Abstract
Background
Variants in cardiomyopathy genes have been identified in patients with cancer therapy-related cardiac dysfunction (CTRCD), suggesting a genetic predisposition for the development of CTRCD. The diagnostic yield of genetic testing in a CTRCD population compared to a cardiomyopathy patient cohort is not yet known and information on which genes should be assessed in this population is lacking.
Methods
We retrospectively included 46 cancer patients with a history of anthracycline induced CTRCD (defined as a decrease in left ventricular ejection fraction (LVEF) to < 50% and a ≥ 10% reduction from baseline by echocardiography). Genetic testing was performed for 59 established cardiomyopathy genes. Only variants of uncertain significance and (likely) pathogenic variants were included. Diagnostic yield of genetic testing was compared with a matched cohort of patients with dilated cardiomyopathy (DCM, n = 46) and a matched cohort of patients without cardiac disease (n = 111).
Results
Average LVEF at time of CTRCD diagnosis was 30.1 ± 11.0%. Patients were 52.9 ± 14.6 years old at time of diagnosis and 30 (65.2%) were female. Most patients were treated for breast cancer or lymphoma, with a median doxorubicin equivalent dose of 300 mg/m2 [112.5-540.0]. A genetic variant, either pathogenic, likely pathogenic or of uncertain significance, was identified in 29/46 (63.0%) of patients with CTRCD, which is similar to the DCM cohort (34/46, 73.9%, p = 0.262), but significantly higher than in the negative control cohort (47/111, 39.6%, p = 0.018). Variants in TTN were the most prevalent in the CTRCD cohort (43% of all variants). All (likely) pathogenic variants identified in the CTRCD cohort were truncating variants in TTN.
There were no significant differences in severity of CTRCD and in recovery rate in variant-harbouring individuals versus non-variant harbouring individuals.
Conclusions
In this case-control study, cancer patients with anthracycline-induced CTRCD have an increased burden of genetic variants in cardiomyopathy genes, similar to a DCM cohort. If validated in larger prospective studies, integration of genetic data in risk prediction models for CTRCD may guide cancer treatment. Moreover, genetic results have important clinical impact, both for the patient in the setting of precision medicine, as for the family members that will receive genetic counselling.
Similar content being viewed by others
Background
Anthracyclines (AC) are one of the most commonly used chemotherapeutic agents, but they are associated with significant toxicities, with cardiotoxicity being the most concerning. Up to 57% of all patients receiving AC develop subclinical cardiotoxicity and up to 9% experience a clinically significant decrease in left ventricular ejection fraction (LVEF) during or within the first year after treatment [1]. Whilst effective cancer treatment has resulted in a growing population of cancer survivors, it underscores the imperative for timely diagnosis, treatment, and ideally, prevention of cancer therapy-related cardiac dysfunction (CTRCD) [2].
Several tools for risk stratification have been developed to assess the individual risk prior to AC treatment [3, 4]. However, the development of AC-induced CTRCD is not fully explained by treatment regimen or patient characteristics alone. This complicates accurate risk assessment and deserves finetuning [2].
Recently, the presence of genetic variants in structural cardiac genes has been described in selected patients with CTRCD [5,6,7,8,9], pointing towards a genetic predisposition. This was confirmed in a larger retrospective and prospective study in cancer patients. In that population, truncating variants in TTN (TTNtv) were significantly more prevalent in patients developing CTRCD (10%) compared to a cohort of self-reported healthy volunteers (0.7%) [10]. In cardiomyocytes, the giant protein titin (encoded by TTN) operates as a bidirectional spring, determining the sarcomeric visco-elasticity and modulating passive stiffness [11]. TTN is the gene with the most identified causal variants, specifically TTNtv, in dilated cardiomyopathy, in up to 15-25% of patients [12, 13]. Truncating variants are variants that are predicted to have a substantial effect on the structure of titin, leading to an unstable transcript in contrast to missense variants, where a substitution of an amino acid occurs, but the overall structure of the transcript is unaffected [13].
Therefore, the identification of genes that are associated with AC-induced CTRCD opened new opportunities to define patients at high-risk and to prevent adverse outcomes. However, some knowledge gaps remain, limiting implication into standard of care. The comparison of the diagnostic yield of genetic testing between CTRCD and dilated cardiomyopathy (DCM) patients remains elusive. Additionally, information on which genes should be prioritized in the CTRCD population is lacking. In the context of a second-hit hypothesis, where a genetic variant may only lead to an overt phenotype after exposure to chemotherapy, the role of variants with milder pathogenic properties serving as potential genetic modifiers remains unclear. And lastly, there are no guidelines advising retrospective genetic testing in historic patients with CTRCD, so further proof of its importance for patients and their family members is needed.
