Abstract
Introduction & Background
The aging of the population assures increased prevalence of Individuals Living with Dementia (ILwD) and there will be an increased representation of this cohort requiring physical rehabilitation. If physical therapists (PTs) manage these patients as they do their age-matched, cognitively-intact peers, they will likely be unsuccessful. ILwD have unique needs related to interpersonal and pragmatic components of rehabilitation. Therapeutic nihilism (doubting the benefit of therapy) is well-documented in PTs, either because of existing biases about dementia or previous challenges in working with ILwD. Physical rehabilitation eligibility and placement decisions are often made by PTs without special training in dementia, based upon brief exposure to patients in environments not well-designed for their best functioning. This can lead to underestimation of rehabilitation potential and denial of future PT services. PTs who work with ILwD desire more practical knowledge and targeted skills. Those with more education and training have a more positive attitude and outlook related to ILwD.
Purpose
The purpose of this paper is to introduce a framework for rehabilitation with ILwD equipped with pragmatic ideas to facilitate therapeutic success. The four primary components of the model are: (1) Establish a personal RELATIONSHIP, (2) Use intentional verbal and nonverbal COMMUNICATION, (3) Understand and optimize MOTOR LEARNING capabilities, and (4) Create a safe, purposeful ENVIRONMENT. Specific strategies to help PTs optimize each component are provided with supporting evidence. The model is intended to be dynamic, encouraging PTs to capitalize on the most accessible strategies within their control for a given patient and setting.
Implications
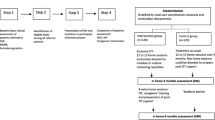
This framework provides a practical resource for working with ILwD with immediate implications for facilitating therapeutic success. The model is displayed in a schematic that reminds the reader of ideas at a glance within the context of each of the components. If an appreciation for this content was among core competencies required among PTs working with ILwD, perhaps there would be significantly fewer patients written off as “uncooperative” or “unable to participate” in PT.
Similar content being viewed by others
Introduction & background
The World Health Organization recognizes dementia as a major cause of disability and dependency, and estimates there are ~ 50 million Individuals Living with Dementia (ILwD) worldwide [1]. The impact of dementia on mobility and gait is complex. Cognitive impairment and falls are interrelated [2] and ILwD fall more and are more likely to be hospitalized from a fall than their cognitively-intact age-matched peers [3,4,5]. Physical therapists (PTs) have much to offer this population, but there are biases and barriers that impact rehabilitation opportunity and success. Therapists who manage ILwD like their cognitively-intact older adult patients will probably be unsuccessful, leading to frustration, underestimation of prognosis, premature discharge, and/or ineffectual care. Therapeutic nihilism (doubting the benefit of therapy), is common in PTs and other healthcare workers [6,7,8,9,10]. Overt negativity, where ILwD are considered void of rehab potential or “unworthy” solely based on a dementia diagnosis has been documented [9, 11]. Healthcare systems also pose challenges and this is true internationally [7, 10, 12,13,14,15]. It is difficult to provide optimal dementia care within a biomedical model or to work within facility/administrative constraints with patients who do not conform easily. Consider Patient Case #1 Part 1 (Table 1).
Experienced PTs recognize the value of specialized training for working with ILwD [13, 15,16,17,18]. Those who work in geriatric residential settings may have more insights into the special needs of ILwD, but they still desire more information, particularly about late stage disease [15, 16]. PTs working in acute care settings, in- and out-patient rehabilitation, community-based, and home care environments may not have anticipated working with ILwD, but are more likely to see these patients as the population ages. In contrast to an older American study which found PTs’ knowledge of AD lacking, [19] a recent Canadian study [12] determined that PTs had knowledge about dementia, but needed more tools and confidence for clinical success, especially in managing advanced cognitive or behavioral issues. Qualitative studies of PTs working with ILwD consistently, regardless of country or practice setting, identify the need for more practical knowledge and targeted skills [6,7,8, 13, 15, 17, 18]. Attitudes about ILwD become increasingly negative as dementia severity increases, [16] and the term “dementia” often evokes an image of severe disease, not the community-dwelling individual with mild or moderate impairment. In a UK study, Bamford et al. [8] describe common categorization of ILwD as “not rehabable” and a tendency to attribute all patient problems to dementia, versus identifying potential contributing issues (e.g., pain, fatigue). An Australian study by Cations et al. [10] identified perceptions of incompatibility between “rehabilitation” and “dementia,” because of a default to a “palliative care” mindset. There is clear need for education to support an accurate, less fatalistic view of dementia, and empower PTs with skills and strategies to enhance rehabilitation efforts. Education related to working with ILwD has been associated with more positive attitudes [12] and more optimistic prognoses for outcome [17] among PTs.
The purpose of this paper is to introduce a framework for rehabilitation success with ILwD and to highlight how understanding the intricacies of these patients can inform and enhance clinical practice. Specific practical strategies, grounded in evidence as available, are divided into four primary components: (1) Establish a personal RELATIONSHIP, (2) Use intentional verbal and nonverbal COMMUNICATION, (3) Understand and optimize MOTOR LEARNING capabilities; and (4) Create a safe, purposeful ENVIRONMENT.
The model
This model (Fig. 1) is offered in response to the need for and benefit of education about working with ILwD. A narrative literature review exploring best practices in rehabilitation, nursing, and allied health professionals led to the four major elements of the model. These four areas are inherently involved in PTs’ interactions with all patients. PTs are movement experts who establish therapeutic relationships and tailor motor learning strategies to the needs of their patients and whose clinical successes routinely rely on modification of communication, interventions, and environments to facilitate optimal patient response. The unique needs of ILwD are considered in this model which provides practical and, in many cases, evidence-based recommendations for therapeutic success.
The therapeutic RELATIONSHIP: establish a personal connection
Person-centeredness is a philosophy of care grounded in a genuine understanding of the individual [20]. In rehabilitation, Clare [21] frames person-centeredness in understanding the unique experiences, values, motivations, strengths, and needs of ILwD. The person, and the relationship with that person, are top priority. Personal information (from documentation or caregivers) can fuel relationship building; however, PTs also need to connect with patients when little or no personal data is available.
