Abstract
Background
Cancer chemotherapy using anthracyclines is associated with cardiotoxicity (CTX), and left ventricular ejection fraction (LVEF) analysis is not sensitive to early cardiotoxic changes. Left ventricular global longitudinal strain (LV GLS) monitoring helps screen subclinical CTX; however, the intervals at which it should be performed remain unclear. We aimed to evaluate the incidence of CTX in women with breast cancer and the associated factors and compare two echocardiographic monitoring strategies using two cutoff points for LV GLS variation.
Methods
Patients with breast cancer prescribed doxorubicin underwent serial LVEF and LV GLS assessments using two-dimensional echocardiography every 3 weeks for 6 months.
Results
We included 43 women; none developed a clinical CTX. Considering a relative reduction of LV GLS > 15%, subclinical CTX was present in 12 (27.9%) and six (14%) patients at 3-week and 3-month intervals, respectively (P = 0.28). Additionally, considering a reduction of > 12%, subclinical CTX was present in 17 (39.5%) and 10 (23.3%) patients (P = 0.16), respectively. There were no significant differences in either reference value at 3-week (P = 0.19) and 3-month intervals (P = 0.41). Age ≥ 60 years (P = 0.018) and hypertension (HTN) (P = 0.022) were associated with subclinical CTX in the univariate analysis.
Conclusions
There was no difference in the incidence of subclinical CTX between the two cutoff points and no benefit in performing echocardiography every 3 weeks compared with quarterly monitoring. Advanced age and HTN were associated with the development of subclinical CTX.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
The number of cancer patients undergoing chemotherapy has increased, which has enabled the identification of several adverse effects of antineoplastic medications, such as cardiotoxicity (CTX) [1]. Typical CTX is characterized by left ventricular dysfunction secondary to the use of anthracyclines, a common class of drugs used in the treatment of breast cancer, acute leukemia, and lymphoma [1,2,3]. This condition influences the prognosis of patients undergoing chemotherapy; hence, it can lead to delayed or interrupted treatment, with an unfavorable impact on the morbidity and mortality of cancer patients [4].
Anthracyclines increase the release of reactive oxygen species, change iron metabolism, and inhibit the enzyme topoisomerase 2ß, thus causing mitochondrial dysfunction and impairment of DNA repair, replication and transcription; therefore, culminating in cardiomyocyte death [2, 3]. Traditionally, CTX is monitored by the serial measurement of left ventricular ejection fraction (LVEF) using transthoracic echocardiography (TTE) [5,6,7]. However, this parameter is not very sensitive, and changes are detected only in a more advanced phase of CTX when myocardial damage has already occurred [8,9,10].
Early diagnosis of CTX at the subclinical stage is one of the main challenges for cardio-oncologists [11]; nevertheless, early cardioprotective therapy has been suggested to prevent and/or attenuate the deleterious effects of chemotherapy [9, 12,13,14,15,16]. Thus, serial TTE with myocardial deformation (strain) assessment using speckle tracking echocardiography has emerged as a useful method for CTX assessment in a preclinical phase. It is a safe, relatively simple, radiation-free method that helps to identify patients at higher risk for ventricular dysfunction. Reduced left ventricular global longitudinal strain (LV GLS) values are associated with the occurrence of CTX [8,9,10, 17, 18].
There is still no consensus regarding the optimal frequency of echocardiographic assessment in patients undergoing chemotherapy and the cutoff points for LV GLS reduction to detect CTX [10].. Therefore, this study aimed to evaluate CTX in women with breast cancer undergoing anthracycline treatment by analyzing the incidence of CTX; comparing two cutoff points for serial LV GLS assessment and two echocardiographic strategies to monitor CTX over the initial 6 months of treatment; and identifying clinical factors associated with the occurrence of CTX.
Methods
Study design and inclusion and exclusion criteria
This was an observational, longitudinal prospective study conducted among adult women with breast cancer without a history of previous cancer treatment who underwent treatment with doxorubicin at Hospital das Clínicas of the Federal University of Goiás (Hospital das Clínicas da Universidade Federal de Goiás - HC/UFG), Goiânia, GO, Brazil. The research project was approved by the Research Ethics Committee of the institution under the substantiated opinion n. 3,281,003, in accordance with the attributions defined in resolution 466/2012 of the Brazilian National Health Council. All participants provided written informed consent.
