Abstract
Background
Universal salt iodization was started before decades but there are communities using the un-iodized salt till now. More than one-tenth of the Ethiopian community uses un-iodized salt.
Objective
This study aimed to identify the hotspots and associate factors of un-iodized salt availability in Ethiopia based on Ethiopian national household survey data.
Methods
We conducted an in-depth analysis of the Ethiopian Demographic and Health Survey 2016 data. A total of 15,567 households were included in the final analysis. We cleaned and weighed the data using Stata version 16 software and descriptive outputs were reported in graphs and tables. We computed the weighted prevalence of un-iodized salt and prepared it for spatial analysis. Global-level spatial autocorrelation, hotspot analysis using the Getis-Ord Gi* statistics, and spatial interpolation using empirical Bayesian interpolation were executed using ArcGIS 10.3 to predict the magnitude of un-iodized salt at the national level. The binary logistics regression model was used to identify the contributing factors of un-iodized salt utilization. Model goodness of fit was tested with Hosmer and Lemeshow goodness-of-fit test (P = 0.96). Finally, the adjusted odds ratio (AOR) with 95% CI was reported to identify significant factors.
Results
The magnitude of un-iodized salt availability was 14.19% (95% CI: 13.65, 14.75) among Ethiopian households. Un-iodized salt hotspots were found in Afar, Somalia, and Benishangul Gumuz regions. Compared to poorest wealth index: poorer (AOR = 0.55, 95% CI: 0.48, 0.64), middle (AOR = 0.51, 95% CI: 0.44, 0.60), richer (AOR = 0.55, 95% CI: 0.47, 0.64), and richest (AOR = 0.61, 95% CI: 0.50, 0.75); compared to uneducated household head: heads with secondary (AOR = 0.72, 95% CI: 0.60, 0.67) and above secondary (AOR = 0.54, 95% CI: 0.43, 0.67) education reduced the odds of un-iodized salt viability, while households living in highland (AOR = 1.16, 95% CI: 1.05, 1.29) had increased the odds of un-iodized salt availability.
Conclusion
More than a tenth of the households in Ethiopia uses un-iodized salt. Hotspots of un-iodized salt availability were found in Somali and Afar regions of Ethiopia. Better wealth index and education of the household heads reduces the odds of un-iodized salt availability while living in a high altitude above 2200 m increases the odds of un-iodized salt availability in Ethiopia.
Similar content being viewed by others
Background
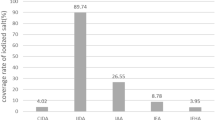
Iodine is one of the most deficient micronutrients and more than a quarter of the world population does not access adequate iodized salt [1]. Iodine deficiency is the most important cause of mental impairment that could be prevented by simple iodization and other public health interventions [2]. Ethiopia is one of the ten key salt-producing country in Sub-Saharan Africa [3]. Many African countries do not achieve at least 90% universal salt iodization and Ethiopia is the 3rd country with the highest rate of non-iodized salt availability in the households (HH) among sub-Saharan countries [4]. Different countries have a varied rate of iodized salt availability; 73.15% Bangladesh [5] and 69.8% in Saudi Arabia [6].The coverage of household iodized salt range from 6.2% in Niger to 97% Uganda among African regions [7] which is lower as compared to the global recommendation of > 90% of households must use iodized salt [8]. In Ethiopia, more than 10% of the households do not use iodized salt [4] nationally and 41.8% of households in Arbaminch town use inadequately iodized salt [1].
To a say a HH used a adequately iodized salt (the salt iodine content should > 15 ppm and < 40 ppm) and more than 90% of the population need to use this amount of iodized salt to declare as the iodized salt is available at the community [8]. Visible geographic variations of iodized salt availability in Bangladesh [5], Saudi Arabia [6], and other countries are observed. Other studies also pointed that the availability of iodized salt varies geographically across different countries [7]. Young and educated household head, poor and rural households significantly increase and decrease the household iodized salt availability in Bangladesh [5]. Different socioeconomic and household-level factors are associated with unavailability of iodized salt in different countries [1, 4, 5, 7, 9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24]. Age and level of education of household head, wealth index, place of residence, knowledge on iodized salt, marital status, family size, using packed salt [1, 4, 10, 11, 14, 25,26,27]. Evidenced from systematic review and meta-analysis, significant geographic variations of iodized salt availability were observed in Ethiopia with the highest in Addis Ababa to the lowest in Dire Dawa [1]. But these studies were not addressing the factors associated with the geographic variations.