Know who and what is uniquely important
Knowing names of important people, places, and things, and having insights into relationships, professions, pastimes, and passions all help to create a picture of the patient. Making relevant conversation with personal references displays prioritization of relationship over task. Personalized interactions (versus generic pleasantries or focus on therapy) can make the person feel “seen” and “known,” important components of effective person-centered care [20, 22]. In the context of rehabilitation, PTs [8, 14, 15], ILwD, and their caregivers [23,24,25] recognize the value of this. Integrating the name of a loved one or a specific hobby in the context of goal setting can be heartening to a confused patient. Consider Patient Case #1 Part 2 (Table 1). As with all strategies presented here, the PT has to “read the room” to assess effect. If using personal information is met with paranoia, the PT needs to redirect conversation and reevaluate use of this tactic.
When there is no access to personal information, other strategies will support a therapeutic relationship. McGilton et al. [26] proposed that reliability (inclusive of trust, protection, and acceptance), empathy (with sensitivity to changing needs), and consistency (predictability) are pivotal to a caregiving relationship. Even in later stages of dementia, meaningful relationships can be established, evidenced by sharing of emotion, affection, and desire for future interaction [27]. PTs should enter relationships with expectations of success.
Reminiscence & empathic curiosity
Reminiscence Therapy (structured use of memories, experiences, and prompts) can have a positive impact on mood and communication/interaction, [28, 29] and sharing memories can allow healthcare providers to better see and know the person with dementia [30]. In rehab, integrating reminiscence concepts can foster the therapeutic relationship and direct functional activities. Consider Patient Case #2 (Table 1). If reminiscence strategies are elusive, the concept of “empathic curiosity” [31] allows interaction in the here and now. Using brief sentences, watching for and responding to emotional cues and metaphors, and sharing responsibility for the interaction can support the therapeutic relationship. Consider Patient Case #1 Part 3 (Table 1).
Recognize & accept the offered reality
There are differing opinions and no strong guidance from research [32, 33] about the value of letting a patient’s reality be THE reality in dementia care. Orientation to the reality of a situation may be appropriate, but quizzing or asking “Do you remember …? ” is rarely productive. Responding to the perceived emotional source of an individual’s statements or behaviors can be validating and helpful, and may be more gentle and productive than a hard to hear truth. Whether lying to a patient should be an option is a complex and controversial determination [34]. Consider Patient Case #3 Part 1 (Table 1). Being flexible is a sound strategy. Perhaps PTs should consider it a privilege to enter the offered reality and do so with grace and humility, rather than feel compelled to force someone back into a world that no longer comforts them.
Learn what brings joy and triggers negativity
Understanding a person’s “good life” helps the PT to frame interventions in an overtly meaningful way. Celebrating success and progress is motivating. Behavioral and psychological symptoms of dementia are impacted by patient, caregiver, and environmental factors [35]. Things that increase patient stress (e.g., acute medical issues, unmet needs [food, hydration, toileting, sleep], lack of meaningful activity, uncomfortable environment) or caregiver stress will have a negative effect on patient behaviors [35]. Saying/doing the “right” thing can endear the PT to a patient; saying/doing the “wrong” thing can bring a session to a screeching halt. ILwD may be surprisingly aware of a care provider’s demeanor, and if they perceive the PT as rushed or distracted (e.g., documenting while treating), this may trigger negative reactions.
Use purposeful COMMUNICATION
Communication tips are abundant on every dementia association/society web page, but empirical research directing best practice is scarce, and very little is known about how ILwD experience communication [36]. Van Manen et al. [37] created a communication model from a scoping literature review, demonstrating the complexity of nursing staff-patient communication in dementia care, many components of which are represented here. Communication is intricately entangled with relationship building, and person-centered care requires a mindset of “working with” rather than “doing to,” [38] which requires the PT to be patient and humble. As with all older adults, assuring that ILwD are equipped with appropriate hearing and vision support will enhance communication efforts.
Verbal “Rules of Engagement”
Research related to communication between care providers and ILwD consistently concludes that use of short, simple phrasing and yes/no options can enhance interactions [39,40,41]. Other potentially useful strategies include: eliminating distractions, repetition and/or paraphrasing, reassurance, and patience (being comfortable with silence). PTs should be careful not to undermine patient capabilities by defaulting immediately to the most basic communication strategies, as those with mild to moderate dementia may have the ability to participate in interactive discussions, follow multi-step commands, or choose from several options.
Excessively slow speech by care providers does not facilitate communication, [39,40,41] and, in fact, “elderspeak” (also called “infantilizing,” where caregiver speaks slowly, with elevated pitch, and terms of endearment) can lead to decreased self-esteem and resistiveness to care [42]. More important than slowing of speech is purposeful pacing, allowing time for processing and response formulation. A confident, friendly voice with deliberate intonation should clearly indicate whether a statement or question is being offered. Attentively and actively listening allows the PT to follow the lead of the person with dementia and be a partner in communication.
Non-verbal “Rules of Engagement”
A measured approach, a genuine smile (sorely missed while hidden behind a mask during the Covid-19 pandemic!), friendly eye contact, and a relaxed demeanor are facilitators to communication. Positioning at eye level (i.e., sit if patient is sitting or supine) can equalize a perceived power dynamic. ILwD may have preserved sensitivity to non-verbal communication and emotional expression of others well into the disease, [41] even as language skills are failing, so sending positive non-verbal messages via face, body language, posture, and movement is essential. Excellent observation of patient non-verbals will help the PT pick up on physical or emotional discomfort that can interfere with therapy.
Recognize behavior as communication
Humans react to the world as they perceive it. Behavior must be evaluated in context, as odd behavior may have a simple explanation: A patient who removes her shirt in the PT gym feels hot! Uncertainty, discomfort, or fear can lead to cantankerous behavior. In post-hip fracture rehabilitation, McGilton et al. [43] studied allied health professionals’ perceptions of behaviors interfering with care in ILwD. Anxiety and irritability were most common, and strategies for management included being calm and reassuring, building relationship, and focusing on individual versus task, but few allied health staff prioritized assessing the reason for the behavior as a component of management [43]. Behavioral issues are common, but not an inevitable sequelae of dementia [44]. When faced with unexpected behaviors, PTs must problem solve! Pain or fear may masquerade as agitation; fatigue or confusion may cause disengagement. Before concluding a patient is “uncooperative” or “non-participatory,” the PT should work to get to the source of obstructive behaviors and try to manage the root problem. Consider Patient Case #4 (Table 1).