In the current paper we aimed to study the genetic burden in CTRCD patients, compared to DCM patients and a negative control cohort without cardiac disease. We also assessed the prevalence and importance of variants of uncertain significance (VUS) in this population. Lastly, we evaluated the impact of a genetic diagnosis in the index on cascade screening and family members.
Methods
CTRCD, DCM and healthy control cohorts
In this single centre cohort study, patients with a history of CTRCD after AC chemotherapy, presenting between 1995 and 2020, were consecutively screened in a large academic heart failure and transplantation centre. Patients were eligible if they had developed CTRCD, defined as a decrease in LVEF to < 50% and a ≥ 10% reduction from baseline by echocardiography [14]. This definition complies with the current definition of moderate (LVEF < 50%) and severe (LVEF < 40%) CTRCD [2]. Both early (onset within one year after chemotherapy) and late (> 1 year after end of chemotherapy) CTRCD were included. Exclusion criteria were presence of LVEF < 50% or known relevant ischemic or valvular heart disease prior to treatment.
A positive control cohort consisted of patients with DCM defined according to the ESC cardiomyopathy definition [15], referred for genetic testing as part of standard clinical care and who were matched for age, gender and familial history of DCM.
A negative control cohort consisted of age and gender-matched patients without cardiac disease that underwent genetic testing for other indications (respectively patients with COVID or thoracic aorta aneurysmal disease). Absence of cardiac disease was verified via medical reports and echocardiography data if these were available.
The study conforms with the principles outlined in the Declaration of Helsinki [16]. The current study was approved by the local ethics committee of the University Hospital of Antwerp. All subjects gave written informed consent to participate in the study.
Clinical evaluation
Clinical data at baseline and follow-up were retrieved from the patient files. Oncological diagnosis, cumulative dose of anthracycline, cardiovascular risk factors, comorbidities and cardiovascular function (echocardiography or gated blood pool scan if echocardiography was not available) were collected. Follow-up data included LVEF decline, LVEF recovery, cardiac transplantation and death.
Genetic analysis
All eligible patients were offered genetic testing. Genomic DNA was extracted from EDTA blood using standard procedures (Chemagic DNA bloodkit special, Perkin Elmer, Waltham, MA, USA). Variant detection was performed using a an in-house HaloPlex targeted gene panel for next-generation sequencing (NGS) of 59 known cardiomyopathy genes (CM59-panel) [17]. Supplementary Table 1 shows the complete list of genes and their corresponding transcript included in the CM-panel. Analysis was performed of all coding exons including intron/exon transitions to a maximum of 15 intronic nucleotides. Variants were classified as benign or likely benign (class 1 and 2), variant of uncertain significance (class 3), likely pathogenic (class 4) or pathogenic (class 5) according to ACMG guidelines [18]. Only class 3, 4 and 5 variants were considered clinically actionable. All reported variants were confirmed using Sanger sequencing if they did not comply to strictly defined next generation sequencing quality criteria [17]. All variants were reviewed by a multidisciplinary cardiogenetic team (clinical geneticist, molecular geneticist, cardiologists and genetic counsellors).
Lastly, overall variant burden for the whole CM 59 panel was calculated as the sum of all variants divided over the total allele number of all genes (Variant burdenCM59 = [sum off all variants]/[Allele numbergene1 + …….. + allele numbergene59]) [19]. For genes located on the X-chromosome (EMD; FHL1; GLA; LAMP2 and TAZ) gender was taken into account for the calculation of the allele numbers. This calculation of variant burden on an allelic level, allows us to adjust for multiple variants in one patient and to compare with databases such as GnomAD. In short, an allele is defined as one (of two) versions of a DNA sequence at a given genomic location (National Human Genome Research Institute). As humans have paired chromosomes, and thus two copies of each gene, for most genes, two alleles are present. For genes located on the X chromosome, the number of alleles depends according to sex, two alleles are present in women whereas only one in men. Next to correcting for the number of alleles per gene, the calculation of variant burden on an allelic level also allows us to account for multiple variants on different genes in one individual.
Cascade testing and segregation analysis
For all three cohorts, cascade screening for the presence of a class 4 or 5 variant was performed in first degree relatives. If a VUS was identified, family members were invited for genetical counselling with clinical and/or molecular segregation analysis where appropriate.
Statistical analysis
Continuous variables are expressed as mean ± SD or median and range in case of skewed distribution.
Frequencies are expressed as numbers and percentages. Unpaired T-test was used for comparisons of continuous variables with normal distribution. Chi-square test was used for comparisons of categorical variables between cohorts. All analyses were performed using SPSS Statistics version 28 (IBM Corporation). A p-value of < 0.05 was considered statistically significant.
Results
Characteristics of the 3 patient cohorts
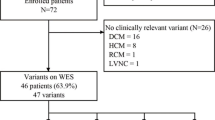
From the 129 screened patients with CTRCD, 46 patients fulfilled the in- and exclusion criteria and agreed to genetic testing. Patient characteristics of the three cohorts are shown in Table 1.