Even though the iodized salt availability is low in Ethiopia, the spatial distribution and determinant factors were not identified. Hence, this study was aimed to assess the geographic variations and associated factors of un-iodized salt availability in Ethiopia using the Ethiopian Demographic and Health Survey (EDHS) 2016 data, which may help to achieve the universal salt iodization program by giving more emphasis on the identified hotspots of un-iodized salt availability in Ethiopia.
Methods
Study design and period we conducted an in-depth secondary data analysis of the Ethiopian demographic survey 2016. The EDHS 2016 was a nationwide cross-sectional study conducted from January to June, 2016 [28].
Study area Ethiopia is a second most populous country in Africa next to Nigeria with more than hundred million peoples living in nine regions and two administrative cities. Nutritional deficiencies like iodine are common public health problems and more than one-tenth of the households use un-iodized salt [28].
Data source and measurement we used the EDHS 2016 household data containing 16,650 households that has been accessed after being registered as an authorized user from the major demographic and health survey (http://www.dhsprogram.com). The households were selected using a stratified multistage sampling technic. The major Demographic and Health Survey (DHS) collects survey on health and health related indicators across different countries. The EDHS 2016 is the fourth major survey in Ethiopia that collected health and health related indicators including household-level un-iodized salt availability. The household questionnaire was used to collect the un-iodized salt availability at the household level. The detail of the data collection and sampling procedure are available elsewhere [28]. A total of 16,650 households from 645 enumeration areas were included for the household characteristics. We included 15,567 households’ data for the final analysis to identify the determinant factors of iodized salt availability (See Fig. 1).
For the spatial analysis, study participants from the clusters where the GPS data were zero (21 clusters) were excluded. Finally, we used 420 and 202 clusters from the rural and urban areas, respectively.
Study variables The dependent variable was un-iodized salt. Independent variables were socio-demographic variables such as age of the household head, marital status, education, occupation, age, religion, region of residence, and wealth index. Here are definitions of some composite variables.
Variable | Measurement |
|---|---|
Hotspots of un-iodized salt (hot spot/cold spot) | Was considered if the clusters had Z-score greater than 1.96 using the Getis-Ord Gi* statistics |
Un-iodized salt (Yes/no) | Was considered if the households salt Iodine shows negative |
Health facility access (good/poor) | Was computed based on the distance from the women’s data. Above the median of the community of distance a big problem to health facilities is considered as communities’ poor health facility access |
Altitude of residence (lowland/highland) | was defined below 2200 m above sea level as low land; 2200 m and above was considered as highland areas based on the median altitude of the community |
Community media exposure (poor/good) | Was computed from the internet or listening television or reading newspaper at least once per week. It was computed to the community level and a community had low media exposure if they got below the median. Low if below the median of the community uses media at least once per week. High if median and above of the cluster uses media at least once per week |
Other variables were directly used from the available data source and you can find them some elsewhere from the EDHS 2016 survey report [28].
