Abstract
Background
Implementation of best-practice care for patients with low back pain (LBP) is an important issue. Physiotherapists’ who hold unhelpful beliefs are less likely to adhere to guidelines and may negatively influence their patients’ beliefs. Pre-registration education is critical in moving towards a biopsychosocial model of care. This study aimed to investigate the changes in 2nd year physiotherapy students’ beliefs about LBP after a module on spinal pain management and determine whether these changes were maintained at the end of academic training.
Methods
During three consecutive calendar years, this longitudinal cohort study assessed physiotherapy students’ beliefs with the Back Pain Attitudes Questionnaires (Back-PAQ) in their 1st year, before and after their 2nd year spinal management learning module, and at the end of academic training (3rd year). Unpaired t-tests were conducted to explore changes in Back-PAQ score.
Results
The mean response rate after the spinal management module was 90% (128/143 students). The mean (± SD) Back-PAQ score was 87.73 (± 14.21) before and 60.79 (± 11.44) after the module, representing a mean difference of − 26.95 (95%CI − 30.09 to − 23.80, p < 0.001). Beliefs were further improved at the end of 3rd year (− 7.16, 95%CI − 10.50 to − 3.81, p < 0.001).
Conclusions
A spinal management learning module considerably improved physiotherapy students’ beliefs about back pain. Specifically, unhelpful beliefs about the back being vulnerable and in need of protection were substantially decreased after the module. Improvements were maintained at the end of academic training one-year later. Future research should investigate whether modifying students’ beliefs leads to improved clinical practice in their first years of practice.
Similar content being viewed by others
Background
Low back pain (LBP) is the leading cause of disability worldwide and is associated with significant reduction in quality of life and severe economic burden [1, 2]. Unhelpful attitudes and beliefs about back pain have been shown to be predictors of outcomes [3]. People commonly believe that the back is vulnerable to injury and needs protection [4,5,6,7,8] and these beliefs may contribute to pain-related fear, catastrophizing and anxiety [9,10,11,12]. These psychological factors are important predictors of unhelpful behaviours and elevated levels of disability [13,14,15,16].
Gaps between evidence and practice in the management of LBP have been identified worldwide indicating that many patients receive sub-optimal care [17, 18]. While there are many factors that influence implementation of best-practice care, evidence suggests that unhelpful beliefs among health professionals is a significant factor associated with reduced guideline adherence [19,20,21,22]. Therefore, addressing health professionals’ unhelpful beliefs has been strongly recommended to improve the quality of care of LBP [11, 17, 18].
Physiotherapists are at the frontline of LBP management and spend a considerable amount of time with patients [18, 23]. Consequently, physiotherapists have the opportunity to significantly influence patients’ beliefs and behaviours (positively or negatively) and, in turn, influence recovery outcomes [11, 12, 19, 22]. Physiotherapists’ beliefs can also strongly influence their clinical decisions and delivery of core guideline recommended treatments [22, 24], such as movement, physical activity and self-management.
While the biopsychosocial model of LBP is largely recognized, management of patients with LBP within a predominantly biomedical framework is still very frequent among physiotherapists [17, 18, 22, 24]. It has been argued that the focus of entry-level education on anatomical, pathological and physical dysfunctions contribute to this problem and hinder the transition towards a biopsychosocial model of care [25], while teaching about the multidimensional nature of LBP and current evidence is an important step toward implementation of the biopsychosocial model in future practice and, ultimately, improve care for patients with LBP [17, 18].
Unhelpful beliefs are prevalent amongst physiotherapy students, albeit to a lesser extent than other health care professions, but highly variable depending of the country and the stage of training [26,27,28,29,30,31]. There is limited information on training approaches that are effective in improving students’ beliefs. Two studies found positive changes in physiotherapy students’ beliefs following biopsychosocially-orientated LBP learning [29, 32]. These studies assessed either students’ beliefs about whether pain justified activity limitation and disability or that back pain is likely to have negative future consequences. However, longitudinal changes in physiotherapy students’ beliefs about their own back or their attitudes about movement, activity, and recovery behaviours or the impact of specific learning on these has not been investigated.
The main objective of this study was to investigate changes in 2nd year physiotherapy students’ attitudes and beliefs about LBP following completion of a biopsychosocially informed spinal pain management learning module. The secondary objective was to determine whether any changes following the module were maintained at the end of academic education (3rd year). We hypothesized that helpful attitudes and beliefs would be more prevalent among physiotherapy students after completing the spinal pain management module (2nd year) and that these changes would be maintained at the end of academic education.
