Abstract
Background
High dietary intake of antioxidants reduces the risk of allergic sensitization in children. However, there was no sufficient evidence for the effect of dietary antioxidants intake on childhood eczema. Herein, this study aimed to explore the roles of different dietary antioxidants in childhood eczema.
Methods
Data of 2305 children and adolescents aged < 18 years old were extracted from the National Health and Nutrition Examination Survey database in 2005–2006 in this cross-sectional study. The associations between dietary antioxidants intake and childhood eczema were explored using univariate and multivariate logistic regression analyses, with odds ratios (ORs) and confidence intervals (CIs). Subgroup analyses based on age and gender were also performed.
Results
A total of 268 (11.6%) children had eczema. After adjusting for covariates, we found no significant associations between dietary intake of β-carotene, vitamin C, selenium (Se), and retinol and childhood eczema. However, compared with children and adolescents whose dietary zinc (Zn) intake < 7.47 mg, those who had dietary Zn intake level ≥ 11.83 mg seemed to have lower odds of eczema [OR 0.45, 95% CI 0.28–0.73]. In addition, subgroup analysis showed that especially in children and adolescents aged 1–11 years old, whatever the gender, a higher dietary intake level of Zn may benefit childhood eczema (all P < 0.05).
Conclusion
We concluded dietary Zn intake was negatively associated with childhood eczema. Further studies are needed to explore the roles of dietary antioxidants intake in childhood eczema.
Similar content being viewed by others
Background
Eczema is a chronic relapsing skin inflammatory disease characterized by defective skin barrier function [1]. The global prevalence of childhood eczema is around 20.0% [2]. The early eczema-related comorbidities increase the risk of future persistent multimorbidity [3]. Results of previous longitudinal birth cohort studies indicated that eczema in early life was associated with up to sevenfold increased risks of asthma and allergy in later life, compared with the never eczema phenotype [4, 5]. Therefore, identification of factors affecting early eczema development is vital to reduce the prevalence of eczema and the overall disease burden.
Eczema as a disease of immunological interest is linked to changes in nutrition along with general environmental changes, especially during a critical period of life [6]. Oxidative stress (OS) is one of the most important factors in eczema pathophysiology. OS is the result of reactive oxygen species (ROS) overproduction or of inadequate antioxidant defense mechanisms, leading to disruption of the oxidant–antioxidant balance toward the oxidants [7]. OS can disrupt barrier function, enhance proinflammatory cytokine production and activate naive T cells and cellular dermal infiltration, and consequently aggravate eczema lesions [8, 9]. Dietary antioxidants, such as vitamin C, β-carotene, vitamin E, selenium (Se), zinc (Zn), and retinol, take part in redox reactions and act by scavenging reactive oxygen-free radicals in order to remit inflammation [10, 11]. A diet low in antioxidants may increase susceptibility to oxidant injury and inflammation [12]. A previous study has reported that increased dietary intakes of Zn was associated with a low risk of atopic eczema (AE) in children [6]. Patel et al. [13] also showed that in children aged 5–8 years old, increased dietary intake of β-carotene was related to a decreased risk of allergic sensitization and serum IgE levels.
Recent studies have not shown sufficient evidences for the effect of dietary intake of Zn, β-carotene and other dietary antioxidants on the risk of childhood eczema. Herein, this study aims to explore the associations between different dietary antioxidants intake and childhood eczema.
Methods
Study design and population
Data of participants in this cross-sectional study were extracted from the National Health and Nutrition Examination Survey (NHANES) in 2005–2006. NHANES is a representative survey research program to assess the health and nutritional status of American adults and children. Regular data collection of approximately 5,000 persons is carried out from 15 areas since 1999 and examines in two-year periods. NHANES 2005–2006 is the only cycle with complete questionnaires on eczema. More details of statistical data can be found on the NHANES website [14].
