Abstract
Background
Mediastinal gray zone lymphoma is a newly recognized rare B cell neoplasm, which is challenging in diagnosis and treatment.
Case presentation
In the current study, we aimed to report a 25-year-old pregnant woman at 25 weeks of gestation who presented with chronic cough and progressive shortness of breath, hypotension, tachycardia, and tachypnea. A large circumferential pericardial effusion with compressive effect on the right atrium and right ventricle and a large extracardiac mass with external pressure to mediastinal structures were seen on trans thoracic echocardiography. The emergency pericardiocentesis was performed with the diagnosis of cardiac tamponade. Also, CMR revealed a huge heterogeneous anterior mediastinal mass, and the pathology and the immunohistochemistry of the mass biopsy revealed gray zone lymphoma with positive CD3, CD20, CD30, CD45, PAX5, and negative CD15 expression. Three courses of chemotherapy with the CHOP regimen were performed with an acceptable response every three weeks before delivery. A caesarian section was performed at 37 weeks without any problem for the patient and fetus, and chemotherapy will be started three weeks after delivery.
Conclusion
Cardiac tamponade as an emergency condition occurred in this pregnant patient by malignant pericardial effusion and mediastinal mass pressure. Accurate diagnosis and on time interventions caused a significant improvement and a successful delivery.
Similar content being viewed by others
Background
Mediastinal gray zone lymphoma was described as a “missing link” with intermediate features between the classic Hodgkin's lymphoma and mediastinal large B cell lymphoma in 2005. Overlap in immunophenotype, histopathology, and clinical features complicates definitive diagnosis and treatment [1]. Lymphoma is the fourth most frequent malignancy in pregnancy, occurring in 1 out of 6000 deliveries. Limitations in the usage of imaging modalities to staging the tumor and choosing the appropriate treatment options during pregnancy have always been a challenge for physicians [2]. Here we introduce a pregnant patient presenting to the hospital with cardiac tamponade caused by an anterior mediastinal mass with morphologic and IHC staining of gray zone lymphoma.
Case presentation
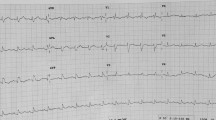
A 25-year-old primigravida female was admitted at 25 weeks of gestation with severe dyspnea that had progressed over the last month. Additionaly, she noticed a progressive, productive cough that started six months ago. At presentation, she had a regular pulse rate of 140 beats per minute, a Blood Pressure of 90/50 mmHg, and a respiratory rate of 30 breaths/min. O2 saturation was 94% in the room air, and she was afebrile. Cardiac examinations revealed muffled heart sounds, pulsus paradoxus, and elevated jugular venous pressure. Other examinations and her past medical history were unremarkable, and she denied experiencing any constitutional sign. Her electrocardiogram showed sinus tachycardia. On echocardiography, the size and the systolic function of the right and left ventricles were normal. There was evidence of a large pericardial effusion with significant right atrial invagination and RVOT diastolic collapse. There were significant respiratory variations of TV and MV inflow velocities, and IVC appeared plethoric. A large extra-cardiac mass at the pulmonary valve site adjacent to distal RVOT was seen, resulting in turbulency in pulmonic outflow without significant gradient and stenosis.
The blood tests showed neutrophilic leukocytosis with a white blood cell count of 16,410 cells/mm3, a hemoglobin level of 9.2 g/dl, a platelet count of 403*103 /mm3, an ESR level of 95 mm/h, an LDH level of 300 IU/L, and CRP more than 90 with standard coagulation test. The results of the pericardial fluid analysis are presented in the Table 1.
Cardiac magnetic resonance determined a 146*126*136 mm heterogeneous mass in the anterior mediastinum attached to the pericardium with a compressive effect on RVOT Fig. 1.
Cardiac magnetic resonance A Short axis T1-W sequence view shows iso-signal tumor. B, C Short axis and axial SSFP sequence views reveal heterogeneous high signal tumor. D Short axis STIR sequence view demonstrates high signal tumor. E Coronal Late Gadolinium Enhancement (LGE) shows heterogeneous enhancement and necrosis (arrow). SSFP = steady-state free precession, STIR = Short tau inversion recovery)
A mass biopsy was performed, and the pathology revealed diffuse and nodular infiltration of lymphocytes, neutrophils, eosinophils, and atypical cells with enlarged hyperchromatic nuclei with irregular contours and prominent nucleoli in the fibrotic stroma. The immunohistochemistry showed negative CD15 and positive CD3, CD20, CD30, CD45, PAX5 expression. According to the clinical and paraclinical findings, the diagnosis of gray zone lymphoma was confirmed Fig. 2.
