Abstract
Background
The aim of the present study was to validate the Lifestyle Behavior Checklist (LBC) questionnaire, to measure Iranian parents' perceptions of their children's weight-related behaviors and their self-efficacy in dealing with those behaviors.
Methods
The LBC was translated into Farsi. Face and content validity of the questionnaire was evaluated by an expert panel. A total of 213 mothers of 3–12-year-old children responded to the questionnaire. Criterion validity of the questionnaire was evaluated through comparing its result with a parenting style questionnaire. Principal component analysis (PCA) and confirmatory factor analyses (CFA) were used to evaluate construct validity of the questionnaire. Reproducibility was measured by twice administration of LBC, one month apart and using Spearman's rho correlation test. The questionnaire's internal consistency was assessed by calculating Cronbach's α.
Results
LBC Problem scale was significantly correlated with authoritarian parenting style score, while the Confidence scale was significantly correlated with authoritative and negatively with permissive and authoritarian parenting styles. PCA suggested a six-factor construct, including, fussy eating, food-related problem behaviors, overeating behaviors, low interest in physical activity, poor self-image and sedentary behaviors. The results of CFA indicated acceptable fit indices for the proposed models. Both, Problem scale (Cronbach's α = 0.8) and Confidence scale (Cronbach's α = 0.95) had high internal consistency. Spearman correlation coefficients indicated acceptable reproducibility for both the Problem scale (r = 0.74) and the Confidence scale (r = 0.70).
Conclusions
The Farsi version of LBC questionnaire is reliable and reasonably valid to measure Iranian mothers' perception of their children's weight-related problem behavior.
Similar content being viewed by others
Introduction
Childhood obesity is one of the major challenges of the twenty-first century [1] that can affect child development and accelerate adverse cardiovascular and metabolic risk factors [2], as well as psychosocial problems [3]. The prevalence of childhood overweight and obesity has increased at an alarming rate in almost all developed and several developing countries [4]. In addition, childhood obesity tracks into the adulthood [5], and its early onset can lead to higher morbidity and mortality risk in later years [6]. In Iran, as a middle-income country experiencing epidemiological and nutrition transition, the prevalence of overweight and obesity among school-age children is 7.9 and 5.6%, respectively [7].
In response to the childhood obesity epidemic, an increasing number of interventions have been designed aiming to prevent childhood excessive weight gain and reduce the risk of obesity [8]. Successful interventions have been indicated the pivotal role of parents to shape eating patterns and physical activity habits in their children which can strongly affect their weight status [9]. However, the majority of parents are shown to have problem handling their children obesity-related behaviors [10, 11]. Two levels of parenting-related behaviors are often distinguished, including parenting practices and general parenting styles [12]. Specific parenting practices are content-specific acts of parenting, such as rules about food intake or daily activities [13]. Parenting style captures two important elements of parental responsiveness and parental demandingness [14]. Both levels of parenting have shown to be of importance in describing and predicting children’s weight-related behaviors [12].
Self-efficacy is an important determinant of parenting behaviors that its impact has increasingly been emphasized [15]. Bandura defined self-efficacy as “a person’s belief in his/her capabilities to organize and execute the course of action required to manage prospective situations” [16]. However, the construct of weight-related parenting self-efficacy has been mostly neglected in the studies on child weight [17]. Over the past few years, many researchers have suggested low parental self-efficacy as a possible obstacle for parents ability to change their children’s nutrition and physical activity behaviors [17, 18]. Thus, it is noteworthy to identify initial parental challenges in managing children’s lifestyle behavior, as well as their self-efficacy. It should also be noted that parents of overweight and obese children compared to those with normal weight children may face additional difficulties. Obese and overweight children may have more physical health problems, poorer emotional functioning and increased school problems than their normal weight peers [19]. Therefore, measurement of parental confidence and skills regarding weight-related challenges are critical in child obesity prevention and management programs. In this regard, valid instruments that can capture specific characteristics of parents in dealing with children’s weight-related behaviors are required.
Considering the lack of a specific instrument to measure weight-related parental self-efficacy, West and Sanders developed and validated the Lifestyle Behavior Checklist (LBC). LBC measures parental perceptions of their children’s behavioral problems with overweight and obesity, as well as parents’ self-efficacy in dealing with these behaviors [20]. The tool was modified and applied in the Netherlands [21] and Sweden [22] and showed to be reliable and reasonably valid. In addition, the LBC scales are shown to be responsive to change following a parenting intervention [23].
