Abstract
Background
This study investigated the prevalence of sarcopenia or sarcopenic obesity and their association with frailty and protein-energy wasting (PEW) in hemodialysis patients.
Methods
The present study enrolled 117 adult hemodialysis patients (35% female, 64 ± 12 years old) from single units of a hemodialysis center. The patients were divided into four groups: normal, obese, sarcopenia, and sarcopenic obesity. Sarcopenia was diagnosed by Asian Working Group for Sarcopenia (AWGS) criteria, and obesity was defined as an extensive percent body fat mass greater than 40% in females and 30% in males. Skeletal muscle mass and percent fat mass were evaluated by multifrequency whole-body bioimpedance electrical analysis after a midweek dialysis session. Handgrip strength and a short physical performance battery (SPPB) were assessed before a dialysis session as indicators of muscle strength and physical performance. Moreover, participants completed the Kihon Checklist and the criteria proposed by the International Society of Renal Nutrition and Metabolism expert panel to classify frailty and PEW. We performed multivariate logistic regression analysis to identify the clinical risk of frailty and PEW in patients with sarcopenia or sarcopenic obesity.
Results
Forty-six (39.3%) patients were classified as normal; 18 (15.4%), as obese; 35 (29.9%), as having sarcopenia; and 18 (15.4%), as having sarcopenic obesity. The sarcopenia or sarcopenic obesity group had significantly lower handgrip strength than the normal or obesity group (all p < 0.05). In addition, the sarcopenia and sarcopenic obesity groups had significantly lower SPPB scores than the normal group (p < 0.05, respectively). In the multivariate analysis, the sarcopenic obesity group had a significantly higher risk of frailty than the normal group in the multivariate analysis after adjusting for age and gender (OR 4.518, 95%CI 1.218–16.752, p = 0.024). However, sarcopenic obesity was not associated with a higher likelihood of PEW, and sarcopenia imposed a significantly higher risk of PEW (OR 4.272, 95%CI 1.157–15.778, p = 0.029) than that in the normal group after adjusting for confounding factors.
Conclusion
Sarcopenic obesity was closely associated with frailty compared with the normal condition in HD patients. However, sarcopenic obesity was not associated with a higher likelihood of PEW.
Similar content being viewed by others
Introduction
Obesity is an independent risk factor for morbidity or mortality in the general population [1]. However, the survival rate of obese patients with hemodialysis (HD) is reported to be better than that of normal weight HD patients [2], which has been referred to as the “obesity paradox.” This phenomenon has been explained as “reverse epidemiology” [2]. In brief, underweight patients or patients with weight loss over time show worse outcomes [2]. Sarcopenia is a common comorbidity in elderly patients with HD, particularly those who are underweight or have undergone weight loss [3].
Several studies have shown that obesity can coexist with sarcopenia [3], which is termed sarcopenic obesity. Although both sarcopenia and obesity are linked to functional impairment, frailty or disability, particularly sarcopenic obesity, also has been associated with worse morbidity and mortality than either sarcopenia or obesity alone [4]. However, the diagnostic criteria for sarcopenic obesity are not universally established [5], and its association with frailty and protein-energy wasting (PEW) has not yet been revealed in HD patients.
The understanding that sarcopenic obesity plays a critical role in several common comorbidities, including frailty and PEW, has led to therapeutic approaches that target different aspects of sarcopenic obesity in HD patients. Therefore, the objective of this study was to investigate the variability in the prevalence of sarcopenic obesity in HD patients, as well as its risk for frailty and PEW.
Methods
Subjects
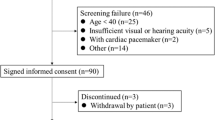
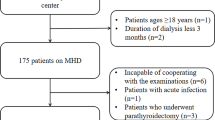
The present study enrolled 117 adult HD patients (35% female, 64 ± 12 years of age) from single units of Meiseikai Toyo Clinic, Japan. Patients were eligible to participate if they were over 18 years of age, had received maintenance HD for at least 6 months, and were able to provide informed consent. This study complied with the principles of the Declaration of Helsinki regarding investigations in humans and was approved by the institutional review boards at the Meisei-kai Toyo clinic. Study collaborators interviewed patients before or during a dialysis session, obtained recent clinical and laboratory data from medical records, and measured muscle strength and physical performance prior to the start of the dialysis session. In addition, study collaborators measured the body composition using a bioimpedance electrical analysis (BIA) after a midweek dialysis session. The various phenotype of interest to this study were sarcopenia, sarcopenic obesity, frailty, anorexia, malnutrition, and PEW (Table 1).
