Abstract
Background
Icodextrin enhances peritoneal filtration for patients on peritoneal dialysis (PD). However, clinically important outcomes have not yet been analyzed using authentic, objective statistical methods. The present systematic review aimed to determine the risks and benefits of icodextrin compared with a glucose-based solution with respect to clinically important and patient-centered outcomes.
Methods
We systematically investigated only randomized controlled trials (RCTs) by adopting the Cochrane Database of Systematic Review (2014) and searched the CENTRAL, MEDLINE, and EMBASE databases for eligible studies reported in the literature. The quality of the evidence was assessed using the GRADE approach.
Results
We finally evaluated important outcomes in 13 RCTs. Icodextrin significantly decreased the number of reported episodes of uncontrolled fluid overload in four RCTs that involved 236 patients (relative risk [RR], 0.31; 95% confidence interval [CI], 0.12 to 0.82; moderate certainty evidence). However, the inclusion of icodextrin for peritoneal ultrafiltration did not significantly differ in six RCTs involving 252 patients (mean difference [MD], 186.76 mL; 95% CI, − 47.08 to 420.59; low certainty evidence). Regarding other clinically important outcomes, all-cause mortality in 10 RCTs involving 1106 patients (RR, 0.75; 95% CI, 0.33 to 1.71; low certainty evidence) and technical survival in five RCTs involving 470 patients (RR, 0.57; 95%CI, 0.29 to 1.12; low certainty evidence) were not significant. Urine volume in four RCTs involving 136 patients, residual renal function in five RCTs involving 181 patients and peritoneal function measured as the ratio of solute concentration in dialysate and plasma (D/P ratio) in two RCTs involving 105 patients were not specifically affected by icodextrin, and the results for adverse events were similar between icodextrin and glucose PD solutions.
Conclusion
Icodextrin could relieve uncontrolled fluid overload without adding risk. However, a significant effect on clinically relevant outcomes such as technical survival and overall patient survival was not suggested. More trials are required to increase the statistical power and to verify the value of icodextrin in clinical practice.
Trial registration
PROSPERO, CRD42018104360
Similar content being viewed by others
Background
Guidelines need to be updated to reflect the current status of patients on peritoneal dialysis (PD) in Japan. Therefore, reliable revised guidelines should be formulated that contain graded evaluations and recommendations to improve patient prognosis. To ensure the reliability of medical information, the Japan Society for Dialysis Therapy (JSDT) revised the clinical practice guideline (CPG) in 2016 based on the GRADE (Grading of Recommendations Assessment, Development and Evaluation) system [1], which is the current global standard method of creating guidelines. In the meantime, icodextrin has become prevalent in Japanese routine clinical practice during the past two decades, and it now occupies an extremely important position based on distinctive characteristics. Ultrafiltration of the peritoneal membrane is essentially important as it is associated with the management of fluid status and it is a determinant of whether or not to continue with PD therapy [2, 3]. Icodextrin is a high-molecular-weight, water-soluble glucose polymer in a sustained colloid osmotic gradient that helps to control excess fluid in patients treated by PD [4]. Icodextrin facilitates prolonged and stable peritoneal filtration regardless of the peritoneal function of patients and has thus improved the global quality of clinical peritoneal dialysis. Considerable evidence has recently accumulated about the role of icodextrin in clinical practice [5, 6]. However, icodextrin as a peritoneal solution has not been fully evaluated at the level of patient-centered outcomes. Furthermore, patient values have not been adopted to evaluate its effect. Thus, the risks of benefits of icodextrin remain obscure. A systematic review should compare clinical effects between icodextrin and glucose solutions.
Methods
Inclusion and exclusion criteria
We included RCTs that compared icodextrin with glucose solutions among patients on PD. The exclusion criteria comprised PD with a neutral-buffered solution, peritonitis associated with PD, and studies other than RCTs. Patients who received PD and HD combination therapy were not included in the RCTs adopted in the present systematic review (SR).
Searches
We created a SR that complied with Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [7] (Additional file 1). Before starting the present SR, we registered the review protocol (PROSPERO: CRD42018104360) and adopted the extant a reliable SR, the Cochrane Database of Systematic Reviews (2014) for an initial systematic review [8]. That search was in accordance with the Cochrane Renal Group’s Specialized Register that comprises studies identified from the CENTRAL, MEDLINE, and EMBASE databases. We then searched MEDLINE and Ichushi-Web to identify further investigation to date. Four reviewers (AK, TF, EF, and KW) independently screened all titles, abstracts and the full texts of articles.