The present study, as part of a larger pilot study on management of childhood obesity and overweight in Iran, aimed to evaluate the validity and reliability of the LBC questionnaire to measure Iranian parents’ perceptions of their children’s behavioral problems with overweight and obesity and their self-efficacy in dealing with these behaviors.
Methods
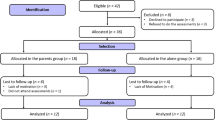
This cross-sectional study was conducted from July to December 2013. The study was designed in two distinct phases: (1) translation and validation of the scale; and (2) confirmatory study to ensure the validity of the scale.
Phase (1) Translation and validation of the Lifestyle Behavior Checklist
The 25-item Lifestyle Behavior Checklist is designed to assess parental perceptions regarding the extent of behavior problems of their overweight and obese children and parents’ confidence about managing their child problem behaviors. The checklist is composed of four sub-scales, including (1) misbehavior in relation to food (e.g., the child yells about food, eats unhealthy snacks, refuses to eat certain foods), (2) overeating (e.g., the child eats too much), (3, 4) emotional correlates of overweight (e.g., the child complains about being overweight) and physical activity (e.g., the child complains about being physically active) [20] and is consisted of two main parts, including (a) Problem scale and (b) Confidence scale. The Problem scale measures the extent to which parents perceive each of the 25 behaviors to be a problem behavior in their child, on a 7-point scale from 1 (not at all) to 7 (very much). The Confidence scale measures the extent to which parents feel confident about managing each behavior on a 10-point scale from 1 (certain I cannot do it) to 10 (certain I can do it).
The clinical cutoff values for the Problem scale are above 50 (range = 25–175) and for the Confidence scale under 204 (range = 25–250) [24].
Translation: The LBC was first translated into Farsi by four experts, including three nutritionists and a health education specialist. To produce a conceptual equivalence of translation to the original English questionnaire, all translators discussed any disparities and agreed on a single version. The final translated version was then translated back into English by a professional translator who was not involved in Farsi translation process and sent back to Dr. West via email. The meaning of the original LBC questions appeared similar in most cases.
Face and content validity: After finalizing the translation process, the questionnaire was pretested among 15 mothers who were part of the target population (but were not included in the final study) to ensure clarity in the linguistic and conceptual equivalence of the translations. The pretest was based on cognitive interviewing, i.e., using verbal probing techniques to identify the optimal format and wording of the questions. Only one item was changed during pretesting due to cultural acceptability (takes food from others instead of steals food from others). Subsequently, another meeting between the experts took place to finalize the questionnaire.
Criterion validity: Criterion validity of Farsi version of LBC was evaluated by comparing its result with a locally validated questionnaire on parenting styles. The latter questionnaire is the only valid questionnaire in Iran for assessing parenting styles [25]. The parenting style questionnaire has been developed for the purpose of measuring Baumrind's [27] permissive, authoritarian and authoritative parental authority prototypes [26]. It consists of 30 items and yields permissive, authoritarian and authoritative scores for both mother and father. Each of these parenting styles reflects different naturally occurring patterns of parental values, practices and behaviors [27]. Permissive parents were seen as more responsive than they are demanding. According to Baumrind’s perspective, permissive indulgent parents were “nontraditional and lenient, did not require mature behavior, allowed considerable self-regulation, and avoided confrontation.” Authoritarian parents, on the other hand, were seen as highly demanding and directive and not responsive. Authoritarian parents appear to provide well-ordered and structured environments with clearly stated rules. However, authoritative parents were both demanding and responsive. They are assertive, but not intrusive and restrictive [27].
Criterion validity was assessed using bivariate correlations (Spearman’s rho correlation tests) between the LBC scales and the parenting styles scores. The magnitude of the relationship (effect size, “r”) was used as a source of information. Interpretation of the strength of the effect size was based on Cohen’s descriptive guidelines. A correlation higher than or equal to 0.50 was regarded as large, between 0.30 and 0.50 as medium and those smaller than or equal to 0.20 as small effect size.
Construct validity: In the present study, principal component analysis (PCA) extraction was used to explore the existing factorial pattern. The number of factors was determined through evaluating four criteria: eigenvalues, percent of explained variance by each factor, scree plot and interpretability.