The inclusion criteria were: female sex, age ≥ 18 years, presence of breast cancer, no history of chemotherapy and radiotherapy and therapeutic planning for the use of doxorubicin. In contrast, the exclusion criteria were as follows: the presence of heart disease at baseline clinical evaluation (heart failure, coronary artery disease, congenital heart disease, cardiomyopathies, stage 3 hypertension (HTN) and clinically significant arrhythmias), echocardiographic changes (LVEF < 50%, moderately severe or severe valvular diseases, and segmental contractility changes) and inadequate acoustic window for TTE.
Study procedures
The data were collected from April 2019 to June 2021. The patients’ demographic, clinical, and physical examination data were collected at the initial appointment. Eligible patients were referred for baseline TTE. The study protocol consisted of TTE complemented with LV GLS assessment before starting chemotherapy (baseline) and at 3-week intervals, coinciding with the cycles of doxorubicin administration (60 mg/m2/cycle). The tests were preferably performed within 48 h after chemotherapy. Each patient underwent a maximum of nine tests over the 6-month follow-up period.
TTE was performed at the department of echocardiography of HC/UFG by an experienced professional using a Philips CX50, Affiniti, or Epic CVx (Philips, Amsterdam, The Netherlands) device equipped with a 2.5–3.5 MHz multifrequency transducer. The images were obtained in multiple planes according to criteria established by the American Society of Echocardiography (ASE) [19]. All available conventional echocardiographic modalities were used to analyze structural and functional cardiac changes. All measurements and the echocardiographic evaluation of the chambers followed the recommendations of the ASE and the European Association of Cardiovascular Imaging (EACVI) [20].
LVEF was calculated using the modified Simpson’s rule. The endocardial border of the left ventricle was traced in apical two- and four-chamber planes at the end of diastole and systole to estimate cavity volumes. The left ventricle was divided into several disks along its longitudinal axis using these tracings, and the final volume was obtained by adding the volumes of the disks. LVEF was obtained by calculating the ratio between ejected (difference between diastolic and systolic volumes) and diastolic volumes [20].
LV GLS images were acquired in apical two-, three-, and four-chamber planes with the optimal electrocardiographic signal amplitude at 40–70 frames/s. The images of three consecutive cardiac cycle beats were digitally stored and analyzed using the Philips Qlab13® automated Cardiac Motion Quantification (aCMQ) software (Philips, Amsterdam, The Netherlands). LV GLS was measured according to consensus recommendations of the EACVI, ASE, and industry representatives [21].
Clinical CTX was defined as an LVEF reduction of 10% or more to values below 50% at any time during the assessment compared with baseline echocardiogram values. Subclinical CTX was defined in two ways: (1) a relative decrease of LV GLS greater than 15% at any time of the assessment and (2) a relative decrease of LV GLS greater than 12% at any time of the assessment, both compared with baseline values. These cutoff points were established based on the recommendations of the ASE, EACVI [5], and Brazilian Society of Cardiology (Sociedade Brasileira de Cardiologia - SBC) [22].
Statistical analysis
The SPSS software version 25.0 (IBM, Armonk, NY, USA) was used for all statistical analyses. Initially, the normality and homogeneity of the variables LVEF and LV GLS were tested using the Shapiro–Wilk and Levene’s tests, respectively. Since the data showed normality and homogeneity, the one-way parametric analysis of variance test with repeated measures was used to compare the scheme every 3-weeks and 3-months. A P value < 0.05 was considered statistically significant.
After identifying subclinical CTX, the Chi-Square or Fisher’s test was used to compare 3-week and 3-month intervals considering both LV GLS cutoff points. A similar strategy was used to compare the 12 and 15% reference values in each regimen. In these analyses, a P value < 0.05 was considered significant.
Univariate Cox regression analysis followed by multivariate analysis was used to verify predisposing factors for CTX (hypertension, diabetes, dyslipidemia, smoking, age, body mass index, total anthracycline dose and use of trastuzumab). The significance level was set at P < 0.05.