Methods
Study design
This study is a longitudinal observational cohort study and was written according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) criteria [33].
Participants
During three consecutive years (2018 to 2020), three cohorts of pre-registration physiotherapy students at Haute Ecole Santé Vaud (HESAV) School of Health Sciences (Lausanne, Switzerland) were invited to participate anonymously in the study. Students received an email invitation for a Google Forms questionnaire at the beginning of the second semester (first year students – BSc-1), before and immediately after a spinal pain management learning module (second year students – Bsc-2) and at the end of the last mandatory module of the pre-registration training (third year students – BSc-3) (Fig. 1). Because the study was conducted from 2018 to 2020, only one cohort (2018–2020) had data collected at all timepoints. No BSc-1 data were collected for the 2017–2019 cohort and no BSc-3 data were collected for the 2019–2021 cohort. The local Research Ethics Committee (CER-VD) confirmed that the project complied with Swiss ethical regulations on studies without identifying data collection (REQ-2018-00146). Participants received information about the study and the right not to participate, and gave their informed consent before completing the questionnaire.
Physiotherapy program
The physiotherapy course at HESAV is a three-year pre-registration Bachelor of Science (BSc) program of 180 European Credits Transfer System (ECTS). Musculoskeletal content of each academic year is briefly described in Fig. 1. The spinal pain management learning module, taught in the second year of the program, is a 6-ECTS module, that covers assessment and management of pelvic, lumbar, thoracic and cervical pain conditions. Within this module, students had 9 lectures (90-min each) about differential diagnosis, current understanding of LBP, and recommendations for assessment and management of non-specific and specific LBP delivered by medical doctors (5 lectures) and academic physiotherapists (4 lectures). In addition, there were 6 practical lessons (3 h each) that covered manual assessment and treatment of clinical cases (2 lessons), progressive and functional exercises (2 lessons), and management of low back-related leg pain (2 lessons). Finally, a three-hours training activity with a focus on communication skills and individual exercise prescription was conducted with simulated patients. Important foci of the module were developing a biopsychosocial understanding of LBP and discussing common misconceptions about LBP (Table 1). Furthermore, students were encouraged to move towards a positive health concept that emphasised the capacity of individuals to adapt and self-manage [17]. The module encouraged progressive loading in daily-life activities to increase tolerance and decrease sensitivity to pain, rather than protecting the back to decrease symptoms (as would be advocated in a traditional biomedical approach). The final academic module of third year students focussed on management of long-term conditions (5-ECTS), particularly persistent pain. In this module, students had two lectures on pain mechanisms (90 min each) and multiple activities based on complex clinical cases to foster a biopsychosocial understanding of chronic pain. They also had a learning activity with simulated patients to foster communication skills (especially building a shared understanding). The BSc-2 spinal pain management module was delivered exclusively online in 2020 due to the COVID-19 pandemic. Online learning included asynchronous lectures and group activities, in which students had to answer questions about their understanding of spinal conditions, demonstrate video-based exercises and propose optimal assessment and management strategies for various patients’ situations based on clinical vignettes. They did not have any practical manual therapy learning. The training activities with simulated patients were also cancelled.
Outcomes
The primary outcome was the validated French version of the Back Pain Attitudes Questionnaire (Back-PAQ) [5, 80]. The questionnaire is composed of 34 items scoring from 1 to 5 points on a Likert scale (False, Possibly false, Unsure, Possibly true, True). Higher total score (range 34 to 170) indicates more unhelpful beliefs and attitudes about LBP. The questionnaire items and themes were created based on findings from qualitative studies with people with LBP [4, 5]. The six different themes are ‘the vulnerability of the back’ (vulnerability), ‘the need to protect the back’ (protection), ‘the correlation between pain and injury’ (pain), ‘the special nature of back pain’ (special pain), ‘activity participation while experiencing back pain’ (activity) and ‘the prognosis of back pain’ (prognosis). Students also gave details about their age and gender.
Statistical analysis
The mean Back-PAQ total score was calculated for each study time (BSc-1, BSc-2 pre module, BSc-2 post module and BSc-3). Unpaired t-tests were conducted to determine whether there were differences in Back-PAQ total score before and after the module for the three cohorts together and for each cohort separately. Because students completed the questionnaire anonymously, paired t-test could not be used. When possible, unpaired t-tests were conducted to test differences in Back-PAQ score between the end of the module and the end of pre-registration academic training as well as between BSc-1 and BSc-2 pre-module. Mean scores and mean differences per Back-PAQ item were also calculated before and after the spinal pain management module. There were no missing data in the questionnaires (all answers were compulsory to submit the questionnaire). Statistical analyses were performed with SPSS (Version 23, IBM, NY, USA), using a significance level corrected for the eight statistical tests and set a priori at α < 0.006.