Data extraction
Four reviewers (AK, TF, EF, and KW) independently extracted data using a pre-specified format in advance and integrated the results. Disagreements about data collection were resolved by consultation with YT. One reviewer (TF) verified the results, and another (KW) stored the data extracted from each study in a specific format suitable for analysis.
Risk of bias (quality) assessment
Two independent reviewers (AK, TF) used the standard Cochrane Collaboration risk of bias tool to assess bias in all eligible studies evaluate it in the present SR. Discrepancies were resolved by group discussion to reach a consensus. The following sources of bias were assessed: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias), and other sources. We evaluated the certainty of evidence for the main outcomes using the GRADE approach [9].
Strategy for data synthesis
Data were integrated using a random-effects model. Results are expressed as RRs with 95% CIs for dichotomous outcomes, and the MD was used for continuous outcomes. Heterogeneity was examined using χ2 on N-1 degrees of freedom with an alpha level of 0.05 for statistical significance, and I2 tests. Data were analyzed using Review Manager (RevMan Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). P values of < 0.05 were defined as statistically significant.
Results
Study selection
Figure 1 shows a PRISMA flow diagram of the present SR. We extracted and assessed 106 studies of SRs and meta-analysis published between 1968 and 2017. Among them, four SRs and one CPG met the eligibility criteria and the antecedent Cochrane review was adopted. We subsequently selected 10 RCTs that compared icodextrin and glucose solutions. While searching RCTs published after the initial SR, we added three RCTs that satisfied our inclusion conditions among 260 studies, and finally, used 13 RCTs as core studies.
Characteristics of included studies
We analyzed data of 1275 patients that included 677 who were treated by PD using icodextrin [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31]. Among 13 studies, five, three, and one were of patients treated with continuous ambulatory peritoneal dialysis (CAPD) [1011–12], automated peritoneal dialysis (APD) [11, 13, 14], and continuous cycling peritoneal dialysis (CCPD) [15], respectively, and the remainder comprised combinations of the modalities. Two studies involved patients only with diabetes [16, 17] and one of the other studies was limited to non-diabetic patients [18]. Three studies allowed a choice of dialysates with appropriate glucose concentrations to achieve desirable control of edema or blood pressure [10, 14, 19]. Three studies were restricted to patients with high or high-average peritoneal solute transport as the principal inclusion criterion [13, 17, 20]. Two studies excluded patients with uncontrolled volume status at the time of entry [10, 21]. Table 1 shows the characteristics and outcomes of the included studies. We also evaluated each outcomes according to the GRADE approach (Table 2).
Risk of bias in included studies
Figure 2 shows the risk of bias in the included studies. Risk of bias was generally low for random sequence generation and allocation concealment, but most studies were considered unclear regarding blinding of outcome assessments and outcome data were incomplete in five studies.
All-cause mortality
The effects of icodextrin and glucose solutions on patient survival did not significant differ in 10 RCTs of 1106 patients (RR, 0.75; 95% CI, 0.33 to 1.71; P = 0.49, I2 = 0%; low certainty evidence; Fig. 3). However, the point estimate was better for icodextrin than glucose solutions by 7 patients’ reductions among 1000 patients.
Technical survival
An overall effect of icodextrin on technical survival was not significant in five RCTs of 470 patients (RR, 0.57; 95% CI, 0.29 to 1.12; P = 0.10, I2 = 0%; low certainty evidence; Fig. 4).
Episodes of uncontrolled peritoneal fluid overload
Icodextrin significantly decreased the frequency of reported episodic uncontrolled peritoneal fluid overload in four RCTs of 236 patients (RR, 0.31; 95% CI, 0.12 to 0.82; P = 0.02, I2 = 0%; moderate certainty evidence; Fig. 5).
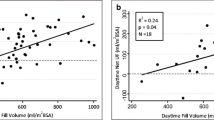
Peritoneal ultrafiltration
Icodextrin solution did not lead to a significant increase in peritoneal ultrafiltration compared with glucose solutions in six RCTs of 252 patients (MD, 186.76 mL/day; 95% CI, − 47.08 to 420.59; P = 0.12, I2 = 64%; low certainty evidence; Fig. 6). Moderate to severe heterogeneity might have been derived from the study design. The design of five studies was open-label and dropout rates were high in all of them. These results might also be biased and attenuated in relation to icodextrin because hypertonic 3.86% and 4.25% glucose PD solutions served as controls without restrictions in two trials [15, 19].
