Abstract
Background
Non-cuffed hemodialysis (HD) catheters are often used for emergency or temporary vascular access. Its complications include thrombosis and catheter-related bloodstream infection (CRBSI); however, thrombophlebitis can also occur. Thrombophlebitis of the internal jugular vein (IJV) may present with symptoms, such as fever, lateral neck pain, and swelling, regardless of the presence or absence of infection; however, symptoms may be minor and easily overlooked. Sore throat is a well-known symptom of Lemierre's syndrome, but has not been reported in cases of thrombophlebitis without infection. We report two cases of HD catheter-associated IJV thrombophlebitis in patients that were diagnosed with sore throat.
Case presentation
Case 1 included a 58-year-old woman with diabetic nephropathy on HD. She was admitted to our hospital due to the occlusion of an arteriovenous fistula (AVF) for dialysis. A temporary HD catheter was placed in the right IJV until an arteriovenous graft (AVG) was fabricated. After admission, CRBSI was suspected because she developed fever; however, bacteremia was ruled out and a sore throat gradually developed. Contrast-enhanced computed tomography (CT) revealed thrombophlebitis of the right IJV. Anticoagulation therapy was initiated and she was discharged due to an improvement of symptoms. Case 2 included an 83-year-old man with end-stage renal disease due to hypertensive nephrosclerosis. He was admitted to our hospital because of AVF occlusion. A temporary HD catheter was inserted into the right IJV and an AVG was created. He had elevated C-reactive protein levels after catheter placement but was asymptomatic. When removing the catheter, he complained of throat discomfort. Ultrasonography of the neck revealed thrombotic obstruction of the right IJV, and contrast-enhanced CT revealed thrombophlebitis of the right IJV. Blood culture results were negative. He was discharged after anticoagulation therapy was started and symptoms improved.
Conclusions
The presence of sore throat leads to the diagnosis of IJV thrombophlebitis. Pharyngeal symptoms that develop after central venous catheter (CVC) placement should be differentiated from thrombophlebitis using a minimally invasive vascular ultrasound.
Similar content being viewed by others
Background
Vascular access is essential for hemodialysis (HD). The vascular access used in emergency or temporary situations is a non-cuffed HD catheter. The use of HD catheters for dialysis initiation should be avoided whenever possible due to the increased length of hospital stay, higher cost, and risk of complications [1]. However, although HD catheters are used less frequently than in the past, they are still frequently used due to lack of patient awareness and unforeseen circumstances [2]. In addition, HD catheters are also mainly used in maintenance dialysis patients as a bridging use until permanent vascular access is created. Unlike other central venous catheters (CVCs), HD catheters have a route for the withdrawal of blood for dialysis treatment and a route for returning blood; therefore, it has a larger catheter diameter [3]. Complications associated with HD catheter placement include catheter-related bloodstream infections (CRBSI), catheter dysfunction, and thrombosis. Thrombosis associated with CVC placement is considered frequent [3,4,5], and venous thrombosis can rarely cause phlebitis. Herein, we report two cases of HD catheter-related thrombophlebitis of the internal jugular vein (IJV). The clinical courses of the two cases were different; however, in both cases, the diagnosis was prompted by pharyngeal symptoms that mimicked Lemierre's syndrome.