Measurements of body fat and skeletal muscle mass
Skeletal muscle mass was evaluated by multifrequency whole-body BIA after a midweek dialysis session. BIA was measured after dialysis for clinical reasons. The fat mass or skeletal muscle value measured by BIA before dialysis does not distinguish the effect of water retention, including extracellular water and intracellular water. The seca mBCA515 (seca®, Hamburg, Germany), which is an integrated platform with a handrail system, was used. Electrodes were placed in the ascending handrail, of which two were chosen depending on the subject’s height. Patients had to stand upright with the arms outstretched. Another two pairs of electrodes contacted the soles of the feet. The consecutive measurements were performed within a 1-min period. The prediction equations for fat free mass, total body water, and extracellular water were validated by a prior study [12]. Fat mass was calculated as the difference between body weight and fat free mass [13]. Resistance (R) and reactance (Xc) values obtained at 5 and 50 kHz for different body segments were used in the prediction equations. The reference values of fat mass or skeletal muscle mass in the Japanese population were validated [14].
Definition of sarcopenia and sarcopenic obesity
Muscle was calculated with BIA, which has been identified as a feasible, valid, and reliable method for measuring muscle mass by the Working Group on Sarcopenia in Older People (EWGSOP) or Asia Working Group for Sarcopenia (AWGS) [6]. Appendicular skeletal muscle mass (ASM) was measured by BIA, and then the skeletal muscle mass index (SMI) was calculated as ASM (kg)/height (m)2. The cutoff value of SMI for muscle wasting was < 7.0 kg/m2 in men and < 5.7 kg/m2 in women. Sarcopenia was diagnosed according to the AWGS criteria; it was based on evidence of low muscle mass plus either low muscle strength or low physical performance. Obesity was defined as an extensive percent body fat mass greater than 40% in females and 30% in males, as described in prior studies [7]. In the present study, sarcopenic obesity was defined by a combination of sarcopenia diagnosed by the AWGS criteria and higher percent fat mass.
Muscle strength and physical performance
Low muscle strength was based on the measurement of handgrip strength and assessed on the nonfistula hand before a dialysis session using a Jamar® Hydraulic Hand Dynamometer (Patterson Medical, Warrenville, IL, USA). Handgrip strength measurements were repeated in two trials for both the dominant hand and nondominant hand. Patients were seated on a chair with the elbow bent at a 90° angle and the shoulder, forearm, and wrist in a neutral position [15]. Patients were directed to press on the handle with as much force as possible to obtain the maximum handgrip strength for 5 s. The best results for each hand were recorded, and the average value of maximum handgrip strength was calculated. Low muscle strength was defined as a handgrip strength of less than 26 kg in men and 18 kg in women.
Short physical performance battery (SPPB) were evaluated as indicators of functional status and physical performance, as previously described [16]. The SPPB consisted of three components of the physical performance test: a balance test, 4 m walking test, and repeat chair stand test. Three performance tests were scored from 0 to 4 points. The balance test consisted of three balance tests including side-by-side, semitandem, and tandem stands for 10 s each. Patients were asked to walk a marked 4 m course at comfortable pace. Poor physical performance was defined as a usual gait speed of ≦ 0.8 m/s. A five-repetition chair stand test required patients to stand up from and sit down on a 40 cm height armless chair as quickly as possible, five times. Patients folded their arms across their chest and were instructed to stand up completely. Patients had SPPB scores ranging from 0 to 12 points, and lower SPPB scores indicated restricted physical function.