Mindful progression of cues
Communicating effectively requires cues to overcome deficits in attention, language, sequencing, and/or judgment [45]. An algorithm of progressive cuing strategies for ADLs introduced by Beck et al. [45] translates to an intuitive progression: Verbal Prompt → Model or Gesture → Physical Prompt → Physical Guidance → Physical Assistance. PTs must determine: [1] the ideal response time before repeating the cue [2]; the minimal amount of cuing that allows the patient to be successful within an activity, and [3] how cuing needs change with task, mood, or time of day. Cuing strategies are pivotal within motor learning and relearning context. In AD in particular, apraxia is not unusual, often presenting clinically as difficulty with imitating gestures, following demonstrations, or mimicking use of tools, [46, 47] so recognizing when these are and are not viable cuing strategies is important.
Be flexible
A toolbox of rapport building and communication strategies and flexibility within and between therapy sessions is advisable. Qualitative studies of PTs experienced in working with ILwD identify themes of “be on your toes” [48] and “think outside the box.” [14] Redirection to benign topics (e.g., the weather, the curtains) or go-to topics (e.g., favorite pet or sports team) may be useful for defusing a situation. Validation of how someone is feeling can create an alliance with an upset patient (e.g., “I know you’re mad. I wish we could start this day over,” “I see you’re upset, let me help”). Communicating to engage and connect supports an authentic therapeutic relationship.
Understand & exploit MOTOR LEARNING strengths
Motor learning literature as it relates to ILwD is limited, but provides some important themes. Rehab focus may be on re-learning skills (e.g., sit to stand, activities of daily living) or may be on skills requiring new learning (e.g., novel use of an assistive device). These strategies can be useful in both contexts.
Prioritize procedural learning
A distinction between procedural/implicit and declarative/explicit memory and learning, and the neural substrates for different types of learning can help direct skill training [49,50,51]. Current motor learning researchers recognize a spectrum versus a dichotomy of implicit and explicit learning, and specific strategies may not be easily categorized as implicit or explicit [52]. For the purposes of this paper, procedural/implicit training is most succinctly understood as “learning by doing,” wherein a motor skill is acquired (or reacquired) using repetitive practice without intentional cognitive oversight. The cerebellum, basal ganglia, and sensorimotor cortical regions all play critical roles in procedural learning [49]. Declarative/explicit learning integrates cognitive strategies with motor practice, such as focused attention and awareness, verbally describing movement, reflecting on performance, and comparing outcome to previous performance. Medial temporal lobe function (hippocampus and adjacent structures) is highly implicated in explicit learning, [49] and these regions are well known to be involved early in AD, rendering these strategies less useful. Research directs prioritization of procedural learning strategies for ILwD, particularly those with AD, with whom this premise has been most studied [49, 50, 53,54,55,56]. Authors have been unable to draw conclusions about relationships between severity of dementia and procedural learning capabilities, [55, 57,58,59] meaning even individuals with moderate to severe dementia should have the opportunity to train motor-based functional tasks with purposeful procedural strategies. PTs should not summarily discount all declarative strategies, especially with individuals with mild dementia, [60, 61] but they must quickly assess usefulness (e.g., Asking someone to self-assess performance on an obstacle course might elicit a meaningful critique or undesirable anxiety).
Consider salience of tasks
Saliency is a relevant component of motor learning for all populations, [62] but even more so for ILwD [8]. Functional relevance may need to be more obvious for ILwD, where lower extremity strengthening is disguised as sit to stand activity drills and balance training is clearly framed within a motivating goal (e.g., “This will make it easier for you to feed your cat, Tabby”). Dutzi et al. [63] demonstrated the capability of rehab participants with mild-moderate dementia to accurately identify functional limitations and set meaningful goals using a structured approach. This reminds PTs not to make assumptions about patients’ insights into their own needs and represents an important integration of person-centered care.
Intentionally design practice sessions: repetitive, consistent, constant, & blocked
Classic work by Dick and colleagues [57,58,59, 64] and literature reviews [50, 53] have been influential in guiding practice structure. Definitions of terminology are included in Table 2. Intentional design of training sessions should include repetitive, consistent, constant (vs. variable), and blocked (vs. random) practice. Massed practice is generally desirable, but fatigue impacts learning, [49, 50] and distributed schedules may be preferred for some patients. Classic motor learning theory favors variable, random practice sessions, which aim to broaden motor programs, preparing learners for real world, unpredictable demands. This requires the learner to have the cognitive wherewithal to: [1] store and later retrieve performance data, [2] evaluate performance on different versions of tasks, and [3] move easily between tasks. ILwD, particularly those with AD, lack the ability to encode, store, and retrieve information. They lack the relational processing (required for variable practice) and the cognitive flexibility to move swiftly between tasks (required for random practice), making constant, blocked practice more effective [57,58,59, 64]. Little is known about optimal feedback type and schedules for ILwD, and processing feedback data may rely too heavily on cognition to be of real use [50]. Some studies suggest visual feedback may be important in motor learning, [50, 65] which highlights the need for appropriate, clean corrective lenses during therapy.
Specificity of training
PTs should strive to create a therapy environment that closely mimics real life. ILwD who learn tasks through constant practice have rigid motor programs that are not easily modified, making specificity of training important for learning/relearning functional tasks [53, 59]. Therapy provided in the living environment (e.g., home care, residential care) has the benefit of being relevant and specific to daily life.
Errorless learning / spaced retrieval / part to whole practice
Errorless learning uses specific strategies (e.g., no guessing, stepwise approach, modeling, vanishing verbal/visual cues, spaced retrieval) [66] to minimize or eliminate errors during training. Avoiding patient-generated motor errors decreases the chance that a faulty movement becomes the default motor strategy. Consistency in error avoidance requires excellent observation and anticipation of movement and a commitment from the entire care team. Errorless learning has been demonstrated superior to “errorful”/trial and error learning for new, non-functional procedural tasks in ILwD [67, 68]. In the context of relearning Instrumental Activities of Daily Living (IADL), including technology use (e.g., phone, computer, appliances), errorless learning is a useful strategy, equivalent [60, 61, 69, 70] or superior [71] to trial and error learning. Spaced retrieval is a formulaic cue fading strategy within errorless learning. The PT increases intervals between cues with correct performance, and immediately corrects performance and decreases cue intervals upon anticipated errors. Spaced retrieval has been effectively used in IADL and functional training in ILwD [72, 73]. Part-whole practice, or deconstructing tasks into component parts, has been effectively used in IADL and sit-to-stand training [60, 74]. Forward chaining (adding next component part upon mastery of preceding step) provides the opportunity to practice parts in relation to one another. Within each treatment session, training culminates with whole task performance. Consider Patient Case #3 Part 2 (Table 1).