Urine volume
Icodextrin was not associated with urine volume in four RCTs of 136 patients (MD, 106.08 mL/day; 95% CI, − 173.29 to 385.45; P = 0.13, I2 = 39%; low certainty evidence; Additional file 2: Figure S1). However, one RCT demonstrated that icodextrin was associated with significantly higher daily urine volumes than glucose dialysate at 12 months [19].
Residual renal function
Residual renal function determined from glomerular filtration rates or renal creatinine clearance was similar between icodextrin and glucose PD solution in five RCTs of 181 patients (MD, 0.56 mL/min; 95% CI − 0.37 to 1.49; P = 0.24, I2 = 0%; moderate certainty evidence; Additional file 2: Figure S2). Among the included studies, one study used the averages of creatinine and urea clearance to indicate residual renal function [14], and this was adopted and evaluated in the preceding SR [8].
Peritoneal function
We adopted dialysate-to-plasma creatinine ratio (D/P Cr) as a marker of peritoneal function. However, the amount of clinical research was insufficient to evaluate outcomes, and icodextrin did not affect the D/P Cr with a moderate level of heterogeneity in two RCTs that included 105 patients (MD, 0.001; 95% CI, − 0.07 to 0.07; P = 0.97, I2 = 65%; very low certainty evidence; Additional file 2: Figure S3).
Peritonitis
Overall peritonitis rates did not significantly differ between icodextrin and glucose PD solutions in eight RCTs of 1034 patients (RR, 0.95; 95% CI, 0.79 to 1.15; P = 0.62, I2 = 0%; low certainty evidence; Additional file 2: Figure S4).
Rash
The occurrence of rash elicited by icodextrin and glucose PD solutions did not significantly differ in four RCTs of 855 patients (RR, 1.84; 95% CI, 0.48 to 7.09; P = 0.35, I2 = 46%; low certainty evidence; Additional file 2: Figure S5). Most reports are based on comparative trials that processed at the time when icodextrin entered the market.
Discussion
The present review found that the quality of evidence supporting icodextrin was moderate and significantly associated with a decreased frequency of uncontrolled fluid overload compared with glucose solutions. However, icodextrin did not contribute to improved all-cause mortality and technical survival. In addition, icodextrin was not associated with increased urine volumes, or the D/P creatinine ratio as an indicator of peritoneal creatinine clearance. Recent results have been consistent with those of an earlier systematic review, which concluded that icodextrin alleviated uncontrolled fluid overload better than glucose solutions [5]. Uncontrolled fluid overload was not strictly defined in the studies included herein, and only one study found excessive volumes lead to technical failure [16]. On the other hand, icodextrin was not associated with a significant increase in peritoneal filtration compared to glucose solutions in the present SR. The lack of significance might be derived, at least in part, from the following. The present SR included prospective RCTs that allowed the choice of dialysates with glucose concentrations up to 4.25% [15, 19]. These studies had considerable weight in the overall evaluation of peritoneal ultrafiltration outcomes. Additionally, the present SR defined peritoneal ultrafiltration as overall daily output, and not as a longer dwell period. Therefore, some studies did not meet our inclusion criteria. The volume of peritoneal ultrafiltration was significantly greater in the control than the icodextrin group in one study, which could be explained by the dialysate comprising > 2.5% glucose [19]. The study protocol required that the control group underwent four exchanges of dialysate with glucose, whereas icodextrin was applied once for the long dwell and the glucose dialysate was exchanged twice in the experimental group. Another explanation might be associated with a need to convert the standard error or 95%CI into standard deviation, which contributed heterogeneity [18, 21]. These factors might have diminished the advantage of icodextrin in terms of peritoneal ultrafiltration compared with glucose solutions.
One study recommended that APD and icodextrin should be considered for patients with high or high-average solute transport and that issues related to high transport could be avoided by using icodextrin for the long exchange to prevent fluid reabsorption [22]. Patients with fluid reabsorption in the long dwell should be identified to maximize the benefits of icodextrin and consider its appropriate indication in clinical practice.