Data analysis we accessed the data from the major DHS program; data cleaning, recoding, and weighting were conducted using Stata 16. The data were weighted using the household weighting variable (hv005) as per the recommendation of the major DHS program. We used Survey (svy) command for descriptive and analytical analysis. The detail of how to weigh the data found from the EDHS 2016 report Annex A [28]. The data were checked for missing values and codes before recoding the independent variables to maintain the integrity. For the spatial analysis, we computed the prevalence of un-iodized salt over the clusters and we used as an outcome variable. We tested the spatial autocorrelations using the global Moran’s index (I) by using an inverse distance with row standardization to balance the sampling errors among the enumeration areas (Clusters). Global Moran’s I is an autocorrelation coefficient with a value ranging from (− 1, 1) indicates the overall spatial clustering at the country level/general but cannot show where are these significant clusters found. If the value is close to − 1 this disease of interest/un-iodized salt utilization was spatially clustered while the reverse indicates spatial dispersion [2,3,4]. If the global Moran’s index was significant, further spatial analysis is required to identify local level significant clusters. The global Moran’s index was significant and we proceed the local level hotspot analysis using the Getis-Ord Gi* statistics. If the Getis-Ord Gi* statistics Z-score < − 1.96, between − 1.96–1.96 and above 1.96 implies significant cold spot (low risk), none significant and hotspot (high) risk clusters, respectively 5(5). As the data were based on the random samples taken, we estimate (predict) the magnitude of un-iodized salt using empirical Bayesian interpolation techniques.
For binary logistic regression to assess factors associated with un-iodized salt availability, Chi-square assumption was tested for each variable. Multi-collinearity was checked using standard errors and variance inflation factors. If standard error is > 2sd, the variance inflation factor greater than 10 multi-collinearity could be declared but no variable has this effect. The multilevel clustering effect was tested using the intra-class correlation coefficient and it was nearly zero (ICC = 0.00001). Hence, the hierarchical nature had no significant effect and we considered the binary logistics regression. The variables with p-value < 0.2 in the univariate analysis were considered for multivariate analysis. A p-value < 0.05 was used as a cutoff point to declare statistical significance and finally adjusted odds ratios (AOR) with 95% confidence interval (95% CI) was reported. The logistics regression model goodness of fit was tested using Hosmer and Lemeshow goodness-of-fit test and it produces a P-value of 0.96, and the model is adequately fit for the data.
Results
The magnitude of un-iodized salt availability was 14.19% (95% CI; 13.65, 14.75) among Ethiopian households. We found that Afar region was a region with lowest iodized salt users while Oromia region accounts more than a one-third of the iodized salt user of the population (see Table 1).
About 12,767 (81.1%) of the study participants were rural resident, 8703(54.6%) of the household heads had no education and 11,847 (74.33%) of the households found in highland (above 2200 m of sea level) areas of the country (see Table 2).
Spatial distribution of un-iodized salt among households
The distribution of un-iodized salt varies across regions. Enumeration areas with low availability (< 25% of HH with un-iodized salt) of un-iodized salt were found in Amhara, Tigray, most parts of Oromia, Addis Ababa, and Benishangul Gumuz, while clusters with high prevalence (> 75% of HH with un-iodized salt) of un-iodized salt were found in Afar and Somali regions (see Fig. 2).
We found a significant geographic variation of un-iodized salt availability among households of Ethiopia at national level with a global Moran’s’ Index (I = 0.31 with P-value < 0.001 and Z-score of 18.90), which shows that the distribution of un-iodized salt was spatially clustered at the national level and further local level test of spatial clustering was required (see Fig. 3).
The hotspot analysis pointed that majority of the clusters were not significant. Hotspot clusters were found in zones of Somali, Afar, and South Nations Nationalities and people’s regions (SNNPR) of the country (see Fig. 4).
We predict the magnitude of the un-iodized salt using empirical Bayesian interpolation techniques. Similar to the hotspot analysis, the prediction map shows most of the Afar and Somali regions with high prevalence of un-iodized salt which showed consistency of the predicted and existing magnitudes of un-iodized salt across different districts (See Fig. 5).
Associated factors of un-iodized salt among households
Among used variables, the wealth index, educational level of the household head, and altitude of residence were significantly associated with households’ un-iodized salt availability. Compared to households with poorest wealth index; the households having poorer [45% (AOR = 0.55, 95% CI: 0.48, 0.64)], middle [49% (AOR = 0.51, 95% CI: 0.44, 0.60)], richer [45% (AOR = 0.55, 95% CI: 0.47, 0.64)], and richest [39% (AOR = 0.61, 95% CI: 0.50, 0.75) times less odds of having un-iodized salt.