Results
The response rate and number of students that participated in the study was 90% (95 students) in BSc-1, 92% (132 students) in BSc-2 before the module, 90% (128 students) in BSc-2 after the module and 87% (80 students) in BSc-3. Their mean age (SD) was 23.8 (2.9) years and 68.3% were female. Participant characteristics, response rates and mean Back-PAQ score at each time point for each cohort are presented in Table 2. Mean Back-PAQ scores reduced following the spinal pain management learning module in the 2017–2019 (− 27.36, 95%CI − 33.04 to − 21.68, p < 0.001), 2018–2020 (− 21.91, 95%CI − 26.84 to − 16.98, p < 0.001) and 2019–2021 (− 31.49, 95%CI − 36.21 to − 26.77, p < 0.001) cohorts. The pooled mean Back-PAQ change across cohorts following module completion was − 26.95 (95%CI − 30.09 to − 23.80, p < 0.001).
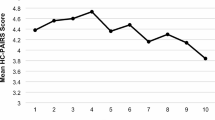
The Back-PAQ score further reduced between the end of the module and the end of BSc-3 for both the 2017–2019 (− 7.34, 95%CI − 12.12 to − 2.57, p = 0.003) and the 2018–2020 (− 7.43, 95%CI − 11.67 to − 3.19, p = 0.001) cohorts (data not available for the 2019–2021 cohort). The pooled mean Back-PAQ change of these two cohorts was − 7.16 (95%CI − 10.50 to − 3.81, p < 0.001). Mean differences between BSc-1 and BSc-2 pre module were also statistically significant for the 2018–2020 (− 12.10, 95%CI − 17.23 to - 6.98, p < 0.001) and the 2019–2021 (− 9.38, 95%CI − 14.39 to − 4.36, p < 0.001) cohorts (Fig. 2). Pooled mean Back-PAQ change was − 10.71 (95%CI − 14.28 to − 7.14, p < 0.001). Mean score per item and mean differences before and after the module are presented in Table 3.
Discussion
Physiotherapy students had predominantly unhelpful beliefs about back pain when they entered the course and these beliefs improved during each year of their training. Second year physiotherapy students’ beliefs became considerably more helpful after completing a learning module that aimed to communicate recent evidence and develop a biopsychosocial understanding of LBP.
While previous cross-sectional studies already demonstrated differences in students’ beliefs between different academic years [26, 30, 31], with more experienced students having more positive beliefs, our results showed that the largest change occurred right after a spinal pain management module, while smaller changes occur before and after this topic was specifically addressed. These changes were consistent and large for the three cohorts and were all above the minimal detectable change (MDC) of the Back-PAQ (14.5 points) [80]. Conversely, changes before and after the module were below the MDC. These results suggest that a biopsychosocially-orientated learning module with a targeted pedagogical approach can effectively improve back pain beliefs among future health professionals. Educators and pre-registration programs should consider integrating similar modules to foster their helpful beliefs that are associated with guideline concordant practice.
The large changes in beliefs about LBP that occurred as a result of the spinal pain management learning module may have resulted from several factors. First, the current multidimensional understanding of LBP and evidenced-based management strategies were frequently discussed to highlight the importance of active strategies and self-care management. Moreover, the ideas that the back can positively adapt to load and that protection does not offer long-term positive effects were central. These concepts were integrated during practical sessions covering exercise progression and the activity with simulated patients. This module used an active learning strategy to foster reflection and discuss disruptive concepts for students. As an example, how and why lumbar flexion can be progressively included in progressive loading exercises was frequently discussed with students as beliefs about the danger with loaded flexion were very prevalent before the module. This module used an integrative approach of both scientific evidence and practical courses to foster a positive image of the back and hinder prevalent unhelpful messages about ergonomic, protection and vulnerability. This consistent message throughout the module may have positively influenced students’ beliefs.