A total of 4,785 children and adolescents (aged < 18 years old) in the NHANES were initially included. The exclusion criteria were (1) missing information of dietary intake of vitamin E, β-carotene, vitamin C, Zn, Se or retinol, and (2) children having an answer of ‘refused,’ ‘don’t know’ or ‘missing’ for the eczema questionnaire. Finally, 2,305 of them were eligible. The NHANES survey is approved by the institutional review board (IRB) of the National Center for Health Statistics (NCHS). The participants’ legal guardians/next of kin have provided written informed consent for participation. Since all the data were de-identified and publicly available, no ethical approval of this study by the IRB of Children’s Hospital Affiliated to Capital Institute of Pediatrics was required. In addition, all study methods were carried out in accordance with relevant guidelines and regulations (declaration of Helsinki).
Measurement of dietary antioxidants intake
In NHANES, dietary antioxidants intake was collected via two 24-h dietary recalls, in which participants reported individual foods and drinks consumed during the midnight-to-midnight 24-h period prior to the in-person dietary interview. Participants under the age of 16 years old were interviewed by a proxy interviewee (typically their parents). The first dietary recall interview is collected in-person in the Mobile Examination Center (MEC), and the second interview is collected by telephone 3 to 10 days later. NHANES conducted the coding of interview data and conversion to total nutrient intakes by using the United States Department of Agriculture (USDA) Food and Nutrient Database for Dietary Studies, 5.0 (FNDDS 5.0) [15].
Data of dietary antioxidants intake including vitamin E, β-carotene, vitamin C, Zn, Se and retinol were extracted in this study. We divided the antioxidants consumption into three levels respectively according to their own quantiles: vitamin E (< 3.82, 3.82 ≤ vitamin E < 6.28, and ≥ 6.28 mg), β-carotene (< 230, 230 ≤ β-carotene < 613, and ≥ 613 mcg), vitamin C (< 35.5, 35.5 ≤ vitamin C < 96.1, and ≥ 96.1 mg), Zn (< 7.47, 7.47 ≤ Zn < 11.83, and ≥ 11.83 mg), Se (< 68.8, 68.8 ≤ Se < 104.4, and ≥ 104.4 mcg) and retinol (< 253, 253 ≤ retinol < 500, and ≥ 500 mcg).
Diagnosis of eczema
The diagnosis of childhood eczema was according to the self-reported NHANES questionnaire. Respondents for the interviews included the following: a proxy for child aged < 6 years old; a proxy with the assistance of the child for those aged 6–8 years old; assistance of a proxy for child aged 9–11 years old; and children aged ≥ 12 years old who answered by themselves. Children and adolescents who had self-reported symptoms (an itchy rash, which was intermittently coming and going) in the last 12 months or a positive answer to the question “Has a doctor or other health professional ever told you that you have eczema?” were recognized as childhood eczema [16].
Covariates selection
We collected variables from the NHANES database including age, gender, race, family educational background, poverty-to-income ratio (PIR), exposure to environmental tobacco smoke, insurance, maternal age, asthma, hay fever, food allergy, peanut allergy, egg allergy, milk allergy, shrimp allergy, height, weight, body mass index (BMI), cotinine, C-reactive protein (CRP), vitamin D, energy intake, polyunsaturated fatty acids (PUFA) intake, and serum immunoglobulin E (IgE) level.
The diagnoses of asthma and hay fever were both according to the NHANES questionnaires similar to that of the eczema. A positive response to both questions: “Has a doctor or other health professional ever told you that you have asthma?” and “In the past 12 months (have you/he/she) had wheezing or whistling in (your/his/her) chest?” were used to recognize asthma. Hay fever (itchy, runny, or blocked nose without a cold accompanied by red itchy eyes) was diagnosed according to the positive response for the question: “Have you had hay fever in the past 12 months?” [17]. The sensitization to common food allergens in the USA, including peanut allergy, egg allergy, milk allergy, and shrimp allergy, was assessed using serum concentrations of allergen specific IgE according to a previous study [18]. Serum samples were collected for the analyses by the Pharmacia Diagnostics Immuno CAP 1000 System (Pharmacia Diagnostics, Kalamazoo, MI, USA) [19].