Patients in the CTRCD cohort were predominantly female (65.2%). LVEF at time of CTRCD diagnosis was 30.1% (± 11.0) which represented a decrease of 26.6% (± 9.9) from baseline. Patients in the DCM cohort were matched for age (53 ± 14 years), gender (65.2% female) and presence of a positive family history for DCM (8/46). Mean LVEF at time of DCM diagnosis was 30.7 ± 10.5%. Presence of cardiovascular risk factors was similar as in the CTRCD group. A smaller proportion of DCM patients showed partial (rise in LVEF > 10%, but LVEF remained < 50%) or complete (LVEF > 50%) recovery after initiation of heart failure therapy compared to CTRCD patients (41.3 and 37% respectively).
Patients in the negative control cohort were age and sex -matched to the CTRCD and DCM cohort (mean age 57 ± 15 years, 56.8% female).
As shown in Table 2, CTRCD patients had been treated for lymphoma (52.2%) and/or breast cancer (43.5%) and total anthracycline dose averaged 300 mg/m2 doxorubicin equivalents (range 112.5-540.0 mg/m2). Most patients (73.9%) presented with late (median time of 7 years between AC treatment and diagnosis) and severe CTRCD (LVEF < 40%). During follow-up, 78.3% of patients showed recovery of LVEF after initiation of heart failure treatment (partial recovery in 41.3% and complete (defined as LVEF > 50%) in 37.0%). One patient received a heart transplantation and one patient died during follow-up (non-cardiovascular mortality).
Diagnostic yield of genetic testing in CTRCD
As shown in Fig. 1A, 29 patients (63%) in the CTRCD cohort carried either a VUS (n = 26; 56.5%) and/or a likely pathogenic variant (n = 3; 6.5%). The latter were all truncating variant in TTN (TTNtv).
Overview of genetic yield in each cohort. Genetic yield of a 59-gene cardiomyopathy panel in a cohort of patients with DCM, CTRCD and a negative control cohort. A Total yield in each cohort, including TTN missense variants, a significant difference is present between control patients and DCM patients (p < 0.001) and CTRCD patients (p = 0.018). B Total yield in each cohort, without TTN missense variants, a significant difference is present between control patients and DCM patients (p < 0.001) and CTRCD patients (p = 0.017). C Prevalence of VUS in each cohort, without TTN missense variants, a significant difference is present between control patients and DCM patients (p < 0.001) and between DCM and CTRCD patients (p = 0.036), but not between CTRCD patients and controls (p = 0.111). D Prevalence of (likely) pathogenic variants in each cohort, a significant difference is present between control patients and DCM patients (p < 0.001) and CTRCD patients (p = 0.007). CTRCD: Cancer Therapy related cardiac dysfunction; DCM: dilated cardiomyopathy; VUS: variant of uncertain significance. *,**,*** respectively p < 0.05, 0.01,0.001
In total, 50 variants were identified fulfilling the filtering criteria (Supplementary Table 2). Thirteen individuals harboured more than one variant (28.3%): seven patients with two variants; four patients with three variants and two patients with four variants.
When comparing variant-harbouring individuals and non-variant-harbouring individuals, no significant differences were observed in demographic, clinical and echocardiographic data. When patients were divided in severe versus moderate CTRCD (LVEF < 40% vs 40-49%) no significant differences in variant burden yield were identified. Patients with early (< 1y after treatment) onset of CTRCD (n = 12) more frequently harboured a variant (10; 83.3%) than patients with late onset (n = 19/34; 55.9%; p = 0.090). In one individual with early onset a likely pathogenic variant was identified (8.3%) compared to two individuals with the late onset (5.7%, p = 0.768).
When looking at the extremes of the spectrum, those three patients who carried a TTNtv did have a similar LVEF after AC (ranging from 9-45%) compared to patients without any variant (range 9–48%) and patients with a VUS only (13-48%).
Patients who carried more than one variant were not significantly worse affected than patients with only one or no variant. LVEF after AC treatment averaged 30.9 ± 10.12% in patients with more than one variant vs 29.8 ± 12.1% with only one variant and 30.6 ± 10.8% in patients without a variant (p = 0.408). There was no difference in recovery of LVEF after heart failure treatment either (LVEF 45.9. ± 9.9% vs 48.2 ± 10.1% vs 45.7 ± 10.5% in patients with more than one, only one or no variant respectively (p = 0.918)).
Comparison with DCM cohort
In DCM, 34/46 patients carried a VUS and/or a (likely) pathogenic variant (73.9%), a burden that is similar to that of the CTRCD cohort (63% p = 0.262) (Fig. 1A). A (likely) pathogenic variant could be identified in 6 individuals (7 variants). A complete overview of all variants identified in the DCM cohort is provided in Supplementary Table 2.