Previous studies have demonstrated that students’ beliefs about the relationship between LBP and physical function can be improved with specific training [29, 32]. Our findings extend these results by demonstrating positive changes in students’ beliefs about their own back and how they should respond to back pain and that these changes were maintained one-year later. Importantly, while changes in beliefs occurred in all items of the Back-PAQ, the questions with the largest changes were mostly related to the beliefs that the back is easy to injure (eg, questions 1, 5, 6, 9, 22 about vulnerability) and needs protection (eg, questions 8, 11). These changes are notable as physiotherapists who hold these beliefs have been found to make less evidenced-based clinical decisions and provide more advice that movement should be avoided [24]. Thus, following the spinal pain management training module, students may be more prepared to deliver adequate messages concerning these unhelpful beliefs, which are very prevalent in people with and without LBP [4,5,6,7,8] and have been associated with important contributors to LBP disability, such as pain-related fear, catastrophizing and anxiety [9,10,11,12].
The COVID-19 pandemic required rapid adaption of the 2020 physiotherapy programmes and a transition to exclusively online learning. For this cohort, the home-based practical courses were exclusively dedicated to exercise progressions and no manual therapy was practiced. The improvement in Back-PAQ score that occurred in this online-only cohort was larger than that of the two previous cohorts with a face-to-face module. While our design precludes any comparison between online or face-to-face modules, this suggests that an online module using active learning strategies is also an effective mechanism to improve physiotherapy students’ beliefs about back pain.
Unhelpful beliefs were relatively prevalent in first year students. These beliefs were more prevalent than amongst practising physiotherapists but less prevalent than in the general population from the same geographic area [8, 24]. These beliefs improved to a small degree over the students’ first year of training (below the questionnaire MDC), suggesting that non-specific education has only a small effect on unhelpful beliefs about LBP and that specific training is needed. Students’ Back-PAQ total and individual item scores following training indicated that their beliefs were more positive than those found in practising physiotherapists in Switzerland [24]. This change may enable these graduates to positively influence the beliefs of their patients and their peers and improve the quality of LBP management.
Future research is necessary to determine whether the changes in LBP beliefs among physiotherapy students are associated with changes in their clinical decisions. Ultimately, it is necessary to understand whether these changes improve the implementation of evidenced-based care in the first years of clinical practice and beyond. Given all the factors that are known to influence guideline implementation [81,82,83,84], further intervention may be necessary post-graduation to maintain or further improve beliefs about back pain and integration of evidence-based care. Given the prevalence of unhelpful beliefs in health care professionals and the efficiency of targeted learning demonstrated in these student cohorts, there may also be an opportunity to develop educational strategies for practising physiotherapists. Online learning may be an effective mechanism to deliver this at scale given the positive changes observed in students who learned exclusively online. Qualitative research on perceived efficiency of educational interventions about LBP beliefs may also improve our understanding of physiotherapy students’ learning experience and identify opportunities to refine educational strategies or support ongoing change.
The finding that a targeted active educational program positively modifies beliefs about LBP is likely to be transferable, but the magnitude of change and final level may have also been influenced by the global training environment and module timing in curriculum. The absence of a control group is a key limitation of this study and leaves open the possibility that the changes observed were due to other factors. However, measuring beliefs immediately before and after the spinal learning module reduced the risk that other learning had influenced these changes. It is often not feasible in an educational environment to randomise students to different learning interventions. The design of this study is analogous to a Single Case Experiment Design (SCED). Within SCED, three consistent replications of experimental are considered to increase the internal validity of the study, which was the case in this study for the three before-after specific module significant differences above MDC [85]. Students also completed a BSc-3 module that included content about persistent pain within a biopsychosocial framework, which may have reinforced the messages delivered in the specific LBP management module. This means that we cannot determine whether the spinal pain learning module has a long term effect or whether multiple interventions are required to maintain the positive beliefs developed. We did not record the students’ identification numbers and this precluded the use of statistical analyses based on paired tests such as repeated-measures models. Nevertheless, the unpaired t-tests used in this study demonstrated highly significant changes in beliefs, despite the reduced statistical power of this technique, making a type 2 error unlikely. The high response rate at all time points increases confidence that the findings represent real changes in beliefs across the student cohort, rather than being biased by those with less helpful beliefs selectively dropping out of the study.
Conclusion
This study found that a biopsychosocially-orientated learning module using active training methods significantly and substantially improved physiotherapy students’ beliefs about LBP. The largest changes occurred in the beliefs that the back is vulnerable and requires protection. Future research is necessary to understand if these changes in beliefs lead to more optimal clinical decisions and enhance high value care for newly graduated.