Case presentation
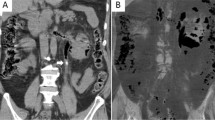
Case 1 A 58-year-old woman, who had started hemodialysis for end-stage renal disease (ESRD) caused by diabetic nephropathy 5 years prior, was admitted to our hospital due to an occluded arteriovenous fistula (AVF) in her left forearm, which was used for dialysis. She had undergone vascular access intervention therapy (VAIVT) for AVF stenosis several months earlier, and restenosis was observed on admission. She had a history of surgery for breast and endometrial cancer, but had no history of oropharyngeal infection. A non-cuffed HD catheter (double lumen, polyurethane, 12 French) was placed in the right IJV on day 2 of admission until an arteriovenous graft (AVG) in the left forearm was fabricated on day 8. As the patient had persistent fever after catheter placement, CRBSI was suspected. The catheter was removed on day 9 of admission and antimicrobial therapy with vancomycin was initiated. However, the blood culture results were negative, and antibiotics were administered for 1 week. The fever persisted and the patient developed sore throat after a few days. Contrast-enhanced computed tomography (CT) on day 16 revealed a complete occlusion of the right IJV due to thrombus formation and phlebitis (Fig. 1a, b). The fever and sore throat were considered to have been caused by right IJV thrombophlebitis, as no other etiology could explain the symptoms. Anticoagulation therapy (initially with heparin 12,000 units per 24 h, then switched to warfarin) was initiated on day 16 and the patient was discharged due to an improvement of symptoms on day 25. Heparin was volume-adjusted to achieve an activated partial thromboplastin time (APTT) value of 1.5 to 2.0 times and warfarin doses were adjusted for prothrombin time international normalized ratio (PT-INR) of approximately 2.0. After discharge from the hospital, anticoagulation therapy was discontinued as the thrombus disappeared on day 162; however, severe venous stenosis of the right IJV persisted (Fig. 1c).
Findings of contrast-enhanced computed tomography (CT) of the neck in Case 1. a The coronal view shows thrombosed obstructions (arrowheads) of the right internal jugular vein (IJV). b The horizontal view shows a right IJV thrombosis (arrowhead) with phlebitis, surrounding soft tissue inflammation, and enlarged lymph nodes (arrows). The thyroid cartilage deviates to the left. c The horizontal view after 1 year shows severe stenosis of the right IJV (arrowhead)
Case 2 An 83-year-old man with ESRD due to hypertensive nephrosclerosis, who was on maintenance HD for months, was admitted to our hospital because of AVF occlusion in his right forearm. He was taking antiplatelet medications for ischemic heart disease. There were no specific symptoms or abnormal physical findings on admission. He had a thrombotic occlusion caused by shunt vein stenosis, and there was a large thrombus in the shunt vein. A non-cuffed HD catheter (triple lumen, polyurethane, 12 French) was inserted into the right IJV on day 2 of admission and an AVG was created on the right elbow region on day 11. The patient had elevated C-reactive protein (CRP) levels (0.235 mg/dL on admission, 6.92–10.93 mg/dL on days 8–12) after catheter placement but was asymptomatic, and blood culture results obtained on day 8 were negative. After catheter removal on day 17, the patient complained of throat discomfort especially during swallowing. Ultrasonography of the neck on the same day revealed thrombotic obstruction of the right IJV (Fig. 2a, b), and a subsequent contrast-enhanced CT on day 18 revealed thrombophlebitis of the right IJV (Fig. 2c) but there was no pulmonary embolism (PE). Furthermore, repeated blood culture results were negative. The patient’s symptoms improved after anticoagulation therapy (continuous intravenous heparin 10,000 units per 24 h on day 17 of admission, followed by oral warfarin on day 19) was commenced, and he was discharged from the hospital on day 23.
Ultrasonographic and contrast-enhanced CT images in Case 2. Ultrasonographic images of the neck (a: cross section, b: longitudinal section) showing dilation of the right IJV and a heterogeneous hyperechoic mass in the lumen (arrowheads). Coronal CT image c showing a right IJV thrombus with surrounding soft tissue inflammation. The thrombus reaches the superior vena cava (arrowheads).
Discussion and conclusions
Thrombophlebitis is a condition characterized by the inflammation of veins associated with venous thrombosis. Thrombophlebitis has been reported to be caused by infections, CVC placement, hypercoagulability, malignancy, and collagen disease [6,7,8,9]. Septic thrombophlebitis, such as Lemierre’s syndrome due to oropharyngeal infection, is the widely recognized form of thrombophlebitis of IJV [6]. There have also been reports of IJV thrombophlebitis associated with CVC placement that is mostly associated with CRBSI [5, 7, 10, 11]. However, there are few reported cases of IJV thrombophlebitis that are not associated with infection.