Sufficient intensity & challenge of training
A common misconception is that older adults will not tolerate intensive training. Monitoring physiological and cognitive/emotional response to therapy allows PTs to make informed decisions about increasing/decreasing level of intensity and challenge within therapy. Rest breaks should be offered judiciously, when needed, not out of habit between activities. Evidence consistently demonstrates high-intensity exercise is safe and effective for ILwD [75]. Physical activity is neuroprotective and supports neuroplasticity, specifically in brain regions implicated in dementias [76]. PTs can confidently and competently oversee intensive interventions and encourage patients to work hard! Sondell et al. [23] found that feeling challenged by exercises/activities was a positive and rewarding experience, associated with increased confidence and self-esteem in ILwD.
A long recognized enemy to functional independence is “excess disability,” in which ILwD are functionally more disabled than they should be, given their impairments [77]. This is often the result of diminished opportunity for task performance, driven by well-intentioned or time-sensitive caregiver assistance. Loss of opportunity leads to loss of skill. Recovery may be possible with new opportunity, [77, 78] which bodes well for rehabilitation and inspires deliberate education of caregivers to provide task opportunities, while being sensitive to their daily demands.
Attend to ENVIRONMENTAL characteristics
Movement is the product of the person, the task, and the environment. Often, PTs have little environmental control, but being mindful of the therapeutic atmosphere can help to meet the needs of ILwD.
Prioritize patient safety and comfort
A safe, calm, and predictable environment is critical for ILwD, who value a sense of security in rehabilitation [23]. Patients desire physical and emotional safety, but sometimes busy staff prioritize physical safety at the expense of emotional safety and dignity [79]. Exceptional communication and relationship building strategies contribute to emotional safety and security when the physical environment is beyond the therapist’s control.
Attend to consistency and familiarity
When memory is impaired, a sense of routine can be reassuring; even without “remembering,” things may feel familiar and comfortable. Thus, consistency in place, people, and timing of therapy may enhance success. While this has not been empirically studied, experienced rehab professionals highlight the importance of consistency and familiarity within the therapeutic environment [10, 14].
Minimize distractions
Minimizing distractions for ILwD is intuitive. Beck et al. [45] identify “stimulus control” as the initial step in their cuing progression framework, for instance closing the door or repositioning within a room to face away from distracting activity. Noise reduction/regulation has been shown to decrease problematic behaviors in ILwD and has implications for rehabilitation [80, 81]. Any negative sensory experiences (e.g., foul odors, uncomfortable temperature) can potentially impact behavior [82] and impede rehab efforts and therefore should be managed.
Environment to support function / participation
Well-lit environments, natural light when possible, and avoidance of glare are anecdotally recommended. Given the prevalence of visual-spatial and spatial-cognitive impairment in this population, [83, 84] it may be difficult to tease out contributing constraints to motor learning, so enhancing environmental opportunity for success is important. Way-finding cues (e.g., signs/pictures for toilet) may be useful for functional independence, and distracting cues (e.g., camouflage door with mural) may help manage exit seeking behavior [85]. Relevant, patient-preferred ambient music can support positive behaviors [80] and can be easily integrated with rehab efforts.
Atmosphere of joy
While it may seem far-reaching, creating a positive atmosphere and capitalizing on the pleasure that recovery of movement and meaningful activities bring, goes a long way. Patients and families are clear that enjoyment is a priority in exercise and rehabilitation [8, 86, 87]. Being in the moment with a patient, having a laugh, making strides toward an agreed upon therapeutic goal are all cause for celebration!
Discussion & conclusion
Dementia brings the slow demise of memory, function, and identity. In reorienting the focus from what is lost to what abilities remain and potential for gain, PTs create opportunity for rehabilitation success. This framework is intended to help PTs understand some idiosyncrasies of ILwD and exploit strengths and positive characteristics. A “strength-based approach” in dementia care has shown some success [88, 89] and is pivotal to person-centered care. Focusing on “reablement” and “living well” with dementia could reframe services and policies related to rehabilitation [21, 90]. Those with dementia are clear in their desire for others to focus on what they can do, not what they cannot [91, 92].
In post-hip fracture rehabilitation for ILwD, underutilization of rehabilitation and physical therapy services is common, despite evidence of benefit [93,94,95]. Physical rehabilitation eligibility and placement decisions are often made based upon limited exposure, in poorly suited environments, by staff under-trained in the management of this population, leading to underestimation of rehab potential and denial of future PT services [6, 14]. The framework offered here provides a grassroots effort to help enhance dementia care one PT at a time, while still working toward systemic solutions to this problem.
The model is intended to be dynamic and flexible, encouraging PTs to capitalize on parameters that are within their control at any given time. Various levels of dementia and different settings may render some strategies more or less available or effective than others. Relationship and communication are prioritized and interrelated, as communication serves relationship building. Personal information is useful, but when unavailable, excellent communication, conveying empathy and investment can foster connection. Intentional motor learning strategies and practice design should be directed toward salient functional goals, developed in partnership when possible. Environmental strategies may be limited (e.g. close door, turn off television), but recognizing the importance of creating a sense of security and comfort is invaluable. Helping family and other care providers understand some of these strategies can serve to support rehab efforts [8, 14, 15].
This model is offered as a starting point to bring attention to and encourage discussion about best practices for rehabilitation with ILwD. Clinicians who work regularly with ILwD may anecdotally support the model, but it has yet to be formally tested. Evidence is provided to support some, but not all components of the model and as more evidence is available within and beyond the four major sections, this could warrant modifications. This model is in response to the documented need for targeted knowledge and specific skills to support PTs in working with ILwD [6, 13, 15,16,17,18]. If an appreciation for these factors was among core competencies for PTs working with ILwD, perhaps there would be significantly fewer patients written off as “uncooperative” or “unable to participate” in PT.