As one patient can carry more than one variant, we next compared the variant burden on an allelic level instead of an individual level. The genetic burden in the CTRCD cohort on an allelic level was significantly lower than in the DCM cohort (0.0094 vs 0.0140; p = 0.023).
Comparison with negative control cohort
In the negative control cohort, 47 patients (42.3%) carried a variant which is significantly less than the CTRCD cohort (p = 0.018) and DCM cohort (p < 0.001). No pathogenic variants were identified in the negative control cohort patients (Fig. 1D). A total of 68 variants were present in the negative control cohort, resulting in a genetic burden in the TAAD cohort on an allelic level of 0.0073 which was significantly lower than in the DCM cohort (p < 0.001) but not the CTRCD cohort (p = 0.175).
TTN missense variants and TTNtv
Of the 47 VUS identified in the CTRCD cohort, 19 were TTN missense variants. Since the role of TTN missense variants in cardiac disease is still under debate, we assessed the yield of genetic testing without inclusion of TTN missense variants. After exclusion of the TTN missense variants, 19 (41.3%) CTRCD patients were identified with a VUS or likely pathogenic variant, compared to 27 (58.7%) DCM patients (p = 0.095) and 25 (22.5%) patients of the negative control cohort (p = 0.017; Fig. 1B). However, variants in TTN, including TTN missense variants were more prevalent in both DCM (71.7%; p < 0.001) and CTRCD patients (47.8%, p = 0.023) compared to the negative control cohort (28.8%). On an allelic level, omitting TTN missense variants resulted in a variant burden of 0.0039 in the negative control cohort, compared to 0.0058 in CTRCD patients (p = 0.092) and 0.0080 in DCM patients (p < 0.001).
As TTNtv were the only (likely) pathogenic variants within the CTRCD cohort, we assessed the difference in variant burden between CTRCD and DCM patient, without taking TTNtv and TTN missense variants into account. Only 34.8% of CTRCDC patients carried a non-TTN variant compared to 58.7% of DCM patients (p = 0.022), illustrating the importance of TTN variants in this population.
Variant characteristics: prevalence and predictive scores
We compared the prevalence of all identified variants in a general population (GnomAD v2.1.1). The VUS in the negative control cohort were significantly more frequent in the GnomAD database compared to the VUS in the CTRCD and DCM cohort (Fig. 2). For all VUS the Combined Annotation Dependent Depletion (CADD) score was obtained. The CADD scores predict the deleteriousness of variants based on a combination of prediction scores and information on conservation, and a higher score means the variant is less likely to be benign [20, 21]. The VUS in the negative control cohort had significantly lower CADD scores than the VUS in the CTRCD and DCM cohort (Fig. 2).
Frequency of the variants in GnomAD and raw CADD scores according to patient cohort. A For each specific VUS identified in our three cohorts, the frequency in the GnomAD population database was checked. The variants in the negative control cohort were significantly more frequent in GnomAD than those in the DCM and CTRCD patient cohorts. B For each specific variant identified in our three cohorts, the raw CADD-score was checked. The variants in the negative control cohort had significantly lower CADD scores than those in the DCM and CTRCD patient cohorts. The median of variants of each cohort are shown, the box displays the interquartile distance and whiskers display the minimal and maximal frequency. CADD: Combined Annotation Dependent Depletion; CTRCD: cancer therapy-related cardiac dysfunction; DCM: dilated cardiomyopathy; VUS: variant of uncertain significance
Definitive DCM genes
The initial analysis included a broad panel of 59 genes linked to both arrhythmogenic cardiomyopathy, DCM and hypertrophic cardiomyopathy. However, CTRCD most typically presents as cardiomyopathy with reduced LVEF, similar to DCM. We therefore repeated the analysis, only considering variants in genes classified as definitive DCM-gene (BAG3, DES, FLNC, LMNA, MYH7, PLN, RBM20, SCN5A, TNNC1, TNNT2, TTN) and genes with strong (DSP) or moderate evidence of involvement in DCM (ACTC1, ACTN2, JPH2, NEXN, TNNI3, TPM1, VCL) [22]. Genetic yield in these 19 genes in the different cohorts is displayed in Table 3. Overall, differences between the three groups were similar when the 19 selected genes or the whole 59 CM panel were considered.
When looking at individual genes, an increased burden of FLNC variants was observed in DCM patients compared to the negative control cohort (21.7% vs 2.7%; p < 0.001) and the CTRCD cohort (4.3%; p = 0.013).