We searched PubMed using the keywords (internal jugular vein AND catheter AND thrombophlebitis OR thrombosis) and excluded reports with no description of symptoms, treatment, or complications. We retrieved 12 relevant articles (Table 1) [10,11,12,13,14,15,16,17,18,19,20,21]. These articles included 14 patients with catheter-related IJV thrombosis, but only three cases of thrombophlebitis [10, 11, 13].
All these reports of IJV thrombophlebitis were associated with infection and showed symptoms such as fever and lateral neck pain and swelling, similar to catheter-related IJV thrombosis. The same is true in reports of IJV thrombophlebitis due to causes other than catheters, and fever, lateral neck pain, and swelling are thought to be the main symptoms, regardless of the presence or absence of infection [6,7,8,9]. Septic thrombophlebitis with pharyngeal infection, as in Lemierre's syndrome, is often accompanied by a sore throat [6, 7]. However, some cases such as IJV thrombosis may be asymptomatic and easily missed [6, 22].
Herein, we report two interesting cases of CVC-related non-pyogenic thrombophlebitis of the IJV that presented with pharyngeal symptoms mimicking Lemierre’s syndrome. Case 1 was accompanied by fever; however, Case 2 initially showed only elevated CRP levels on blood tests and minimal symptoms.
Although the clinical course was different, the pharyngeal symptoms led to the diagnosis of IJV thrombophlebitis. Sore throat is mainly caused by pharyngeal infections, often due to respiratory viruses and group A Streptococcus (GAS), which are spread by droplet infection [23]. The possibility that viral pharyngitis, a self-limiting condition, may have existed cannot be ruled out, because detailed observation of the pharynx was not performed in these cases. However, since there was no patient with similar symptoms in the same room, it is unlikely that acute pharyngitis was caused by inhaling infectious droplet; moreover, based on the clinical course, it is more reasonable to consider that the symptoms were associated with IJV thrombophlebitis. It may be a clinical manifestation of IJV thrombophlebitis due to the anatomically dense nature of this region, which would make it conducive to the spread of infection to adjacent structures, including the pharynx. CVC placement is a risk factor for venous thrombosis and thrombophlebitis [4, 5, 22]; therefore, pharyngeal symptoms in patients, after the placement of indwelling CVCs in the IJV, should be differentiated from thrombophlebitis; moreover, these symptoms should first be assessed for venous thrombus using a minimally invasive vascular ultrasound.
Our patients were later evaluated for thrombogenic predisposition; however, no previous thrombosis, new malignancy, or other causes, such as antiphospholipid syndrome or protein C and S deficiency were identified. However, Case 1 had a history of catheter placement, and repeated venous endothelial injury may have caused thrombophlebitis. Among CVCs, HD catheters are considered more prone to complications than other CVCs because of their larger diameter; therefore, special care should be taken when using HD catheters.
PE and infection were ruled out in our patients. However, PE, which can be fatal, is known to occur more frequently in patients with infectious thrombophlebitis [6, 7]. There were no cases of PE in catheter-related thrombosis, including catheter-related septic thrombophlebitis, as shown in Table 1. However, cases of serious complications such as SVC syndrome and the development of dural sinus thrombosis have been reported [17, 20]. Therefore, if a thrombus is found in the IJV on vascular ultrasound and thrombophlebitis is strongly suspected based on the clinical situation, infectious complications, PE, and extension of the IJV thrombus to other sites should be excluded, and CT scans would be useful to evaluate these complications.