Availability of data and materials
Not Applicable.
References
World Health Organization. Dementia [Internet]. 2020 [cited 2021 Jun 17]. Available from: https://www.who.int/news-room/fact-sheets/detail/dementia
Montero-Odasso M, Speechley M. Falls in cognitively impaired older adults: implications for risk assessment and prevention. J Am Geriatr Soc. 2018;66(2):367–75. https://doi.org/10.1111/jgs.15219.
Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med Boston. 1988;319(26):1701–7. https://doi.org/10.1056/NEJM198812293192604.
Allan LML, Ballard CGC, Rowan ENE, Kenny RAR. Incidence and prediction of falls in dementia: a prospective study in older people. PLoS One. 2009;4(5):e5521. https://doi.org/10.1371/journal.pone.0005521.
Harvey L, Mitchell R, Brodaty H, Draper B, Close J. The influence of dementia on injury-related hospitalisations and outcomes in older adults. Injury. 2016;47(1):226–34. https://doi.org/10.1016/j.injury.2015.09.021.
Hall AJ, Fullam J, Lang IA, Endacott R, Goodwin VA. Community physiotherapy for people with dementia following hip fracture: fact or fiction? A qualitative study. Dement Lond Engl. 2020;19(8):2750–60. https://doi.org/10.1177/1471301219857027.
Staples WH, Killian CB. Development of an instrument to measure attitudes of physical therapy providers working with people with dementia. Am J Alzheimers Dis Other Dement. 2012;27(5):331–8. https://doi.org/10.1177/1533317512452041.
Bamford C, Wheatley A, Shaw C, Allan LM. Equipping staff with the skills to maximise recovery of people with dementia after an injurious fall. Aging Ment Health. 2019;23(11):1524–32. https://doi.org/10.1080/13607863.2018.1501664.
Goodwin VA, Allan LM. “Mrs Smith has no rehab potential”: does rehabilitation have a role in the management of people with dementia? Age Ageing. 2019;48(1):5–7. https://doi.org/10.1093/ageing/afy152.
Cations M, May N, Crotty M, Low L-F, Clemson L, Whitehead C, et al. Health professional perspectives on rehabilitation for people with dementia. Gerontologist. 2020;60(3):503–12. https://doi.org/10.1093/geront/gnz007.
Digby R, Lee S, Williams A. The ‘unworthy’ patient with dementia in geriatric rehabilitation hospitals. Collegian. 2018;25(4):377–83. https://doi.org/10.1016/j.colegn.2017.10.002.
Hunter SW, Divine A. Understanding the factors influencing physiotherapists’ attitudes towards working with people living with dementia. Physiother Theory Pract. 2020;22:1–8.
Buddingh S, Liang J, Allen J, Koziak A, Buckingham J, Beaupre LA. Rehabilitation for long-term care residents following hip fracture: a survey of reported rehabilitation practices and perceived barriers to delivery of care. J Geriatr Phys Ther. 2013;36(1):39–46. https://doi.org/10.1519/JPT.0b013e3182569b4f.
Hall AJ, Watkins R, Lang IA, Endacott R, Goodwin VA. The experiences of physiotherapists treating people with dementia who fracture their hip. BMC Geriatr. 2017;17(1):91. https://doi.org/10.1186/s12877-017-0474-8.
McCarroll C, Riet C, Halter M. How is the emerging role of domiciliary physiotherapists who treat residents with dementia in nursing homes perceived by allied health professionals? A phenomenological interview study. Health Soc Care Community. 2020;28(1):279–90. https://doi.org/10.1111/hsc.12862.
Staples WH, Killian CB. Education affects attitudes of physical therapy providers toward people with dementia. Educ Gerontol. 2012;38(5):350–61. https://doi.org/10.1080/03601277.2010.544605.
Miles JD, Staples WH, Lee DJ. Attitudes About Cognitive Screening: A Survey of Home Care Physical Therapists. J Geriatr Phys Ther 2001. 2019;42(4):294–303.
McGilton KS, Vellani S, Zheng N, Wang D, Yeung L, Escrig-Pinol A. Healthcare professionals’ perspectives on rehabilitating persons with cognitive impairment. Dement Lond Engl. 2021;20(5):1772–90. https://doi.org/10.1177/1471301220969615.
Lusardi MM, Wong RA. Physical therapists’ understanding of Alzheimer’s disease: implications for education. J Phys Ther Educ. 1994;8(1):18–24. https://doi.org/10.1097/00001416-199401000-00004.
Fazio S, Pace D, Flinner J, Kallmyer B. The Fundamentals of Person-Centered Care for Individuals With Dementia. Gerontologist. 2018;58(suppl_1):S10–9.
Clare L. Rehabilitation for people living with dementia: A practical framework of positive support. PLoS Med. 2017;14(3):e1002245. https://doi.org/10.1371/journal.pmed.1002245.
Maslow K, Fazio S, Ortigara A, Kuhn D, Zeisel J. From concept to practice: training in person-centered Care for People with dementia. Generations. 2013;37(3):100–7.
Sondell A, Lampinen J, Conradsson M, et al. Experiences of community-dwelling older people with dementia participating in a person-centred multidimensional interdisciplinary rehabilitation program. BMC Geriatr. 2021;21(1):341. https://doi.org/10.1186/s12877-021-02282-y.
Benbow SM, Tsaroucha A, Ashley M, Morgan K, Kingston P. Patients’ and carers’ views on dementia workforce skills. J Ment Health Train Educ Pract. 2011;6(4):195–202. https://doi.org/10.1108/17556221111194536.
Hall AJ, Burrows L, Lang IA, Endacott R, Goodwin VA. Are physiotherapists employing person-centred care for people with dementia? An exploratory qualitative study examining the experiences of people with dementia and their carers. BMC Geriatr. 2018;18(1):63. https://doi.org/10.1186/s12877-018-0756-9.
McGilton KS. Enhancing relationships between care providers and residents in long-term care: designing a model of care. J Gerontol Nurs. 2002;28(12):13–21. https://doi.org/10.3928/0098-9134-20021201-05.
Williams CL, Tappen RM. Can we create a therapeutic relationship with nursing home residents in the later stages of Alzheimer’s disease? J Psychosoc Nurs Ment Health Serv. 1999;37(3):28–35. https://doi.org/10.3928/0279-3695-19990301-16.