Impact of genetic diagnosis on family members and further approach
Three patients with CTRCD carried a likely pathogenic TTNtv. Twelve family members were screened, of whom eight (66.7%) were variant carriers. All the variant harbouring family members were asymptomatic at the time of genetic diagnosis. Genotype positive family members were on average 50 years old (± 18). Further cardiac evaluation identified mild left ventricular dysfunction in one patient (LVEF 47%). In comparison, in the DCM population sixteen family members from five different families of patients with (likely) pathogenic variants were screened. Eleven of them carried the familial variant of whom three family members with TTNtv (average age: 46 year ± 20 year). In the DCM families, three patients had a DCM phenotype (27.3% of genotype positive family members), of whom two were symptomatic at time of diagnosis.
In three of the sixteen CTRCD patients carrying a VUS combined clinical and genetic cascade screening was performed. Six family members were tested of whom two carried the variant. Both family members were asymptomatic and had normal cardiac function at the time of genetic diagnosis. In the DCM cohort, fourteen family members from six families were screened and five were variant carriers. Only one of these genotype positive family members had a cardiac phenotype.
Discussion
In this single centre retrospective analysis we were able to identify a significantly higher burden of cardiomyopathy-related genetic variants in adult patients with AC-induced CTRCD, compared to a negative control population.
Recently, several reports have hinted at a role for structural cardiac variants in the development of CTRCD following AC, describing selected cases of CTRCD patients with identified genetic variants.
Firstly, Linschoten et. al. described two cases of severe symptomatic CTRCD (LVEF decline to < 20%) after AC therapy, who were both harbouring a truncating variant in TTN [6]. Thereafter, other case series and case reports described selected CTRCD patients with a severe evolution or the presence of a positive family history of DCM in whom pathogenic variants in TTN, MYH7 and TNNT2 were identified [5, 7,8,9].
Garcia-Pavia and colleagues described the genetic burden in a larger CTRCD population, the comparison of the diagnostic yield of genetic testing between CTRCD and dilated cardiomyopathy remains elusive. In the present work we showed that diagnostic yield of genetic testing does not differ significantly between DCM and CTRCD patients but differs significantly compared to a negative control cohort.
All (likely) pathogenic variants in the CTRCD cohort were truncating variants in TTN (TTNtv), which were absent from the negative control cohort. Prevalence was 6.5% in our CTRCD cohort which is higher than the prevalence of TTNtv in the general population, described before (0.5-3%) [10, 13]. The increased prevalence of TTNtv in our CTRCD patients is in line with the data of Garcia-Pavia and colleagues who described a prevalence of 7.5% [10]. TTNtv are a common cause of dilated cardiomyopathy (DCM), occurring in approximately 25% of familial DCM [13]. In our DCM cohort in this study the prevalence of TTNtv was 6.5%. Previous work from our group showed TTNtv in 26% of patients who received a heart transplant due to non-ischemic DCM [23]. TTNtv are also predisposing for peripartum cardiomyopathy and alcoholic cardiomyopathy, two acquired forms of DCM [24, 25]. These findings support the 'second-hit theory' in (acquired forms of) DCM, stating that an external trigger might be required to reveal TTNtv effects. CTRCD is now comprehensively approached as systolic dysfunction (based on LVEF or global longitudinal strain) or signs of damage (based on cardiac troponins or (NT-pro)BNP) [2]. In the past however, only severe systolic dysfunction, often combined with dilatation of the left ventricle, was recognized as cardiotoxicity due to anthracyclines, and this was generally seen as a form of acquired dilated cardiomyopathy, hence the comparison with a ‘possibly genetic’ DCM cohort in the current work [26].
Knowledge on which genes could be useful for screening in this population is still lacking. Analysis with a more selective panel of 19 DCM-associated genes showed comparable results to the analysis with the broader 59 gene panel. When looking at specific single genes, variants in FLNC were overrepresented in the DCM cohort compared to the negative control and CTRCD cohort. It is likely that FLNC variants have a higher overall penetrance and are less dependent on environmental factors to develop an overt phenotype. In contrast, variants in TTN showed a similar prevalence in CTRCD and DCM groups but were significantly enriched compared to the negative control group. This highlights the importance of 'second hits' in the setting of TTNtv. We cannot exclude that CTRCD patients with a TTNtv variant would have developed a DCM phenotype, even when not treated with anthracycline chemotherapy. Nonetheless, these results show that an underlying genetic predisposition is present in some CTRCD patients and that genetic screening in patient with CTRCD is warranted. CTRCD patients with an underlying variant had a tendency to earlier presentation than CTRCD patients without an underlying variant, but no difference in disease severity. The earlier presentation with an DCM phenotype, might be explained by a built-up of risk factors and strain on the heart throughout life, thereby passing a critical threshold and leading to a cardiac phenotype. Whereas patients without a variant might need more exposure to additional risk factors, even after exposure to AC, patients with a variant will reach this threshold sooner and could therefore present earlier.
Therapy-related risk factors increasing risk for CTRCD include concomitant treatment with radiotherapy (of the left chest) and/or trastuzumab. One could hypothesize that such ‘traditional’ risk factors are more frequent in patients without a genetic variant presenting with CTRCD. However, the current study was not powered to assess these differences.