Availability of data and materials
The data used in this study are available on request from the corresponding author.
References
Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, Williams G, Smith E, Vos T, Barendregt J, Murray C, Burstein R, Buchbinder R. The global burden of low back pain: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(6):968–74. https://doi.org/10.1136/annrheumdis-2013-204428.
Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, Hoy D, Karppinen J, Pransky G, Sieper J, Smeets RJ, Underwood M, Buchbinder R, Hartvigsen J, Cherkin D, Foster NE, Maher CG, Underwood M, van Tulder M, Anema JR, Chou R, Cohen SP, Menezes Costa L, Croft P, Ferreira M, Ferreira PH, Fritz JM, Genevay S, Gross DP, Hancock MJ, Hoy D, Karppinen J, Koes BW, Kongsted A, Louw Q, Öberg B, Peul WC, Pransky G, Schoene M, Sieper J, Smeets RJ, Turner JA, Woolf A. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356–67. https://doi.org/10.1016/S0140-6736(18)30480-X.
Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity / disability in prospective cohorts of low Back pain. Spine (Phila Pa 1976). 2002;27(5):E109–20. https://doi.org/10.1097/00007632-200203010-00017.
Darlow B, Dowell A, Baxter GD, Mathieson F, Perry M, Dean S. The enduring impact of what clinicians say to people with low back pain. Ann Fam Med. 2013;11(6):527–34. https://doi.org/10.1370/afm.1518.
Darlow B, Perry M, Mathieson F, Stanley J, Melloh M, Marsh R, Baxter GD, Dowell A. The development and exploratory analysis of the Back pain attitudes questionnaire (Back-PAQ). BMJ Open. 2014;4(5):e005251. https://doi.org/10.1136/bmjopen-2014-005251.
Darlow B, Perry M, Stanley J, Mathieson F, Melloh M, Baxter GD, Dowell A. Cross-sectional survey of attitudes and beliefs about back pain in New Zealand. BMJ Open. 2014;4(5):e004725. https://doi.org/10.1136/bmjopen-2013-004725.
Pierobon A, Policastro PO, Soliño S, Andreu M, Novoa G, Raguzzi I, Villalba F, Darlow B. Beliefs and attitudes about low back pain in Argentina: a cross-sectional survey using social media. Musculoskelet Sci Pract. 2020;49:102183. https://doi.org/10.1016/j.msksp.2020.102183.
Christe G, Pizzolato V, Meyer M, Nzamba J, Pichonnaz C. Unhelpful beliefs and attitudes about low back pain in the general population: a cross-sectional survey. Musculoskelet Sci Pract. 2021;52:102342. https://doi.org/10.1016/j.msksp.2021.102342.
Bunzli S, Smith A, Watkins R, Schütze R, O’Sullivan P. What do people who score highly on the Tampa scale of Kinesiophobia really believe? A mixed methods investigation in people with chronic non specific low Back pain. Clin J Pain. 2015;31(7):621–32. https://doi.org/10.1097/AJP.0000000000000143.
Darlow B, Dean S, Perry M, Mathieson F, Baxter GD, Dowell A. Easy to harm, hard to heal: patient views about the back. Spine (Phila Pa 1976). 2015;40(11):842–50. https://doi.org/10.1097/BRS.0000000000000901.
Darlow B. Beliefs about back pain: the confluence of client, clinician and community. Int J Osteopath Med. 2016;20:53–61. https://doi.org/10.1016/j.ijosm.2016.01.005.
Briggs AM, Jordan JE, Buchbinder R, Burnett AF, O'Sullivan PB, Chua JYY, Osborne RH, Straker LM. Health literacy and beliefs among a community cohort with and without chronic low back pain. Pain. 2010;150(2):275–83. https://doi.org/10.1016/j.pain.2010.04.031.
Crombez G, Eccleston C, Van Damme S, et al. Fear-avoidance model of chronic pain: the next generation. Clin J Pain. 2012;28(6):475–83. https://doi.org/10.1097/AJP.0b013e3182385392.
Wertli MM, Eugster R, Held U, Steurer J, Kofmehl R, Weiser S. Catastrophizing—a prognostic factor for outcome in patients with low back pain: a systematic review. Spine J. 2014;14(11):2639–57. https://doi.org/10.1016/j.spinee.2014.03.003.
Linton SJ. A review of psychological risk factors in back and neck pain. Spine (Phila Pa 1976). 2000;25(9):1148–56. https://doi.org/10.1097/00007632-200005010-00017.