Woods B, O’Philbin L, Farrell EM, Spector AE, Orrell M. Reminiscence therapy for dementia. Cochrane Database Syst Rev. 2018;3:CD001120.
Park K, Lee S, Yang J, Song T, Hong G-RS. A systematic review and meta-analysis on the effect of reminiscence therapy for people with dementia. Int Psychogeriatr. 2019;31(11):1581–97. https://doi.org/10.1017/S1041610218002168.
Cooney A, Hunter A, Murphy K, Casey D, Devane D, Smyth S, et al. “Seeing me through my memories”: a grounded theory study on using reminiscence with people with dementia living in long-term care. J Clin Nurs John Wiley Sons Inc. 2014;23(23–24):3564–74. https://doi.org/10.1111/jocn.12645.
Mcevoy P, Plant R. Dementia care: using empathic curiosity to establish the common ground that is necessary for meaningful communication. J Psychiatr Ment Health Nurs. 2014;21(6):477–82. https://doi.org/10.1111/jpm.12148.
Woods B, Aguirre E, Spector AE, Orrell M. Cognitive stimulation to improve cognitive functioning in people with dementia. Cochrane Database Syst Rev. 2012;2:CD005562. https://doi.org/10.1002/14651858.CD005562.pub2.
Neal M, Barton WP. Validation therapy for dementia. Cochrane Database Syst Rev. 2003;3:CD001394. https://doi.org/10.1002/14651858.CD001394.
Seaman AT, Stone AM. Little white lies: interrogating the (un) acceptability of deception in the context of dementia. Qual Health Res. 2017;27(1):60–73. https://doi.org/10.1177/1049732315618370.
Kales HC, Gitlin LN, Lyketsos CG. Assessment and management of behavioral and psychological symptoms of dementia. BMJ. 2015;350(mar02 7):h369. https://doi.org/10.1136/bmj.h369.
Alsawy S, Mansell W, McEvoy P, Tai S. What is good communication for people living with dementia? A mixed-methods systematic review. Int Psychogeriatr. 2017;29(11):1785–800. https://doi.org/10.1017/S1041610217001429.
van Manen AS, Aarts S, Metzelthin SF, Verbeek H, Hamers JPH, Zwakhalen SMG. A communication model for nursing staff working in dementia care: results of a scoping review. Int J Nurs Stud. 2021;113:103776. https://doi.org/10.1016/j.ijnurstu.2020.103776.
Bright FAS, Boland P, Rutherford SJ, Kayes NM, McPherson KM. Implementing a client-centred approach in rehabilitation: an autoethnography. Disabil Rehabil. 2012;34(12):997–1004. https://doi.org/10.3109/09638288.2011.629712.
Small JA, Gutman G, Makela S, Hillhouse B. Effectiveness of communication strategies used by caregivers of persons with Alzheimer’s disease during activities of daily living. J Speech Lang Hear Res. 2003;46(2):353–67. https://doi.org/10.1044/1092-4388(2003/028).
Wilson R, Rochon E, Mihailidis A, Leonard C. Examining success of communication strategies used by formal caregivers assisting individuals with Alzheimer’s disease during an activity of daily living. JSLHR. 2012;55(2):328–41. https://doi.org/10.1044/1092-4388(2011/10-0206).
Smith ER, Broughton M, Baker R, Pachana NA, Angwin AJ, Humphreys MS, et al. Memory and communication support in dementia: research-based strategies for caregivers. Int Psychogeriatr. 2011;23(2):256–63. https://doi.org/10.1017/S1041610210001845.
Zhang M, Zhao H, Meng F-P. Elderspeak to resident dementia patients increases Resistiveness to care in health care profession. Inq J Med Care Organ Provis Financ. 2020;57:46958020948668. https://doi.org/10.1177/0046958020948668.
McGilton K, Wells J, Teare G, Davis A, Rochon E, Calabrese S, et al. Rehabilitating patients with dementia who have had a hip fracture: part I: behavioral symptoms that influence care. Top Geriatr Rehabil. 2007;23(2):161–73. https://doi.org/10.1097/01.TGR.0000270185.98402.a6.
Sadak TI, Katon J, Beck C, Cochrane BB, Borson S. Key neuropsychiatric symptoms in common dementias. Res Gerontol Nurs. 2014;7(1):44–52. https://doi.org/10.3928/19404921-20130918-01.
Beck C, Heacock P, Rapp CG, Mercer SO. Assisting cognitively impaired elders with activities of daily living. Am J Alzheimers Care Relat Disord Res. 1993;8(6):11–20. https://doi.org/10.1177/153331759300800602.
Lesourd M, Le Gall D, Baumard J, Croisile B, Jarry C, Osiurak F. Apraxia and Alzheimer’s disease: review and perspectives. Neuropsychol Rev. 2013;23(3):234–56. https://doi.org/10.1007/s11065-013-9235-4.
Farina E, Borgnis F, Pozzo T. Mirror neurons and their relationship with neurodegenerative disorders. J Neurosci Res. 2020;98(6):1070–94. https://doi.org/10.1002/jnr.24579.
Fjellman-Wiklund A, Nordin E, Skelton DA, Lundin-Olsson L. Reach the Person behind the Dementia - Physical Therapists' Reflections and Strategies when Composing Physical Training. PLoS One. 2016;11(12):e0166686. https://doi.org/10.1371/journal.pone.0166686.
Vidoni ED, Boyd LA. Achieving enlightenment: what do we know about the implicit learning system and its interaction with explicit knowledge? J Neurol Phys Ther. 2007;31(3):145–54. https://doi.org/10.1097/NPT.0b013e31814b148e.
van Halteren-van Tilborg IADA, Scherder EJA, Hulstijn W. Motor-skill learning in Alzheimer’s disease: a review with an eye to the clinical practice. Neuropsychol Rev. 2007;17(3):203–12. https://doi.org/10.1007/s11065-007-9030-1.
Roemmich RT, Bastian AJ. Closing the Loop: From Motor Neuroscience to Neurorehabilitation. Annu Rev Neurosci. 2018;41:415–29.
Kleynen M, Braun SM, Bleijlevens MH, Lexis MA, Rasquin SM, Halfens J, et al. Using a Delphi technique to seek consensus regarding definitions, descriptions and classification of terms related to implicit and explicit forms of motor learning. PLoS One. 2014;9(6):e100227. https://doi.org/10.1371/journal.pone.0100227.
