Abstract
Background
The Philippines has been one of the most affected COVID-19 countries in the Western Pacific region, but there are limited data on COVID-19-related mortality and associated factors from this setting. We aimed to describe the epidemiological and clinical characteristics and associations with mortality among COVID-19-confirmed individuals admitted to an infectious diseases referral hospital in Metro Manila.
Main text
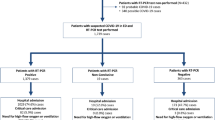
This was a single-centre retrospective analysis including the first 500 laboratory-confirmed COVID-19 individuals admitted to San Lazaro Hospital, Metro Manila, Philippines, from January to October 2020. We extracted clinical data and examined epidemiological and clinical characteristics and factors associated with in-hospital mortality. Of the 500 individuals, 133 (26.6%) were healthcare workers (HCW) and 367 (73.4%) were non-HCW, with HCW more likely presenting with milder symptoms. Non-HCW admissions were more likely to have at least one underlying disease (51.6% vs. 40.0%; p = 0.002), with hypertension (35.4%), diabetes (17.4%), and tuberculosis (8.2%) being the most common. Sixty-one (12.2%) died, comprising 1 HCW and 60 non-HCW (0.7% vs. 16.3%; p < 0.001). Among the non-HCW, no death occurred for the 0–10 years age group, but deaths were recorded across all other age groups. Compared to those who recovered, individuals who died were more likely to be older (p < 0.001), male (p = 0.015), report difficulty of breathing (p < 0.001), be HIV positive (p = 0.008), be intubated (p < 0.001), categorised as severe or critical (p < 0.001), have a shorter mean hospital stay (p < 0.001), or have an additional diagnosis of pneumonia (p < 0.001) or ARDS (p < 0.001).
Conclusion
Our analysis reflected significant differences in characteristics, symptomatology, and outcomes between healthcare and non-healthcare workers. Despite the unique mix of cohorts, our results support the country’s national guideline on COVID-19 vaccination which prioritises healthcare workers, the elderly, and people with comorbidities and immunodeficiency states.
Similar content being viewed by others
Background
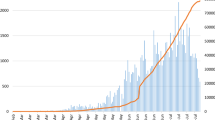
The COVID-19 pandemic caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is now in its second year [1, 2]. The Philippines, already with a high burden of infectious disease [3], has been one of the hardest hit countries in the Western Pacific region [4]. As of April 2021, the densely populated National Capital Region (NCR) has been the epicentre of COVID-19, contributing to almost half the cases in the Philippines [5, 6]. Significant progress has been made in a short period of time in terms of understanding the virus’ pathogenesis, transmission, and symptomatology [7, 8]. Therapeutic modalities have been evaluated and vaccines developed [9,10,11]. While initial doses of the COVID-19 vaccine have been given to priority populations (healthcare workers, the elderly, and those with comorbidities) in the Philippines since March 2021 [9, 10], only 739,000 individuals had received at least one dose of vaccine, comprising < 1% of the total population [9]. Hospitals in the NCR are still experiencing a heavy influx of patients presenting with severe to critical symptoms of COVID-19. One way to help alleviate the burden in the hospitals is to further identify those who would benefit most from the available COVID-19 vaccines. While numerous publications are available for Western and high-income settings, to date, there are still limited and underrepresented data among Filipinos and Asians in low-resource settings.
We previously reported an analysis of the first 100 individuals with suspected COVID-19 admitted to San Lazaro Hospital (SLH), a tertiary infectious diseases hospital in Metro Manila, during the first months of the pandemic [11]. Being the national infectious disease referral centre in the country, SLH caters mostly to patients with communicable diseases. When the pandemic started, adjustments in the admission policy were made to provide care to COVID-19 patients, particularly prioritising healthcare workers serving as frontliners in the fight against the disease. The policy for admission has changed over time, with subsequent revisions in the criteria for admission (i.e. cases with mild symptoms are isolated at home or in an isolation facility and not admitted to a hospital) in order to prioritise those with more severe presentations. In this follow-up paper, we aim to describe the epidemiological and clinical characteristics and associations with mortality among the first 500 laboratory-confirmed COVID-19 inpatients from the same hospital, with a view to identifying individuals most at risk who could be prioritised for vaccination.