In the setting of a ‘second-hit’ on a genetic vulnerable background, variants of unknown significance, may play a role as well. The assessment of prevalence of variants of uncertain significance (VUS) and TTN missense variants in CTRCD in our study are novel.
Whether the current findings should lead to implementation of genetic screening before the start of AC in all patients, remains to be investigated. Ideally, a prospective study should be performed, assessing whether genetic screening, and subsequent adaptation of chemotherapeutic regimen, adapted follow-up and/or implementation of preventive measures, lead to improved outcomes in patients with a reduction of CTRCD and an increase in quality of life for patients. Possible measurements in high risk patients related to genetic susceptibility, can include the reduction of AC dose in genetic susceptible patients or a change in dosing regimen (with longer continuous administration) or the use of liposomal AC [1]. Additionally, follow-up can be adapted to be more regular and to include more modalities (including more frequent biomarker and/or echocardiographic assessment). Lastly, these patients at increased risk might be eligible for preventive treatment, with either classic heart-failure treatment, such as beta-blockade or inhibition of the renin-angiotensin-aldosterone axis, or with the only FDA- and EMA- approved, but expensive, preventive drug dexrazoxane [1].
Lastly, we performed (limited) cascade screening in family members of CTRCD patients harbouring a (likely) pathogenic variant. Despite the small sample size, we were able to identify eight family members at risk, of whom one had a decreased LVEF. The average age at time of genetic screening was 50 years and as a DCM phenotype can develop beyond this age, further follow-up of these family members is needed. Early identification of family members at risk allows for early diagnosis and initiation of treatment, before symptoms develop, which leads to better outcomes overall. This highlights the importance of genetic diagnosis in historical CTRCD patients.
The design and clinical use of a combined clinical, genetic and polygenetic risk score (taking both rare variants and more frequent single nucleotide polymorphisms into account) to stratify individuals before the start of AC treatment, seems feasible as this has been done in other cardiovascular diseases [27]. Of note, several studies have shown variation in genes with a role in the metabolism or transport of AC in patients with CTRCD [28, 29]. Both rare variants and single nucleotide polymorphisms seem to affect the pharmacogenomic CTRCD risk. For example, a large GWAS analysis revealed PRDM2, a transcription factor involved in repair of double strand DNA-breaks and oxidative stress, as a susceptible locus for LVEF decline after AC [30]. Some groups have even tried to include some of these pharmacogenomic risk factors in risk prediction scores [31,32,33,34]. This information is an additional piece to the unsolved puzzle of CTRCD but was outside the scope of the current work.
Some limitations of the current work should be addressed. Firstly, we did not include a cohort of patients with a prior history of cancer treated with anthracyclines who did not develop CTRCD. Although it is unlikely that a group of patients with cancer and the absence of cardiac disease would have a higher burden of variants in cardiomyopathy-related genes than the diverse control cohorts used in the current manuscript we cannot exclude this with certainty. Second, longitudinal follow-up was not performed systematically, and future development of cardiac dysfunction is not assessed. Overall, the current cohort is a rather small cohort, limiting the possibility for additional analyses on the influence of modifiers and additional risk factors.
Conclusion
In patients with CTRCD an increased burden of genetic variants in cardiomyopathy genes is observed, similar to that of DCM patients. Variant harbouring status did not impact the severity of CTRCD, nor the rate of recovery after cessation of chemotherapy and start of heart failure treatment. But patients with a variant more frequently presented with early (< 1 year) CTRCD.
Since a definite genetic diagnosis can be made for a clinically important number of patients, with important consequences on familial screening, genetic testing should be considered in patients presenting with CTRCD.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AC:
-
Anthracyclines
- ACMG:
-
American College of Medical Genetics and Genomics
- CM:
-
Cardiomyopathy
- CTRCD:
-
Cancer therapy-related cardiac dysfunction
- DCM:
-
Dilated cardiomyopathy
- ESC:
-
European Society of Cardiology
- ESMO:
-
European Society for Medical Oncology
- GEN ± :
-
Genotype positive/negative
- LVEF:
-
Left Ventricular Ejection Fraction
- TAAD:
-
Thoracic Aorta Aneurysmatic Disease
- TTNtv:
-
Truncating variants in Titin gene
- VUS:
-
Variant of Unknown Significance
References
McGowan JV, Chung R, Maulik A, Piotrowska I, Walker JM, Yellon DM. Anthracycline chemotherapy and cardiotoxicity. Cardiovasc Drugs Ther. 2017;31(1):63–75.
Lyon AR, López-Fernández T, Couch LS, Asteggiano R, Aznar MC, Bergler-Klein J, et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS): developed by the task force on cardio-oncology of the European Society of Cardiology (ESC). Eur J. 2022;43(41):4229–361.