Considering the household heads level of Education, those who had a secondary and above secondary education had 28% (AOR = 0.72, 95% CI: 0.60, 0.67) and 46% (AOR = 0.54, 95% CI: 0.43, 0.67) less odds of having un-iodized salt as compared to uneducated household heads, respectively. Those households living in a community of above 2200 m altitude above sea level had 16% (AOR = 1.16, 95% CI: 1.05, 1.29) higher odds of having un-iodized salt compared to their counterpart (See Table 3).
Discussions
This study was undertaken to assess the spatial distribution and determinants of un-iodized salt availability among households of Ethiopian households. The overall availability of iodized salt in Ethiopia was low as compared to other countries elsewhere [2, 9, 12, 16, 19, 29,30,31,32,33,34,35] and the utilization of un-iodized salt remains high as public health problem. This may cause a number of iodine deficiency-related complications including Goiter and other cardiovascular problems.
Significant hotspots of un-iodized salt were found in most parts of Somali, Afar, and Benishangul Gumuz regions of Ethiopia. This finding was comparable with other systematic review and meta-analysis reports where the availability of un-iodized salt varies significantly across regions of Ethiopia [36]. Another study pointed that the existence of significant regional variations in access to iodized salt across 11 lower income countries [29]. The possible justifications for the spatial variations of un-iodized salt in Ethiopia might be different across regions; Afar and Somali regions were the places where most hotspots of un-iodized salt users found and this might be explained by the reasons given herewith. For Afar and Somali regions, there are places used for local and un-iodized salt extraction including the Afdera and Asale lacks and other lands in Somali [37, 38]. These local dwellers extract/produce un-iodized salts to other parts of the country. Evidences show that the transportation and iodization cost was high as compared to local produced salts and small (local) producers can compete with low price and none-iodized salt [3, 39]. These local small-scale producers have a challenged the salt trade in Sub-Saharan Africa and this might works true for afar region where a number of small producers extract none-iodized salt and sell with cheap price for local residents of the region [3, 40]. Even lack of commitment by the local salt producers to iodize, the harsh weather in Afdera, low productivity of the iodization machines challenges Ethiopia to have adequately iodized salt [41].
Having better wealth index reduces the households’ odds of un-iodized salt utilization as compared to these households with poorest wealth index. This evidence is supported by other studies conducted in Ethiopia [1, 14, 42, 43], Bangladesh [5], and Tanzania [13] where improved wealth index reduces the odds of households utilization of iodized salt. This might be due to accessibility and cost of the iodized salt is more acceptable by the wealthier than the poorest [3, 4, 7, 41]. As it is known, iodized salt is more expensive than un-iodized one due to the cost of transportation and iodization process and the poor may access locally produced un-iodized salts in low price [3, 41].
Compared to uneducated household heads, those with secondary and above secondary educations had 28 and 46% less odds of using un-iodized salt, respectively. These findings are supported by reports of studies conducted in Ethiopia different parts of Ethiopia [14, 25, 44], Sub-Saharan Africa [4], and Bangladesh [5]. This might be explained by those who are educated may have better knowledge about the benefits of salt iodization and risks of iodine deficiency disorders [45].
Considering the altitude of residence, we found that living in high land areas above 2200 m increases the odds of un-iodized salt availability and we could not find any study considering altitude as significant predictors of un-iodized salt. And this might be due to the fact that most of the highland areas are difficult to reach areas for different goods and services. Iodized salt transportation is one of the challenges of its utilization by different communities [3, 29].
Limitations we used a secondary data and we are not immune of the limitations of secondary data. The geographic distortions of the coordinate data for the security purpose may limit us to determine the specific locations accurately. Unavailability of behavioral factors, women cooking practices, and their knowledge and practice about iodized salt were missed to clearly interpret the utilization.
Conclusions and recommendations Household-level un-iodized salt availability was spatially clustered. The majority of significant hotspot clusters were found in Somali, Benishangul Gumuz, and Afar regions. Better wealth index and education of the household heads reduces the odds of un-iodized salt availability while living in a high altitude above 2200 m increases the odds of un-iodized salt availability in Ethiopia. Giving more emphasis on hotspot clusters and improving the household heads' education and wealth index might reduce the availability of un-iodized salt in Ethiopia.