Main text
We conducted a secondary analysis of the first 500 laboratory-confirmed COVID-19 inpatients at SLH, from January 25, 2020, to October 24, 2020. Anonymised data on confirmed and suspected cases within the hospital from COVID-19 case investigation forms (CIF) were provided by the SLH Epidemiology Department (SLH-ED). We limited our analysis to individuals with complete data on case classification and patient outcome. Clinical status (asymptomatic, mild, moderate, severe) was assessed according to the Philippine Department of Health’s Interim Guidelines on the COVID-19 Disease Severity Classification and Management [12]. Available laboratory data on cycle threshold (Ct) value was collected from the hospital’s laboratory department. The Philippines’ Department of Health (DOH) defines a “confirmed case” of COVID-19 as “any individual, irrespective of the presence or absence of clinical signs and symptoms, who is laboratory-confirmed for COVID-19 in a test conducted at the national or subnational reference laboratory, and/or officially accredited laboratory testing facility”. For the purpose of this analysis, we included individuals categorised in the CIF as confirmed cases of COVID-19. We clarified any unclear information in the dataset with the staff of the SLH-ED. We analysed the descriptive statistics of cases, deaths, and recoveries by socio-demographics and clinical presentation. We used proportions and percentages to describe the characteristics of the study population. Continuous data were described as means (standard deviation (SD)) if the data was normally distributed; otherwise, medians (interquartile range) were used. We calculated time in days from the onset of symptoms to hospital admission, and length of hospitalisation until death or discharge. Categorical variables were analysed using χ2 testing. Analysis of associations with mortality was restricted to non-healthcare workers, given that all the deaths apart from one occurred in this group. Stata IC 16.1 was used for all analyses. The study was approved by the SLH research ethics and review unit (Ref: SLH-RERU-2020-022-I) and the School of Tropical Medicine and Global Health, Nagasaki University Ethical Committee (NU_TMGH_2020_119_1).
Table 1 presents the epidemiological and clinical characteristics of the 500 individuals included in the analysis, comparing 133 (26.6%) HCW and 367 (73.4%) non-HCW. Most were aged over 20 with a median age of 48 years (IQR 34–61). HCW tended to be younger (p < 0.001). All 16 individuals aged under 20 were non-HCW. Just over half were males (55.8%), similar for both groups. All (99.6%) were Filipino nationals apart from two individuals from China. The majority (73.0%) could not identify a possible exposure to COVID-19; however, HCW were more likely to report risk of exposure in the workplace (p < 0.001). Non-HCW were more likely to have at least one underlying disease (55.9% vs. 40.0%; p = 0.002), with hypertension (38.1%), diabetes (20.2%), and tuberculosis (10.1%) being the most common. The predominant symptoms among the admitted cases were cough (76.2%), fever (56.2%), and difficulty of breathing (37.0%). Non-HCW were more likely to have symptoms of fever (p < 0.001), cough (p < 0.001), difficulty of breathing (p < 0.001), malaise or fatigue (p = 0.034), and loss of appetite (p < 0.002), whereas HCW were more likely to report coryzal symptoms (p = 0.003). All admitted individuals had symptoms. HCW were more likely to be classified as mild or moderate whereas non-HCW were more likely to be severe or critical cases (p < 0.001). Twenty-nine (5.8%) individuals needed mechanical ventilator support, all non-HCW. The median duration between the onset of symptoms to admission was 6 days (IQR 4–9 days), less for HCW compared with non-HCW (5.5 days vs. 7 days; p < 0.001). The median duration of hospital stay was 10 days (IQR 7–14 days) with no difference between HCW and non-HCW. HCW were more likely to be admitted within 14 days from the symptom onset than non-HCW (96.9% vs. 87.8%; p < 0.016). Ct-values for the RT-PCR results were available for 332 (66.4%) individuals. The majority of Ct-values are within the range of 31–40 (67.9%) with no difference between HCW and non-HCW. Additional diagnoses were more common among non-HCW than among HCW: pneumonia (49.3% vs. 16%; p < 0.001) and acute respiratory distress syndrome (ARDS) (13.3% vs. 3%; p = 0.001). Among the 500 COVID-19-confirmed cases, 61 (12.2%) died. Mortality was higher among non-HCW compared with HCW (16.3% vs. 0.7%; p < 0.001).
Table 2 shows the characteristics of the 367 non-HCW by mortality. No death occurred for the 0–10 years age group, but deaths were recorded across all other age groups. Compared to those who recovered, individuals who died were more likely to be older (p < 0.001), male (p = 0.015), report difficulty of breathing (p < 0.001), be HIV positive (p = 0.008), be intubated (p < 0.001), categorised as severe or critical (p < 0.001), have a shorter mean hospital stay (p < 0.001), or have an alternative diagnosis of pneumonia (p < 0.001) or ARDS (p < 0.001). There were no significant associations in mortality by nationality, exposure history, duration between onset of symptoms and admission, and Ct-value.