Statistical analyses
Normal distribution data were expressed as mean ± standard deviation (Mean ± SD), and t test was used for comparison between groups. Skewed distribution data were expressed as median and quartiles [M (Q1, Q3)], and used rank sum test for comparison. Categorical data were expressed as frequency and constituent ratio [N (%)], and chi-square test (χ2) was used for comparison.
Univariate logistic regression analysis was used for covariates screening. Univariate and multivariate logistic regression analyses were used to explore the association between dietary antioxidants intake and childhood eczema. Model 1 was the crude model. Model 2 adjusted for age, gender, race, family educational background, PIR, insurance, asthma, hay fever, food allergy, BMI, energy intake, PUFA intake and serum IgE level. Model 3 adjusted for variables included in the Model 2 and different dietary antioxidants. Subgroup analyses of age and gender were also performed.
The evaluation index was odds ratios (ORs) with 95% confidence intervals (CIs). Two-sided P < 0.05 was considered significant. To eliminate differences results from dimension, we normalized the data [with the formula: (x-mean)/standard deviation], and the normalization can magnify the influencing of these variables on the outcome to make it more direct. Statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA). Missing data were deleted (accounting for more than 20%) or interpolated using the multiple interpolation method (accounting for ≤ 20%). The sensitive analysis of characteristics of participants before and after interpolation of missing variables is shown in Additional file 1: Table S2.
Results
Characteristics of eligible children
There are 4,785 children and adolescents aged < 18 years old in the NHANES database in 2005–2006. Those who without information of eczema (n = 536), Zn intake (n = 816), serum IgE level (n = 571), cotinine (n = 454), family educational background (n = 84), exposure to environmental tobacco smoke (n = 8), insurance (n = 9), and hay fever (n = 3) were excluded. Finally, 2,304 of them were eligible.
Table 1 showed the characteristics of participants in non-eczema group and eczema group. Among the eligible children and adolescents, 268 (11.6%) children had eczema. The average age of the study population was 12 years old, and there were 1175 (51.0%) females. Among total population, 384 (16.7%) had asthma, 86 (3.7%) had hay fever, and 593 (25.7%) had food allergy. The median dietary intakes of Zn (9.62 mg vs. 8.49 mg) and Se (87.75 mcg vs. 79.80 mcg) were significantly different between non-eczema group and eczema group. In addition, race, family educational background, PIR, insurance, peanut allergy, egg allergy, height, weight, BMI, and serum IgE level were all different between these two groups (all P < 0.05).
Association between dietary antioxidants intake and childhood eczema
We first screened the covariates associated with childhood eczema (Additional file 1: Table S1). The results showed that age, race, family educational background, PIR, insurance, asthma, hay fever, food allergy, BMI, and serum IgE level were associated with childhood eczema (all P < 0.05). In addition, gender, energy intake, and PUFA intake have all been reported to be associated with allergic diseases, so that they were all included in the adjusted models [20,21,22].
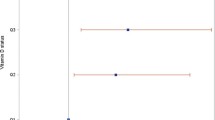
Then we explored the relationship between different antioxidants intake and childhood eczema (Table 2). After adjusting for the above covariates, we found no significant association of dietary intakes of β-carotene, vitamin C, Se, and retinol with eczema (P > 0.05). Dietary intakes of vitamin E [OR 0.95, 95% CI 0.90–0.99] and Zn [OR 0.96, 95% CI 0.93–0.99] were both negatively associated with eczema. However, when further adjusted for these antioxidants to each other, we only found the negative relationship between dietary Zn intake and eczema [OR 0.96, 95% CI 0.93–0.99]. Compared with children and adolescents whose dietary intake of Zn < 7.47 mg, those who had dietary Zn intake level ≥ 11.83 mg seemed to have lower odds of eczema [OR 0.45, 95% CI 0.28–0.73].
