Abstract
Background
In the Japanese guidelines on combination peritoneal dialysis (PD) and hemodialysis (HD) therapy, patients with serum beta 2 microglobulin (β2MG) levels less than 30 mg/L are recommended. And PD patients with β2MG more than 30 mg/L are considered to transfer to the PD + HD combination therapy. However, the resultant changes in serum β2MG levels by the introduction of PD + HD combination therapy and the factors influencing the change have not clearly elucidated.
Methods
We retrospectively studied 11 PD patients (mean age 56.4 ± 12.9 years, 10 males) with baseline β2MG levels > 30 mg/L with respect to changes in β2MG and its related factors for 12 months after the introduction of combination therapy of PD plus once a week HD (4 h) using a high-performance dialyzer. Laboratory data including hemoglobin, albumin, C-reactive protein, blood urea nitrogen, creatinine, and the patients’ demographic profiles, and HD-related factors, such as Kt/V and blood flow rate, were assessed.
Results
Serum β2MG levels decreased statistically significantly after the introduction of combination therapy: from 36.7 ± 6.7 mg/L at 0 months, to 33.4 ± 6.1 mg/L at 3 months (p = 0.030, compared to baseline), 32.9 ± 4.5 mg/L at 6 months (p = 0.009), and 33.3 ± 5.3 mg/L at 12 months (p = 0.023), respectively. However, only 27–36% patients achieved target β2MG levels of < 30 mg/L during the observation period. Regarding influencing factors, serum albumin levels, blood flow rates of HD, residual renal function and baseline β2MG were associated with a decrease in serum β2MG levels on univariate analysis. In multivariate analysis, serum albumin at 3 and 12 months correlated significantly with Δβ2MG (β = − 0.990, p = 0.032 at 3 months, β = − 0.551, p = 0.033 at 12 months). Urine volume at 12 months correlated significantly with Δβ2MG (β = 0.507, p = 0.019).
Conclusions
Combination therapy of PD and HD might reduce serum β2MG levels, but with marginal efficacy. Our preliminary data indicate that the combination therapy of PD and once weekly HD is not sufficient to significantly decrease serum β2MG levels. Additional HD prescriptions, such as increase in blood flow rate and hemodiafiltration, need to be tested in order to improve β2MG levels in these patients.
Similar content being viewed by others
Background
In Japan, combination therapy with peritoneal dialysis and hemodialysis (PD + HD) is widely used in PD patients as an alternative method for various reasons, such as to decrease serum beta 2 microglobulin (β2MG), improve fluid overload, and maintain residual kidney function [1]. Importantly, Murashima, et al. have reported using the Japanese Society for Dialysis Therapy registry data that combination of once-weekly HD with PD is associated with lower mortality compared with peritoneal dialysis alone [2]. At the end of 2014, 1913 PD patients were receiving PD + HD combination therapy in Japan, which is 20.7% of all PD patients [1]. Typically, combination therapy with 5 or 6 days of PD and once weekly HD is used to counteract the decline in total solute clearance caused by decreased residual kidney function and decline in ultrafiltration caused by increase in peritoneal permeability [3].
Serum β2MG has been widely accepted as a marker of overall middle molecular uremic toxins and is a key factor in the genesis of dialysis-associated amyloidosis [4]. Since β2MG is exclusively eliminated by the kidneys [5], its levels are particularly elevated in patients with HD or PD who have low residual kidney function [6,7,8,9,10,11,12]. Therefore, if the residual kidney function declines in patients receiving PD monotherapy, the removal of middle molecular weight substances, such as β2MG, is limited.
Managing serum β2MG at an appropriate level is one of the important reasons for initiation of PD + HD combination therapy. Recently, several studies have shown that higher serum β2MG is associated with poor prognosis, including worse survival in dialysis patients [13,14,15,16]. Okuno et al. demonstrated in hemodialysis patients that serum β2MG is a significant predictor of all-cause mortality [15] and the HEMO Study Group also showed that every 10 mg/L increase in serum β2MG in HD patients is a significant predictor of death due to infection, after adjustment for multiple confounding factors [13]. Koh et al. demonstrated that every 1 mg/L increase in serum β2MG is a significant predictor of all-cause mortality in PD patients [16]. Based on these findings, the new Japanese Society of Dialysis Therapy guidelines for Peritoneal Dialysis in 2019 recommended a target serum β2MG value of 30 mg/L or less [17].