The occurrence of rash in icodextrin was marginally significant compared with glucose solution. Previous studies have concluded that the incidence of rash is not significantly higher for icodextrin than glucose solutions, and notable, rash was most frequently reported when icodextrin first entered the market [13, 23]. However, the prevalence of rash has remarkably decreased since then [10, 11]. The present SR included maculopapular reactions as rash, unlike previous studies. Consequently, the incidence of rash did not significantly differ between icodextrin and glucose solutions.
Here, we determined which outcomes were important to clinical practice after discussion at two consecutive panel meetings. Differences in their opinions were addressed by voting among committees and the process of creating an SR was developed. Four independent investigators collected the studies for review and analyzed the data. A standardized method of peritoneal function assessment has not been established and the numbers of RCT were insufficient to evaluate the reliability of this parameter as an indicator. Therefore, the importance of peritoneal function, determined as D/P creatinine, was not as critical as all-cause mortality and technical survival. Finally, the last panel meeting concluded that peritoneal function as an outcome should be modified and downgraded.
The present review had some limitations. Firstly, the degree of heterogeneity was high in eligible studies with respect to the glucose concentrations of control PD dialysates. Secondly, some outcomes had no definite criteria or indicators, which might have resulted in selection bias derived from the extracted studies. As to technical survival, we defined it as the number of patients who were forced to discontinue PD and transited to HD treatment, while death, transplantation, recovery of renal function, and loss to follow-up were not counted. Consequently, the difference in the definition of technical survival resulted in a discrepancy of the number of events reported in each study. Thirdly, we use icodextrin for patients with excessive fluid tendencies in clinical practice. However, the patients in the reviewed studies did not necessarily have issues with fluid management. This discrepancy might lead to a concern regarding routine icodextrin treatment for more efficient water removal among patients on PD without a fluid excess. Finally, subgroups were not analyzed when analytical findings found no overall effect. Therefore, patients that might benefit from icodextrin could not be confirmed for each outcome.
Conclusions
The present SR suggests that icodextrin could reduce the frequency of uncontrolled fluid overload and ameliorate impaired peritoneal ultrafiltration among patients with PD. However, all-cause mortality, technical survival and peritoneal ultrafiltration did not significantly differ between icodextrin and PD solutions. The present SR reflects an important relationship between icodextrin dialysate and patient-centered outcomes among PD patients.
Abbreviations
- APD:
-
Automated peritoneal dialysis
- CAPD:
-
Continuous ambulatory peritonealdialysis
- CCPD:
-
Continuous cycling peritonealdialysis
- CI:
-
Confidence interval
- CPG:
-
Clinical practice guideline
- D/P Cr:
-
Dialysate-to-plasma creatinine ratio
- GRADE:
-
Grading of Recommendations Assessment, Development and Evaluation
- JSDT:
-
Japan Society for Dialysis Therapy
- MD:
-
Mean difference
- PD:
-
Peritoneal dialysis
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA)
- RCTs:
-
Randomized controlled trials
- RR:
-
Relative risk
- SR:
-
Systematic review
References
GRADE (Grading of Recommendations Assessment, Development and Evaluation) working group, http://www.gradeworkinggroup.org/. Accessed 1 May 2019.
Davies SJ, Phillips L, Griffiths AM, Russell LH, Naish PF, Russell GI. What really happens to people on long-term peritoneal dialysis? Kidney Int. 1988;54(6):2207–17.
Churchill DN, Thorpe KE, Nolph KD, Keshaviah PR, Oreopoulos DG, Pagé D. Increased peritoneal membrane transport is associated with decreased patient and technique survival for continuous peritoneal dialysis patients. The Canada-USA (CANUSA) peritoneal Dialysis study group. J Am Soc Nephrol. 1988;9(7):1285–92.
Moberly JB, Mujais S, Gehr T, Hamburger R, Sprague S, Kucharski A, et al. Pharmacokinetics of icodextrin in peritoneal dialysis patients. Kidney Int Suppl. 2002;81:S23–33.
Cho Y, Johnson DW, Badve S, Craig JC, Strippoli GF, Wiggins KJ. Impact of icodextrin on clinical outcomes in peritoneal dialysis: a systematic review of randomized controlled trials. Nephrol Dial Transplant. 2013;28(7):1899–907.
Qi H, Xu C, Yan H, Ma J. Comparison of icodextrin and glucose solutions for long dwell exchange in peritoneal dialysis: a meta-analysis of randomized controlled trials. Perit Dial Int. 2011;31(2):179–88.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34.