Mediastinal mass pathology A, B Microscopic examination (H&E staining) shows diffuse and nodular infiltration of lymphocytes, neutrophils, eosinophils and some large atypical cells with enlarged hyperchromatic nuclei with irregular contour and prominent nucleoli in fibrotic stroma. C All lymphoid cells including some large atypical cells are positive for CD45. D Many large atypical cells are positive for CD20. E Many small lymphocytes are positive for CD3. F Large atypical cells are negative for CD15. G Large atypical cells are positive for CD30. H Large atypical cells are strongly positive for PAX5)
Subcutaneous Pericardiocentesis under fluoroscopy with a subxiphoid approach was performed, and after drainage of 200CC serous fluid, the pigtail catheter was fixed under negative pressure. While the patient's hemodynamic status improved, it did not fully recover until receiving the high dose of dexamethasone.
An oncology consultation was requested, and dexamethasone was started at 40 mg daily for four days. Three courses of chemotherapy were administered using the CHOP regimen (Cyclophosphamide 750/m2, Hydroxydaunorubicin 50/m2, Vincristine Sulfate 2 mg, and Prednisone 75 mg/m2 day1-day5) with intervals of twenty-one days. The treatment was stopped three weeks before delivery to avoid the coincidence of the next date of chemotherapy with delivery and prevent any potential complications for the mother and fetus, such as bleeding during childbirth and neonatal myelosuppression [3]. The patient demonstrated an improvement in the symptoms that prompted her admission, indicating a suitable response to chemotherapy. All the fetal ultrasounds performed during chemotherapy were normal. After completing two courses of chemotherapy and giving birth, the mother underwent trans-thoracic echocardiography to monitor her cardiac health. The result showed normal LV and RV function, as well as normal LVEF, with no presence of pericardial effusion.
An elective cesarean section was performed at 37 weeks of gestation. The mother's health status during and after delivery was good, and her son was in perfect health with no observable abnormalities. Chemotherapy will commence three weeks after delivery.
Discussion
Cardiac involvement, which can occur as a secondary complication of malignancies or as a result of chemotherapy agents or radiation therapy, represents a significant challenge in cancer treatment. The pericardium can be affected in the form of pericarditis or pericardial effusion by local invasion, obstruction of lymphatic and venous drainage, and hematogenous or lymphatic spread during malignancies. Lung, breast, leukemia, and lymphoma are the most common neoplasms with malignant pericardial effusion [4]. Cardiac tamponade is a life-threatening medical emergency that requires immediate intervention. The compression of heart chambers through tamponade is caused by fluid, gas, or extracardiac mass effect and leads to decreased cardiac output and shock [5].
The term "Gray zone lymphoma" was first used to delineate the border cases between classic Hodgkin's and non-Hodgkin's lymphoma in 1998; then, in 2008, included in the WHO classification of lymphoid neoplasm as an "unclassifiable B-cell lymphoma, with features intermediate between diffuse large B-cell lymphoma and classical Hodgkin lymphoma" and finally in 2022 WHO named this entity as Mediastinal Gray Zone lymphoma (MGZL) [6,7,8]. Overlap in immunophenotype, histopathology, and clinical features complicates definitive diagnosis and treatment. CD45, CD20, PAX5, BOB1, CD79a, OCT2 expression, and the absence of CD15 expression are common immunohistochemical findings in MGZL. Strong expression of CD20 and PAX5 as B cell associated markers, frequently not seen in CHL. CD45 expression is highly specific for DLBCL and reported in 100% of non-Hodgkin's lymphoma. CD15 expression is positive in 75–90% of CHL cases, and CD30 is more expressed in CHL than DLBCL. Differences in therapeutic regimen and lower survival rate compared to CHL and DLBCL demonstrate the importance of identifying MGZL to find an appropriate treatment for this neoplasm [9].
Physiologic changes in pregnancy can imitate or hide the cancer symptoms and lead to a delay in diagnosis. Cancer staging and treatment are also challenging in pregnancy because of the risk that threatens the mother and fetus [10]. Currently, the R-CHOP regimen is the prefered treatment for gray zone lymphoma [11]. chemotherapy without Rituximab was started for the patient because the evidence showed CHOP regimen is safe beyond the first trimester [12]. It is recommended to schedule the delivery of pregnant cancer patients between 37 and 39 weeks of gestation, with vaginal delivery being the optimal mode of childbirth [13]. Although the preferred mode of delivery was explained to the patient, she refused to consider a vaginal birth. She insisted on cesarean birth, which was ultimately performed at 37 weeks and six days of gestation.