Results
Participants
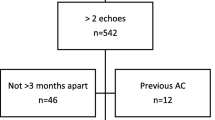
Initially, the study included 54 female patients. Of these, 11 were excluded (Fig. 1). Thus, data of 43 women aged between 34 and 73 years were included in the analysis (Table 1). All patients had an adequate echocardiographic window to calculate LVEF and LV GLS over the follow-up period.
Clinical cardiotoxicity
No patient had clinical CTX. The comparison of absolute LVEF values at baseline (64,53%), three (64,84%), and 6 months (64,19%) showed no significant differences (P = 0.63). A similar result was observed when comparing all evaluated times (P = 0.41) (Fig. 2).
Subclinical cardiotoxicity
The comparison of all absolute LV GLS values every 3 weeks showed no significant difference (P = 0.40) (Fig. 3). In contrast, the comparison of absolute LV GLS values at baseline (− 22,7%), three (− 22,2%), and 6 months (− 21,1%) showed a significant difference (P < 0.001), with the absolute value at 6 months being lower than that at baseline (P < 0.001) and at 3 months (P < 0.001). No significant differences were observed between baseline and 3-month values (P = 0.22) (Table 2).
Analysis with a cutoff point of the percentage LV GLS variation of > 15% showed that 12 (27.9%) and six (14%) patients had subclinical CTX at 3-week and 3-month intervals, respectively. However, the comparison of the two regimens showed no statistically significant difference (P = 0.28). After applying a cutoff point of > 12%, 17 (39.5%) and 10 (23.3%) patients had subclinical CTX at 3 weeks and 3 months, respectively. In addition, the comparison of these values showed no significant differences (P = 0.16) (Figs. 4 and 5).
Central Illustration. Comparison of the two echocardiographic strategies for detecting subclinical cardiotoxicity. Although the absolute numbers of patients with subclinical cardiotoxicity are greater at 3-week intervals for both LV GLS variation cutoff values, the differences are not statistically significant (> 12% vs. > 15%, P = 0.16 vs. P = 0.28). Within both intervals, the numbers were not significantly different at both cutoff values (P = 0.19 vs. P = 0.41). Thus, quarterly monitoring of LV GLS may be the most appropriate echocardiographic strategy
Finally, comparing the number of patients with subclinical CTX using both reference values demonstrated no statistically significant differences in either the 3-week (P = 0.19) or the 3-month (P = 0.41) regimen. Considering these results, the Cox regression analysis considered only data from the 3-month interval regimen and a relative LV GLS decrease of > 12%. Univariate analysis revealed that age ≥ 60 years and HTN are associated with subclinical CTX. However, these associations were not confirmed in multivariate analysis (Table 3).
Discussion
In this study, none of the 43 patients undergoing chemotherapy with doxorubicin developed clinical CTX. Although, we have identified some cases of subclinical CTX with both the cutoff points utilized (LV GLS relative reduction > 15 and > 12%). Advanced age and HTN were associated with the occurrence of subclinical CTX in univariate analysis.
Ventricular dysfunction and heart failure (HF) risks vary according to the cumulative dose of doxorubicin administered, ranging from 3 to 5% to 18–48% with doses of 400 mg/m2 and 700 mg/m2, respectively [23]. A study conducted among 2625 patients undergoing treatment with anthracyclines showed that the incidence rate of CTX was 9% during a mean follow-up period of 5.2 years. The cumulative dose of doxorubicin was 359 (± 172) mg/m2 in the group with CTX and 299 (± 144) mg/m2 in the group without CTX (P < 0.001) [24].
An extensive systematic review that analyzed data from 18 studies and included approximately 23,000 patients treated with anthracyclines reported an incidence rate of 17.9% for ventricular dysfunction and 6.3% for clinical HF during a mean follow-up period of 9 years. The cumulative dose of anthracyclines was consistently reported across studies as an accurate and robust predictor of CTX [25].
We identified no cases of clinical CTX, which may be due to the short follow-up period (patients were followed up for 6 months after starting chemotherapy) and/or low cumulative dose of doxorubicin administered (248.4 ± 30.9 mg/m2). However, there were cases of subclinical CTX (the incidence rate was 14–39.5%, depending on the criterion used).