However, it is unclear how much serum β2MG levels improve in PD patients who also undergo once-weekly HD. In addition, it is unclear which factors contribute to the improvement in β2MG levels. Here, we retrospectively investigated PD patients with baseline β2MG levels > 30 mg/L who started once-weekly HD combination therapy and analyzed the magnitude of the decrease in β2MG levels and its related factors for 12 months.
Methods
Study design and participants
This study was a 12-month, single-center, retrospective, observational study conducted at the Kidney Center of St. Luke's International Hospital (Tokyo, Japan) between June 2011 and August 2020. The study was approved by the research ethics committee of St Luke's International Hospital (approval number 21-R156) and adhered to the ethical principles set by the Declaration of Helsinki.
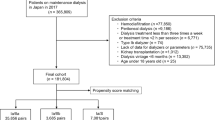
Patient selection in the present study is shown in Fig. 1. Nineteen patients were initially registered, from among whom 11 patients were finally included in this study. The inclusion criteria were as follows: (1) patients who started combination therapy of PD and HD at St. Luke's International Hospital, (2) those in whom the observation period was more than 12 months, and (3) patients with β2MG levels > 30 mg/L at the initiation of PD + HD combination therapy. Of the remaining eight patients, six patients were excluded due to a short observation period, and two cases were excluded since their β2MG levels were < 30 mg/L at the initiation of PD + HD combination therapy. The types of HD dialyzer used were I-a (n = 10) and II-a (n = 1) at 3 months, I-a (n = 8) and II-a (n = 3) at 6 months, and I-a (n = 6), II-a (n = 4), and S (n = 1) at 12 months. Clinical characteristics of the patients in this study in the present study is shown in Table 1. Timing of taking the blood sample for β2MG was before the HD session at 3, 6, 12 months in all patients.
Measurements and outcomes
The primary outcome was change in β2MG level at 12 months after the start of PD + HD combination therapy. The secondary outcome was the relationship between the decrease in β2MG levels and its related factors for 12 months. The related factors included age, sex, body mass index (BMI), β2MG level, blood urea nitrogen, creatinine, albumin, C-reactive protein, PD fluid volume, vintage of PD, weekly Kt/V of PD, dry weight, type of dialyzer, blood flow rate, HD treatment time per session, and Kt/V of HD at 0, 3, 6, and 12 months after the start of PD + HD combination therapy.
For analysis of the changes in β2MG after the initiation of PD + HD combination therapy over 12 months, the patients were divided into three groups according to the magnitude of the change in β2MG (Δβ2MG) in each patient as: increased: Δβ2MG of more than + 0.789 mg/L, no change: Δβ2MG between − 0.789 and + 0.789 mg/L, and decreased group: Δβ2MG of less than − 0.789 mg/L. This cut-off value was calculated using the data from 10 stable HD patients for 12 months. The average value of the 95% confidence interval of the coefficient of variation of the β2MG value of the 10 HD patient’s over a 12-month period was determined as − 0.789 and + 0.789 mg/L.
Statistical analysis
Results are presented as the mean ± standard deviation for normally distributed data and the median (minimum–maximum) for data with non-normal distribution. Comparisons of β2MG values after the initiation of PD + HD treatment were performed with repeated-measures analysis of variance (ANOVA), followed by the Tukey test. Cochran’s Q test was applied to compare the changes in β2MG between 0, 3, 6, and 12 months. Multiple regression analysis and Pearson's correlation coefficient were used to detect factors that affect Δβ2MG. All statistical analyses were performed using SPSS software (version 24) with p values < 0.05 considered to be significant.