Availability of data and materials
The data used for preparation of this manuscript are available from http://www.dhsprogram.comand anyone can access through online request as authorized user. The authors prepared the data that were used for preparation of this manuscript can be shared if required. The shape files of the maps were freely available without any restriction at Open Africa (https://africaopendata.org/dataset/ethiopia-sha.pefiles).
Abbreviations
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- EDHS:
-
Ethiopian Demographic and Health Survey
- EA:
-
Enumeration area
- HH:
-
Households
References
Ajema D, Bekele M, Yihune M, Tadesse H, Gebremichael G, Mengesha MM. Socio-demographic correlates of availability of adequate iodine in household salt: a community-based cross-sectional study. BMC Res Notes. 2020;13(1):125.
Voth M, Lustenberger T, Auner B, Frank J, Marzi I. What injuries should we expect in the emergency room? Injury. 2017;48(10):2119–24.
Mannar V, Yusufali R. Salt production and trade in Africa. IDD Newsletter. 2013;41:19–20.
Ba DM, Ssentongo P, Liao D, Du P, Kjerulff KH. Non-iodized salt consumption among women of reproductive age in sub-Saharan Africa: a population-based study. Public Health Nutr. 2020. https://doi.org/10.1017/S1368980019003616.
Khan JR, Biswas RK, Sheikh MT, Huq M. Factors associated with the availability of iodized salt at household level: a case study in Bangladesh. Public Health Nutr. 2019;22(10):1815–23.
Al-Dakheel MH, Haridi HK, Al-Bashir BM, Al-Shangiti AM, Al-Shehri SN, Hussein I. Assessment of household use of iodized salt and adequacy of salt iodization: a cross-sectional National Study in Saudi Arabia. Nutr J. 2018;17(1):35.
Knowles JM, Garrett GS, Gorstein J, Kupka R, Situma R, Yadav K, et al. Household coverage with adequately iodized salt varies greatly between countries and by residence type and socioeconomic status within countries: results from 10 national coverage surveys. J Nutr. 2017;147(5):1004s-s1014.
Organization WH. Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers. 2007.
Rohner F, Nizamov F, Petry N, Yuldasheva F, Ismailov S, Wegmüller R, et al. Household coverage with adequately iodized salt and iodine status of nonpregnant and pregnant women in Uzbekistan. Thyroid Off J Am Thyroid Assoc. 2020. https://doi.org/10.1089/thy.2019.0788.
Tariku WB, Mazengia AL. Knowledge and utilization of iodized salt and its associated factors at household level in Mecha District, Northwest Ethiopia. J Nutr Metab. 2019;2019:9763830.
Desta AA, Kulkarni U, Abraha K, Worku S, Sahle BW. Iodine level concentration, coverage of adequately iodized salt consumption and factors affecting proper iodized salt utilization among households in North Ethiopia: a community based cross sectional study. BMC Nutr. 2019;5:28.
Pandav CS, Yadav K, Salve HR, Kumar R, Goel AD, Chakrabarty A. High national and sub-national coverage of iodised salt in India: evidence from the first National Iodine and Salt Intake Survey (NISI) 2014–2015. Public Health Nutr. 2018;21(16):3027–36.
Luvanda HB, Paul E, Marwa YP, Hussein A, Mbogoro E, editors. Socio-economic and Spatial Correlates of Iodized Salt Usage among Tanzanian Households. In Proceedings of the Annual Statistical Conference University of Dodoma; 2018.
Kumma WP, Haji Y, Abdurahmen J, Mehretie AY. Factors affecting the presence of adequately iodized salt at home in Wolaita, Southern Ethiopia: community based study. Int J Food Sci. 2018;2018:4394908.
Knowles J, Kupka R, Dumble S, Garrett GS, Pandav CS, Yadav K, et al. Regression analysis to identify factors associated with household salt iodine content at the sub-national level in Bangladesh, India, Ghana and Senegal. Nutrients. 2018. https://doi.org/10.3390/nu10040508.