Conclusions
In this study, we describe the epidemiological and clinical characteristics of the first 500 confirmed COVID-19 individuals admitted to an infectious disease referral hospital in Metro Manila. There were significant differences in characteristics, symptomatology, and outcomes between healthcare and non-healthcare workers. This likely reflects the changes in policy for admission and access to testing, with many frontline healthcare workers with mild symptoms admitted to the hospital in the early days of the epidemic [13]. Non-healthcare workers were more likely to report cough, fever, and difficulty of breathing and have pneumonia and more severe disease [14, 15].
The mortality rate among non-HCW was 16.4%, comparable to the 17.5% mortality reported among the first 200 COVID-19 cases at the Philippine General Hospital and a similar population in Indonesia with a mortality rate of 12% [15, 16], but lower compared to those reported in large cohorts in high-income countries [17, 18]. Older age was associated with mortality as consistently reported elsewhere [14, 17, 18]. The presence of an underlying illness among COVID-19 non-HCW (82.4%) is similar to other case series reported in North America (88%) [17] and the UK (77.5%) [18], but comorbidities of diabetes and hypertension were not associated with mortality in our study as would be expected [14, 19]. This may reflect reporting biases or our limited sample size. HIV positivity was significantly associated with mortality (p = 0.008). As the tertiary referral hospital for infectious diseases in the country, SLH preferentially caters to complex cases of infectious diseases even before the pandemic started, such as HIV. Further investigation suggested that these individuals included referrals from other hospitals with medical problems in addition to COVID-19.
Our analysis has some limitations. The retrospective design of our study and reliance on the available data from the CIF meant that some variables were incomplete. Details on the patients’ course in the wards and treatment received were also not available. As data from an infectious disease referral hospital, caution should be considered in interpreting the results in the context of the general population. In conclusion, we report various sociodemographic and clinical characteristics associated with increased COVID-19 mortality among hospitalised individuals in Metro Manila, Philippines. Our results support the country’s national guideline on COVID-19 vaccination which prioritises healthcare workers, the elderly population, and people with comorbidities and immunodeficiency states.
Availability of data and materials
The dataset for this study is available from the corresponding author and San Lazaro Hospital on a reasonable request. Data without names and identifiers will be made available after approval from the corresponding author and San Lazaro Hospital.
Change history
13 July 2021
A Correction to this paper has been published: https://doi.org/10.1186/s41182-021-00346-8
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- CIF:
-
Case investigation form
- Ct-value:
-
Cycle threshold value
- DOH:
-
Department of Health
- HCW:
-
Healthcare workers
- NCR:
-
National Capital Region
- non-HCW:
-
Non-healthcare worker
- SLH:
-
San Lazaro Hospital
- SLH – ED:
-
San Lazaro Hospital – Epidemiology Department
References
WHO | Novel Coronavirus – China [Internet]. WHO. World Health Organization; [cited 2021 Apr 23]. Available from: http://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/
Zhu H, Wei L, Niu P. The novel coronavirus outbreak in Wuhan, China. Glob Health Res Policy. 2020;5(1):6. https://doi.org/10.1186/s41256-020-00135-6.
Infectious disease crisis in the Philippines - The Lancet Infectious Diseases [Internet]. [cited 2021 Apr 23]. Available from: https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(19)30642-5/fulltext
COVID-19 Case Bulletin | Department of Health website [Internet]. [cited 2021 Apr 23]. Available from: https://doh.gov.ph/bulletin?page=3
Department of Health. COVID-19 Situationer #360 [Internet]. doh.gov.ph. [cited 2021 Apr 23]. Available from: https://drive.google.com/file/d/1rtHpB5JyKsaOzFbHf2l8RQ5YVizA4x-z/view?fbclid=IwAR2UZxP09_ZMtjVW_PGt1JcKQWIsnZ_htJblnoIhchKJRoMSb0HA_wn8mok&usp=embed_facebook
National Nutrition Council. Region NCR Profile [Internet]. [cited 2021 Apr 23]. Available from: https://www.nnc.gov.ph//regional-offices/luzon/national-capital-region/57-region-ncr-profile
Cevik M, Kuppalli K, Kindrachuk J, Peiris M. Virology, transmission, and pathogenesis of SARS-CoV-2. BMJ. 2020;371:m3862.
Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020 Aug 25;324(8):782–93. https://doi.org/10.1001/jama.2020.12839.