All patients completed the Japanese version of EAT-10 (J-EAT-10), which is a reliable, valid, and practicable screening to assess dysphagia symptom severity. The J-EAT-10 included ten questions, and each question was scored from 0 (no problem) to 4 (severe problem). A higher J-EAT-10 sum score indicated a self-perception of poor swallowing function. Dysphagia was defined as a J-EAT-10 sum score ≧ 3 points as described in a prior study [17, 18].
Assessment of malnutrition and anorexia
Patients were asked to respond to a Mini Nutritional Assessment short form (MNA-SF) [19]. The MNA-SF comprises a 6-item questionnaire: food intake, weight loss, mobility, psychological or acute disease stress, neuropsychological problems, and body mass index. MNA-SF scores range from 0 to 14 points, with lower scores indicating a suspected risk of malnutrition. MNA-SF scores ≦ 11 were defined as being at risk of malnutrition and receiving a subsequent nutritional assessment. The Global Leadership Initiative on Malnutrition (GLIM) criteria diagnose malnutrition using two components: phenotype and etiologic criteria. Malnutrition was defined as present if the patients met at least one criterion from each phenotypic and etiologic component [8]. The prevalence of malnutrition was evaluated according to the GLIM criteria.
Participants completed the Japanese version of the Simplified Nutritional Appetite Questionnaire (SNAQ) [9]. The SNAQ is a 4-item single-domain questionnaire that is verbally labeled on a 5-point Likert scale. The total SNAQ score is the sum of each item score; a lower score indicates more appetite deterioration, and a score of 13 and lower has been proposed as being diagnostic for anorexia. SNAQ is sufficiently reliable and valid for assessing appetite among community-dwelling older adults in Japan [20]. Moreover, SNAQ has a good predictive ability for future protein-energy malnutrition [21].
Assessment of frailty
Participants completed the Kihon Checklist, which is a useful tool for frailty screening including physical, emotional, and social aspects [10]. The Kihon Checklist consists of a 25-item questionnaire with two categories (yes/no questions). The total Kihon Checklist score is the sum of each item score, and the Kihon Checklist score is divided into three categories: robust (0 to 3 points), prefrailty (4 to 7 points), and frailty (≧ 8 points).
Definition of PEW
The criteria proposed by the International Society of Renal Nutrition and Metabolism (ISRNM) expert panel were used to classify PEW [11], which has been described elsewhere [22]. PEW was scored as the grading of 1 selected item in each of the four categories of wasting syndrome as follows: serum albumin, body mass index or unintentional weight loss, predialysis serum creatinine normalized by the body surface area (sCr/BSA), and normalized protein nitrogen appearance (nPNA). The cutoff values were as follows: serum albumin, 3.8 g/dL; BMI, 23 kg/m2 or unintentional weight loss (5% over 3 month or 10% over 6 months); sCr/BSA, 380 μmol/L/m2; and nPNA, 0.8 g/kg per day. BSA was estimated by the following formula: Body surface (cm2) = (weight) 0.425 × (height) 0.725 × 0.007184. A lower value than the cutoff value was scored as 1 point, and the PEW score was calculated as the sum of the four-item score. PEW was defined as a PEW score ≧ 3 points as described by previous studies.
Statistical analysis
Clinical characteristics are described as the mean ± SD and as counts and percentages as appropriate. Continuous data were tested using one-way analysis of variance (ANOVA) to determine whether there were any statistically significant differences among the means of four groups, and categorical or dichotomous variables were compared using Pearson’s chi-squared test. To adjust the effect of potential confounders for sarcopenia and obesity, multivariate logistic regression models of frailty, risk of malnutrition, and PEW were performed, and odds ratios (ORs) and 95% confidence intervals (95% CI) were estimated. Statistical analyses were performed using SPSS software, version 21, and in all statistical calculations, a two-tailed p < 0.05 was considered statistically significant.
Results
One hundred seventeen patients with complete major data were included in the analysis. The average age of patients in the analysis was 64 ± 12 years; 35% of patients were female; dialysis vintage was 7 ± 6 years.