Results
Effect of PD + HD combination therapy on β2 microglobulin reduction
The combination therapy of PD and once-weekly HD statistically significantly reduced β2MG levels, and the effect was maintained for 12 months. Mean values of β2MG at baseline, and 3, 6, and 12 months were 36.7 ± 6.7 mg/L, 33.4 ± 6.1 mg/L, 32.9 ± 4.5 mg/L, and 33.3 ± 5.3 mg/L, respectively. Mean values of β2MG at 3, 6, and 12 months were decreased significantly compared to baseline values, as seen by repeated-measures ANOVA with Tukey’s correction (Fig. 2).
Changes in serum β2 microglobulin by PD + HD combination therapy over 12 months. PD peritoneal dialysis, HD hemodialysis. Repeated-measures analysis of variance (ANOVA) with Tukey corrections revealed statistically significant decreases in serum β2 microglobulin over the 12-month follow-up (p = 0.006). Mean values of β2MG (mean ± standard deviation) at 0, 3, 6, and 12 months were 36.7 ± 6.7 mg/L, 33.4 ± 6.1 mg/L, 32.9 ± 4.5 mg/L and 33.3 ± 5.3 mg/L, respectively
Changes in Δβ2MG after the initiation of PD + HD combination therapy over 12 months are shown in Fig. 3. Mean values of Δβ2MG at 3, 6, and 12 months were − 3.3 ± 4.3 mg/L, − 3.8 ± 4.0 mg/L, and − 3.4 ± 4.6 mg/L, respectively. Nine patients (82%) experienced a decrease in β2MG throughout the 12-month observation period.
Changes in β2 microglobulin (Δβ2MG) after the initiation of PD + HD combination therapy over 12 months. PD peritoneal dialysis, HD hemodialysis. We divided the patients into three groups based on changes in β2 microglobulin: increased group, no change group, decreased group. Δβ2MG ranged from − 0.789 mg/L to 0.789 mg/L in the no change group, defined based on the data from 10 stable HD patients. Mean values of Δβ2MG (mean ± standard deviation) at 3, 6, and 12 months were − 3.3 ± 4.3 mg/L, − 3.8 ± 4.0 mg/L, and − 3.4 ± 4.6 mg/L, respectively
The percentage of patients with β2MG values less than 30 mg/L after the initiation of PD + HD combination therapy over the 12-month period is shown in Fig. 4. Only 27–36% of all patients achieved the target β2MG value of less than 30 mg/L at different points during the observation period: 4 cases (36%) at 3 months, 3 cases (27%) at 6 months, and 3 cases (27%) at 12 months. Cochran’s Q test did not show significant differences in the percentages of such patients in each group for any period (p = 0.717).
Percentage of patients with β2 microglobulin values less than 30 mg/L after the initiation of PD + HD combination therapy over 12 months. The number of patients whose β2 microglobulin value was less than 30 was approximately 30% throughout the observation period. Cochran’s Q test did not show significant differences in the percentages of patients in each group in all the study periods (p = 0.717)
No statistically significant difference was observed in the characteristics, including BMI, dialysis history, and urine volume, renal Kt/V and renal CCr between β2MG level of < 30 mg/L-achievement group and the non-achievement group. BMI, dialysis history, and urine volume, renal Kt/V, and renal CCr in the achievement group at 12 months were 26.9 ± 5.3 kg/m2 (BMI), 3.5 ± 0.9 years (dialysis history), 0 mL/day (urine volume), 0.0 (renal Kt/V), and 0.0 (renal CCr), respectively.
In this study, we changed the dialyzer from I-a to II-a in three patients during the study period to increase the removal efficiency of β2MG. As the time of the dialyzer was changed, β2MG values of the three patients were 34.7, 44.4, and 29.2 mg/dL, respectively. None of these three patients achieved β2MG levels less than 30 mg/dL at 12 months (38.9, 39.5 and 32.9 md/dL). Also, no correlation was found between Δβ2MG and dialyzer type.
