Abstract
Background
Mucopolysaccharidosis (MPS) are inborn errors of metabolism (IEM) recognized by deficient enzymes enrolled in glycosaminoglycans catabolism. The resulting accumulation of glycosaminoglycans leads to clinical progressive and generalized manifestations. Considering the severity of MPS and the relevance of establishing dietetic strategies to these patients, the present study was tailored to evaluate the food intake in patients with MPS types I, II, and VI.
Methods
Food intake in patients with MPS I, II, and VI was assessed. A descriptive cross-sectional study was conducted. Energetic demand based on estimated necessity of energy equations and reported food intake was analyzed. Total energetic value and nutrients (vitamins B1, B2, C, calcium, iron, and phosphate) were analyzed in accordance with the standardized interval for macronutrient distribution and the method of apparent adequacy for nutrient intake.
Results
Food intake of 17 patients (6- to 30-year-olds) was considered adequate regarding macronutrients. Children and adolescents failed in presenting this parameter. Macronutrients were satisfactory in both groups. Children and adolescents displayed increased intake of iron and vitamins B1 (p < 0.05), B2, B3, and C (p < 0.077) and probability of adequacy ≥ 50%. Calcium and phosphorus intake was greater in adults.
Conclusions
The results obtained demonstrated that patients with MPS have nutrition deficiency in their diet, which may directly or indirectly influence the course of the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Mucopolysaccharidosis (MPS) are inborn errors of metabolism (IEM) recognized by deficient enzymes enrolled in glycosaminoglycans catabolism. The resulting accumulation of glycosaminoglycans leads to clinical progressive and generalized manifestations inherited by autosomal recessive, except in MPS type II inherited as an X-linked trait [1]. The most frequent clinical manifestations comprehend short stature, coarse facial features, cornea opacification, heart disease, hepatosplenomegaly, multiple dysostoses, joint stiffness, claw hands, and arthralgia. Repetitive respiratory infections, hypertrophy of the tongue, palatine and adenoid tonsils, alterations in the stomatognathic system, hirsutism, thickening of the skin and mucous membranes, hearing loss and neurological dysfunction [2].
The treatment of IEM has been developed throughout the last years. Even though the new therapeutics achieved does not represent cure for many conditions, they are a significant hallmark in improving quality of life and lifespan increase of patients. The treatment of MPS is based on ameliorating symptomatic manifestations organized by a multidisciplinary team, bone marrow transplantation, and enzymatic replacement therapy [3].
Although MPS are not IEM specifically treated with diet, patients take advantage of nutritional assistance. In fact, some aspects of this disease such as osteoarticular involvement and small stature demand caution in follow-up when related to nutritional condition [4].
Studies have pointed out to alterations in the stomatognathic system, which lead to dysfunction in mastication and deglutition [2] and promote gastrointestinal alterations, especially diarrhea and constipation [5,6,7]. Moreover, neurological symptoms may influence food intake by appetite alterations as well as by a dependence on a caregiver for nutritional handling [8].
Evidence has shown alterations in energetic need since there is an increase in caloric intake and body mass maintenance and decreased accumulation in lipids in adipocytes [9, 10].
Considering the severity of MPS and the relevance of establishing dietetic strategies to these patients, the present study was tailored to evaluate the food intake in patients with MPS types I, II, and VI.
Methods
A transversal descriptive study was conducted including patients with MPS under enzyme replacement therapy (ERT) from the Centro de Referência em Erros Inatos do Metabolismo da Universidade Federal de São Paulo (CREIM/UNIFESP). Patients who displayed severe neurological symptoms, hyperactive behavior, or irritability were not included in the study because their evaluation could be hampered.
During the inclusion period, 33 patients were receiving ERT in CREIM. Ten patients were excluded from the study for not fulfilling the criteria. Three patients did not accept participation or their participation was not allowed, and 20 patients voluntarily accepted participation. These patients received specific instructions regarding the procedures. All of the patients or their legal responsible read and signed the informed consent form.
Energetic necessity was obtained by prediction equations that considered gender, body mass (kg), height (m), and levels of physical activity (sedentary, low active, active, and very active). Food intake found between two standard deviations of estimated necessity was considered adequate.