Table 2 shows the difference in clinical characteristics. The patients were divided into four groups on the basis of sarcopenia and obesity: 46 (39.3%) patients were normal, 18 (15.4%) were obese, 35 (29.9%) had sarcopenia, and 18 (15.4%) had sarcopenic obesity. Serum creatinine levels in the sarcopenic obesity and sarcopenia groups were significantly lower than those in the normal and obesity groups (all p < 0.05). Moreover, the SMI in the sarcopenic obesity and sarcopenia groups was significantly lower than that in the normal group (p < 0.05, respectively). However, the prevalence of muscle wasting in the normal and obesity groups was 68% and 94%, respectively. BMI and %fat mass in sarcopenic obesity were significantly higher than those in the normal and sarcopenia groups (all p < 0.05). The sarcopenia group was significantly older than the normal group. However, there were no significant differences among the four groups related to dialysis efficacy, protein intake, swallowing function, and appetite.
Figure 1 shows the results of muscle strength and physical performance. The sarcopenia and sarcopenic obesity groups had a significantly lower handgrip strength than the normal and obesity groups (all p < 0.05). In addition, the sarcopenia and sarcopenic obesity groups had significantly lower SPPB sum scores than the normal group (all p < 0.05). However, the usual gait speed and five-time chair stand test were not associated with sarcopenia/obesity categories.
Figure 2 shows the prevalence of nutritional status, dysphagia, and anorexia. Our findings demonstrated that 22% of subjects in the normal group, 11% in the obese group, 45% in the sarcopenia group, and 18% in the sarcopenic obesity group exhibited at risk of malnutrition based on the MNA-SF (p < 0.05) (Fig. 2a). In addition, the prevalence of malnutrition was 15% in the normal group, 11% in the obese group, 34% in the sarcopenia group, and 12% in the sarcopenic obesity group, as assessed by GLIM criteria (p = 0.07) (Fig. 2a). Our findings demonstrated that 18% of subjects in the normal group, 15% in the obese group, 13% in the sarcopenia group, and 12% in the sarcopenic obesity group exhibited dysphagia based on the J-EAT-10 (p = 0.95) (Fig. 2b). The prevalence of anorexia was 47% in the normal group, 38% in the obese group, 52% in the sarcopenia group, and 41% in the sarcopenic obesity group, as assessed by SNAQ (p = 0.83) (Fig. 2c). Figure 3 shows the prevalence of frailty and PEW. Our findings demonstrated that 18% of subjects in the normal group, 33% in the obese group, 34% in the sarcopenia group, and 43% in the sarcopenic obesity group exhibited frailty based on the Kihon Checklist (p < 0.05). In addition, the prevalence of PEW was 20% in the normal group, 5% in the obese group, 31% in the sarcopenia group, and 18% in the sarcopenic obesity group, as assessed by ISRNM simplified criteria.
In the univariate analysis, the sarcopenia group had a significantly higher risk of PEW (OR 7.000, 95% CI 2.049–15.912, p = 0.002) than the normal group. In the multivariate analysis, the sarcopenia group also had a significantly higher risk of PEW (OR 4.272, 95% CI 1.157–15.778, p = 0.029) after adjusting for age, gender, and diabetes mellitus(Fig. 4). On the other hand, the sarcopenia group and the sarcopenic obesity group had a significantly greater risk of frailty than the normal group in the univariate analysis (OR 4.105, 95% CI 1.422–11.851, p = 0.009) and (OR 5.571, 95% CI 1.636–18.968, p = 0.006). However, only sarcopenic obesity had a significantly higher risk of frailty than the normal group in the multivariate analysis after adjusting for age, gender, and diabetes mellitus (OR 4.518, 95% CI 1.218–16.752, p = 0.024) (Fig. 4).
Discussion
We found that sarcopenic obesity was associated with reduced muscle strength and physical performance and with a greater risk of frailty than was the normal condition in HD patients. On the other hand, sarcopenic obesity was not associated with a higher likelihood of PEW, though the sarcopenia group showed a higher risk of PEW than the normal group.