Patterson JT, Wessel J. Strategies for retraining functional movement in persons with Alzheimer disease: a review. Physiother Can. 2002;54(4):274–80.
Harrison BE, Son G-R, Kim J, Whall AL. Preserved implicit memory in dementia: a potential model for care. Am J Alzheimers Dis Other Dement. 2007;22(4):286–93. https://doi.org/10.1177/1533317507303761.
De Wit L, Marsiske M, O’Shea D, Kessels RPC, Kurasz AM, DeFeis B, et al. Procedural learning in individuals with amnestic mild cognitive impairment and Alzheimer’s dementia: a systematic review and Meta-analysis. Neuropsychol Rev. 2021;31(1):103–14. https://doi.org/10.1007/s11065-020-09449-1.
Chauvel G, Maquestiaux F, Gemonet E, Hartley A, Didierjean A, Masters R, et al. Intact procedural knowledge in patients with Alzheimer’s disease: evidence from golf putting. J Mot Behav. 2018;50(3):268–74. https://doi.org/10.1080/00222895.2017.1341376.
Dick MB, Shankle RW, Beth RE, Dick-Muehlke C, Cotman CW, Kean ML. Acquisition and long-term retention of a gross motor skill in Alzheimer’s disease patients under constant and varied practice conditions. J Gerontol B Psychol Sci Soc Sci. 1996;51(2):103–11. https://doi.org/10.1093/geronb/51B.2.P103.
Dick MB, Hsieh S, Bricker J, Dick-Muehlke C. Facilitating acquisition and transfer of a continuous motor task in healthy older adults and patients with Alzheimer’s disease. Neuropsychology. 2003;17(2):202–12. https://doi.org/10.1037/0894-4105.17.2.202.
Dick MBM, Hsieh SS, Dick-Muehlke CC, Davis DSD, Cotman CWC. The variability of practice hypothesis in motor learning: does it apply to Alzheimer’s disease? Brain Cogn. 2000;44(3):470–89. https://doi.org/10.1006/brcg.2000.1206.
Bourgeois J, Laye M, Lemaire J, Leone E, Deudon A, Darmon N, et al. Relearning of activities of daily living: a comparison of the effectiveness of three learning methods in patients with dementia of the Alzheimer type. J Nutr Health Aging. 2016;20(1):48–55. https://doi.org/10.1007/s12603-016-0675-4.
van Tilborg IA, Kessels RP, Hulstijn W. How should we teach everyday skills in dementia? A controlled study comparing implicit and explicit training methods. Clin Rehabil. 2011;25(7):638–48. https://doi.org/10.1177/0269215510396738.
Kleim JA, Jones TA. Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. JSLHR. 2008;51(1):S225–39. https://doi.org/10.1044/1092-4388(2008/018).
Dutzi I, Schwenk M, Kirchner M, Bauer JM, Hauer K. “What would you like to achieve?” Goal-Setting in Patients with Dementia in Geriatric Rehabilitation. BMC Geriatr. 2019;19(1):N.PAG.
Dick MB, Nielson KA, Beth RE, Shankle WR, Cotman CW. Acquisition and long-term retention of a fine motor skill in Alzheimer’s disease. Brain Cogn. 1995;29(3):294–306. https://doi.org/10.1006/brcg.1995.1283.
Dick MB, Andel R, Bricker J, Gorospe JB, Hsieh S, Dick-Muehlke C. Dependence on visual feedback during motor skill learning in Alzheimer’s disease. Aging Neuropsychol Cogn. 2001;8(2):120–36. https://doi.org/10.1076/anec.8.2.120.840.
de Werd MME, Boelen D, Rikkert MGMO, Kessels RPC. Errorless learning of everyday tasks in people with dementia. Clin Interv Aging. 2013;8:1177–90. https://doi.org/10.2147/CIA.S46809.
Kessels RPC, Hensken LMGO. Effects of errorless skill learning in people with mild-to-moderate or severe dementia: a randomized controlled pilot study. NeuroRehabilitation. 2009;25(4):307–12. https://doi.org/10.3233/NRE-2009-0529.
Schmitz X, Bier N, Joubert S, Lejeune C, Salmon E, Rouleau I, et al. The benefits of errorless learning for serial reaction time performance in Alzheimer’s disease. JAD. 2014;39(2):287–300. https://doi.org/10.3233/JAD-130887.
Voigt-Radloff S, de Werd MM, Leonhart R, et al. Structured relearning of activities of daily living in dementia: the randomized controlled REDALI-DEM trial on errorless learning. Alzheimers Res Ther. 2017;9(1):22. https://doi.org/10.1186/s13195-017-0247-9.
Kerkhof YJF, Bergsma A, Mangiaracina F, Planting CHM, Graff MJL, Dröes RM. Are people with mild dementia able to (re) learn how to use technology? A literature review. Int Psychogeriatr. 2021;15:1–16. https://doi.org/10.1017/S1041610221000016.
Dechamps A, Fasotti L, Jungheim J, Leone E, Dood E, Allioux A, et al. Effects of different learning methods for instrumental activities of daily living in patients with Alzheimer’s dementia: a pilot study. Am J Alzheimers Dis Other Dement. 2011;26(4):273–81. https://doi.org/10.1177/1533317511404394.
Creighton AS, van der Ploeg ES, O’Connor DW. A literature review of spaced-retrieval interventions: a direct memory intervention for people with dementia. Int Psychogeriatr. 2013;25(11):1743–63. https://doi.org/10.1017/S1041610213001233.
Thivierge S, Jean L, Simard M. A randomized cross-over controlled study on cognitive rehabilitation of instrumental activities of daily living in Alzheimer disease. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psychiatry. 2014;22(11):1188–99. https://doi.org/10.1016/j.jagp.2013.03.008.
Werner C, Wiloth S, Lemke NC, Kronbach F, Jansen C-P, Oster P, et al. People with dementia can learn compensatory movement maneuvers for the sit-to-stand task: a randomized controlled trial. JAD. 2017;60(1):107–20. https://doi.org/10.3233/JAD-170258.