Herrmann J, Lerman A, Sandhu NP, Villarraga HR, Mulvagh SL, Kohli M. Evaluation and management of patients with heart disease and cancer: cardio-oncology. Mayo Clin Proc. 2014;89(9):1287–306.
Lyon AR, Dent S, Stanway S, Earl H, Brezden-Masley C, Cohen-Solal A, et al. Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies: a position statement and new risk assessment tools from the Cardio-Oncology Study Group of the Heart Failure Association of the European Society of Cardiology in collaboration with the International Cardio-Oncology Society. Eur J Heart Fail. 2020;22(11):1945–60.
Moghadasi S, Fijn R, Beeres S, Bikker H, Jongbloed JDH, Josephus Jitta D, et al. Case series, chemotherapy-induced cardiomyopathy: mind the family history! Eur Heart J Case Rep. 2021;5(10):ytab333.
Linschoten M, Teske AJ, Baas AF, Vink A, Dooijes D, Baars HF, Asselbergs FW. Truncating Titin (TTN) Variants in Chemotherapy-Induced Cardiomyopathy. J Cardiac Fail. 2017;23(6):476–9.
van den Berg MP, van Spaendonck-Zwarts KY, van Veldhuisen DJ, Gietema JA, Postma A, van Tintelen JP. Familial dilated cardiomyopathy: another risk factor for anthracycline-induced cardiotoxicity? Eur J Heart Fail. 2010;12(12):1297–9.
Shipman KE, Arnold I. Case of epirubicin-induced cardiomyopathy in familial cardiomyopathy. J Clin Oncol. 2011;29(18):e537–8.
Wasielewski M, van Spaendonck-Zwarts KY, Westerink ND, Jongbloed JD, Postma A, Gietema JA, et al. Potential genetic predisposition for anthracycline-associated cardiomyopathy in families with dilated cardiomyopathy. Open Heart. 2014;1(1):e000116.
Garcia-Pavia P, Kim Y, Restrepo-Cordoba MA, Lunde IG, Wakimoto H, Smith AM, et al. Genetic variants associated with cancer therapy-induced cardiomyopathy. Circulation. 2019;140(1):31–41.
Franssen C, González MA. The role of titin and extracellular matrix remodelling in heart failure with preserved ejection fraction. Neth Heart J. 2016;24(4):259–67.
Wilcox JE, Hershberger RE. Genetic cardiomyopathies. Curr Opin Cardiol. 2018;33(3):354–62.
Herman DS, Lam L, Taylor MRG, Wang L, Teekakirikul P, Christodoulou D, et al. Truncations of titin causing dilated cardiomyopathy. N Engl J Med. 2012;366(7):619–28.
Zamorano JL, Lancellotti P, Rodriguez Muñoz D, Aboyans V, Asteggiano R, Galderisi M, et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines. Eur J Heart Fail. 2017;19(1):9–42.
Elliott P, Andersson B, Arbustini E, Bilinska Z, Cecchi F, Charron P, et al. Classification of the cardiomyopathies: a position statement from the european society of cardiology working group on myocardial and pericardial diseases. Eur Heart J. 2007;29(2):270–6.
Rickham PP. Human experimentation.Ccode of ethics of the world medical association. Declaration of Helsinki. Br Med J. 1964;2(5402):177.
Proost D, Saenen J, Vandeweyer G, Rotthier A, Alaerts M, Van Craenenbroeck EM, et al. Targeted next-generation sequencing of 51 genes involved in primary electrical disease. J Mol Diagn. 2017;19(3):445–59.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405–24.
Luyckx I, Kumar AA, Reyniers E, Dekeyser E, Vanderstraeten K, Vandeweyer G, et al. Copy number variation analysis in bicuspid aortic valve-related aortopathy identifies TBX20 as a contributing gene. Eur J Hum Genet. 2019;27(7):1033–43.
Kircher M, Witten DM, Jain P, O’Roak BJ, Cooper GM, Shendure J. A general framework for estimating the relative pathogenicity of human genetic variants. Nat Genet. 2014;46(3):310–5.
Rentzsch P, Witten D, Cooper GM, Shendure J, Kircher M. CADD: predicting the deleteriousness of variants throughout the human genome. Nucleic Acids Res. 2019;47(D1):D886–94.
Jordan E, Peterson L, Ai T, Asatryan B, Bronicki L, Brown E, et al. Evidence-based assessment of genes in dilated cardiomyopathy. Circulation. 2021;144(1):7–19.
Boen HM, Loeys BL, Alaerts M, Saenen JB, Goovaerts I, Van Laer L, et al. Diagnostic yield of genetic testing in heart transplant recipients with prior cardiomyopathy. J Heart Lung Transplant. 2022;41(9):1218-27.