Sarcopenia is well known as one of the key components of physical frailty or PEW in HD patients [23]. Assessment of sarcopenia is currently defined as generalized loss of skeletal muscle mass combined with reduced strength or physical performance [6]. However, almost all prior studies considering sarcopenia defined it by only low muscle mass in HD patients [24]. In the present study, sarcopenia was defined by AWGS criteria, including the presence of decreased muscle mass and reduced muscle strength or physical performance. We found that both muscle wasting (75%) and sarcopenia (44%) defined by the AWGS criteria resulted in a higher prevalence than that reported in prior research in HD patients according to different diagnosis criteria [25]. Several factors may explain the higher prevalence of muscle wasting or sarcopenia, including a different cutoff for defining low muscle mass between studies as well as different methodologies, diagnostic definitions, and clinical characteristics of the study populations. In this study, the prevalence of sarcopenic obesity was 15% as assessed with the AWGS criteria and %fat mass (women < 40%, men < 30%). The prevalence of sarcopenic obesity in this study was slightly lower than that in prior studies of patients with HD, which varied from 12 to 62% for men and 2 to 74% for women according to the different definition [5]. However, few comparative studies have shown the prevalence of sarcopenic obesity in Asians. The prevalence of obesity in patients with type 2 diabetes mellitus or HD, defined as % fat mass or body mass index ≧ 30 kg/m2, is low in most Asian countries compared with that in Western countries [26, 27].
Although the gait speed and chair stand test were not significantly different among four groups, these values of the current study were lower than those in age-adjusted community-dwelling Japanese older adults [28]. On the other hand, handgrip strength in sarcopenia and sarcopenic obesity group were significantly lower than those in normal or obesity group. Our findings are similar to a previous report that muscle mass loss was more associated with reduced muscle strength than impaired physical performance [29]. Moreover, muscle strength (both handgrip strength and leg strength) was positively associated with the ability to maintain standing balance in elderly population [30]. These results indicated that reduced muscle strength and/or impaired balance function may contribute to lower SPPB score in sarcopenia and sarcopenic obesity group.
Only a few prior clinical studies have assessed the relationship between body composition and PEW in maintenance dialysis patients [31]. The prevalence of PEW in underweight patients characterized by low muscle mass was significantly higher than that in obese patients. In this study, 20% of the normal group, 5% of the obese group, 31% of the sarcopenia group, and 18% of the sarcopenic obesity group had PEW according to the ISRNM simplified criteria; sarcopenic obesity was not associated with a higher likelihood of PEW. The concept of PEW is discriminated from malnutrition associated with inadequate nutritional intake caused by anorexia, swallowing function, or dietary restrictions. Because CKD or HD treatment-related uremic toxins, hypercatabolic status, and hyperinflammatory status also contribute to the development of PEW [32]. The present study demonstrated that despite the variation in malnutrition-associated factors, there were no significant difference of nPCR, SNAQ, or EAT-10 between sarcopenia and sarcopenic obesity group. These results suggest that higher risk of PEW in sarcopenia group may be explained by its links with CKD or HD treatment-related uremic toxins, hypercatabolic status, and hyperinflammatory status. Hence, sarcopenia group may progress into the kidney disease cachexia stage, which is conceptual framework proposed as a continuum with PEW first followed by cachexia [33]. Thus, we recognize that the evaluation of sarcopenia or sarcopenic obesity is useful in clinical practice, especially in planning effective interventions. Our results suggested that sarcopenic obesity patients were necessary to improve muscle strength, and get out of a physical frailty cycle. On the other hand, it is reported that the concurrence of sarcopenia and obesity were closely associated with metabolic impairments, increased CVD risk, and physical disability [34, 35]. Increasing fat mass leads to secrete adipocytokines that further promote insulin resistance as well as confer potentially direct catabolic effects on muscle. Thus, these vicious cycles between muscle loss and fat gain lead to more sarcopenia, and fat accumulation, increased risk of CVD, and physical disability [36]. The disadvantage of long-term effects of obesity or high amount of adipose tissue on future incidence of CVD may be overwhelmed by the short-term effects of underweight or sarcopenia. From the view point, it is important to improve muscle mass, muscle strength, and physical performance in both sarcopenia and sarcopenic obesity group. Although several evidences demonstrated the benefit of exercise or regular physical activity intervention for sarcopenia; however, there was very little evidence against the patients with sarcopenic obesity [37]. Sarcopenic obesity is often difficult to prescribed effective exercise training or regular physical activity by impairments physical function and physical performance or increased arthralgia of weight-bearing joints [38]. There is a need to develop new strategies to promote sustainable exercise training or regular physical activity intervention for sarcopenic obesity.