Relationships between antioxidants and childhood eczema in age and gender subgroups
We further explored these associations in age (Table 3) and gender subgroups. In children aged 1–5 years old, dietary Zn intake was negatively associated with eczema [OR 0.87, 95% CI 0.76–0.98], while that of β-carotene [OR 1.01, 95% CI 1.01–1.01] and retinol [OR 1.01, 95% CI 1.01–1.01] were both positively associated with eczema. Among children aged 1–11 years old, dietary Zn intake level ≥ 7.47 mg was significantly associated with lower odds of eczema, compared with dietary Zn intake level < 7.47 mg (all P < 0.05). Besides, compared with dietary Zn intake level < 7.47 mg, that ≥ 11.83 mg was linked to lower odds of eczema in both male [OR 0.51, 95% CI 0.26–0.99] and female [OR 0.41, 95% CI 0.21–0.82] children and adolescents.
Discussion
This study explored the relationships between different dietary antioxidants intake and childhood eczema. Our results showed that higher dietary intake of Zn was associated with lower odds of childhood eczema, and this relationship was also found in children aged 1–11 years old regardless of gender.
The essential micronutrients Zn and Se have complex influences on human immune system and are associated with allergic diseases such as asthma, rhinitis, and atopic dermatitis [23]. A follow-up study from birth to 4 years showed that an increased intake of Zn, with perinatal administration of probiotics, reduced the risk of AE [6]. Topic et al. [24] found that increased Zn- superoxide dismutase (SOD) was associated with eczema in asthmatic children. Another study showed a deficiency of serum Zn (52.0%) and Cu (33.0%) in atopic children characterized by eczema, stomatitis, relapsing herpes, and neurosis [25]. Amin et al. [26] suggested that malonaldehyde (MDA) significantly raised and antioxidants level decreased may be possible causative factors for the pathogenesis of eczema. Similarly, in the current study, the results indicated that higher dietary intake of Zn was associated with lower odds of childhood eczema, and however, we have not found the relationship between dietary Se intake and eczema. Zn is primarily found in animal products and seafood, such as milk and dairy products, meat and meat products [27]. Low fish consumption could explain the insufficient intake of Zn [28]. Also, Zn is a vital nutrient for skin health, which involved in many skin functions, such as the regeneration of skin cells, activation of skin hormone, and control of skin inflammation [29]. In our body, several Zn bound proteins depends on the concentration of Zn for exhibiting their biological activities [30]. Nevertheless, there were some inconsistent results as well on the associations between dietary intake of antioxidant vitamins and minerals and allergic diseases, which discrepancies may be explained by the different roles of nutrients depending on the end-organ manifestation [31, 32]. Therefore, potential mechanisms of dietary Zn intake affecting the childhood eczema needed further exploration.
In subgroup analyses, the association between dietary intake of Zn and childhood eczema was also found in children who aged 1–11 years old. Zn deficiency is highly prevalent in young children (from 6 months to 12 years old) since during periods of rapid growth, they have increased requirements of Zn, which lead to an increased risk of developing Zn deficiency [33]. Similarly, our results supported this opinion, indicating that higher dietary Zn intake may have a potential beneficial effect on eczema in children aged less than 11 years old, which possibly because children during rapid growth may be more sensitive to inflammatory skin disease related to Zn deficiency such as eczema. Besides, with the dietary intake of β-carotene and retinol elevated, the odds of childhood eczema were increased in children aged 1–5 years old. In fact, whether the β-carotene and retinol play risk or preventive roles in allergic disorders is uncertain. A cross-sectional analysis showed no significant difference in activity of retinol in Children with asthma compared with controls [34]. Patel et al. [13] suggested no association between antioxidant intakes and eczema in children aged 5–8 years old. Due to the lack of references on relationships between β-carotene and retinol and eczema in children of 1–5 year of age, our findings need further clarification. Simonsen et al. [35] found that the risk of hand eczema was significantly associated with female gender. Although gender difference has been reported to be related to allergic diseases in children [20], a study oppositely showed no difference between adolescents with different gender in the prevalence of eczema [36]. Results in the current study similarly manifested the relationship between higher dietary intake of Zn and lower odds of childhood eczema in children regardless of gender. Hormones significantly influence the pathogenesis of inflammatory diseases, such as asthma, rhinitis, and eczema [37]. Gender-related difference in asthma persistence may due to gender-related difference in susceptibility to oxidative stress, and the levels of 8-oxodG/creatinine was slightly higher in female gender [25]. However, the specific mechanisms of the gender difference between dietary antioxidants intake and childhood eczema needs further exploration.