According to the ASE and EACVI Expert Consensus for Multimodality Imaging Evaluation of Adult Patients During and After Cancer Therapy, it was suggested that a relative reduction of LV GLS > 15% (compared with baseline) is a diagnostic criterion for subclinical CTX [5]. In an Italian study analyzing strain as a guide for cardioprotective therapy in 116 patients with breast cancer, 19.8% of patients developed subclinical CTX (LV GLS reduction > 15% during a 3-month follow-up period). The prevention of clinical HF development could result from patients completing their chemotherapy after administering cardioprotective drugs (ramipril and carvedilol) [26].
The 1-year follow-up analysis of the Strain Surveillance of Chemotherapy for Improving Cardiovascular Outcomes (SUCCOUR) study has been recently published. This was the first randomized clinical trial comparing a serial analysis (every 3 months) of LV GLS vs LVEF to monitor cardioprotective therapy. Overall, 331 patients undergoing doxorubicin treatment (mean dose of 218 mg/m2) were analyzed. LV GLS reduction ≥12% at any time (compared with baseline) was considered an indicator of subclinical CTX. The incidence rate of subclinical CTX was 29% in the LV GLS group, whereas clinical CTX was 13.7% in the LVEF-guided group [27]. The study failed to meet the primary endpoint after the 1-year follow-up period, with no statistically significant difference in LVEF over the period evaluated (− 3.0% in the LVEF-guided group and − 2.7% in the LV GLS-guided group, P = 0.69). Cases of hospitalization for HF were rare (one in each group) [27]. Patients in the LV GLS group were prescribed cardioprotective therapy twice as often as those in the LVEF group. The detection of subclinical CTX resulted in interrupted cancer treatment in five patients in the LV GLS group) and two patients in the LVEF group) [27]. In addition to the higher risk of exposure to side effects and costs associated with cardiological treatment, patients in the LV GLS group had a higher risk of unfavorable cancer progression when chemotherapy was interrupted. Moreover, there were no differences in LVEF and LV GLS at the end of the 1-year follow-up period [27]. Therefore, in the absence of definitive evidence, the LV GLS should be used judiciously in the clinical follow-up of cancer patients [28]. Based on this study, the SBC adopted LV GLS change > 12% as a recommendation in the recently published Brazilian Positioning on the Use of Multimodality Imaging in Cardio-Oncology – 2021 [22]. In this study, the incidence rate of subclinical CTX observed was similar to that found in the literature. The comparison of the two LV GLS cutoffs showed no differences in the occurrence of subclinical CTX.
A systematic review and meta-analysis published in 2014 analyzed the role of myocardial strain in the early detection of CTX during and after chemotherapy. This study evaluated 1504 patients and reported that a LV GLS reduction between 10 and 15% during chemotherapy appeared to be the most useful parameter to predict the future occurrence of CTX [17]. Additionally, a systematic review and meta-analysis published by Oikonomou et al. [1] analyzed the role of LV GLS as a predictor of CTX. This analysis showed that the nine studies evaluating the percentage LV GLS variation had cutoff points that ranged from 2.3 to 15.9% (mean, 13.7%), with a sensitivity of 45 to 100% (mean, 86%) and specificity of 65 to 95% (mean, 79%) [18]. However, due to the heterogeneity of the studies analyzed and the possible existence of publication bias (limited description of the population analyzed and lack of adjustment for relevant risk factors), the meta-analysis concluded that more robust prospective studies should be conducted to define the ideal cutoff point [18].
There is still no consensus in the literature on the best cutoff point for the percentage variation of LV GLS as a predictor of CTX. This study revealed no differences in the incidence of subclinical CTX with both cutoff points, probably due to the small sample size. There were no differences in the occurrence of subclinical CTX between the two-time intervals used.
Gripp et al. analyzed the role of LV GLS as a predictor of CTX in 49 patients with breast cancer undergoing chemotherapy and identified two cases of reduced LVEF in the third month of follow-up and another three in the sixth month. The authors suggested that if the LV GLS had been analyzed after each cycle of chemotherapy (3-week interval) rather than every 3 months (routine procedure), the change in strain would have probably occurred before the decrease in LVEF. Therefore, they recommend performing echocardiography after each cycle of chemotherapy [29], which does not corroborate the findings in this study.