During appointment, patients were interrogated about food intake from 24 h prior to consultation. This procedure was made twice with intervals that varied from 6 to 12 months. Data were analyzed (total energetic value (TEV), proteins, carbohydrates, lipids, and percent of macronutrients and micronutrients: vitamins B1, B2, B3, and C and calcium, iron, and phosphorus) using AVANUTRI Software (Version Revolution 4.0; Avanutri & Nutrition Services and Informatics Limited ME).
Carbohydrate, lipid, and protein intake evaluation was made using the percent of macronutrients in relation to TEV. The obtained value was ranked in accordance to the acceptable distribution interval of macronutrients, namely acceptable macronutrient distribution range (AMDR) [11].
Individual’s micronutrient intake (vitamins and minerals) was assessed by the “apparent dietary adequacy” method which was proposed by Institute of Medicine’s Food and Nutrition Board [12]. In this method, the probability of adequacy (or inadequacy risk) is assessed by comparing the usual dietary intake to the Dietary Reference Intakes (DRIs): EAR (estimated average requirement), AI (adequate intake), and UL (upper level) [12, 13].
The result is a z-score value obtained using the observation of average nutrient intake. The individual intake evaluation was based on the probability of adequacy in accordance to the obtained z-score. When the obtained z-score was equal or higher than 50%, the probability of adequacy was determined. Oppositely, if the obtained z-score was smaller than 50%, it was considered inadequate.
Children and adolescents were grouped together for the evaluation of studied variables. The probability of adequacy for each nutrient was compared to the normal distribution (Kolgomorov-Smirnov). A posterior t test was applied. A level of significance of 10% was adopted.
The study was approved by the local Institutional Review Boards/the Ethics Committee of the Universidade Federal de São Paulo/Hospital São Paulo under the protocol #0763/11. Consent to publish has been obtained from all involved participants and parent or guardian for children.
Results
The food intake of 17 patients was analyzed: 8 patients with MPS I (4 females), 5 male patients with MPS II, and 4 patients with MPS VI (3 females and 1 male). The minimum age of the sample was 6 years and the maximum 30. The food intake of three patients was not analyzed because the companion was not the caregiver.
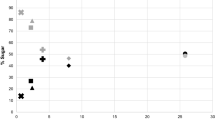
Table 1 details the energy and macronutrients intake (kcal) and the evaluation of average intake of children, adolescents, and adults according to standard deviation. None of the children or adolescents displayed adequate intake (± 2 standard deviations). Of note, 71.4% of children presented food intake higher than 2 standard deviations. In the adult group, the energy consumption was adequate in 60% of the patients and none of the patients presented energy consumption above the recommended levels. Regarding macronutrient distribution, no alteration was detected (Fig. 1).
Analyzing the four studied vitamins, more than half of the children sample presented probability of adequacy higher than 50% (71.4 to 85%). Conversely, more than half of the adults showed probability of adequacy for vitamin B2 intake smaller than 50%. Concerning mineral intake, calcium intake should be highlighted. Indeed, the intake of this mineral presented probability of adequacy smaller than 50% in 13 out of 17 evaluated patients (76.5%). On the other hand, the probability of inadequacy of iron intake was approximately 50% among patients irrespective of age (Table 2).
When the food intake patterns of children and adolescents were compared to those presented by adults, children and adolescents displayed a better pattern of vitamin intake (B1, B2, B3, and C) and iron. Indeed, the frequency of the probability of adequacy was ≥ 50%, especially for vitamin B1 (p < 0.05) and C (p < 0.77). The calcium and phosphorus intake was better in adults compared to that in children and adolescents.
The average intake of macronutrients, vitamins, and minerals as well as the minimum and maximum intake for each group are detailed in Table 3.
Discussion
Nutritional recommendation for patients with MPS is similar to that for healthy patients, with no especial pattern of recommendation. The dietetic treatment does not only aim to correct diarrhea and constipation but also help in the consistency of the dysphagia treatment.
In the present study, approximately half of the evaluated patients presented probable adequacy in vitamin (B1, B2, and B3) levels since they are largely spread in the food. These vitamins may participate in energetic metabolism, in redox reactions. In this regard, niacin plays a critical role in nucleic acids, fatty acids and cholesterol synthesis, DNA repair, and steroid hormones production [14].
The intake of vitamins and iron was higher in children and adolescents than that in adults, especially that of vitamins B1 and C. The increased levels of nutrient intake in children may be related to the average daily calorie quantity. Conversely, the intake of calcium and phosphorus, which are found in milk and milk derivatives, was higher in adults.