The study population were from the NHANES database that were relatively representative for the population in the USA. We explored the association between different dietary antioxidants intake and childhood eczema, which may provide some information for future studies to clarify the roles of antioxidants on eczema, and thus may help to develop dietary prevention strategies for childhood eczema. However, there are some limitations in our study. Our study is an across-sectional study that was difficult to determine causal association and had inevitable biases. Information of dietary antioxidants intake was collected using the 24-h recalls of face-to-face interviews, which could only represent short-term dietary intake. Also, the prevalence of eczema may be underestimated by self-reported physician diagnoses. In addition, information of dietary antioxidants supplement, the family history of allergic diseases, vegetable and fruit allergy, antioxidants came from mother’s milk, and the subtype of eczema in the NHANES was not available. Therefore, further prospective cohort studies are warranted to explore the roles of different dietary antioxidants in childhood eczema in the future.
Conclusion
Zn consumption was negatively associated with childhood eczema, and the roles of dietary antioxidants in childhood eczema are still needed further exploration.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the NHANES database, https://wwwn.cdc.gov/nchs/nhanes/.
Abbreviations
- OS:
-
Oxidative stress
- ROS:
-
Reactive oxygen species
- Se:
-
Selenium
- Zn:
-
Zinc
- NHANES:
-
National Health and Nutrition Examination Survey
- MEC:
-
Mobile Examination Center
- PIR:
-
Poverty-to-income ratio
- BMI:
-
Body mass index
- CRP:
-
C-reactive protein
- IgE:
-
Immunoglobulin E
- PUFA:
-
Polyunsaturated fatty acids
- Mean ± SD:
-
Mean ± standard deviation
- ORs:
-
Odds ratios
- CIs:
-
Confidence intervals
References
Lopez DJ, Lodge CJ, Bui DS, Waidyatillake NT, Abramson MJ, Perret JL, et al. Establishing subclasses of childhood eczema, their risk factors and prognosis. Clin Exp Allergy. 2022;52:1079–90.
Stefanovic N, Flohr C, Irvine AD. The exposome in atopic dermatitis. Allergy. 2020;75:63–74.
Haider S, Fontanella S, Ullah A, Turner S, Simpson A, Roberts G, et al. Evolution of eczema, wheeze, and rhinitis from infancy to early adulthood: four birth cohort studies. Am J Respir Crit Care Med. 2022;206:950–60.
Paternoster L, Savenije OEM, Heron J, Evans DM, Vonk JM, Brunekreef B, et al. Identification of atopic dermatitis subgroups in children from 2 longitudinal birth cohorts. J Allergy Clin Immunol. 2018;141:964–71.
Roduit C, Frei R, Depner M, Karvonen AM, Renz H, Braun-Fahrlander C, et al. Phenotypes of atopic dermatitis depending on the timing of onset and progression in childhood. JAMA Pediatr. 2017;171:655–62.
Laitinen K, Kalliomaki M, Poussa T, Lagstrom H, Isolauri E. Evaluation of diet and growth in children with and without atopic eczema: follow-up study from birth to 4 years. Br J Nutr. 2005;94:565–74.