Reliability: Internal consistency of the scales was assessed using Cronbach’s alpha coefficient. To assess reproducibility, the LBC questionnaire was filled by 27 of the mothers twice, one month apart (test–retest).
Participants: The study sample consisted of 213 mothers who were selected through convenient sampling from those who were visiting primary healthcare centers in districts 4, 7 and 8 in the city of Tehran. Respondents were included if they were mothers of children aged 3–12 years and agreed to take part in the study by signing an informed consent.
Data collection: Mothers filled out the questionnaire in the waiting room of the selected health centers. Demographic information including mother and father’s age, education level, employment and marital status were obtained. Child characteristics (date of birth, gender, height and weight) were recorded out of the health records. Children’s BMI was calculated and recoded into BMI Z-scores curves. Weight status based on BMI Z-scores was classified into healthy weight (Z-score BMI for age between − 2 and + 1), overweight (between ≥ 1 and + 2) or obese (≥ + 2) as defined by WHO references in 2007 [28]. Children with underweight were excluded.
Phase (2) Confirmatory study
In order to evaluate the factor structures identified through this analysis, mothers of 174 children aged 6–7 years were selected from districts 7 and 8 in Tehran city. To assess the consistency of the results, the selected samples were different from those studied in the previous phase. Written informed consent was obtained from students and their parents. Confirmatory factor analysis (CFA) was performed by AMOS 21.0, using the same parameters and fit indices, as phase 2.
Discriminative validity: To examine discriminative validity, group means for all the individual items of the Problem scale and the Confidence scale were compared between parents of children with normal weight and those with overweight or obese children (Table 3).
Statistical analysis
Descriptive statistics were used to examine the normality and quality of the items. A quality item should have a mean that represents the middle of the response scale and a larger standard deviation. The total score of each scale was computed by summing up items related to the scale and used in the analysis. Data were presented as “Mean ± SD” for the quantitative continuous variables. Percentages of the categorical data were also calculated. All p values < 0.05 were regarded significant. Statistical Package for the Social Sciences (SPSS) for Windows, version 21.0; IBM Co., Armonk, NY, USA, was used for data analysis.
PCA was performed to determine the number and nature of underlying factors in the scale. Sampling adequacy was evaluated by Kaiser–Meyer–Olkin (KMO). Bartlett's test of sphericity and total variance explained were used for the evaluation of factor analysis. Factor loadings were used to keep or drop items. CFA was performed to test whether data fit the hypothesized measurement model that was extracted by PCA.
Weighted least squares (WLS) estimation method was used at CFA. Asymptomatic covariance matrix was considered as a weighted matrix. Goodness-of-fit indices (GFIs) and reasonable threshold levels of these indices for CFA were considered as χ2/df < 3, root mean square error of approximation (RMSEA) < 0.08, goodness-of-fit index (GFI) > 0.9 and adjusted goodness-of-fit index (AGFI) > 0/8 [29].
Results
Phase (1) Validation of the scale
A total of 213 mothers of 3–12-year-old children took part in the study. They were all the biological mothers of the children. Characteristics of the participants are summarized in Table 1. Of the children, 26.3% were overweight or obese.
Criterion validity: Problem scale score was positively correlated only with authoritarian style (r = 0.16, p = 0.014), while Confidence scale was positively correlated with authoritative parenting style (r = 0.14, p = 0.04) and negatively correlated with permissive (r = − 0.14, p = 0.03) and authoritarian (r = − 0.19, p = 0.004). In other words, mothers with authoritarian parenting style had a higher score on the Problem scale.
Construct validity: PCA on Problem scale resulted in extraction of 5 components. The KMO (Kaiser–Meyer–Olkin Measure of Sampling Adequacy) was 0.71 exceeding the recommended value of > 0.6, which indicates sufficient sample size. Bartlett’s test confirmed factor analysis appropriateness (χ2 = 1475.19, df = 300 and p < 0.001). The five-component solution accounted for 49% of the variance (Table 2). Item 17 in component 1 (fussy eating) and item 16 in component 2 (food-related problem behaviors) had low factor loading, and theoretically, they were meaningless; therefore, they were categorized as the sixth component. The six components were labeled as “fussy eating (FE),” including items 4, 5, 6 and 7, “food-related problem behaviors (FPB)” including items 3, 10, 11, 12, 13, 14 and 15, “overeating behaviors (OB)” including items 1, 2, 8 and 9, “low interest in physical activity (LPA)” including items 18, 19 and 20, “poor self-Image (PSI)” including items 21, 22, 23, 24 and 25 and “sedentary behaviors (SB)” including items 16 and 17.
