. Drug therapy in Chinese traditional medicine. J Clin Pharmacol. 2000;40(5):445–50.
Hoffmann KM, Herbrechter R, Ziemba PM, Lepke P, Beltrán L, Hatt H, Werner M, Gisselmann G. Kampo medicine: evaluation of the pharmacological activity of 121 herbal drugs on GABAA and 5-HT3A receptors. Front Pharmacol. 2016;7:219.
Chen X, Xiang L, Shi L, Li G, Yao H, Han J, Lin Y, Song J, Chen J. Identification of crude drugs in the Japanese pharmacopoeia using a DNA barcoding system. Sci Rep. 2017;7:42325.
Li F-S, Weng J-K. Demystifying traditional herbal medicine with modern approach. Nat Plants. 2017;3:17109.
Pan S-Y, Litscher G, Gao S-H, Zhou S-F, Zhi-Ling Yu, Chen H-Q, Zhang S-F, Tang M-K, Sun J-N, Ko K-M. Historical perspective of traditional indigenous medical practices: the current renaissance and conservation of herbal resources. Evid Based Complementary Altern Med. 2014;2014: 525340.
Francisco AF, Lewis MD, Jayawardhana S, Taylor MC, Chatelain E, Kelly JM. Limited ability of posaconazole to cure both acute and chronic Trypanosoma cruzi infections revealed by highly sensitive in vivo imaging. Antimicrob Agents Chemother. 2015;59(8):4653–61.
Narahara C, Saeheng T, Chaijaroenkul W, Dumre SP, Na-Bangchang K, Karbwang J. β-Eudesmol induces the expression of apoptosis pathway proteins in cholangiocarcinoma cell lines. J Res Med Sci. 2020;25:7.
Hashimoto M, Morales J, Fukai Y, Suzuki S, Takamiya S, Tsubouchi A, Inoue S, Inoue M, Kita K, Harada S, Tanaka A, Aoki T, Nara T. Critical importance of the de novo pyrimidine biosynthesis pathway for Trypanosoma cruzi growth in the mammalian host cell cytoplasm. Biochem Biophys Res Commun. 2012;417(3):1002–6.
Tani O, Akutsu Y, Ito S, Suzuki T, Tateishi Y, Yamaguchi T, Niimi T, Namatame I, Chiba Y, Sakashita H, Kubota T, Yanagi T, Mizukami S, Hirayama K, Furukawa K, Yamasaki K. NMR biochemical assay for oxidosqualene cyclase: evaluation of inhibitor activities on Trypanosoma cruzi and human enzymes. J Med Chem. 2018;61(11):5047–53.
Bettiol E, Samanovic M, Murkin AS, Raper J, Buckner F, Rodriguez A. Identification of three classes of heteroaromatic compounds with activity against intracellular Trypanosoma cruzi by chemical library screening. PloS Negl Trop Dis. 2009;3(2): e384.
Alonso-Padilla J, Cotillo I, Presa JL, Cantizani J, Peña I, Bardera AI, Martín JJ, Rodriguez A. Automated high-content assay for compounds selectively toxic to Trypanosoma cruzi in a myoblastic cell line. PLoS Negl Trop Dis. 2015;9(1): e0003493.
De Rycker M, Thomas J, Riley J, Brough SJ, Miles TJ, Gray DW. Identification of trypanocidal activity for known clinical compounds using a new Trypanosoma cruzi hit-discovery screening cascade. PLoS Negl Trop Dis. 2016;10(4): e0004584.
Imanol Peña M, Manzano P, Cantizani J, Kessler A, Alonso-Padilla J, Bardera AI, Alvarez E, Colmenarejo G, Cotillo I, Roquero I, de Dios-Anton F, Barroso V, Rodriguez A, Gray DW, Navarro M, Kumar V, Sherstnev A, Drewry DH, Brown JR, Fiandor JM, Julio Martin J. New compound sets identified from high throughput phenotypic screening against three kinetoplastid parasites: an open resource. Sci Rep. 2015;5:8771.
Zuma AA, da Silva RB, Simon J, Garden SJ, de Souza W. In vitro study of the trypanocidal activity of anilinophenanthrolines against Trypanosoma cruzi. Parasitol Int. 2021;83:102338.
Caldas S, Caldas IS, de Figueiredo DL, de Lima WG, de Paula OR, Cecílio AB, Ribeiro I, Talvani A, Bahia MT. Real-time PCR strategy for parasite quantification in blood and tissue samples of experimental Trypanosoma cruzi infection. Acta Trop. 2012;123(3):170–7.