Factors that contribute to the decrease in β2 microglobulin
Next, we analyzed the correlation between Δβ2MG and related factors, including patient background (age, BMI, vintage of PD therapy), laboratory data (hemoglobin, albumin, blood urea nitrogen, creatinine, C reactive protein, baseline value of β2MG), dialysis-related factors (total PD fluid volume per day, weekly Kt/V of PD, blood flow rate of HD session, Kt/V of HD), and residual renal function (urine volume, renal creatinine clearance, renal Kt/V) (Table 2). On univariate analysis, serum albumin levels, blood flow rates of HD, residual renal function, and baseline β2MG were associated with a decrease in serum β2MG levels. Albumin and urine output were suggested to be independent influencing factors of Δβ2MG in multivariate analysis. Serum albumin at 3 and 12 months correlated significantly with Δβ2MG (β = − 0.990, p = 0.032 at 3 months, β = − 0.551, p = 0.033 at 12 months). Urine volume at 12 months correlated significantly with Δβ2MG (β = 0.507, p = 0.019). On the other hand, no significant difference was observed in multivariate analysis for baseline β2MG and blood flow rates, which showed significant difference in univariate analysis.
Discussion
Studies examining how much serum β2MG levels improve with combination PD + HD therapy, and which factors contribute to the improvement in β2MG levels, have been limited.
The present study revealed that the combination therapy of PD and once-weekly HD statistically significantly reduced serum β2MG levels, and the effect was maintained for 12 months. However, although statistically significant, the effect is clinically limited (Δβ2MG = − 3.4 mg/L/12 months), with only 27–36% of patients showing β2MG values less than 30 mg/L after the initiation of PD + HD combination therapy. A previous study showed similar results. In that study, serum β2MG levels were not decreased even after the introduction of combination therapy [18]. Additionally, serum β2MG levels were not significantly reduced with both short-term and long-term combination therapy in that study, with levels of 31.9 ± 6.5 mg/L at 0 months, 31.7 ± 6.9 (p = 0.8452) at 6 months, and 30.3 ± 6.3 (p = 0.1247) at 12 months.
Although Japanese guidelines for PD recommend that the target serum β2MG level for combination therapy should be below 30 mg/L, introduction of combination therapy failed to achieve this target level in our patients. One of the reasons for the limited decrease in serum β2MG levels was the decline in residual renal function during the course of the study, which is a major elimination route of β2MG in PD patients. Another factor was probably an inadequate HD prescription, e.g., the choice of dialysis membrane, setting of blood flow rate, and time on HD after the combination therapy.
In terms of the factors contributing to the reduction of serum β2MG are serum albumin levels, blood flow during HD sessions, residual renal function (urine volume, renal creatinine clearance, renal Kt/V), and baseline β2MG levels. In this study, β2MG levels were significantly lower at 3 and 12 months in patients with higher albumin levels (β = − 0.990, p = 0.032 at 3 months, β = − 0.551, p = 0.033 at 12 months). Our treatment protocol is probably one of the reasons for this phenomenon. At our hospital, we replace the dialysis membrane to increase the efficiency of dialysis. A serum albumin level 3.4 g/dL or more is considered as a replacement requirement of dialyzer type. When serum albumin is less than 3.4 g/dL, we don’t change the dialysis membrane in order to minimize the risk of albumin loss by high-efficiency dialysis. Hence, it is likely that the high-efficiency dialyzer was positively selected in cases with high albumin levels, resulting in greater clearance of β2MG and a higher Δβ2MG in these patients. Blood flow rate in HD session is an important factor for determining Kt/V and the clearance of low molecular solutes, such as urea. The relationship between blood flow rate and β2MG reduction has been demonstrated by Leclerc et al. [19]. They showed that the reduction ratio of β2MG slightly but significantly increased from 0.40 ± 0.07 to 0.45 ± 0.06 and 0.48 ± 0.06 when the blood flow rate was increased (300, 350 and 450 mL/min) [20]. Accordingly, our data and this previous report indicating that increasing the blood flow rate is a useful method for increasing the clearance of β2MG suggest that achieving highly efficient HD with a high blood flow rate is recommended.
Interestingly, serum β2MG at 6 and 12 months tended to decrease more in cases with high baseline β2MG (6 months: r = − 0.764, p = 0.006; 12 months: r = − 0.629, p = 0.038). This is probably a reflection of the appropriate adjustment of the dialysis prescription when β2MG values at baseline were high. The fact that there was a correlation between baseline β2MG levels and blood flow in HD sessions at 6 and 12 months (6 months: r = 0.804, p = 0.003, 12 months: r = 0.799, p = 0.003) might well support this notion.