Cho Y, Johnson DW, Craig JC, Strippoli GF, Badve SV, Wiggins KJ. Biocompatible dialysis fluids for peritoneal dialysis. Cochrane Database Syst Rev. 2014;27(3):CD007554. https://doi.org/10.1002/14651858.CD007554.pub2.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Chang TI, Ryu DR, Yoo TH, Kim HJ, Kang EW, Kim H, et al. Effect of icodextrin solution on the preservation of residual renal function in peritoneal dialysis patients: a randomized controlled study. Medicine. 2016;95(13):e2991. https://doi.org/10.1097/MD.0000000000002991.
Lin A, Qian J, Li X, Yu X, Liu W, Sun Y, et al. Randomized controlled trial of icodextrin versus glucose containing peritoneal dialysis fluid. Clin J Am Soc Nephrol. 2009;4(11):1799–804.
Mistry CD, Gokal R, Peers E. A randomized multicenter clinical trial comparing isosmolar icodextrin with hyperosmolar glucose solutions in CAPD. MIDAS study group. Multicenter investigation of Icodextrin in ambulatory Dialysis. Kidney Int. 1994;46(2):496–503.
Finkelstein F, Healy H, Abu-Alfa A, Ahmad S, Brown F, Gehr T, et al. Superiority of Icodextrin compared with 4.25% dextrose for peritoneal ultrafiltration. J Am Soc Nephrol. 2005;16(2):546–54.
Plum J, Gentile S, Verger C, Brunkhorst R, Bahner U, Faller B, et al. Efficacy and safety of a 7.5% icodextrin peritoneal dialysis solution in patients treated with automated peritoneal dialysis. Am J Kidney Dis. 2002;39(4):862–71.
Posthuma N, ter Wee P, Donker, AJ, Dekker HA, Oe PL, Verbrugh HA. Peritoneal defense using icodextrin or glucose for daytime dwell in CCPD patients. Perit Dial Int. 1999;19(4):334–42.
Takatori Y, Akagi S, Sugiyama H, Inoue J, Kojo S, Morinaga H, et al. Icodextrin increases technique survival rate in peritoneal dialysis patients with diabetic nephropathy by improving body fluid management: a randomized controlled trial. Clin J Am Soc Nephrol. 2011;6(6):1337–44.
Posthuma N, ter Wee PM, Donker AJ, Oe PL, van Dorp W, Peers EM, et al. Serum disaccharides and osmolality in CCPD patients using icodextrin or glucose as daytime dwell. Perit Dial Int. 1997;17(6):602–7.
de Moraes TP, Andreoli MC, Canziani ME, da Silva DR, Caramori JC, Ponce D, et al. Icodextrin reduces insulin resistance in non-diabetic patients undergoing automated peritoneal dialysis: results of a randomized controlled trial (STARCH). Nephrol Dial Transplant. 2015;30(11):1905–11.
Yoon HE, Chang YK, Shin SJ, Choi BS, Kim BS, Park CW, et al. Benefits of a continuous ambulatory peritoneal dialysis (CAPD) technique with one icodextrin- containing and two biocompatible glucose-containing dialysates for preservation of residual renal function and biocompatibility in incident CAPD patients. J Korean Med Sci. 2014;29(9):1217–25.
Davies SJ, Woodrow G, Donovan K, Plum J, Williams P, Johansson AC, et al. Icodextrin improves the fluid status of peritoneal dialysis patients: results of a double-blind randomized controlled trial. J Am Soc Nephrol. 2003;14(9):2338–44.
Konings CJ, Kooman J, Schonck M, Gladziwa U, Wirtz J, van del Wall Bake AW, et al. Effect of icodextrin on volume status, blood pressure and echocardiographic parameters: a randomized study. Kidney Int. 2003;63(4):1556–63.
Woodrow G, Fan SL, Reid C, Denning J, Pyrah AN. Renal Association Clinical Practice Guideline on peritoneal dialysis in adults and children. BMC Nephrol. 2017;18(1):333.
Wolfson M, Piraino B, Hamburger RJ, Morton AR; Icodextrin Study Group. A randomized controlled trial to evaluate the efficacy and safety of icodextrin in peritoneal dialysis. Am J Kidney Dis. 2002;40(5):1055–65.