Assíria Fontes Martins T, de Figueiredo Diniz L, Mazzeti AL, da Silva do Nascimento AF, Caldas S, Caldas IS, de Andrade IM, Ribeiro I, Bahia MT. Benznidazole/itraconazole combination treatment enhances anti-Trypanosoma cruzi activity in experimental Chagas disease. PLoS ONE. 2015;10(6):e0128707.
Novaes RD, Santos EC, Cupertino MC, Bastos DS, Oliveira JM, Carvalho TV, Neves MM, Oliveira LL, Talvani A. Trypanosoma cruzi infection and benznidazole therapy independently stimulate oxidative status and structural pathological remodeling of the liver tissue in mice. Parasitol Res. 2015;114(8):2873–81.
Francisco AF, Jayawardhana S, Lewis MD, White KL, Shackleford DM, Chen G, Saunders J, Osuna-Cabello M, Read KD, Charman SA, Chatelain E, Kelly JM. Nitroheterocyclic drugs cure experimental Trypanosoma cruzi infections more effectively in the chronic stage than in the acute stage. Sci Rep. 2016;6:35351.
Bahia MT, Nascimento AF, Mazzeti AL, Marques LF, Gonçalves KR, Mota LW, Diniz LD, Caldas IS, Talvani A, Shackleford DM, Koltun M, Saunders J, White KL, Scandale I, Charman SA, Chatelain E. Antitrypanosomal activity of fexinidazole metabolites, potential new drug candidates for Chagas disease. Antimicrob Agents Chemother. 2014;58(8):4362–70.
Teixeira AR, Hecht MM, Guimaro MC, Sousa AO, Nitz N. Pathogenesis of Chagas’ disease: parasite persistence and autoimmunity. Clin Microbiol Rev. 2011;3:592–630.
Coura JR, Borges-Pereira J. Chagas disease: 100 years after its discovery. A systemic review. Acta Trop. 2010;115(1–2):5–13.
Kirchhoff L. Chagas Disease (American Trypanosomiasis) Clinical Presentation: History, Physical, Causes [Internet]. Emedicine.medscape.com. 2019 [cited 9 July 2021]. Available from: https://emedicine.medscape.com/article/214581-clinical.
Zhang Z, Deng A, Yu J. Current research status on pharmacological activities of coptisine. China J Chin Mater Med. 2013:2750–2754.
Jiasi Wu, Luo Yu, Deng D, Siyu Su, Li S, Xiang Li, Yingfan Hu, Wang P, Meng X. Coptisine from Coptis chinensis exerts diverse beneficial properties: a concise review. J Cell Mol Med. 2019;12:7946–60.
Lang L, Hu Q, Wang J, Liu Z, Huang J, Lu W, Huang Y. Coptisine, a natural alkaloid from Coptidis Rhizoma, inhibits plasmodium falciparum dihydroorotate dehydrogenase. Chem Biol Drug Des. 2018;92(1):1324–32.
Kim SY, Hwangbo H, Kim MY, Ji SY, Lee H, Kim G-Y, Kwon C-Y, Leem SH, Hong SH, Cheong JH, Choi YH. Coptisine induces autophagic cell death through down-regulation of PI3K/Akt/mTOR signaling pathway and up-regulation of ROS-mediated mitochondrial dysfunction in hepatocellular carcinoma Hep3B cells. Arch Biochem Biophys. 2021;697: 108688.
Kim SY, Hwangbo H, Lee H, Park C, Kim G-Y, Moon S-K, Yun SJ, Kim W-J, Cheong J, Choi YH. Induction of apoptosis by coptisine in Hep3B hepatocellular carcinoma cells through activation of the ROS-mediated JNK signaling pathway. Int J Mol Sci. 2020;21(15):5502.
Teklemichael AA, Mizukami S, Toume K, Mosaddeque F, Kamel MG, Kaneko O, Komatsu K, Karbwang J, Huy NT, Hirayama K. Anti-malarial activity of traditional Kampo medicine Coptis rhizome extract and its major active compounds. Malar J. 2020;19(1):204.
Nonaka M, Murata Y, Takano RY, Han Y, Bin Kabir MH, Kentaro Kato K. Screening of a library of traditional Chinese medicines to identify anti-malarial compounds and extracts. Malar J. 2018;17(1):244.
Cheleski J, Rocha JR, Pinheiro MP, Wiggers HJ, da Silva ABF, Nonato MC, Montanari CA. Novel insights for dihydroorotate dehydrogenase class 1A inhibitors discovery. Eur J Med Chem. 2010;45(12):5899–909.