To the best of our knowledge, no study has directly compared the two-time intervals for monitoring subclinical CTX. Despite the limitations of sample size and the short follow-up period, more frequent monitoring does not seem to benefit the diagnosis of CTX and is associated with increased costs.
In this study, advanced age and HTN were associated with the occurrence of subclinical CTX in univariate analysis. Similarly, a systematic review and meta-analysis by Lotrionte et al. showed that in addition to the cumulative anthracycline dose, extremes of age, HTN, diabetes mellitus, extremes of weight, radiotherapy, African-American ethnicity and severe comorbidities were predictors of anthracycline-induced CTX [25].
Henry et al. observed that 4.2% of 16,456 patients with breast cancer undergoing chemotherapy developed CTX. HTN was associated with the occurrence of CTX (relative risk, 1.28; 95% confidence interval, 1.09–1.51). In addition, younger individuals (age < 50 years) were less likely to develop CTX than older ones (age ≥ 65 years) [30], thereby corroborating the findings of this study. Therefore, serial LV GLS monitoring is useful for the follow-up of patients undergoing chemotherapy with anthracyclines. Despite the small sample size and being conducted at a single center, the present study indicated that quarterly monitoring was the most appropriate for clinical practice.
Study limitations
Intra-observer agreement was not analyzed. The low incidence of CTX in the analyzed sample was probably a result of the short follow-up period and the low cumulative dose of doxorubicin administered. Larger sample size may increase the impact of the conclusions of this study. The concomitant use of biomarkers and cardiac magnetic resonance imaging would provide additional value to the serial analysis of the strain as a predictor of CTX in suspected cases. High risk patients, specially those with cardiac structural diseases, were excluded from this analysis. This population could be the one that should be most beneficiated of the more frequent monitoring strategy. These observations should be analyzed in future studies to increase knowledge.
Competency in patient care
Monitoring the development of subclinical CTX in patients with breast cancer who undergo treatment with doxorubicin is pivotal to the cardiovascular management of these patients. This study suggests that quarterly monitoring of LV GLS is the most appropriate echocardiographic strategy.
Translational outlook
Further studies with larger sample sizes and extended follow-up periods are required to validate the results of the present study. Early diagnosis and treatment of CTX is necessary for improving the outcomes in female patients with breast cancer undergoing chemotherapy. Serial LV GLS monitoring is useful in this scenario. Defining the optimal cutoff point for the relative variation in the LV GLS (compared with baseline) and ideal frequency of performing serial exams are necessary measures to establish routines, avoid unnecessary expenses, and provide better care to patients with breast cancer.
Conclusions
In this study, no patient developed clinical CTX and had a significantly reduced LVEF. The occurrence of subclinical CTX was revealed by serial measurement of the LV GLS. There was no significant difference in the incidence rates of subclinical CTX between the two LV GLS cutoff points used. More frequent echocardiographic monitoring showed no benefits compared with quarterly monitoring. Advanced age and HTN were associated with the occurrence of subclinical CTX in the analyzed population.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- ASE:
-
American Society of Echocardiography
- CTX:
-
Cardiotoxicity
- EACVI:
-
European Association of Cardiovascular Imaging
- HF:
-
Heart failure
- HTN:
-
Hypertension
- LVEF:
-
Left ventricular ejection fraction
- LV GLS:
-
Left ventricular global longitudinal strain
- SBC:
-
Brazilian Society of Cardiology (Sociedade Brasileira de Cardiologia)
- TTE:
-
Transthoracic echocardiography
References
Clasen SC, Wald JW. Left ventricular dysfunction and chemotherapeutic agents. Curr Cardiol Rep. 2018;20:20. https://doi.org/10.1007/s11886-018-0967-x.
Henriksen PA. Anthracycline cardiotoxicity: an update on mechanisms, monitoring and prevention. Heart. 2018;104:971–7. https://doi.org/10.1136/heartjnl-2017-312103.
Saleh Y, Abdelkarim O, Herzallah K, Abela GS. Anthracycline-induced cardiotoxicity: mechanisms of action, incidence, risk factors, prevention, and treatment. Heart Fail Rev. 2021;26:1159–73. https://doi.org/10.1007/s10741-020-09968-2.