Ware JS, Amor-Salamanca A, Tayal U, Govind R, Serrano I, Salazar-Mendiguchía J, et al. Genetic Etiology for Alcohol-Induced Cardiac Toxicity. J Am Coll Cardiol. 2018;71(20):2293–302.
van Spaendonck-Zwarts KY, Posafalvi A, van den Berg MP, Hilfiker-Kleiner D, Bollen IAE, Sliwa K, et al. Titin gene mutations are common in families with both peripartum cardiomyopathy and dilated cardiomyopathy. Euro Heart J. 2014;35(32):2165–73.
Heymans S, Lakdawala NK, Tschöpe C, Klingel K. Dilated cardiomyopathy: causes, mechanisms, and current and future treatment approaches. Lancet. 2023;402(10406):998–1011.
Harper AR, Goel A, Grace C, Thomson KL, Petersen SE, Xu X, et al. Common genetic variants and modifiable risk factors underpin hypertrophic cardiomyopathy susceptibility and expressivity. Nat Genet. 2021;53(2):135–42.
Bhatia S. Genetics of anthracycline cardiomyopathy in cancer survivors. JACC CardioOncol. 2020;2(4):539–52.
Ding Y, Du K, Niu Y-J, Wang Y, Xu X. Genetic susceptibility and mechanisms underlying the pathogenesis of anthracycline-associated cardiotoxicity. Oxid Med Cell Longev. 2022;2022:5818612.
Wells QS, Veatch OJ, Fessel JP, Joon AY, Levinson RT, Mosley JD, et al. Genome-wide association and pathway analysis of left ventricular function after anthracycline exposure in adults. Pharmacogenet Genomics. 2017;27(7):247–54.
Armenian SH, Ding Y, Mills G, Sun C, Venkataraman K, Wong FL, et al. Genetic susceptibility to anthracycline-related congestive heart failure in survivors of haematopoietic cell transplantation. Br J Haematol. 2013;163(2):205–13.
Chaix MA, Parmar N, Kinnear C, Lafreniere-Roula M, Akinrinade O, Yao R, et al. Machine learning identifies clinical and genetic factors associated with anthracycline cardiotoxicity in pediatric cancer survivors. JACC CardioOncol. 2020;2(5):690–706.
Visscher H, Ross CJ, Rassekh SR, Barhdadi A, Dubé MP, Al-Saloos H, et al. Pharmacogenomic prediction of anthracycline-induced cardiotoxicity in children. J Clin Oncol. 2012;30(13):1422–8.
Wang X, Chen Y, Hageman L, Singh P, Landier W, Blanco JG, et al. Risk prediction of anthracycline-related cardiomyopathy (AC) in childhood cancer survivors (CCS): a COG-ALTE03N1 and CCSS report. J Clin Oncol. 2019;37(15_suppl):10015.
Acknowledgements
Not applicable.
Funding
This work was supported by the Flanders Research Foundation- FWO (research grant G055821N, doctoral research grant 1192420N to HMB and senior clinical investigator grant 1804320N to EMVC) and by the Belgian Foundation against Cancer (research grant C/2020/1374 and clinical mandate grant to CF 2021/1594). BL holds a consolidator grant from the European Research Council (Genomia – ERC-COG-2017-771945).
Author information
Authors and Affiliations
Contributions
H.M.B: Patient inclusion, aided in study design, Acquisition, analysis and interpretation of the data; first draft of the manuscript. M.A.: Conceptualisation, study design, interpretation of the data, revision of the manuscript. I.G.: Acquisition of the data, revision of the manuscript. C.F.: Patient inclusion, acquisition of the data, revision of the manuscript. J.B.S.: Acquisition and interpretation of the data, revision of the manuscript. CF: Patient inclusion, revision of the manuscript. A.V: Patient inclusion, revision of the manuscript. T.V.: Patient inclusion, revision of the manuscript. H.H. Conceptualisation, revision of the manuscript. L.VL: Conceptualisation, study design, analysis and interpretation of the data, revision of the manuscript. B.L: Conceptualisation, study design, interpretation of the data, revision of the manuscript. E.M.VC.: Conceptualisation, study design, interpretation of the data, second draft of the manuscript. All authors read and approved the final manuscript.
Authors’ information
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective study was approved by the local Ethics Committee of the University Hospital Antwerp (reference number:20/02/009). Written informed Consent was obtained from all included patients.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
Overview of genes included in panel. Supplementary Table 2. Overview and classification of all variants identified in the CTRCD and DCM patient cohorts.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Boen, H.M., Alaerts, M., Goovaerts, I. et al. Variants in structural cardiac genes in patients with cancer therapy-related cardiac dysfunction after anthracycline chemotherapy: a case control study. Cardio-Oncology 10, 26 (2024). https://doi.org/10.1186/s40959-024-00231-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40959-024-00231-3