Coronavirus (COVID-19) vaccinations - statistics and research [Internet]. Our World in Data. [cited 2021 Apr 23]. Available from: https://ourworldindata.org/covid-vaccinations
Department of Health. Interim Omnibus Guidelines for the Implementation of the National Vaccine Deployment Plan (NVDP) for COVID-19 [Internet]. [cited 2021 Apr 23]. Available from: https://doh.gov.ph/sites/default/files/health-update/dm2021-0099.pdf
Salva EP, Villarama JB, Lopez EB, Sayo AR, Villanueva AMG, Edwards T, et al. Epidemiological and clinical characteristics of patients with suspected COVID-19 admitted in Metro Manila, Philippines. Tropical Medicine and Health. 2020;48(1):51. https://doi.org/10.1186/s41182-020-00241-8.
Department of Health. Interim guidelines on the COVID-19 disease severity classification and management | Department of Health website [Internet]. 2020 [cited 2021 Jun 1]. Available from: https://doh.gov.ph/node/24520
Villanueva AMG, Lazaro J, Sayo AR, Han SM, Ukawa T, Suzuki S, et al. COVID-19 screening for healthcare workers in a tertiary infectious diseases referral hospital in Manila, the Philippines. American Journal of Tropical Medicine and Hygiene. 2020;103(3):1211–4. https://doi.org/10.4269/ajtmh.20-0715.
Koh J, Shah SU, Chua PEY, Gui H, Pang J. Epidemiological and clinical characteristics of cases during the early phase of COVID-19 pandemic: a systematic review and meta-analysis. Front Med (Lausanne). 2020;7:295.
Surendra H, Elyazar IR, Djaafara BA, Ekawati LL, Saraswati K, Adrian V, et al. Clinical characteristics and mortality associated with COVID-19 in Jakarta, Indonesia: a hospital-based retrospective cohort study. The Lancet Regional Health - Western Pacific [Internet]. 2021 [cited 2021 Apr 23];9. Available from: https://ora.ox.ac.uk/objects/uuid:1a3189fd-00b6-4fad-bc3b-de8bc7046432
Salamat MS, Malundo AFG, Abad CL, Sandejas JC, Planta JE, Poblete J, et al. Characteristics and factors associated with mortality of 200 COVID-19 patients at a Philippine COVID-19 tertiary referral center. Acta Medica Philippina [Internet]. 2021 Apr 27 [cited 2021 May 3];55(2). Available from: https://actamedicaphilippina.upm.edu.ph/index.php/acta/article/view/2845
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–9. https://doi.org/10.1001/jama.2020.6775.
Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, et al. Features of 20 133 UK patients in hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985.
Guan W, Liang W, Zhao Y, Liang H, Chen Z, Li Y, et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: a nationwide analysis. European Respiratory Journal [Internet]. 2020 1 [cited 2021 Apr 23]; Available from: https://erj.ersjournals.com/content/early/2020/03/17/13993003.00547-2020
Acknowledgements
We thank the encoders of the Departments of Epidemiology and Laboratories, San Lazaro Hospital.
Funding
This work is in part funded by Nagasaki University (salary support for CS, KAA, and SS). This study is partially funded by Japan Agency for Medical Research and Development, Grant/Award Numbers: JP19fk0108104h0401, JP20fk0108104h0402.
Author information
Authors and Affiliations
Contributions
Kristal An Agrupis: study design, data analysis and interpretation, and writing—original draft. Chris Smith: supervision, study design, data analysis and interpretation, and writing. Shuichi Suzuki: study design and data interpretation. Annavi Marie Villanueva: data interpretation and writing. Rontgene Solante: data interpretation. Elizabeth Freda Telan: data interpretation. Kelly Anne Estrada: data interpretation. Ann Celestyn Uichanco: data interpretation. Jocelyn Sagurit: data interpretation. Joy Calayo: data interpretation. Dorcas Umipig: data interpretation. Zita dela Merced: data interpretation. Efren Dimaano: data interpretation. Edmundo Lopez: data interpretation. Jose Benito Villarama: data interpretation. Ana Ria Sayo: supervision, data interpretation, and writing. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the SLH research ethics and review unit (Ref: SLH-RERU-2020-022-I) and the School of Tropical Medicine and Global Health–Nagasaki University Ethical Committee (NU_TMGH_2020_119_1).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: the funding section was updated.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Agrupis, K.A., Smith, C., Suzuki, S. et al. Epidemiological and clinical characteristics of the first 500 confirmed COVID-19 inpatients in a tertiary infectious disease referral hospital in Manila, Philippines. Trop Med Health 49, 48 (2021). https://doi.org/10.1186/s41182-021-00340-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41182-021-00340-0