The majority of the patients showed probability of adequacy ≥ 50% for vitamin C. The inflammatory nature of the lysosomal diseases should be highlighted [15] especially MPS [16]. Thus, this pattern may lead to increased necessity of nutrients with antioxidant action such as ascorbic acid [17] because the disease-induced oxidative stress may deplete this nutrient [18].
In a previous study in the same population, the fruit, vegetable, and green intake was smaller than that recommended by the guidelines on nutrition for Brazilian population. The majority of enrolled population had inadequate quantities of grains, tubercle, fruit, and vegetables (submitted data).
The decrease in fruit, vegetable, and legume intake is an ordinary phenomenon observed in Brazilian population due to an increased consumption of ultra-processed in substitution to minimally processed food [19].
Calcium and phosphorus intake was higher in adults since the majority of children and adolescents presented probability of adequacy smaller than 50%. In Sao Paulo state, it was reported that calcium intake inadequacy was higher than 70% among adolescents and adults [20].
Regarding low adequacy of calcium and phosphorus intake, children with MPS demand more attention in regulating the intake of these nutrients since they participate in structural formation (teeth, bones, and connective tissues) and diverse metabolic ways. Additionally, the intake of these nutrients is also critical for growth, development, and good physiological function [21].
In MPS, the establishment of an ideal calcium metabolism constitutes an obstacle due to the altered calcium homeostatic and cellular metabolism found in IEM [22]. In line with this assumption, studies have shown that these patients may present low bone mineral density when chronological age and gender are considered. However, these data are questionable because bone diseases, as osteoporosis and osteomalacia for instance, are not accurately diagnosed in MPS. In fact, abnormal bone geometry may hamper precise diagnostics [23]. Apart from that, the equipment and equations involved in diagnostics are set for normal pattern of morphology found in the general population, not in MPS.
Over 50% of studied population displayed probability of adequacy ≥ 50% in iron intake. This nutrient has deficiency in higher magnitude worldwide and is verified in all segments being associated to insufficient iron quantity in the diet able to provide individual nutritional necessity [24]. The deficiency of this nutrient may affect both growth and development in children and adolescents and also influence the work ability and the immune response [25, 26]. For this reason, Brazil adopted a compulsory iron fortification of wheat or corn flour, which is considered the best cost-benefit measure to reduce the prevalence of iron deficiency [25].
In MPS, an important factor of iron intake is inflammation [15], because this process leads to a reduction in hepcidin, a hormone responsible for iron absorption [27].
Herein, macronutrients intake was found in accordance with that recommended by AMDR [11] as well as the intake proportion found in the Brazilian survey of familiar budget [19, 28]. However, the energy consumption of none of the children and adolescents was adequate energetic intake. The majority of children had more caloric intake than that estimated for age, gender, and stature. On the other hand, caloric intake was adequate in adults. Together, these results may suggest that the increased physiology energetic demand in childhood and adolescence allied to the metabolic alterations found in MPS may establish or decrease during adulthood.
Studies that evaluated the food intake or energetic demand in MPS are scarce. A study had analyzed seven patients with MPS II at age of 5 to 14 years. The authors have verified that the average energetic intake was smaller than the energetic demand. However, the energetic value may have been super estimated because activity is a factor with large variability in this population [29].
Studies using animal models of MPS types I and VII have reported that there is an increase in food intake that could lead to a decreased use of energy due to lysosomal accumulation [9].
In the same context, an increased autophagy caused by an energetic misbalance was found in animals. The authors have attributed this misbalance to lysosomal dysfunction, which may had kidnaped metabolites, stimulating protein degradation. This greater protein degradation occurred to maintain the intermediary metabolism in response to carbohydrates and lipids, corrected after higher intake of carbohydrates and fat [10]. ERT also contributed by increasing the glycosaminoglycans catabolism and releasing monosaccharaides into the cytosol. Such mechanism leads to a reduction in the energy requirement from the de novo synthesis, thus the demand for raw material was lower.
The current phenomenon of nutritional transition amplifies the risk of developing non-transferable chronic diseases and their morbidity or associated nutritional deficiencies in the general population. Patients with MPS are also part of this context even though their nutritional pattern, such as necessity of energy or micronutrients or even macronutrients adequate intake, still remains neglected, worsening this clinical condition.