In this study, multivariate analysis revealed urine volume correlated significantly with Δβ2MG (β = 0.507, p = 0.019) at 12 months. Preservation of residual renal function is associated with better long-term survival in dialysis patients and increased serum β2MG clearance and lower serum β2MG [20, 21]. Our data confirmed that the reduction in β2MG was greater in patients with higher residual renal function. Therefore, even in patients with PD + HD combination therapy, preservation of residual renal function is suggested to be important.
Furthermore, we cannot detect the significant difference in background between β2MG increased group and decreased group (Table 3). Also, no statistically significant difference in body weight, serum blood urea nitrogen, serum albumin, hemoglobin, and blood pressure were observed between 0 and 12 months (Table 4). Only serum creatine was significantly lower at 12 months compared to 0 months (p = 0.041).
Hemodialysis prescriptions need to be adjusted to reduce serum β2MG levels in combination therapy with PD and HD. Despite this, however, we observed that serum β2MG levels did not satisfactorily decrease in our patients. When looking at the changes in β2MG levels of eight patients (age 67.0 ± 7.0 years, PD duration 3.7 ± 1.8 years) who had transferred from PD alone to regular HD (three times weekly using a high performance membrane, 4–5 h each session with QB 200–250 mL/min) at our institution, there were no significant changes in β2MG levels: 30.5 ± 2.2 mg/L at 0 months and 31.1 ± 3.8 at 12 months (p = 0.697) (unpublished data) following the switch to HD. Taking these data together, it seems that there is a limitation in respect to the decreasing serum β2MG levels by combination therapy of PD plus once a week HD(4 h).
On the other hand, several previous studies have reported that hemodiafiltration (HDF), especially online HDF, can effectively reduce serum β2MG [22, 23]. Lin CL et al. reported that long term HDF further reduced pre-dialysis serum β2MG levels compared to high flux HD [22]. This suggests that online HDF might be more beneficial than HD using high-flux membranes for β2MG management in PD + HD combination therapy. This needs to be studied in future.
The limitations of this study are the: (1) single-center retrospective design, (2) small number of participants, (3) short observation period, and 4) insufficient bias adjustment for related factors that might contribute to the decrease in β2MG.
Conclusion
Combination therapy of PD and HD might reduce serum β2MG levels, but with marginal efficacy. Our preliminary data indicate that the combination therapy of PD and once weekly HD is not sufficient to significantly decrease serum β2MG levels. Additional HD prescriptions, such as increase in blood flow rate and hemodiafiltration, need to be tested in order to improve β2MG levels in these patients.
Availability of data and materials
Not applicable.
References
Masakane I, Nakai S, Ogata S, et al. Annual dialysis data report. 2014, JSDT renal data registry (JRDR). Renal Replace Ther. 2017;2017(3):18.
Murashima M, Hamano T, Abe M, et al. Combination of once-weekly haemodialysis with peritoneal dialysis is associated with lower mortality compared with peritoneal dialysis alone: a longitudinal study. Clin Kidney J. 2020;14:1610–7.
Fukui H, Hara S, Hashimoto Y, et al. Review of combination of peritoneal dialysis and hemodialysis as a modality of treatment for end-stage renal disease. Ther Apher Dial. 2004;8:56–61.
Koch KM. Dialysis-related amyloidosis. Kidney Int. 1992;41:1416–29.
Drueke TB, Massy ZA. Beta2-microglobulin. Semin Dial. 2009;22:378–80.
Acchiardo S, Kraus AP Jr, Jennings BR. Beta 2-microglobulin levels in. patients with renal insufficiency. Am J Kidney Dis. 1989;13:70–4.
Donadio C, Lucchesi A, Ardini M, et al. Cystatin C, beta 2-microglobulin, and retinol-binding protein as indicators of glomerular filtration rate: comparison with plasma creatinine. J Pharm Biomed Anal. 2001;24:835–42.
Bianchi C, Donadio C, Tramonti G, et al. Reappraisal of serum beta2-microglobulin as marker of GFR. Ren Fail. 2001;23:419–29.