Christe G, Crombez G, Edd S, Opsommer E, Jolles BM, Favre J. The relationship between psychological factors and spinal motor behaviour in low back pain. Pain. 2021;162(3):672–86. https://doi.org/10.1097/j.pain.0000000000002065.
Buchbinder R, van Tulder M, Öberg B, Costa LM, Woolf A, Schoene M, Croft P, Buchbinder R, Hartvigsen J, Cherkin D, Foster NE, Maher CG, Underwood M, van Tulder M, Anema JR, Chou R, Cohen SP, Menezes Costa L, Croft P, Ferreira M, Ferreira PH, Fritz JM, Genevay S, Gross DP, Hancock MJ, Hoy D, Karppinen J, Koes BW, Kongsted A, Louw Q, Öberg B, Peul WC, Pransky G, Schoene M, Sieper J, Smeets RJ, Turner JA, Woolf A. Low back pain: a call for action. Lancet. 2018;391(10137):2384–8. https://doi.org/10.1016/S0140-6736(18)30488-4.
Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, Ferreira PH, Fritz JM, Koes BW, Peul W, Turner JA, Maher CG, Buchbinder R, Hartvigsen J, Cherkin D, Foster NE, Maher CG, Underwood M, van Tulder M, Anema JR, Chou R, Cohen SP, Menezes Costa L, Croft P, Ferreira M, Ferreira PH, Fritz JM, Genevay S, Gross DP, Hancock MJ, Hoy D, Karppinen J, Koes BW, Kongsted A, Louw Q, Öberg B, Peul WC, Pransky G, Schoene M, Sieper J, Smeets RJ, Turner JA, Woolf A. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018;391(10137):2368–83. https://doi.org/10.1016/S0140-6736(18)30489-6.
Darlow B, Fullen BM, Dean S, et al. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: A systematic review. Eur J Pain (United Kingdom). 2012;16:3–17.
Houben RMA, Ostelo RWJG, Vlaeyen JWS, Wolters PMJC, Peters M, Berg SGMSV. Health care providers’ orientations towards common low back pain predict perceived harmfulness of physical activities and recommendations regarding return to normal activity. Eur J Pain. 2005;9(2):173–83. https://doi.org/10.1016/j.ejpain.2004.05.002.
Coudeyre E, Rannou F, Tubach F, Baron G, Coriat F, Brin S, Revel M, Poiraudeau S. General practitioners’ fear-avoidance beliefs influence their management of patients with low back pain. Pain. 2006;124(3):330–7. https://doi.org/10.1016/j.pain.2006.05.003.
Gardner T, Refshauge K, Smith L, McAuley J, Hübscher M, Goodall S. Physiotherapists’ beliefs and attitudes influence clinical practice in chronic low back pain: a systematic review of quantitative and qualitative studies. J Physiother. 2017;63(3):132–43. https://doi.org/10.1016/j.jphys.2017.05.017.
Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJEM, Ostelo RWJG, Guzman J, van Tulder MW. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ. 2015;350(feb18 5):h444. https://doi.org/10.1136/bmj.h444.
Christe G, Nzamba J, Desarzens L, Leuba A, Darlow B, Pichonnaz C. Physiotherapists’ attitudes and beliefs about low back pain influence their clinical decisions and advice. In Press.
Foster NE, Delitto A. Embedding psychosocial perspectives within clinical Management of low Back Pain : integration of practice — challenges and opportunities. Phyiscal Ther. 2011;91(5):790–803. https://doi.org/10.2522/ptj.20100326.
Ryan C, Murphy D, Clark M, Lee A. The effect of a physiotherapy education compared with a non-healthcare education on the attitudes and beliefs of students towards functioning in individuals with back pain: an observational, cross-sectional study. Physiotherapy. 2010;96(2):144–50. https://doi.org/10.1016/j.physio.2009.09.010.
Briggs AM, Slater H, Smith AJ, Parkin-Smith GF, Watkins K, Chua J. Low back pain-related beliefs and likely practice behaviours among final-year cross-discipline health students. Eur J Pain. 2013;17(5):766–75. https://doi.org/10.1002/j.1532-2149.2012.00246.x.
Ferreira PH, Ferreira ML, Latimer J, Maher CG, Refshauge K, Sakamoto A, Garofalo R. Attitudes and beliefs of Brazilian and Australian physiotherapy students towards chronic back pain: a cross-cultural comparison. Physiother Res Int. 2004;9(1):13–23. https://doi.org/10.1002/pri.296.