Limitations
Several limitations of our present study should be noted. First, our findings are limited to a relatively small number of patients at a single dialysis center and thus may not have enough statistical power. However, most of the results are comparable to those from prior clinical studies. Second, we defined PEW according to ISRNM simplified criteria consisting of the following four categories: lower BMI (< 23 kg/m2), sCr/BSA, Alb, and nPNA. Therefore, most of the sarcopenic obesity patients did not meet the BMI criteria, which might have led to a lower prevalence of PEW in the sarcopenic obesity patients. Third, skeletal muscle mass and fat mass were evaluated by BIA after a midweek dialysis session. These estimated skeletal muscle mass or fat mass measurements can be affected by fluid status or hydration status. However, most patients received optimal fluid management and completed the appropriate dialysis sessions. Fourth, it has become apparent in recent studies that PEW can be induced by inflammatory processes in hemodialysis patients. However, the present study unfortunately could not assess the specific inflammatory markers such as tumor necrosis factor α (TNF-α) and interleukin 6 (interleukin-6). It remains unclear whether inflammatory status in hemodialysis patients with sarcopenic obesity; further studies are therefore needed to assess this result.
Conclusion
Sarcopenic obesity was closely associated with frailty compared with the normal condition in HD patients. However, sarcopenic obesity was not associated with a higher likelihood of PEW.
Availability of data and materials
Not applicable.
Abbreviations
- ANOVA:
-
Analysis of variance
- ASM:
-
Appendicular skeletal muscle mass
- AWGS:
-
Asia Working Group for Sarcopenia
- BIA:
-
Bioimpedance electrical analysis
- CI:
-
Confidence intervals
- EWGSOP:
-
European Working Group on Sarcopenia in Older People
- GLIM:
-
Global Leadership Initiative on Malnutrition
- HD:
-
Hemodialysis
- ISRNM:
-
International Society of Renal Nutrition and Metabolism
- J-EAT-10:
-
Japanese version of EAT-10
- MNA-SF:
-
Mini Nutritional Assessment short form
- nPNA:
-
Normalized protein nitrogen appearance
- OR:
-
Odds ratios
- PWE:
-
Protein-energy wasting
- sCr/BSA:
-
Serum creatinine normalized by the body surface area
- SMI:
-
Skeletal muscle mass index
- SNAQ:
-
Simplified Nutritional Appetite Questionnaire
- SPPB:
-
Short physical performance battery
References
Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol. 2009;53:1925–32.
Kalantar-Zadeh K, Kopple JD. Obesity paradox in patients on maintenance dialysis. Contrib Nephrol. 2006;151:57–69.
Kittiskulnam P, Carrero JJ, Chertow GM, Kaysen GA, Delgado C, Johansen KL. Sarcopenia among patients receiving hemodialysis: weighing the evidence. J Cachexia Sarcopenia Muscle. 2017;8(1):57–68.
Prado CM, Wells JC, Smith SR, Stephan BC, Siervo M. Sarcopenic obesity: A Critical appraisal of the current evidence. Clin Nutr. 2012;31:583–601.
Malhotra R, Deger SM, Salat H, Bian A, Stewart TG, Booker C, et al. Sarcopenic obesity definitions by body composition and mortality in the hemodialysis patients. J Ren Nutr. 2017;27(2):84–90.
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15:95–101.
Dufour AB, Hannan MT, Murabito JM, Kiel DP, McLean RR. Sarcopenia definitions considering body size and fat mass are associated with mobility limitations: the Framingham Study. J Gerontol A Biol Sci Med Sci. 2013;68(2):168–74.