Kooman JP, Schalkwijk CG, Konings CJ. The increase in plasma levels of Nepsilon-(Carboxymethyl) lysine during icodextrin treatment of peritoneal dialysis patients is not associated with increased plasma levels of vascular cell adhesion molecule-1. Perit Dial Int. 2006;26(3):410–11.
Gokal R, Mistry CD, Peers E. Peritonitis occurrence in a multicenter study of icodextrin and glucose in CAPD. MIDAS Study Group. Multicenter Investigation of Icodextrin in Ambulatory Dialysis. Perit Dial Int. 1995;15(6):226–30.
Paniagua R, Orihuela O, Ventura MD, Avila-Díaz M, Cisneros A, Vincénte-Martínez M, et al. Echocardiographic, electrocardiographic and blood pressure changes induced by icodextrin solution in diabetic patients on peritoneal dialysis. Kidney Int. 2008;(108):S125–30.
Paniagua R, Ventura MD, Avila-Díaz M, Cisneros A, Vincénte-Martínez M, Furlong MD, et al. Icodextrin improves metabolic and fluid management in high and high-average transport diabetic patients. Perit Dial Int. 2009;29(4):422–32.
Orihuela O, de Jesús Ventura M, Ávila-Díaz M, Cisneros A, Vincenté-Martínez M, Furlong MD, et al. Effect of icodextrin on heart rate variability in diabetic patients on peritoneal dialysis. Perit Dial Int. 2014;34(1):57–63.
Posthuma N, ter Wee PM, Donker AJ, Oe PL, Peers EM, Verbrugh HA. Assessment of the effectiveness, safety, and biocompatibility of icodextrin in automated peritoneal dialysis. The Dextrin in APD in Amsterdam (DIANA) Group. Perit Dial Int. 2000;20 (Suppl 2):S106–13.
Posthuma N, ter Wee PM, Niessen H, Donker AJ, Verbrugh HA, Schalkwijk CG. Amadori albumin and advanced glycation end-product formation in peritoneal dialysis using icodextrin. Perit Dial Int. 2001;21(1):43–51.
Posthuma N, ter Wee PM, Verbrugh HA, Oe PL, Peers E, Sayers J, et al. Icodextrin instead of glucose during the daytime dwell in CCPD increases ultrafiltration and 24-h dialysate creatinine clearance. Nephrol Dial Transplant. 1997;12(3):550–3.
Posthuma N, ter Weel PM, Donker AJ, Peers EM, Oe PL, Verbrugh HA. Icodextrin use in CCPD patients during peritonitis: ultrafiltration and serum disaccharide concentrations. Nephrol Dial Transplant. 1998;13(9):2341–4.
Posthuma N, Verbrugh HA, Donker AJ, van Dorp W, Dekker HA, Peers EM, et al. Peritoneal kinetics and mesothelial markers in CCPD using icodextrin for daytime dwell for two years. Perit Dial Int. 2000;20(2):174–80.
Guo A, Wolfson M, Holt R. Early quality of life benefits of icodextrin in peritoneal dialysis. Kidney Int Suppl. 2002;(81):S72–9.
Acknowledgements
The authors sincerely acknowledge the contribution of the National Diet Library of Japan, and are grateful to Shinichi Abe, Mieko Mitsuya, and Chihiro Ishihara for assistance with the initial medical literature search preceding this review.
Funding
None.
Author information
Authors and Affiliations
Contributions
YT, HY, and YI contributed to the research concept and study design. AK, YT, TF, EF, and KW contributed to the data acquisition and AK, YT, TF, EF, KW, and HY contributed to the data analysis/interpretation. AK, YT, TF, and HY contributed to the quality assessment of risk of bias. YT, HY, YI, and HN contributed to the supervision or mentorship. All authors contributed important intellectual content during manuscript drafting or revision and approved the final version of the submitted manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:
The PRISMA checklist of items to include when reporting a systematic review.
Additional file 2:
Figure S1. Effects of icodextrin on urine volume. Figure S2. Effects of icodextrin on residual renal function. Figure S3. Effects of icodextrin on peritoneal function. Figure S4. Effects of icodextrin on peritonitis. Figure S5. Effects of icodextrin on rash.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kanno, A., Tsujimoto, Y., Fujii, T. et al. Comparison of clinical effects between icodextrin and glucose solutions on outcomes of peritoneal dialysis: systematic review and meta-analysis of randomized controlled trials. Ren Replace Ther 6, 7 (2020). https://doi.org/10.1186/s41100-019-0253-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-019-0253-4