Krämer M, Kupka R, Subramanian SV, Vollmer S. Association between household unavailability of iodized salt and child growth: evidence from 89 demographic and health surveys. Am J Clin Nutr. 2016;104(4):1093–100.
Chao H, Zhang YF, Liu P, Han YF, Liu SJ. Relationship between Iodine content in household iodized salt and thyroid volume distribution in children. Biomed Environ Sci BES. 2016;29(6):391–7.
Rah JH, Anas AM, Chakrabarty A, Sankar R, Pandav CS, Aguayo VM. Towards universal salt iodisation in India: achievements, challenges and future actions. Matern Child Nutr. 2015;11(4):483–96.
Khatiwada S, Gelal B, Tamang MK, Kc R, Singh S, Lamsal M, et al. Iodized salt use and salt iodine content among household salts from six districts of Eastern Nepal. J Nepal Health Res Counc. 2014;12(28):191–4.
Gewa CA, Leslie TF, Pawloski LR. Geographic distribution and socio-economic determinants of women’s nutritional status in Mali households. Public Health Nutr. 2013;16(9):1575–85.
Ebrahim SM, Muhammed NK. Consumption of iodized salt among households of Basra city, south Iraq. Eastern Mediterranean Health J = La revue de sante de la Mediterranee orientale = al-Majallah al-sihhiyah li-sharq al-mutawassit. 2012;18(9):980–4.
Andersson M, de Benoist B, Rogers L. Epidemiology of iodine deficiency: salt iodisation and iodine status. Best Pract Res Clin Endocrinol Metab. 2010;24(1):1–11.
Kulwa KB, Kamuzora K, Leo G. Urinary iodine concentration and availability of iodated salt in school children in a goitre-endemic district of Tanzania. East Afr Med J. 2006;83(4):79–84.
Yamada C, Oyunchimeg D, Enkhtuya P, Erdenbat A, Buttumur A, Umenai T. Current status of iodine deficiency in Mongolia in 1998–1999. Asia Pac J Public Health. 2000;12(2):79–84.
Anteneh ZA, Engidayehu M, Abeje G. Iodine content of dietary salt at household level and associated factors using Iodometric titration methods in Dera District, Northwest Ethiopia. BMC Nutr. 2017;3:83.
Yaye AB, Baraki N, Endale BS. Availability of adequately iodized salt at household level and associated factors in Dire Dawa, Eastern Ethiopia. Int J Public Health Sci. 2016;5(4):392–9.
Abebe Z, Tariku A, Gebeye E. Availability of adequately iodized in Northwest Ethiopia: a cross-sectional study. Arch Public Health. 2017;75(1):33.
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF.
Tran TD, Hetzel B, Fisher J. Access to iodized salt in 11 low- and lower-middle-income countries: 2000 and 2010. Bull World Health Organ. 2016;94(2):122–9.
Banza BI, Lumbu JB, Donnen P, Twite EK, Kwete DM, Kazadi CM, et al. Iodine concentration in cooking salt consumed in Lubumbashi and the iodine status of vulnerable people: case study of pregnant women living in underprivileged areas. Pan Afr Med J. 2016;23:129.
Lohiya A, Yadav K, Kant S, Kumar R, Pandav CS. Prevalence of iodine deficiency among adult population residing in Rural Ballabgarh, district Faridabad, Haryana. Indian J Public Health. 2015;59(4):314–7.
Laillou A, Mam B, Oeurn S, Chea C. Iodized salt in Cambodia: trends from 2008 to 2014. Nutrients. 2015;7(6):4189–98.
Kassim IA, Moloney G, Busili A, Nur AY, Paron P, Jooste P, et al. Iodine intake in Somalia is excessive and associated with the source of household drinking water. J Nutr. 2014;144(3):375–81.
Bath SC, Button S, Rayman MP. Availability of iodised table salt in the UK—is it likely to influence population iodine intake? Public Health Nutr. 2014;17(2):450–4.