Second-order confirmatory factor analysis for Problem scale is shown in Fig. 1 (χ2/df = 1.699, p < 0.001; CFI = 0.847; GFI = 0.832, AGFA = 0.797, RMSEA = 0.064). All factor loadings were statistically significant (p < 0.001). Therefore, CFA confirmed the accuracy of the 6 component structure. Since both parts of the questionnaire (Problem scale and Confidence scale) are designed to estimate a number of common concepts, the same model of six components was used for Confidence scale and confirmed by CFA (χ2/df = 2.074, p < 0.001; CFI = 0.880; GFI = 0.808, AGFA = 0.768, RMSEA = 0.079) (Fig. 2).
Discriminant validity: To examine discriminant validity, group means for all items of the Problem scale and the Confidence scale were provided and compared between parents of children with normal weight and those whose children were overweight or obese (Table 3). On the Problem scale, 9 of the 25 items significantly differed between the groups. The mean and standard deviation of total scores on the Problem scale for parents of children with normal weight were lower (58.2 ± 15.2) than those for parents of overweight or obese children (62.8 ± 19.9); however, they were not significant.
On the Confidence scale, no significant difference was observed between the two group’s total scores. However, parents of overweight or obese children scored lower on 14 of the items and two of them were close to statistically significant: argues about food (e.g., when you say no more) (p = 0.054) and complains about being overweight (p = 0.057).
Reliability: Both Problem scale (Cronbach’s α = 0.80) and Confidence scale (Cronbach’s α = 0.95) had high internal consistency. Internal consistency of Problem scale components (sub-scales) included: fussy eating 0.78, food-related problem behaviors 0.67, overeating behaviors 0.68, low interest in physical activity 0.76, poor self-image 0.58 and sedentary behaviors was 0.61. Internal consistency of Confidence scale components was as follows: fussy eating 0.82, food-related problem behaviors 0.85, overeating behaviors 0.8, low interest in physical activity 0.85, poor self-image 0.89 and sedentary behaviors was 0.71. Poor self-image and sedentary behaviors scales had the lowest Cronbach’s α.
Means and standard deviations of the Problem scale and Confidence scale are presented in Table 3. Based on Pearson correlation coefficient, both Problem scale (r = 0.606, p = 0.001) and Confidence scale (r = 0.751, p < 0.001) had acceptable test–retest reliability. Spearman correlation between Problem scale and Confidence scale showed a significant negative correlation that means high scores on the Problem scale correlated with lower scores on the Confidence scale (r = − 0.38, p < 0.0001). There was no significant difference in the Problem scale and Confidence scale of mothers according to the sex of their child.
The maximum score in the Confidence scale was related to item 14 (takes food) in both normal and overweight/obese children and the minimum score in overweight/obese children was related to item 10 (Requests food continuously between meals).
Discussion
This study showed that LBC is a relatively valid and reliable tool to assess children’s obesity-related behaviors and parental self-efficacy to handle these behaviors in the Iranian population. In the present study, evaluating the construct of the questionnaire resulted in 6 components (fussy eating, food-related problem behaviors, overeating behaviors, low interest in physical activity, poor self-Image and sedentary behaviors). Previous studies on the psychometric analysis of LBC have all used EFA [20, 22], except for Gerards et al. study in the Netherlands [21]. The study by West et al. for Problem scale EFA resulted in 4 factors [30] (misbehavior in relation to food, overeating, emotional correlates of being overweight and physical activity); however, CFA was not done. On the other hand, in Ek study, 5 components were extracted, including Overeating, Physical Activity, Emotional correlates of being overweight, Misbehavior in relation to food and Screen Time. In the original model, sedentary behaviors were part of the physical activity scale, but based on Ek study and the present study, they were identified as two separate dimensions. The three dimensions that are present in all 3 studies include overeating, physical activity and emotional correlates of being overweight. In general, the six components scale adopted in the current study is closer to the modified scale by Ek; however, the correlations coefficients are smaller. Ek et al. omitted 6 items [3, 4, 7, 13, 20, 23] in their final model [22]. In addition, poor fit to the target population, as well as cultural and age differences between the study subjects may have had an effect on these results.