Brown PH, Kalra PA, Turney JH, et al. Serum low-molecular-weight proteins in haemodialysis patients: effect of residual renal function. Nephrol Dial Transplant. 1988;3:169–73.
Eknoyan G, Beck GJ, Cheung AK, et al. Effect of dialysis dose and membrane flux in maintenance hemodialysis. N Engl J Med. 2002;347:2010–9.
Penne EL, van der Weerd NC, Blankestijn PJ, et al. Role of residual kidney function and convective volume on change in beta2-microglobulin levels in hemodiafiltration patients. Clin J Am Soc Nephrol. 2010;5:80–6.
Amici G, Virga G, Da Rin G, et al. Serum beta-2-microglobulin level and residual renal function in peritoneal dialysis. Nephron. 1993;65:469–71.
Cheung AK, Rocco MV, Yan G, et al. Serum beta-2 microglobulin levels predict mortality in dialysis patients: results of the HEMO study. J Am Soc Nephrol. 2006;17:546–55.
Cheung AK, Greene T, Leypoldt JK, et al. Association between serum 2-microglobulin level and infectious mortality in hemodialysis patients. Clin J Am Soc Nephrol. 2008;3:69–77.
Okuno S, Ishimura E, Kohno K, et al. Serum beta2-microglobulin level is a significant predictor of mortality in maintenance hemodialysis patients. Nephrol Dial Transplant. 2008;24:571–7.
Koh ES, Lee K, Kim SH, et al. Serum B2-microglobulin predicts mortality in peritoneal dialysis patients: a prospective cohort study. Am J Nephrol. 2015;42:91–8.
Peritoneal Dialysis Guideline Revision Working Group. Japanese Society of Dialysis Therapy Guidelines for Peritoneal Dialysis. 2019 https://minds.jcqhc.or.jp/docs/gl_pdf/G0001152/4/peritoneal_dialysis.pdf(in Japanese)
Kanda R, Io H, Nakata J, et al. Evaluation of long-term combination therapy with peritoneal dialysis and hemodialysis. Ther Apher Dial. 2017;21(2):180–4.
Leclerc M, Bechade C, Henri P, et al. Does the blood pump flow rate have an impact on the dialysis dose during low dialysate flow rate hemodialysis? Blood Purif. 2018;46:279–85.
Wang AY, Woo J, Wang M, et al. Important differentiation of factors that predict outcome in peritoneal dialysis patients with different degrees of residual renal function. Nephrol Dial Transplant. 2005;20:396–403.
Bammens B, Evenepoel P, Verbeke K, et al. Time profiles of peritoneal and renal clearances of different uremic solutes in incident peritoneal dialysis patients. Am J Kidney Dis. 2005;46:512–9.
Panich A, Tiranathanagul K, Praditpornsilpa K, et al. The effectiveness of on-line hemodiafiltration on beta-2 microglobulin clearance in end stage renal disease. J Med Assoc Thai. 2006;89:S1-8.
Lin CL, Yang CW, Chiang CC, et al. Long-term on-line hemodiafiltration reduces predialysis beta-2-microglobulin levels in chronic hemodialysis patients. Blood Purif. 2001;19:301–7.
Acknowledgements
The manuscript publication of present study was supported by fund from Japanese Society for Peritoneal Dialysis (2022).
Funding
This study was supported by the funding from Japanese Society for Peritoneal Dialysis (Co-medical award of 2021 JSPD annual meeting).
Author information
Authors and Affiliations
Contributions
MN presented the idea of the study. All authors participated in the planning of the study and discussed the results. SM, SN, and YT collected the data, and YT and KW analyzed the data. SM, KW, and MN finalized the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the research ethics committee of St Luke's International Hospital (Approval Number 21-R156).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Moriya, S., Nishizawa, S., Tsuchihashi, Y. et al. Impact on change in serum beta 2 microglobulin by combination therapy of peritoneal dialysis and hemodialysis: a 12-month preliminary observational study. Ren Replace Ther 8, 55 (2022). https://doi.org/10.1186/s41100-022-00447-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-022-00447-y