Conclusions
Cardiac tamponade is an emergency condition that needs immediate pericardiocentesis. Tamponade occurred in this patient by mediastinal mass pressure and malignant pericardial effusion. The simultaneous occurrence of cardiac tamponade and mediastinal gray zone lymphoma, a rare neoplasm in pregnancy, creates a complex condition for patient and physicians.
Availability of data and materials
The authors can confirm that all relevant data are included in the article.
Abbreviations
- RVOT:
-
Right ventricular outflow tract
- TV:
-
Tricuspid valve
- MV:
-
Mitral valve
- IVC:
-
Inferior vena cava
- CMR:
-
Cardiac magnetic resonance
- R-CHOP:
-
Rituximab + (Cyclophosphamide, Hydroxydaunorubicin, vincristine sulfate, and Prednisone)
- CHL:
-
Classic Hodgkin’s lymphoma
- DLBCL:
-
Diffuse large B cell lymphoma
References
Traverse-Glehen A, Pittaluga S, Gaulard P, Sorbara L, Alonso MA, Raffeld M, et al. Mediastinal gray zone lymphoma: the missing link between classic Hodgkin’s lymphoma and mediastinal large B-cell lymphoma. Am J Surg Pathol. 2005;29(11):1411–21.
Pereg D, Koren G, Lishner M. The treatment of Hodgkin’s and non-Hodgkin’s lymphoma in pregnancy. Haematologica. 2007;92(9):1230–7.
Boulay R, Podczaski E. Ovarian cancer complicating pregnancy. Obstet Gynecol Clin North Am. 1998;25(2):385–99.
Adler AC, Cestero C. Symptomatic pericardial effusion in Hodgkin’s lymphoma: a rare occurrence. Case report and review of the literature. Tumori. 2012;98(2):50e–2e.
Spodick DH. Acute cardiac tamponade. N Engl J Med. 2003;349(7):684–90.
Rüdiger T, Jaffe E, Delsol G, deWolf-Peeters C, Gascoyne R, Georgii A, et al. Workshop report on Hodgkin’s disease and related diseases (‘grey zone’lymphoma). Ann Oncol. 1998;9:s31–8.
Alaggio R, Amador C, Anagnostopoulos I, Attygalle AD, Araujo IBdO, Berti E, et al. The 5th edition of the World Health Organization classification of haematolymphoid tumours: lymphoid neoplasms. Leukemia. 2022;36(7):1720–48.
Campo E, Swerdlow SH, Harris NL, Pileri S, Stein H, Jaffe ES. The 2008 WHO classification of lymphoid neoplasms and beyond: evolving concepts and practical applications. Blood. 2011;117(19):5019–32.
Bhargava R, Dabbs D. Diagnostic Immunohistochemistry. 5th ed. Pennsylvania: Elsevier; 2019. p. 187.
Botha MH, Rajaram S, Karunaratne K. Cancer in pregnancy. Int J Gynecol Obstet. 2018;143:137–42.
Simon Z, Virga B, Pinczés L, Méhes G, Miltényi Z, Barna S, et al. Transition Between Diffuse Large B-Cell Lymphoma and Classical Hodgkin Lymphoma–Our Histopathological and Clinical Experience With Patients With Intermediate Lymphoma. Pathol Oncol Res. 2021:47.
Lishner M, Avivi I, Apperley JF, Dierickx D, Evens AM, Fumagalli M, et al. Hematologic malignancies in pregnancy: management guidelines from an international consensus meeting. J Clin Oncol. 2016;34(5):501–8.
Van Calsteren K, Amant F. Cancer during pregnancy. Acta Obstet Gynecol Scand. 2014;93(5):443–6.
Acknowledgements
Non to report.
Funding
Non to report.
Author information
Authors and Affiliations
Contributions
AA and ND: critical revision and major contributor in writing the manuscript. KR: acquisition of data by performing the oncologic treatment. MH and FK: acquisition of data by performing the histological examinations. HP: acquisition of data by performing the radiologic examinations. MM: acquisition of data by performing the echocardiographic examinations. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study protocol was approved by Rajaie Cardiovascular, Medical and Research Center ethics committee.
Consent for publication
Consent for publication obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Alizadehasl, A., Roudini, K., Hesami, M. et al. Mediastinal gray zone lymphoma in a pregnant woman presenting with cardiac tamponade. Cardio-Oncology 9, 27 (2023). https://doi.org/10.1186/s40959-023-00173-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40959-023-00173-2