In estimating dimensions of the model, due to the lack of consensus among Structural Equation Model (SEM) specialists, several model fit indices have been used, including Chi-square (χ2), goodness-of-fit index (GFI), the adjusted goodness-of-fit index (AGFI) and root mean square error of approximation (RMSEA) and Comparative Fit Index (CFI) [31]. The RMSEA is currently the most popular measure of fitness which was almost within the acceptable range (≤ 0.08) in both parts of LBC (0.06 and 0.07 in Problem scale and Confidence scale, respectively). Based on the results of SEM, the optimum model of the scale is marginally acceptable.
Discriminate validity of the Problem scale showed a significant difference in 8 items, mostly related to overeating and fussy eating. There was no significant difference in Confidence scale scores between mothers of normal weight and overweight/obese children that indicated its poor discriminatory function. Overall, the Confidence scale seemed to be less sensitive than Problem scale.
In the present study, compared to Ek et al. and Gerards et al. reports, the mean score of mothers of overweight/obese children was higher in the Problem scale and lower in the Confidence scale. It can be concluded that in the present study mothers have more problems with child obesity-related behaviors while having lower self-efficacy to deal with the problems.
West et al. reported statistically significant differences between groups with different child weight status, for both scales [20]. However, they did not consider overweight children, when comparing parents of healthy weights with those of obese children. This difference in the samples may be responsible for higher mean scores of parents of Australian obese children on all Problem scale items compared to those of the parents of overweight and obese children in our study. In the present study, compared with Ek [22] and West’s study, each of the two parts of LBC had less discriminatory function. However, the internal consistency of the scales was similar to what was reported by West and Gerards [21].
This is the first study evaluating the psychometric properties of the LBC in Iran. Considering a heterogeneous sample of children with weight status, as well as a high response rate (75%) are strengths of the present study. However, the present study had some limitations that should be considered when evaluating its results. First, the weight and height measures of children were self-reported. Lack of measurement of mother’s weight is another limitation of this study. Also, to achieve more accurate results, it would be better to use another criterion measure in addition to Baumrind questionnaire. The cross-sectional design of the present study does not allow any conclusion on the causal effect of child behavior, parenting styles and self-efficacy. Considering different dimensions of validity parameters, more studies on Iranian mothers are recommended.
Availability of data and materials
It will be available from the author upon reasonable request.
References
World Health Organization. Population-based prevention strategies for childhood obesity: report of a WHO forum and technical meeting, Geneva, 15-17 December 2009. 2010.
Rademacher ER, Jacobs DR Jr, Moran A, Steinberger J, Prineas RJ, Sinaiko A. Relation of blood pressure and body mass index during childhood to cardiovascular risk factor levels in young adults. J Hypertens. 2009;27(9):1766.
Puhl RM, Latner JD. Stigma, obesity, and the health of the nation’s children. Psychol Bull. 2007;133(4):557.
Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1(1):11–25.
Brisbois T, Farmer A, McCargar L. Early markers of adult obesity: a review. Obes Rev. 2012;13(4):347–67.
Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101(Supplement 2):518–25.
Siassi F, Pour Aram H, Djazayery G, Jalali M HR, Khodaverdan K, Dorosti-Motlagh A, Sotoudeh G, Sojoudi F, Abdollahi Z, Mohammad K, Yar Parvar A, Sadrzadeh Yeganeh H. National integrated micronutrient survey 2012 (NIMS-2). Iran: Andshesheh Mandegar; 2016.
Wang Y, Wu Y, Wilson RF, Bleich S, Cheskin L, Weston C, et al. Childhood obesity prevention programs: comparative effectiveness review and meta-analysis. 2013.
Lindsay AC, Sussner KM, Kim J, Gortmaker S. The role of parents in preventing childhood obesity. Future Child. 2006;16:169–86.
Styles JL, Meier A, Sutherland LA, Campbell MK. Parents’ and caregivers’ concerns about obesity in young children: a qualitative study. Fam Community Health. 2007;30(4):279–95.
Borra ST, Kelly L, Shirreffs MB, Neville K, Geiger CJ. Developing health messages: qualitative studies with children, parents, and teachers help identify communications opportunities for healthful lifestyles and the prevention of obesity. J Am Diet Assoc. 2003;103(6):721–8.