Conclusion
The nutritional assessment in the present study showed that despite the overall macronutrients intake in levels recommended by AMDR, MPS patients presented an inadequate energy and micronutrient consumption. The present data suggests that patients with MPS could benefit from monitoring and nutritional counseling, given the inadequacy of the nutrient intake and its direct and/or indirect implications for the course of the disease in different stages of life. Such strategies could promote quality of life and minimize the effects of possible nutritional deficiencies (both macro and micronutrients) in this population.
Abbreviations
- AI:
-
Adequate intake
- AMDR:
-
Acceptable macronutrient distribution range
- DRIs:
-
Dietary Reference Intakes
- EAR:
-
Estimated average requirement
- ERT:
-
Enzyme replacement therapy
- IEM:
-
Inborn errors of metabolism
- MPS:
-
Mucopolysaccharidosis
- TEV:
-
Total energetic value
- UL:
-
Upper level
References
Clarke LA. The mucopolysaccharidoses: a success of molecular medicine. Expert Rev Mol Med. 2008;10:e1.
Turra GS, Schwartz VD. Evaluation of orofacial motricity in patients with mucopolysaccharidosis: a cross-sectional study. J Pediatr. 2009;85(3):254–60.
Schwartz IV, Souza CF, Giuliani R. Treatment of inborn errors of metabolism. J Pediatr. 2008;84(4):S8–19.
Pinto LL, Schwartz IV, Puga AC, et al. Prospective study of 11 Brazilian patients with mucopolysaccharidosis II. J Pediatr. 2006;82(4):273–8.
Neufeld EF, Muenzer J. The mucopolysaccharidoses. In: Valle D, Beaudet AL, Vogelstein B, Kinzler KW, et al, eds. Scriver's Online Metabolic and Molecular Bases of Inherited Disease. https://doi.org/10.1036/ommbid.172. Published January 2006. Last access: Dec 10, 2012.
Sibilio M, Miele E, Ungaro C, et al. Chronic diarrhea in mucopolysaccharidosis IIIB. J Pediatr Gastroenterol Nutr. 2009;49(4):477–80.
Wegrzyn G, Kurlenda J, Liberik A, et al. Atypical microbial infections of digestive tract may contribute to diarrhea in mucopolysaccharidosis patients: a MPS I case study. BMC Pediatr. 2005;5(1):9.
Gauche H, Calvo MCM, Assis MAA. Food consumption circadian rhythms in adult snacks and meals: application to weekly menu. Rev Nutr Campinas. 2006;19(2):177–85.
Woloszynek JC, Coleman T, Semenkovic CF, et al. Lysosomal dysfunction results in altered energy balance. J Biol Chem. 2007;282(49):35765–71.
Woloszynek JC, Kovacs A, Ohlemiller KK, et al. Metabolic adaptations to interrupted glycosaminoglycan recycling. J Biol Chem. 2009;284(43):29684–91.
Institute of Medicine (US) Subcommittee on Interpretation and Uses of Dietary Reference Intakes, Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. DRI Dietary Reference Intakes: Applications in Dietary Assessment. Washington (DC): National Academies Press (US); 2000.
Trumbo P, Schlicker S, Yates AA, et al. Food and Nutrition Board of the Institute of Medicine, the National Academies. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J Am Diet Assoc 102(11):1621-1630, 2002.
Marchioni DML, Slater B, Fisberg RM. Application of dietary reference intakes for assessment of individuals. Rev Nutr. 2004;17(2):207–16.
Chawla J, Kvarnberg D. Hydrosoluble vitamins. Handb Clin Neurol. 2014;120:891–914.
Vitner EB, Platt FM, Futerman AH. Common and uncommon pathogenic cascades in lysosomal storage diseases. J Biol Chem. 2010;285(27):20423–7.
Filippon L, Vanzin CS, Biancini GB, et al. Oxidative stress in patients with mucopolysaccharidosis type II before and during enzyme replacement therapy. Mol Genet Metab. 2011;103(2):121–7.
Grosso G, Bei R, Mistretta A, et al. Effects of vitamin C on health: a review of evidence. Front Biosci. 2013;18(1):1017–29.
Sorice A, Guerriero E, Capone F, et al. Ascorbic acid: its role in immune system and chronic inflammation diseases. Mini Rev Med Chem. 2014;14(5):444–52.