Caro Codón J, Rosillo Rodríguez SO, López Fernández T. Cardiotoxicity from the cardiologist’s perspective. Futur Cardiol. 2015;11:425–32. https://doi.org/10.2217/fca.15.47.
Plana JC, Galderisi M, Barac A, Ewer MS, Ky B, Scherrer-Crosbie M, et al. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2014;27:911–39. https://doi.org/10.1016/j.echo.2014.07.012.
Dobson R, Ghosh AK, Ky B, Marwick T, Stout M, Harkness A, et al. BSE and BCOS Guideline for Transthoracic Echocardiographic Assessment of Adult Cancer Patients Receiving anthracyclines and/or trastuzumab. JACC Cardiooncol. 2021;3:1–16. https://doi.org/10.1016/j.jaccao.2021.01.011.
Zamorano JL, Lancellotti P, Rodriguez Muñoz D, et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: the Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur J Heart Fail. 2017;19:9–42. https://doi.org/10.1002/ejhf.654.
Liu JE, Barac A, Thavendiranathan P, Scherrer-Crosbie M. Strain imaging in cardio-oncology. JACC Cardiooncol. 2020;2:677–89. https://doi.org/10.1016/j.jaccao.2020.10.011.
Makavos G, Ikonomidis I, Palios J, Rigopoulos A, Katogiannis K, Parissis J, et al. Cardiac imaging in cardiotoxicity: a focus on clinical practice. Heart Fail Rev. 2021;26:1175–87. https://doi.org/10.1007/s10741-020-09952-w.
Sanna GD, Canonico ME, Santoro C, Esposito R, Masia SL, Galderisi M, et al. Echocardiographic longitudinal strain analysis in heart failure: real usefulness for clinical management beyond diagnostic value and prognostic correlations? A comprehensive review. Curr Heart Fail Rep. 2021;18:290–303. https://doi.org/10.1007/s11897-021-00530-1.
Bikiewicz A, Banach M, von Haehling S, Maciejewski M, Bielecka-Dabrowa A. Adjuvant breast cancer treatments cardiotoxicity and modern methods of detection and prevention of cardiac complications. ESC Heart Fail. 2021;8:2397–418. https://doi.org/10.1002/ehf2.13365.
Graffagnino J, Kondapalli L, Arora G, Hawi R, Lenneman CG. Strategies to prevent cardiotoxicity. Curr Treat Options in Oncol. 2020;21:32. https://doi.org/10.1007/s11864-020-0722-6.
Kikuchi R, Shah NP, Dent SF. Strategies to prevent cardiovascular toxicity in breast cancer: is it ready for primetime? J Clin Med. 2020;9:896. https://doi.org/10.3390/jcm9040896.
Avila MS, Siqueira SRR, Ferreira SMA, Bocchi EA. Prevention and treatment of chemotherapy-induced cardiotoxicity. Methodist Debakey CardioVasc J. 2019;15:267–73. https://doi.org/10.14797/mdcj-15-4-267.
Bansal N, Adams MJ, Ganatra S, Colan SD, Aggarwal S, Steiner R, et al. Strategies to prevent anthracycline-induced cardiotoxicity in cancer survivors. Cardiooncology. 2019;5:18. https://doi.org/10.1186/s40959-019-0054-5.
Padegimas A, Clasen S, Ky B. Cardioprotective strategies to prevent breast cancer therapy-induced cardiotoxicity. Trends Cardiovasc Med. 2020;30:22–8. https://doi.org/10.1016/j.tcm.2019.01.006.
Thavendiranathan P, Poulin F, Lim KD, Plana JC, Woo A, Marwick TH. Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy: a systematic review. J Am Coll Cardiol. 2014;63:2751–68. https://doi.org/10.1016/j.jacc.2014.01.073.
Oikonomou EK, Kokkinidis DG, Kampaktsis PN, Amir EA, Marwick TH, Gupta D, et al. Assessment of prognostic value of left ventricular global longitudinal strain for early prediction of chemotherapy-induced cardiotoxicity: a systematic review and meta-analysis. JAMA Cardiol. 2019;4:1007–18. https://doi.org/10.1001/jamacardio.2019.2952.