Sleddens EF, Gerards SM, Thijs C, Vries NK, Kremers SP. General parenting, childhood overweight and obesity-inducing behaviors: a review. Int J Pediatr Obes. 2011;6(2Part2):e12.
Gubbels JS, Kremers SP, Stafleu A, de Vries SI, Goldbohm RA, Dagnelie PC, et al. Association between parenting practices and children’s dietary intake, activity behavior and development of body mass index: the KOALA Birth Cohort Study. Int J Behav Nutr Phys Act. 2011;8(1):18.
Power TG. Parenting dimensions and styles: a brief history and recommendations for future research. Child Obes. 2013;9(s1):S-14-S-21.
Jones TL, Prinz RJ. Potential roles of parental self-efficacy in parent and child adjustment: a review. Clin Psychol Rev. 2005;25(3):341–63.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191.
Nelson M, Davis MC. Development and preliminary validation of the parent efficacy for child healthy weight behaviour scale. J Health Psychol. 2013;18(2):282–91.
Smith BJ, Grunseit A, Hardy LL, King L, Wolfenden L, Milat A. Parental influences on child physical activity and screen viewing time: a population based study. BMC Public Health. 2010;10(1):593.
Haugstvedt KTS, Graff-Iversen S, Bechensteen B, Hallberg U. Parenting an overweight or obese child: a process of ambivalence. J Child Health Care. 2011;15(1):71–80.
West F, Sanders MR. The Lifestyle Behaviour Checklist: a measure of weight-related problem behaviour in obese children. Int J Pediatr Obes. 2009;4(4):266–73.
Gerards SM, Hummel K, Dagnelie PC, de Vries NK, Kremers SP. Parental self-efficacy in childhood overweight: validation of the Lifestyle Behavior Checklist in the Netherlands. Int J Behav Nutr Phys Act. 2013;10(1):1–10.
Ek A, Sorjonen K, Nyman J, Marcus C, Nowicka P. Child behaviors associated with childhood obesity and parents’ self-efficacy to handle them: confirmatory factor analysis of the Lifestyle Behavior Checklist. Int J Behav Nutr Phys Act. 2015;12(1):1–13.
West F, Sanders MR, Cleghorn GJ, Davies PS. Randomised clinical trial of a family-based lifestyle intervention for childhood obesity involving parents as the exclusive agents of change. Behav Res Ther. 2010;48(12):1170–9.
West F. Lifestyle Triple P Project: exploring the link between parenting and childhood obesity. 2007.
Esfandiari. Assessing and evaluating of parenting styles of normal and abnormal children (in Persian), Tehran; 1995.
Buri JR. Parental authority questionnaire. J Pers Assess. 1991;57(1):110–9.
Baumrind D. Current patterns of parental authority. Dev Psychol. 1971;4(1p2):1.
World Health Organization. Growth reference data for 5–19 years/indicators/BMI-for-age (5–19 years). World Health Organization. https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/bmi-for-age (2007).
Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88(3):588.
West F, Morawska A, Joughin K. The Lifestyle Behaviour Checklist: evaluation of the factor structure. Child Care Health Dev. 2010;36(4):508–15.
Hu L-T, Bentler PM, Kano Y. Can test statistics in covariance structure analysis be trusted? Psychol Bull. 1992;112(2):351.
Acknowledgements
We acknowledge the contribution of all health workers who conducted data collection. Also, the authors would like to thank Dr M. Ghazi-Tabatabaie and Dr A. Djazayeri for their technical consultation.
Funding
This study was supported by UNICEF and Ministry Of Health of Iran, Community Nutrition Office.
Author information
Authors and Affiliations
Contributions
NO, PA and SN formulated the study concept, designed the study and carried out the literature search. SN and SRS acquired the data. SN, NO, HE-Z, PA, AD and SRS prepared the manuscript. NO, HE-Z, SN and AD carried out statistical analysis. NO, HE-Z, PA, SN and AD analyzed and interpreted the data. NO performed the supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All subjects signed a written informed consent. The study protocol was approved by the ethics committee of the National Nutrition and Food Technology Research Institute.
Consent for publication
All of the authors agreed for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Omidvar, N., Narmcheshm, S., Eini-Zinab, H. et al. Assessing parents’ self-efficacy to handle child obesity-related behaviors: validation of the Lifestyle Behavior Checklist in Iran. J Health Popul Nutr 41, 9 (2022). https://doi.org/10.1186/s41043-022-00288-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41043-022-00288-9