Munier-Lehmann H, Vidalain PO, Tangy F, Janin YL. On dihydroorotate dehydrogenases and their inhibitors and uses. J Med Chem. 2013;56(8):3148–67.
Inaoka DK, Iida M, Hashimoto S, Tabuchi T, Kuranaga T, Balogun EO, Honma T, Tanaka A, Harada S, Nara T, Kita K, Inoue M. Design and synthesis of potent substrate-based inhibitors of the Trypanosoma cruzi dihydroorotate dehydrogenase. Bioorg Med Chem. 2017;25(4):1465–70.
Chuenkova MV, PereiraPerrin M. Trypanosoma cruzi targets Akt in host cells as an intracellular antiapoptotic strategy. Sci Signal. 2009;2(97):ra74.
Wilkowsky SE, Barbieri MA, Stahl P, Isola EL. Trypanosoma cruzi: phosphatidylinositol 3-kinase and protein kinase B activation is associated with parasite invasion. Exp Cell Res. 2001;264(2):211–8.
Todorov AG, Einicker-Lamas M, de Castro SL, Oliveira MM, Guilherme A. Activation of host cell phosphatidylinositol 3-kinases by Trypanosoma cruzi infection. J Biol Chem. 2000;275(41):32182–6.
López-Peláez M, Soria-Castro I, Boscá L, Fernández M, Alemany S. Cot/tpl2 activity is required for TLR-induced activation of the Akt p70 S6k pathway in macrophages: implications for NO synthase 2 expression. Eur J Immunol. 2011;41(6):1733–41.
Silva MC, Davoli-Ferreira M, Medina TS, Sesti-Costa R, Silva GK, Lopes CD, Cardozo LE, Gava FN, Lyroni K, Dias FC, Frade AF, Baron M, Nakaya HI, Figueiredo F, Alves-Filho JC, Cunha FQ, Tsatsanis C, Chevillard C, Cunha-Neto E, Hirsch E, Silva JS, Cunha TM. Canonical PI3Kγ signaling in myeloid cells restricts Trypanosoma cruzi infection and dampens chagasic myocarditis. Nat Commun. 2018;9(1):1513.
Jiasi Wu, Zhang H, Boyang Hu, Yang L, Wang P, Wang F, Meng X. Coptisine from Coptis chinensis inhibits production of inflammatory mediators in lipopolysaccharide-stimulated RAW 264.7 murine macrophage cells. Eur J Pharmacol. 2016;780:106–14.
Chen H-B, Luo C-D, Liang J-L, Zhang Z-B, Lin G-S, Jia-Zhen Wu, Li C-L, Tan L-H, Yang X-B, Zi-Ren Su, Xie J-H, Zeng H-F. Anti-inflammatory activity of coptisine free base in mice through inhibition of NF-κB and MAPK signaling pathways. Eur J Pharmacol. 2017;811:222–31.
Zou Z-Y, Yin-Ran Hu, Ma H, Wang Y-Z, He K, Xia S, Hao Wu, Xue D-F, Li X-G, Ye X-L. Coptisine attenuates obesity-related inflammation through LPS/TLR-4-mediated signaling pathway in Syrian golden hamsters. Fitoterapia. 2015;105:139–46.
Zhou K, Hu LI, Liao W, Yin D, Rui F. Coptisine prevented IL-β-induced expression of inflammatory mediators in chondrocytes. Inflammation. 2016;39(4):1558–65.
Ai G, Huang Z, Cheng J, Xie J, Zeng H, Liu Y, Li Y, Huang X, Chen J, Ziren Su. Gut microbiota-mediated transformation of coptisine into a novel metabolite 8-oxocoptisine: insight into its superior anti-colitis effect. Front Pharmacol. 2021;12: 639020.
Wang Y, Liu J, Huang Z, Li Y, Liang Y, Luo C, Ni C, Xie J, Ziren Su, Chen J, Li C. Coptisine ameliorates DSS-induced ulcerative colitis via improving intestinal barrier dysfunction and suppressing inflammatory response. Eur J Pharmacol. 2021;896: 173912.
Campos MA, Closel M, Valente EP, Cardoso JE, Akira S, Alvarez-Leite JI, Ropert C, Gazzinelli RT. Impaired production of proinflammatory cytokines and host resistance to acute infection with Trypanosoma cruzi in mice lacking functional myeloid differentiation factor 88. J Immunol. 2004;172(3):1711–8.