Latimer J, Maher C, Refshauge K. The attitudes and beliefs of physiotherapy students to chronic Back pain. Clin J Pain. 2004;20(1):45–50. https://doi.org/10.1097/00002508-200401000-00009.
Leahy A, O’Keeffe M, Robinson K, O’Sullivan K. The beliefs of healthcare students about the harmfulness of daily activities for their back: a cross-sectional study. Eur J Phys. 2019;23(1):34–40. https://doi.org/10.1080/21679169.2019.1630854.
Burnett A, Sze CC, Tam SM, Yeung KM, Leong M, Wang WTJ, Tan BK, O'Sullivan P. A cross-cultural study of the Back pain beliefs of female undergraduate healthcare students. Clin J Pain. 2009;25(1):20–8. https://doi.org/10.1097/AJP.0b013e3181805a1e.
Domenech J, Sánchez-Zuriaga D, Segura-Ortí E, Espejo-Tort B, Lisón JF. Impact of biomedical and biopsychosocial training sessions on the attitudes, beliefs, and recommendations of health care providers about low back pain: a randomised clinical trial. Pain. 2011;152(11):2557–63. https://doi.org/10.1016/j.pain.2011.07.023.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7. https://doi.org/10.1016/S0140-6736(07)61602-X.
Brinjikji W, Luetmer PH, ComstockB, et al. Systematic literature review of imaging features of spinaldegeneration in asymptomatic populations. AJNRAm J Neuroradiol. 2015;36: 811–16.
Berg L, Hellum C, Gjertsen Ø, etal. Do more MRI findings imply worse disability or more intense lowback pain? A cross-sectional study of candidates for lumbar discprosthesis. SkeletalRadiol. 2013; 42:1593–602.
Suri P, Boyko EJ, Goldberg J, etal. Longitudinal associations between incident lumbar spine MRIfindings and chronic low back pain or radicular symptoms:retrospective analysis of data from the longitudinal assessment ofimaging and disability of the back (LAIDBACK). BMCMusculoskelet Disord. 2014;15:152.
Hoy D, Bain C, Williams G, et al.A systematic review of the global prevalence of low back pain.Arthritis Rheum.2012; 64: 2028–37.
Henschke N, Maher CG, RefshaugeKM, et al. Prevalence of and screening for serious spinal pathologyin patients presenting to primary care settings with acute low backpain. Arthritis Rheum.2009;60:3072–80.
Galliker G, Scherer DE,Trippolini MA, et al. Low Back Pain in the Emergency Department:Prevalence of Serious Spinal Pathologies and Diagnostic Accuracy ofRed Flags. Am J Med.2020;133:60–72.e14.
O’Sullivan P, Caneiro JP,O’Keeffe M, et al. Unraveling the Complexity of Low Back Pain. JOrthop Sport Phys Ther.2016;46: 932–7.
Jarvik JG, Gold LS, Comstock BA,et al. Association of early imaging for back pain with clinicaloutcomes in older adults. JAMA- J Am Med Assoc. 2015;313:1143–53.
Balagué F, Mannion AF, PelliséF, et al. Non-specific low back pain.Lancet.2011;379:482–91.
Bialosky JE, George SZ, BishopMD. How Spinal Manipulative Therapy Works: Why Ask Why? JOrthop Sport Phys Ther.2008;38:293–5.
Bialosky JE, Beneciuk JM, BishopMD, et al. Unraveling the Mechanisms of Manual Therapy: Modeling anApproach. J OrthopSport Phys Ther. 2017;1–31.
NICE. Lowback pain and sciatica in over 16s: assessment and management. 2016; https://www.nice.org.uk/guidance/ng59.
Dreischarf M, Rohlmann A,Graichen F, et al. In vivo loads on a vertebral body replacementduring different lifting techniques. JBiomech. 2015;49:890–5.
Khoddam-Khorasani P, Arjmand N,Shirazi-Adl A. Effect of changes in the lumbar posture in lifting ontrunk muscle and spinal loads: A combined in vivo, musculoskeletal,and finite element model study. JBiomech. 2020;104:109728.
Lagersted-Olsen J, Thomsen BL,Holtermann A, et al. Does objectively measured daily duration offorward bending predict development and aggravation of low-back pain?A prospective study. ScandJ Work Environ Health.2016;42:528–37.
Wai EK, Roffey DM, Bishop P, etal. Causal assessment of occupational bending or twisting and lowback pain: results of a systematic review. SpineJ. 2010;10:76–88.