Mitchell C, Rahko PS, Blauwet LA, Canaday B, Finstuen JA, Foster MC, et al. Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2019;32:1–64. https://doi.org/10.1016/j.echo.2018.06.004.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39.e14. https://doi.org/10.1016/j.echo.2014.10.003.
Voigt JU, Pedrizzetti G, Lysyansky P, Marwick TH, Houle H, Baumann R, et al. Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/Ase/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging. 2015;16:1–11. https://doi.org/10.1093/ehjci/jeu184.
Melo MDT, Paiva MG, Santos MVC, Rochitte CE, Moreira VM, Saleh MH, et al. Brazilian position statement on the use of multimodality imaging in cardio-oncology −2021. Posicionamento Brasileiro sobre o uso da Multimodalidade de Imagens na cardio-oncologia −2021. Arq Bras Cardiol. 2021;117:845–909. https://doi.org/10.36660/abc.20200266 Article in English, Portuguese.
Curigliano G, Cardinale D, Dent S, Criscitiello C, Aseyev O, Lenihan D, et al. Cardiotoxicity of anticancer treatments: epidemiology, detection, and management. CA Cancer J Clin. 2016;66:309–25. https://doi.org/10.3322/caac.21341.
Cardinale D, Colombo A, Bacchiani G, Tedeschi I, Meroni CA, Veglia F, et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation. 2015;131:1981–8. https://doi.org/10.1161/CIRCULATIONAHA.114.013777.
Lotrionte M, Biondi-Zoccai G, Abbate A, Lanzetta G, D’Ascenzo F, Malavasi V, et al. Review and meta-analysis of incidence and clinical predictors of anthracycline cardiotoxicity. Am J Cardiol. 2013;112:1980–4. https://doi.org/10.1016/j.amjcard.2013.08.026.
Santoro C, Esposito R, Lembo M, Sorrentino R, De Santo I, Luciano F, et al. Strain-oriented strategy for guiding cardioprotection initiation of breast cancer patients experiencing cardiac dysfunction. Eur Heart J Cardiovasc Imaging. 2019;20:1345–52. https://doi.org/10.1093/ehjci/jez194.
Thavendiranathan P, Negishi T, Somerset E, Negishi K, Penicka M, Lemieux J, et al. Strain-guided management of potentially cardiotoxic cancer therapy. J Am Coll Cardiol. 2021;77:392–401. https://doi.org/10.1016/j.jacc.2020.11.020.
Barberato SH, Hajjar LA. Strain in monitoring cancer therapy-induced cardiotoxicity: where are we after the SUCCOUR study? ARQ Bras Cardiol Imagem CardioVasc. 2021;34:1–3.
Gripp EA, Oliveira GE, Feijó LA, Garcia MI, Xavier SS, Sousa AS. Global longitudinal strain accuracy for cardiotoxicity prediction in a cohort of breast cancer patients during anthracycline and/or trastuzumab treatment. Arq Bras Cardiol. 2018;110:140–50. https://doi.org/10.5935/abc.20180021.
Henry ML, Niu J, Zhang N, Giordano SH, Chavez-MacGregor M. Cardiotoxicity and cardiac monitoring among chemotherapy-treated breast cancer patients. JACC Cardiovasc Imaging. 2018;11:1084–93. https://doi.org/10.1016/j.jcmg.2018.06.005.
Acknowledgements
The authors appreciate the HC/UFG services of Oncology, Breast Cancer, and Echocardiography for their support in conducting this study.
Funding
The study has no external funding sources.
Author information
Authors and Affiliations
Contributions
All authors have participated in the conception, design, analysis, and interpretation of data. Also, they have contributed to the drafting of the manuscript or revising it critically for important intellectual content; and granted final approval of the manuscript submitted. DPSS and JBMS also have done data collection.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research project was approved by the Research Ethics Committee of the institution under the substantiated opinion n. 3,281,003, in accordance with the attributions defined in resolution 466/2012 of the Brazilian National Health Council. All participants signed the informed consent form.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sampaio, D.P.S., Silva, J.B.M., do Carmo Rassi, D. et al. Echocardiographic strategy for early detection of cardiotoxicity of doxorubicin: a prospective observational study. Cardio-Oncology 8, 17 (2022). https://doi.org/10.1186/s40959-022-00143-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40959-022-00143-0