In the treatment of infectious thrombophlebitis, appropriate treatment of the underlying infection is important, and anticoagulation therapy for the prevention of complications such as PE and post-thrombotic syndrome is considered on an individual basis [6, 7]. Thrombophlebitis without infection is considered equivalent to the treatment of venous thrombosis, but the indication for anticoagulation in venous thrombosis of the IJV is controversial [4, 24]. This is because the risk of developing PE or post-thrombotic syndrome, which is a serious complication, varies in frequency depending on the venous site and literature [22, 24]. Most patients reported in Table 1 were treated with anticoagulants for venous thrombosis. Although it is difficult to explain the absence of PE in all cases as an effect of anticoagulation therapy, the absence of bleeding complications indicates a certain level of safety. We considered that the thrombus in our cases posed a high risk of PE because it was large and partially suspended; therefore, we administered antithrombotic therapy. No pulmonary embolization occurred and we confirmed that the thrombus had disappeared. However, in Case 1, the right IJV atrophied, and severe venous stenosis occurred after the thrombus disappeared. Similarly, in Case 2, the right IJV was atrophic and organic, and the collateral tract developed accordingly. There have been no detailed reports on the treatment and outcomes of non-infectious thrombophlebitis associated with CVC placement, and it would be desirable to accumulate more cases in the future to clarify the necessity of treatment.
In conclusion, the symptoms of IJV thrombophlebitis associated with CVC placement may be minimal; however, the presence of sore throat may lead to the diagnosis of IJV thrombophlebitis. Pharyngeal symptoms that develop after CVC placement should be differentiated from thrombophlebitis using a minimally invasive vascular ultrasound.
Availability of data and materials
All data and materials have been included in the manuscript.
Abbreviations
- HD:
-
Hemodialysis
- CVC:
-
Central venous catheter
- CRBSI:
-
Central venous catheter-related bloodstream infection
- IJV:
-
Internal jugular vein
- ESRD:
-
End-stage renal disease
- AVF:
-
Arteriovenous fistula
- AVG:
-
Arteriovenous graft
- CT:
-
Computed tomography
- APTT:
-
Activated partial thromboplastin time
- PT-INR:
-
Prothrombin time international normalized ratio
- CRP:
-
C-reactive protein
- PE:
-
Pulmonary embolism
- GAS:
-
Group A Streptococcus
References
Kukita K, Ohira S, Amano I, Naito H, Azuma N, Ikeda K, et al. 2011 Update Japanese Society for dialysis therapy guidelines of vascular access construction and repair for chronic hemodialysis. Ther Apher Dial. 2015;19(Suppl 1):1–39.
Nakaya I, Goto T, Nakamura Y, Yoshikawa K, Oyama J, Tamayama Y, et al. Temporary central venous catheter at hemodialysis initiation and reasons for use: a cross-sectional study. Renal Replace Ther. 2021;7(1):2.
Gallieni M, Brenna I, Brunini F, Mezzina N, Pasho S, Giordano A. Dialysis central venous catheter types and performance. J Vasc Access. 2014;15(Suppl 7):S140–6.
Scerrati A, Menegatti E, Zamboni M, Malagoni AM, Tessari M, Galeotti R, et al. Internal jugular vein thrombosis: etiology, symptomatology, diagnosis and current treatment. Diagnostics (Basel, Switzerland). 2021;11(2):378.
Picardi M, Pagliuca S, Chiurazzi F, Iula D, Catania M, Rossano F, et al. Early ultrasonographic finding of septic thrombophlebitis is the main indicator of central venous catheter removal to reduce infection-related mortality in neutropenic patients with bloodstream infection. Ann Oncol. 2012;23(8):2122–8.
Kuppalli K, Livorsi D, Talati NJ, Osborn M. Lemierre’s syndrome due to Fusobacterium necrophorum. Lancet Infect Dis. 2012;12(10):808–15.
Chirinos JA, Garcia J, Alcaide ML, Toledo G, Baracco GJ, Lichtstein DM. Septic thrombophlebitis: diagnosis and management. Am J Cardiovasc Drugs. 2006;6(1):9–14.
Chera HH, Cohen M, Ishakis R, Rosen Y, Ozeri DJ. Lemierre’s syndrome in an aseptic patient with systemic lupus erythematosus. Isr Med Assoc J. 2018;20(7):448–50.
Oshinyemi P, Lee C, Gough-Palmer A, McKay-Davies I. IJV thrombophlebitis: be wary of the occult. BMJ Case Rep. 2021;14(3):e238813.
