Abstract
Background
Heated, humidified, high-flow nasal cannula (HHFNC) oxygen therapy allows optimal humidification of inspired gas at high flows and creates a distending pressure similar to nasal continuous positive airway pressure [1]. It has been safely used in adults with moderate hypoxemia with few complications [2, 3]. Hereby, we report serious complications occurred during HHFNC oxygen therapy.
Case presentation
A 53-year-old female with hemophagocytic lymphohistiocytosis (HLH) was admitted to the intensive care unit because of respiratory failure. After weaning from mechanical ventilation which lasted for 2 weeks, HHFNC therapy at 40 L/min with an FiO2 of 0.5 was started for hypoxemia. Four days later, dyspnea and hypoxemia occurred and chest X-ray and CT scan revealed localized pneumothorax, subcutaneous emphysema, and massive pneumomediastinum. After cessation of HHFNC, respiratory condition improved.
Conclusion
Subcutaneous emphysema, pneumothorax, and pneumomediastinum should be notified as a serious complication during HHFNC therapy.
Similar content being viewed by others
Background
Humidified high-flow nasal cannula (HHFNC) is useful before and after mechanical ventilation in tracheal intubation. Above all, it has been considered to be of advantage that it can be done safely and that the patient’s QOL is maintained. There are other benefits as well. For example, the positive end-expiratory pressure (PEEP) effect of HHFNC is considered to have a positive effect on acute heart failure, and it is also said that it has a CO2 washout effect at high flow rates. Meanwhile, as an adverse effect, Kang and colleagues found that using HHFNC for longer than 48 h before intubation was associated with higher ICU mortality and less success at extubation and ventilator weaning, and fewer ventilator-free days. They examined all subjects who failed HHFNC delayed and required intubation [4]. In this time, we experienced patients with severe complications. This manuscript was contributed for the purpose of making it widely known and hoping that preventing such complications will ensure the safety of the patient.
Case presentation
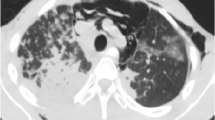
A 53-year-old female with hemophagocytic lymphohistiocytosis (HLH) was admitted to the intensive care unit (ICU) because of respiratory failure. Immediately after admission, her airway was established using a cuffed 7.0-mm tracheal tube. Her chest X-ray showed severe bilateral infiltrates, and blood gas showed moderate level of acute respiratory distress syndrome (ARDS). Immediately after beginning of mechanical ventilation, high positive end-expiratory pressure (PEEP) combined with low tidal volume was applied. Her respiratory status gradually improved. Two weeks after commencement of mechanical ventilation, finally, her trachea was extubated. However, she developed mild hypoxemia with standard oxygen therapy and was suffering from tenacious secretion. HHFNC therapy at 40 L/min with an FIO2 of 0.5 (Optiflow system™, MR850 heated humidified RT202 delivery tubing; Fisher and Paykel Healthcare Ltd., Auckland, New Zealand) was applied through nasal cannula (Optiflow™; Fisher and Paykel, Auckland, New Zealand), and a mini tracheostomy cannula (Portex™ Mini-Trach™ II, Smith Medical, Kent, UK) was placed to treat her sputum. Her oxygenation was improved, and FIO2 was decreased to 0.35. Four days later, she complained of respiratory discomfort. Her oxygenation worsened and hemodynamic status also deteriorated. Specifically, FIO2 was 0.35 and PaO2 was about 60 mmHg, and PaCO2 was less than 30 mmHg because of respiratory acceleration (35 per minute). In hemodynamics, blood pressure itself was maintained, but it became sinus tachycardia of about 100 to 130 times per minute. Her chest X-ray revealed a localized pneumothorax and subcutaneous emphysema (Fig. 1a). A subsequent chest CT showed massive pneumomediastinum and a localized right-side pneumothorax, and subcutaneous emphysema were confirmed (Fig. 2). Regarding these air leaks, they seemed difficult to release. We decided to observe her course with changing HHFNC therapy to the standard oxygen therapy (5 L/min of O2 administration through a standard oxygen mask). She could not improve subjective discomfort easily, but her oxygenation and hemodynamic status gradually improved. On the next day, it was confirmed by a chest X-ray that the localized pneumothorax and emphysema disappeared (Fig. 1b).