Watutantrige Fernando S, Barollo S, Nacamulli D, Pozza D, Giachetti M, Frigato F, et al. Iodine status in schoolchildren living in northeast Italy: the importance of iodized-salt use and milk consumption. Eur J Clin Nutr. 2013;67(4):366–70.
Alamneh AA, Leshargie CT, Desta M, Birhanu MY, Assemie MA, Denekew HT, et al. Availability of adequately iodized salt at the household level in Ethiopia: a systematic review and meta-analysis. PLoS ONE. 2021;16(2):e0247106.
Woldekiros HS. The route most traveled: the Afar Salt Trail, North Ethiopia 1. Chungara. 2019;51(1):95–110.
Gebre-Mariam A. The critical issue of land ownership. Violent conflict between the Abdalla Tolo-mogge and the Awlihan in Godey Zone, Somali Region, Ethiopia: NCCR North-South Dialogue; 2007.
Ugas M, Eggenberger W. Drought and floods stress livelihoods and food security in the Ethiopian Somali region. Addis Abeba: United Nations Development Programme Emergencies Unit of Ethiopia (UNDP-EUE). 1999.
Getahun A. Lake Afdera: a threatened saline lake in Ethiopia. SINET Ethiop J Sci. 2001;24(1):127–31.
Adish A, Chuko T, Abay A, Assey V, Desta T. Ethiopia: breaking through with a new iodized salt law. IDD Newsletter. 2013;41(4):1–24.
Mekonnen TC, Eshete S, Wasihun Y, Arefaynie M, Cherie N. Availability of adequately iodized salt at household level in Dessie and Combolcha Towns, South Wollo, Ethiopia. BMC Public Health. 2018;18(1):1152.
Ftwi G, Mengistie B, Abdo M, Roba KT. Household salt iodine level and associated factors in Dire Dawa City administration, Eastern Ethiopia. East Afr J Health Biomed Sci. 2018;2(2):35–44.
Tahir A, Seyoum B, Kadir H. Use of iodized salt at household level in Jig Jiga Town, Eastern Ethiopia. Asian J Agric Life Sci. 2016;1(2):18–24.
Sen TK, Das DK, Biswas AB, Chakrabarty I, Mukhopadhyay S, Roy R. Limited access to iodized salt among the poor and disadvantaged in North 24 Parganas district of West Bengal, India. J Health Popul Nutr. 2010;28(4):369–74.
Chen Y. New approaches for calculating Moran’s index of spatial autocorrelation. PLoS ONE. 2013;8(7):e68336.
Cheniti H, Cheniti M, Brahamia K. Use of GIS and Moran’s I to support residential solid waste recycling in the city of Annaba, Algeria. Environ Sci Pollut Res Int. 2021;28(26):34027–41.
Islam A, Sayeed MA, Rahman MK, Ferdous J, Islam S, Hassan MM. Geospatial dynamics of COVID-19 clusters and hotspots in Bangladesh. Transbound Emerg Dis. 2021;68(6):3643–57.
Jana M, Sar N. Modeling of hotspot detection using cluster outlier analysis and Getis-Ord Gi* statistic of educational development in upper-primary level, India. Model Earth Syst Environ. 2016;2(2):1–10.
Acknowledgements
The authors are happy to acknowledge the Institute of Public Health, College of Medicine and Health Science, University of Gondar. Our thanks also extend to the international Major DHS program for giving permission for data access.
Funding
No funding organization.
Author information
Authors and Affiliations
Contributions
AG, GM and MW developed the proposal, extracted the data, worked on analysis, interpreted the results, and prepared the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Permission for data access was obtained from Major DHS program after registered as authorized user. All the data used for this manuscript are publicly available and confidentiality was maintained anonymously.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Muluneh, A.G., Merid, M.W.M. & Kassa, G.M. Hotspots of un-iodized salt availability among Ethiopian households, evidence from the national survey data. J Health Popul Nutr 42, 20 (2023). https://doi.org/10.1186/s41043-023-00359-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41043-023-00359-5