Uysal P, Avcil S, Neselioglu S, Bicer C, Catal F. Association of oxidative stress and dynamic thiol-disulphide homeostasis with atopic dermatitis severity and chronicity in children: a prospective study. Clin Exp Dermatol. 2018;43:124–30.
Wright RJ, Cohen RT, Cohen S. The impact of stress on the development and expression of atopy. Curr Opin Allergy Clin Immunol. 2005;5:23–9.
Pastore S, Korkina L. Redox imbalance in T cell-mediated skin diseases. Mediat Inflamm. 2010;2010:861949.
Rosenlund H, Magnusson J, Kull I, Hakansson N, Wolk A, Pershagen G, et al. Antioxidant intake and allergic disease in children. Clin Exp Allergy. 2012;42:1491–500.
Green MH, Ford JL, Green JB. Development of a compartmental model to investigate the influence of inflammation on predictions of vitamin A total body stores by retinol isotope dilution in theoretical humans. J Nutr. 2021;151(3):731–41.
Romieu I, Castro-Giner F, Kunzli N, Sunyer J. Air pollution, oxidative stress and dietary supplementation: a review. Eur Respir J. 2008;31:179–97.
Patel S, Murray CS, Woodcock A, Simpson A, Custovic A. Dietary antioxidant intake, allergic sensitization and allergic diseases in young children. Allergy. 2009;64:1766–72.
The NHANES database. https://wwwn.cdc.gov/nchs/nhanes/tutorials/module2.aspx.
The United States Department of Agriculture (USDA) Food and nutrient database for dietary studies. http://www.ars.usda.gov/ba/bhnrc/fsrg.
Wei J, Jaleel T, MacLeod AS, Ji JS. Inverted U-shaped relationship between vitamin D and ever-reported eczema in US adults. Allergy. 2019;74:964–75.
Odebeatu CC, Taylor T, Fleming LE, Jo N. Phthalates and asthma in children and adults: US NHANES 2007–2012. Environ Sci Pollut Res Int. 2019;26:28256–69.
Fu T, Keiser E, Linos E, Rotatori RM, Sainani K, Lingala B, et al. Eczema and sensitization to common allergens in the United States: a multiethnic, population-based study. Pediatr Dermatol. 2014;31(1):21–6.
The NHANES laboratory and quality control procedures. http://www.cdc.gov/nchs/data/nhanes/nhanes_05_06/al_ige_d.pdf.
Ying X, Qi X, Yin Y, Wang H, Zhang H, Jiang H, et al. Allergens sensitization among children with allergic diseases in Shanghai, China: age and sex difference. Respir Res. 2022;23(1):95.
Kong W, Xie Y, Zhong J, Cao C. Ultra-processed foods and allergic symptoms among children and adults in the United States: a population-based analysis of NHANES 2005–2006. Front Public Health. 2022;10:1038141.
Kremmyda LS, Vlachava M, Noakes PS, Diaper ND, Miles EA, Calder PC. Atopy risk in infants and children in relation to early exposure to fish, oily fish, or long-chain omega-3 fatty acids: a systematic review. Clin Rev Allergy Immunol. 2011;41(1):36–66.
Podlecka D, Jerzynska J, Sanad K, Polanska K, Bobrowska-Korzeniowska M, Stelmach I, et al. Micronutrients and the risk of allergic diseases in school children. Int J Environ Res Public Health. 2022;19:12187.
Topic A, Francuski D, Nikolic A, Milosevic K, Jovicic S, Markovic B, et al. The role of oxidative stress in the clinical manifestations of childhood asthma. Fetal Pediatr Pathol. 2017;36:294–303.
De Luca L, Vacca C, Pace E, Vuillemier PL, Del Vecchio L, Berni Canai R. Immunological and trace element study in 50 children with various diseases caused by food allergens and aeroallergens. Pediatr Med Chir. 1987;9:589–91.