Cederholm T, Jensen GL, Correia MITD, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition—a consensus report from the global clinical nutrition community. Clin Nutr. 2019;38(1):1–9.
Wilson MM, Thomas DR, Rubenstein LZ, Chibnall JT, Anderson S, Baxi A, et al. Appetite assessment: simple appetite questionnaire predicts weight loss in community-dwelling adults and nursing home residents. Am J Clin Nutr. 2005;82(5):1074–81.
Nemoto M, Yabushita N, Kim M, Matsuo T, Seino S, Tanaka K. Assessment of vulnerable older adult’s physical function according to the Japanese Long-Term Care Insurance (LTCI) system and Fried’s criteria for frailty syndrome. Arch Gerontol Geriatr. 2012;55:385–91.
Fouque D, Kalantar-Zadeh K, Kopple J, Cano N, Chauveau P, Cuppari L, et al. A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int. 2008;73:391–8.
Bosy-Westphal A, Schautz B, Later W, Kehayias JJ, Gallagher D, Müller MJ. What makes a BIA equation unique? Validity of eight-electrode multifrequency BIA to estimate body composition in a healthy adult population. Eur J Clin Nutr. 2013;67(Suppl 1):S14–21.
Bosy-Westphal A, Jensen B, Braun W, Pourhassan M, Gallagher D, Müller MJ. Quantification of whole-body and segmental skeletal muscle mass using phase-sensitive 8- electrode medical bioelectrical impedance devices. Eur J Clin Nutr. 2017;71(9):1061–7.
Jensen B, Moritoyo T, Kaufer-Horwitz M, Peine S, Norman K, Maisch M, et al. Ethnic differences in fat and muscle mass and their implication for interpretation of bioelectrical impedance vector analysis. Appl Physiol Nutr Metab. 2018. https://doi.org/10.1139/apnm-2018-0276.
Fess EE. The effects of Jamar dynamometer handle position and test protocol on normal grip strength. J Hand Surg. 1981;7:308–9.
Guralnik JM, Simonsick EM, Ferrucci L. A short physical performance battery assessing lower extremity function: as- sociation with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94.
Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, et al. Validity and reliability of the Eating Assessment Tool (EAT-10). The Annals of otology, rhinology, and laryngology. 2008;117(12):919–24.
Wakabayashi H, Kayashita J. Translation, reliability, and validity of the Japanese version of the 10-item Eating Assessment Tool (EAT-10) for the screening of dysphagia. JJSPEN. 2014;29(3):871–6 Japanese.
Hasselmann M, Alix E. Tools and procedures for screening for malnutrition and its associated in risks in hospital. Nutr Clin Metabol. 2003;17:218–26.
Nakatsu N, Sawa R, Misu S, Ueda Y, Ono R. Reliability and validity of the Japanese version of the simplified nutritional appetite questionnaire in community-dwelling older adults. Geriatr Gerontol Int. 2015;15(12):1264–9.
Rolland Y, Perrin A, Gardette V, Filhol N, Vellas B. Screening older people at risk of malnutrition or malnourished using the Simplified Nutritional Appetite Questionnaire (SNAQ): a comparison with the Mini-Nutritional Assessment (MNA) tool. J Am Med Dir Assoc. 2012;13(1):31–4.
Saitoh M, Ogawa M, Dos Santos MR, Kondo H, Suga K, Itoh H, et al. Effects of intradialytic resistance exercise on protein energy wasting, physical performance and physical activity in ambulatory patients on dialysis: a single-center preliminary study in a Japanese Dialysis Facility. Ther Apher Dial. 2016;20(6):632–8.
Kim JC, Kalantar-Zadeh K, Kopple JD. Frailty and protein-energy wasting in elderly patients with end stage kidney disease. J Am Soc Nephrol. 2013;24(3):337–51.
Johansen KL, Lee C. Body composition in chronic kidney disease. Curr Opin Nephrol Hypertens. 2015;24(3):268–75.