Moreover, she had a lung with bulla, and it is undeniable that the bulla ruptured due to cough caused by suction after extubation, and the pressure by HHFNC was applied to it and pneumothorax occurred.
Discussion
The air leak is a well-known complication of positive pressure ventilation, and HHFNC provides increased pressure within airways [5], which may potentially cause air leak.
In the present case, air leak would have been ascribed to positive airway pressure generated by HHFNC through micro-tear of the trachea caused by mini-tracheostomy cannula placement or damage to the tracheal wall due to suctioning through the mini-tracheostomy. Otherwise, air leak might have occurred due to rupture of bulla and alveoli due to cough associated with suctioning. However, these could not go beyond speculation. Serious air leaks related to HHFNC therapy have been reported in pediatric patients [6]. Our case was an adult patient; however, her background status, which means post-ARDS, seemed to predispose to air leaks. In this case, we think from the image findings that air may initially leak into the mediastinum and the subcutaneous tissue, and then into a part of pleural space.
The reason why the pneumothorax was localized is probably because her pleural space was adhesive after inflammatory reaction. After cessation of HHFNC therapy, airflow under spontaneous breathing without any artificial support was regulated in her airway because of the absence of excessive airway pressure, which did not worsen air leaks and improved her respiratory condition.
Conclusion
Positive pressure ventilation should be used with caution if there is a possible airway injury. HHFNC also may contribute to the development of air leak syndrome although HHFNC therapy tends to be sought gentler than other conventional therapy.
Availability of data and materials
The authors have the availability of supporting data.
References
Lampland AL, Plumm B, Meyers PA, et al. Observational study of humidified high-flow nasal cannula compared with nasal continuous positive airway pressure. J Pediatr. 2009;154(2):177–82.
Sztrymf B, Messika J, Bertrand F, et al. Beneficial effects of humidified high flow nasal oxygen in critical care patients: a prospective pilot study. Intensive Care Med. 2011;37(11):1780–6.
Sztrymf B, Messika J, Mayot T, et al. Impact of high-flow nasal cannula oxygen therapy on intensive care unit patients with acute respiratory failure: a prospective observational study. J Crit Care. 2012;324(27):e9–13.
Kang BJ, Koh Y, Lim CM, et al. Failure of high-flow nasal cannula therapy may delay intubation and increase mortality. Intensive Care Med. 2015;41(4):623–32.
Roca, et al. Current evidence for the effectiveness of heated and humidified high flow nasal cannula supportive therapy in adult patients with respiratory failure. Crit Care. 2016;20:109.
Hegde S, Prodhan P. Serious air leak syndrome complicating high-flow nasal cannula therapy: a report of 3 cases. Pediatrics. 2013;131(3):e939–44.
Acknowledgements
The authors would like to extend their gratitude to the patient and her family members.
Funding
The authors received no external funding.
Author information
Authors and Affiliations
Contributions
KM and IS drafted the manuscript. NT and EJ treated and followed up on the patient in the intensive care unit. KM supervised the drafting of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The consent of the patient’s next of kin was obtained; however, institutional review board approval was exempted because neither ethical problem nor description to identify the patient was included in this case report.
Consent for publication
Informed consent for scientific publication was obtained from the patient’s next of kin.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sonobe, S., Inoue, S., Nishiwada, T. et al. A case of subcutaneous emphysema/mediastinal emphysema during the use of humidified high-flow nasal cannula. JA Clin Rep 5, 85 (2019). https://doi.org/10.1186/s40981-019-0305-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40981-019-0305-3