Caccese R, Carfagna P, Pistilli N, Massetti AP, Falcone M, Venditti M. Candidal thrombophlebitis of central veins: case report and review. Med Mycol. 2012;50(3):299–304.
Hagiya H, Kajioka H. Successful treatment of recurrent candidemia due to candidal thrombophlebitis associated with a central venous catheter using a combination of fosfluconazole and micafungin. Intern Med. 2013;52(18):2139–43.
Harter C, Salwender HJ, Bach A, Egerer G, Goldschmidt H, Ho AD. Catheter-related infection and thrombosis of the internal jugular vein in hematologic-oncologic patients undergoing chemotherapy: a prospective comparison of silver-coated and uncoated catheters. Cancer. 2002;94(1):245–51.
Leon LR Jr, Patel J, Labropoulos N, Rodriguez HE. Excision of internal jugular vein for catheter-related thrombophlebitis. Ann Vasc Surg. 2006;20(1):117–9.
Lee N, Coco M. Chylous pericardial tamponade in a haemodialysis patient with catheter-associated thrombosis of internal jugular and subclavian veins. Nephrol Dial Transplant. 2006;21(9):2650–3.
Pratap B, Gupta P, Kumar P, Abraham G, Santhanam R. Multiple myeloma and hypercoagulability leading to internal jugular vein thrombosis in a dialysis patient. Hemodial Int. 2007;11(1):35–7.
Saranteas T, Mandila C, Poularas J, Papanikolaou J, Patriankos A, Karakitsos D, et al. Transesophageal echocardiography and vascular ultrasound in the diagnosis of catheter-related persistent left superior vena cava thrombosis. Eur J Echocardiogr. 2009;10(3):452–5.
Di Cocco P, Orlando G, Di Cesare E, Mazzotta C, Rizza V, Pisani F, et al. Superior vena cava syndrome due to thrombotic occlusion in a thrombophilic renal transplant recipient: a case report. Transplant Proc. 2010;42(4):1358–61.
Smith KA, Kibbee NM, Moak JH. Acute internal jugular venous thrombosis from dialysis catheter. J Emerg Med. 2012;42(2):e41–2.
Minami K, Iida M, Iida H. Case report: central venous catheterization via internal jugular vein with associated formation of perioperative venous thrombosis during surgery in the prone position. J Anesth. 2012;26(3):464–6.
Binnani P, Bahadur MM, Dalal K. Dural sinus thrombosis—a rare manifestation of internal jugular venous occlusion. Saudi J Kidney Dis Transplant. 2012;23(4):799–803.
Ma W, Qiu Y, Cui Y, Yang G, Wang Z, Liu B. Catheter-related right internal jugular vein large thrombus formation after inadvertently malposition in the cranial direction. J Thromb Thrombolysis. 2019;48(2):355–7.
Gbaguidi X, Janvresse A, Benichou J, Cailleux N, Levesque H, Marie I. Internal jugular vein thrombosis: outcome and risk factors. QJM. 2011;104(3):209–19.
Krüger K, Töpfner N, Berner R, Windfuhr J, Oltrogge JH. Clinical practice guideline: sore throat. Dtsch Arztebl Int. 2021;118(11):188–94.
Baumann Kreuziger L, Onwuemene O, Kolesar E, Crowther M, Lim W. Systematic review of anticoagulant treatment of catheter-related thrombosis. Thromb Res. 2015;136(6):1103–9.
Acknowledgements
We would like to thank Editage (www.editage.jp) for the English language editing.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SY wrote the initial draft. SY, KU, TN, IN, and MW participated in the discussion and treatment of the patients. TN, IN, and MW reviewed and revised the manuscript accordingly. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patients for the publication of this article.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yoshida, S., Usui, K., Naganuma, T. et al. Two cases of aseptic internal jugular vein thrombophlebitis associated with hemodialysis catheter, presenting as sore throat: case report and literature review. Ren Replace Ther 9, 4 (2023). https://doi.org/10.1186/s41100-023-00458-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-023-00458-3