Bataille S, Serveaux M, Carreno E, Pedinielli N, Darmon P, Robert A. The diagnosis of sarcopenia is mainly driven by muscle mass in hemodialysis patients. Clin Nutr. 2017;36(6):1654–60.
Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368:1681–8.
Park J, Jin DC, Molnar MZ, Dukkipati R, Kim YL, Jing J, et al. Mortality predictability of body size and muscle mass surrogates in Asian vs white and African American hemodialysis patients. Mayo Clin Proc. 2013;88(5):479–86.
Makizako H, Shimada H, Doi T, Tsutsumimoto K, Lee S, Harada K, et al. Age-dependent changes in physical performance and body composition in community-dwelling Japanese older adults. J Cachexia Sarcoepnia Muscle. 2017;8(4):607–14.
Cawthon PM, Peters KW, Shardell MD, McLean RR, Dam TT, Kenny AM, et al. Cutpoints for low appendicular lean mass that identify older adults with clinically significant weakness. J Gerontol A Biol Sci Med Sci. 2014;69:567–75.
Bijlsma AY, Pasma JH, Lambers D, Stijintjes M, Blauw GJ, Meskers CG, et al. Muscle strength rather than muscle mass is associated with standing balance in elderly outpatients. J Am Med Assoc. 2013;14(7):493–8.
Honda H, Qureshi AR, Axelsson J, Heimburger O, Suliman ME, Barany P, et al. Obese sarcopenia in patients with end-stage renal disease is associated with inflammation and increased mortality. Am J Clin Nutr. 2007;86:633–8.
Wang XH, Mitch WE. Mechanisms of muscle wasting in chronic kidney disease. Nat Rev Nephrol. 2014;10(9):504–16.
Koppe L, Fouque D, Kalantar-Zadeh K. Kidney cachexia or protein-energy wasting in chronic kidney disease: facts and numbers. J Cachexia Sarcopenia Muscle. 2019;10(3):479–84.
Kim JH, Cho JJ, Park YS. Relationship between sarcopenic obesity and cardiovascular disease risk as estimated by the Framingham risk score. J Korean Med Sci. 2015;30(3):264–71.
Nilsson MI, Dobson JP, Greene NP, Wiggs MP, Shimkus KL, Wudeck EV, et al. Abnormal protein turnover and anabolic resistance to exercise in sarcopenic obesity. FASEB J. 2013;27(10):3905–16.
Anton SD, Karabetian C, Naugle K, Buford TW. Obesity and diabetes as accelerators of functional decline: Can lifestyle interventions maintain functional status in high risk older adults? Exp Gerontol. 2013;48(9):888–97.
Goisser S, Kemmler W, Porzel S, Volkert D, Sieber CC, Bollheimer LC, et al. Sarcopenic obesity and complex interventions with nutrition and exercise in community-dwelling older persons: A narrative review. Clin Interv Aging. 2015;10:1267–82.
Vasconcelos KS, Dias J, Araújo MC, Pinheiro AC, Moreira BS, Dias RC. Effects of a progressive resistance exercise program with high-speed component on the physical function of older women with sarcopenic obesity: A randomized controlled trial. Brazilian Journal of Physical Therapy. 2016;20(5):432–40.
Acknowledgments
The authors wish to thank the doctors, nurses, and clinical engineers who engaged in the treatment of our patients in Meiseikai Toyo Clinic Yachimata.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SM provided the research design, data measurements and analysis, and wrote the manuscript. OM and KH provided the data collection and measurements. SK, IH, and TY participated in the research design and substantially contributed to the study concept. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent was obtained from all patients, and this study protocol was conducted in accordance with the Principles of the Declaration of Helsinki and the Declaration of Istanbul, and was approved by the institutional review boards at the Meisei-kai Toyo clinic, Chiba, Japan.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Saitoh, M., Ogawa, M., Kondo, H. et al. Sarcopenic obesity and its association with frailty and protein-energy wasting in hemodialysis patients: preliminary data from a single center in Japan. Ren Replace Ther 5, 46 (2019). https://doi.org/10.1186/s41100-019-0240-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41100-019-0240-9