Amin MN, Liza KF, Sarwar MS, Ahmed J, Adnan MT, Chowdhury MI, et al. Effect of lipid peroxidation, antioxidants, macro minerals and trace elements on eczema. Arch Dermatol Res. 2015;307:617–23.
Madrigal C, Soto-Méndez MJ, Hernández-Ruiz Á, Ruiz-López MD, Samaniego-Vaesken ML, Partearroyo T, et al. Dietary intake, nutritional adequacy, and food sources of selected antioxidant minerals and vitamins; and their relationship with personal and family factors in Spanish children aged 1 to <10 years: results from the EsNuPI study. Nutrients. 2022;14(19):4132.
Olza J, Aranceta-Bartrina J, González-Gross M, Ortega RM, Serra-Majem L, Varela-Moreiras G, et al. Reported dietary intake and food sources of zinc, selenium, and vitamins a, e and c in the Spanish population: findings from the ANIBES study. Nutrients. 2017;9:697.
Rostami Mogaddam M, Safavi Ardabili N, Maleki N, Soflaee M. Correlation between the severity and type of acne lesions with serum zinc levels in patients with acne vulgaris. Biomed Res Int. 2014;2014:474108.
Fukada T, Yamasaki S, Nishida K, Murakami M, Hirano T. Zinc homeostasis and signaling in health and diseases: Zinc signaling. J Biol Inorg Chem. 2011;16:1123–34.
Nagel G, Nieters A, Becker N, Linseisen J. The influence of the dietary intake of fatty acids and antioxidants on hay fever in adults. Allergy. 2003;58:1277–84.
Harik-Khan RI, Muller DC, Wise RA. Serum vitamin levels and the risk of asthma in children. Am J Epidemiol. 2004;159:351–7.
Mayo-Wilson E, Junior JA, Imdad A, Dean S, Chan XH, Chan ES, et al. Zinc supplementation for preventing mortality, morbidity, and growth failure in children aged 6 months to 12 years of age. Cochrane Database Syst Rev. 2014;5:CD009384.
Powell CV, Nash AA, Powers HJ, Primhak RA. Antioxidant status in asthma. Pediatr Pulmonol. 1994;18(1):34–8.
Simonsen AB, Ruge IF, Quaade AS, Johansen JD, Thyssen JP, Zachariae C. Increased occurrence of hand eczema in young children following the Danish hand hygiene recommendations during the COVID-19 pandemic. Contact Dermatitis. 2021;84:144–52.
Nafei Z, Behniafard N, Mirzaei M, Karimi M, Akbarian E. Prevalence of allergic rhinitis and eczema in adolescents living in Yazd City: part of global asthma network survey. Iran J Allergy Asthma Immunol. 2021;20:271–8.
Weare-Regales N, Chiarella SE, Cardet JC, Prakash YS, Lockey RF. Hormonal effects on asthma, rhinitis, and eczema. J Allergy Clin Immunol Pract. 2022;10:2066–73.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
JX designed the study and wrote the manuscript. HL collected, analyzed and interpreted the data. JX critically reviewed, edited and approved the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The requirement of ethical approval for this was waived by the Institutional Review Board of Children’s Hospital Affiliated to Capital Institute of Pediatrics, because the data was accessed from NHANES (a publicly available database). The need for written informed consent was waived by the Institutional Review Board of Children’s Hospital Affiliated to Capital Institute of Pediatrics due to retrospective nature of the study. All methods were carried out in accordance with relevant guidelines and regulations (declaration of Helsinki).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Covariates associated with childhood eczema. Table S2. Sensitivity analysis of characteristics before and after interpolation of missing data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, J., Li, H. Association between dietary antioxidants intake and childhood eczema: results from the NHANES database. J Health Popul Nutr 43, 12 (2024). https://doi.org/10.1186/s41043-024-00501-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41043-024-00501-x