Levy RB, Claro RM, Mondini S, et al. rsp Regional and socioeconomic distribution of household food availability in Brazil, in 2008–2009. Rev Saúde Pública. 46(1):6-15, 2012.
Martini LA, Verly E Jr, Marchioni DM, et al. Prevalence and correlates of calcium and vitamin D status adequacy in adolescents, adults, and elderly from the Health Survey–São Paulo. Nutrition. 2013;29(6):845–50.
Uush T. Calcium intake and serum calcium status in Mongolian children. J Steroid Biochem Mol Biol. 2014;144:67–71.
Pereira VG, Gazarini ML, Rodrigues LC, et al. Evidence of lysosomal membrane permeabilization in mucopolysaccharidosis type I: rupture of calcium and protonhomeostasis. J Cell Physiol. 2010;223(2):335–42.
Polgreen LE, Thomas W, Fung E, et al. Low bone mineral content and challenges in interpretation of dual-energy X-ray absorptiometry in children with mucopolysaccharidosis types I, II, and VI. J Clin Densitom. 2014;17(1):200–6.
Brazil. Ministry of Health. Department of Health Care. Department of Primary Care. National Program for Iron Supplementation: Guidelines/ Ministry of Health Scretary of Health Care Department of Primary Care. Brasilia: Ministry of Health, 2013. 24 p.: il.
Buzzo ML, Carvalho MFH, Tigela P, et al. Monitoring the wheat and corn flours enriched with iron. Rev Inst Adolfo Lutz. 2012;71(4):645–9.
Haimi M, Lerner A. Nutritional deficiencies in the pediatric age group in a multicultural developed country, Israel. World J Clin Cases. 2014;12(5):120–5.
Ganz T. Hepcidin: a regulator of intestinal iron absorption and iron recycling by macrophages. Best Pract Res Clin Haematol. 2005;18(2):171–82.
Brazilian Institute of Geography and Statistics (IBGE). Familiar budget survey 2008-2009: expenses, income and living conditions. Rio de Janeiro; 2010.
Ferreira ACRG, Oliveira AC, Veiga LLP, et al. Interference of oropharyngeal dysphagia in food consumption in patients with mucopolysaccharidosis II. Rev CEFAC. 2012;14:1184–96.
Acknowledgements
The authors would like to thank the Laboratório de Erros Inatos do Metabolismo (LEIM), Centro de Estudos em Psicobiologia e Exercício (CEPE), Centro Referência em Erros Inatos do Metabolismo (CREIM), and Centro de Diagnósticos Brasil (CDB).
Funding
This research was supported by fellowships from Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES). The authors have no financial relationships relevant to this article to disclose.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on a reasonable request.
Author information
Authors and Affiliations
Contributions
VCLM conceptualized and designed the study, drafted the initial manuscript, carried out the initial analyses, reviewed and revised the manuscript, and approved the final manuscript as submitted. JAOS carried out the initial analyses, designed the data collection instruments, coordinated and supervised the data collection, reviewed and revised the manuscript, and approved the final manuscript as submitted. RBO and BJF reviewed and revised the manuscript and approved the final manuscript as submitted. PRD designed the data collection instruments, coordinated and supervised the data collection, reviewed and revised the manuscript, and approved the final manuscript as submitted. ANP drafted the initial manuscript, carried out the initial analyses, reviewed and revised the manuscript, and approved the final manuscript as submitted. AMM reviewed and revised the manuscript and approved the final manuscript as submitted. RCA drafted the initial manuscript, carried out the initial analyses, reviewed and revised the manuscript, and approved the final manuscript as submitted. VDA conceptualized and designed the study, drafted the initial manuscript, carried out the initial analyses, reviewed and revised the manuscript, and approved the final manuscript as submitted. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the local Institutional Review Boards/the Ethics Committee of the Universidade Federal de São Paulo/Hospital São Paulo under the protocol #0763/11.
Consent for publication
All of the patients or their legal responsible read and signed the informed consent form.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Monteiro, V.C.L., Araújo de Oliveira Silva, J., Oliveira, R.B. et al. Evaluation of food intake in patients with mucopolysaccharidosis. Nutrire 43, 9 (2018). https://doi.org/10.1186/s41110-018-0066-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41110-018-0066-1