Mukherjee S, Huang H, Petkova SB, Albanese C, Pestell RG, Braunstein VL, Christ GJ, Wittner M, Lisanti MP, Berman JW, Weiss LM, Tanowitz HB. Trypanosoma cruzi infection activates extracellular signal-regulated kinase in cultured endothelial and smooth muscle cells. Infect Immun. 2004;72(9):5274–82.
Soto CD, Solana ME, Poncini CV, Pino-Martinez AM, Tekiel V, González-Cappa SM. Dendritic cells devoid of IL-10 induce protective immunity against the protozoan parasite Trypanosoma cruzi. Vaccine. 2010;28(46):7407–13.
Suman S, Rachakonda G, Mandape SN, Sakhare SS, Villalta F, Pratap S, Lima MF, Nde PN. Phospho-proteomic analysis of primary human colon epithelial cells during the early Trypanosoma cruzi infection phase. PLoS Negl Trop Dis. 2018;12(9): e0006792.
Wan X, Wen JJ, Koo SJ, Liang LY, Garg NJ. SIRT1-PGC1α-NFκB pathway of oxidative and inflammatory stress during Trypanosoma cruzi infection: benefits of SIRT1-targeted therapy in improving heart function in Chagas disease. PLoS Pathog. 2016;12(10): e1005954.
Vásquez VC, Russomando G, Espínola EE, Sanchez Z, Mochizuki K, Roca Y, Revollo J, Guzman A, Quiroga B, Rios Morgan S, Vargas Ortiz R, Zambrana Ortega A, Espinoza E, Nishizawa JE, Kamel MG, Kikuchi M, Mizukami S, Na-Bangchang K, Tien Huy N, Hirayama K. IL-17A, a possible biomarker for the evaluation of treatment response in Trypanosoma cruzi infected children: a 12-months follow-up study in Bolivia. PLoS Negl Trop Dis. 2019;13(9): e0007715.
Kheir MM, Wang Y, Hua L, Jun Hu, Li L, Lei F, Lijun Du. Acute toxicity of berberine and its correlation with the blood concentration in mice. Food Chem Toxicol. 2010;48(4):1105–10.
Francisco AF, Jayawardhana S, Olmo F, Lewis MD, Wilkinson SR, Taylor MC, Kelly JM. Challenges in Chagas disease drug development. Molecules. 2020;25(12):2799.
Beltran-Hortelano I, Alcolea V, Font M, Pérez-Silanes S. Examination of multiple Trypanosoma cruzi targets in a new drug discovery approach for Chagas disease. Bioorg Med Chem. 2022;58:116577.
Acknowledgements
The authors thank the Institute of Natural Medicine (The University of Toyama, Toyama, Japan) for providing the natural drug library.
Funding
Financial support interims of experimental chemicals, laboratory instruments and the Animal house facility was provided by the Joint Usage/Research Center on Tropical Disease, Institute of Tropical Medicine, Nagasaki University (29-Ippan-17, 2018-Ippan-21), on Science-Based Natural Medicine. And We received funding from Institute of Natural Medicine, University of Toyama (Ippan Kenkyu I) for providing compounds and purchasing materials for experiments.
Author information
Authors and Affiliations
Contributions
YT and SM performed the experiments, analyzed the data. KT, KK, TN and TY provided experimental materials and provided technical advice on experimental design and data collection. YT, NTH and KH wrote the manuscript initial draft. PT, KT and KK edited the manuscript. SH and KH provided instructions for the experiments. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Female BALB/c mice aged 6–10 weeks (n = 18) were obtained from SLC (Japan). The total number of mice was determined from the results of previous experiments. (Calculate the mean and standard deviation, and calculate the number of samples for which a significant difference can be determined.) Mice were housed in 3 per cage. The mice were raised under the following conditions: 12 h light/dark cycles, temperature of 23 + 2 °C, and relative humidity of 55%, at the Nagasaki University Animal House Facility; food and water were provided freely. The mice were randomly divided into three groups: control (n = 6), benznidazole (n = 6) and coptisine (n = 6) groups. All experiments were approved and performed according to the guidelines of the Care and Use of Laboratory Animals of the University of Nagasaki (approval number R12005). Mice were observed daily during the experiment to check for rapid weight loss and sudden mouse death. Prior to being subjected to experimentation or killing, the mice received isoflurane inhalation to minimize suffering. All methods were reported in accordance with the ARRIVE guidelines (https://arriveguidelines.org).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary tables and figures.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tayama, Y., Mizukami, S., Toume, K. et al. Anti-Trypanosoma cruzi activity of Coptis rhizome extract and its constituents. Trop Med Health 51, 12 (2023). https://doi.org/10.1186/s41182-023-00502-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41182-023-00502-2