Yeh S-W, Lin L-F, Chen H-C, Huang L-K, Hu C-J, Tam K-W, et al. High-intensity functional exercise in older adults with dementia: a systematic review and meta-analysis. Clin Rehabil. 2021;35(2):169–81. https://doi.org/10.1177/0269215520961637.
Domingos C, Pêgo JM, Santos NC. Effects of physical activity on brain function and structure in older adults: a systematic review. Behav Brain Res. 2021;402:113061. https://doi.org/10.1016/j.bbr.2020.113061.
Brody EM, Kleban MH, Lawton MP, Silverman HA. Excess disabilities of mentally impaired aged: impact of individualized treatment. The Gerontologist. 1971;11(2):124–33. https://doi.org/10.1093/geront/11.2_Part_1.124.
Slaughter SE, Eliasziw M, Morgan D, Drummond N. Incidence and predictors of excess disability in walking among nursing home residents with middle-stage dementia: a prospective cohort study. Int Psychogeriatr. 2011;23(1):54–64. https://doi.org/10.1017/S1041610210000116.
Røsvik J, Rokstad AMM. What are the needs of people with dementia in acute hospital settings, and what interventions are made to meet these needs? A systematic integrative review of the literature. BMC Health Serv Res. 2020;20(1):723. https://doi.org/10.1186/s12913-020-05618-3.
Jensen L, Padilla R. Effectiveness of environment-based interventions that address behavior, perception, and falls in people with Alzheimer’s disease and related major neurocognitive disorders: a systematic review. Am J Occup Ther. 2017;71(5):1–10. https://doi.org/10.5014/ajot.2017.027409.
Marquardt G, Bueter K, Motzek T. Impact of the design of the built environment on people with dementia: an evidence-based review. HERD. 2014;8(1):127–57. https://doi.org/10.1177/193758671400800111.
Van Vracem M, Spruytte N, Declercq A, Van Audenhove C. Agitation in dementia and the role of spatial and sensory interventions: experiences of professional and family caregivers. Scand J Caring Sci. 2016;30(2):281–9. https://doi.org/10.1111/scs.12240.
Arvanitakis Z, Shah RC, Bennett DA. Diagnosis and Management of Dementia: a review. JAMA. 2019;322(16):1589–99. https://doi.org/10.1001/jama.2019.4782.
Agrawal Y, Smith PF, Rosenberg PB. Vestibular impairment, cognitive decline and Alzheimer’s disease: balancing the evidence. Aging Ment Health. 2020;24(5):705–8. https://doi.org/10.1080/13607863.2019.1566813.
Woodbridge R, Sullivan MP, Harding E, Crutch S, Gilhooly KJ, Gilhooly M, et al. Use of the physical environment to support everyday activities for people with dementia: a systematic review. Dement Lond Engl. 2018;17(5):533–72. https://doi.org/10.1177/1471301216648670.
Gonçalves A-C, Cruz J, Marques A, Demain S, Samuel D. Evaluating physical activity in dementia: a systematic review of outcomes to inform the development of a core outcome set. Age Ageing. 2018;47(1):34–41.
Bechard LE, Beaton D, McGilton KS, Tartaglia MC, Black SE. Physical activity perceptions, experiences, and beliefs of older adults with mild cognitive impairment or Alzheimer’s disease and their care partners. Appl Physiol Nutr Metab. 2020;45(11):1216–24. https://doi.org/10.1139/apnm-2019-0730.
Dawson N, Judge KS, Trapuzzano A. Knowledge gains and intent to change practice patterns after the Leveraging Existing Abilities in Dementia (LEAD)™ Training Program. Dement 14713012. 2021 Feb;20(2):814–25.
Dawson N, Gerhart H, Judge KS. Findings from a strength-based moderate-intensity exercise interventions for individuals with dementia (innovative practice). Dement Lond Engl. 2017;1(4):1471301217730951–1273. https://doi.org/10.1177/1471301217730951.
Poulos CJ, Bayer A, Beaupre L, Clare L, Poulos RG, Wang RH, et al. A comprehensive approach to reablement in dementia. Alzheimers Dement N Y N. 2017;3(3):450–8. https://doi.org/10.1016/j.trci.2017.06.005.
Mitchell G, McTurk V, Carter G, Brown-Wilson C. Emphasise capability, not disability: exploring public perceptions, facilitators and barriers to living well with dementia in Northern Ireland. BMC Geriatr. 2020;20(1):525. https://doi.org/10.1186/s12877-020-01933-w.
Laver KE, Crotty M, Low L-F, Clemson L, Whitehead C, McLoughlin J, et al. Rehabilitation for people with dementia: a multi-method study examining knowledge and attitudes. BMC Geriatr. 2020;20(1):531. https://doi.org/10.1186/s12877-020-01940-x.
Seitz DP, Gill SS, Austin PC, Bell CM, Anderson GM, Gruneir A, et al. Rehabilitation of older adults with dementia after hip fracture. J Am Geriatr Soc. 2016;64(1):47–54. https://doi.org/10.1111/jgs.13881.
McGilton KS, Campitelli MA, Bethell J, Guan J, Vellani S, Krassikova A, et al. Impact of Dementia on Patterns of Home Care Following Inpatient Rehabilitation Discharge for Older Adults After Hip Fractures. Arch Phys Med Rehabil [Internet]. 2021;102(10):1972-81. [cited 2021 Jul 15];0(0). Available from: https://www.archives-pmr.org/article/S0003-9993(21)00495-0/fulltext
Mitchell R, Draper B, Brodaty H, Close J, Ting HP, Lystad R, et al. An 11-year review of hip fracture hospitalisations, health outcomes, and predictors of access to in-hospital rehabilitation for adults ≥ 65 years living with and without dementia: a population-based cohort study. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 2020;31(3):465–74. https://doi.org/10.1007/s00198-019-05260-8.
Acknowledgements
This paper is the product of many years of working with individuals with dementia, their loved ones, care providers committed to excellent care, and enthusiastic colleagues and students, all for whom I am very grateful.
Funding
Not Applicable.
Author information
Authors and Affiliations
Contributions
Julie Ries is responsible for conceptualization and writing of this manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not Applicable.
Consent for publication
Not Applicable.
Competing interests
Julie Ries has no competing financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ries, J.D. A framework for rehabilitation for older adults living with dementia. Arch Physiother 12, 9 (2022). https://doi.org/10.1186/s40945-022-00134-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40945-022-00134-5