Saraceni N, Kent P, Ng L, et al.To Flex or Not to Flex? Is There a Relationship Between Lumbar SpineFlexion During Lifting and Low Back Pain? A Systematic Review With Meta-Analysis. J Orthop Sports Phys Ther 2020;50:121–30. http://www.jospt.org/doi/10.2519/jospt.2020.9218.
Verbeek JH, Martimo K-P,Karppinen J, et al. Manual material handling advice and assistivedevices for preventing and treating back pain in workers. CochraneDatabase Syst Rev.2011;CD005958.
Hogan DAM, Greiner BA, O’SullivanL. The effect of manual handling training on achieving trainingtransfer, employee’s behaviour change and subsequent reduction ofwork-related musculoskeletal disorders: a systematic review.Ergonomics.2014;57: 93–107.
Nolan D, O’Sullivan K, NewtonC, et al. Are there differences in lifting technique between thosewith and without low back pain? A systematic review. ScandJ Pain. 2019. https://doi.org/10.1515/sjpain-2019-0089.
Laird RA, Gilbert J, Kent P, etal. Comparing lumbo-pelvic kinematics in people with and without backpain: a systematic review and meta-analysis. BMCMusculoskelet Disord2014;15:229.
Geisser ME, Ranavaya M, Haig AJ,et al. A Meta-Analytic Review of Surface Electromyography AmongPersons With Low Back Pain and Normal, Healthy Controls. JPain. 2005;6:711–26.
Christe G, Rochat V, Jolles BM,et al. Lumbar and thoracic kinematics during step ‐ up :Comparison of three ‐ dimensional angles between patients withchronic low back pain and asymptomatic individuals. JOrthop Res 2020;1–9.
Christe G, Redhead L, Legrand T,et al. Multi-segment analysis of spinal kinematics duringsit-to-stand in patients with chronic low back pain. JBiomech. 2016;49:2060–7.
Gatton ML, Pearcy MJ. Kinematicsand movement sequencing during flexion of the lumbar spine. ClinBiomech .1999;14:376–83.
Laird RA, Keating JL, Kent P.Subgroups of lumbo-pelvic flexion kinematics are present in peoplewith and without persistent low back pain. BMCMusculoskelet Disord. 2018;19:309.
Lehman GJ. The role and value ofsymptom-modification approaches in musculoskeletal practice. JOrthop Sports Phys Ther.2018;48:430–5.
Battié MC, Videman T, Kaprio J,et al. The Twin Spine Study: Contributions to a changing view of discdegeneration†. SpineJ. 2009;9:47–59.
Belavý DL, Albracht K,Bruggemann GP, et al. Can Exercise Positively Influence theIntervertebral Disc? SportMed. 2016; 46:473–85.
Belavy DL, Adams M, Brisby H, etal. Disc herniations in astronauts: What causes them, and what doesit tell us about herniation on earth? EurSpine J. 2016;25:144–54.
Belavý DL, Quittner MJ, RidgersN, et al. Running exercise strengthens the intervertebral disc. SciRep. 2017;7:45975.
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976). 2005;30(3):346–53.
Roussouly P, Pinheiro-Franco JL.Biomechanical analysis of the spino-pelvic organization andadaptation in pathology. EurSpine J. 2011;20 (Suppl5): 609–18.
Schmidt H, Bashkuev M, Weerts J,et al. How do we stand? Variations during repeated standing phases ofasymptomatic subjects and low back pain patients. JBiomech. 2018;70:67–76.
Been E, Kalichman L. Lumbarlordosis. spine. J Off JNorth Am Spine Soc.2014;14:87–97.
Dankaerts W, O’Sullivan P,Burnett A, et al. Altered patterns of superficial trunk muscleactivation during sitting in nonspecific chronic low back painpatients: importance of subclassification. Spine(Phila Pa 1976) .2006;31:2017–23.
Mannion AF, Caporaso F, PulkovskiN, et al. Spine stabilisation exercises in the treatment of chroniclow back pain: A good clinical outcome is not associated withimproved abdominal muscle function. EurSpine J. 2012; 21:1301–10.
Wong AYL, Parent EC, Funabashi M, et al. Do Changes in Transversus Abdominis and Lumbar Multifidus During Conservative Treatment Explain Changes in Clinical Outcomes Related to Nonspecific Low Back Pain? A Systematic Review. J Pain. 2014;15:377.e1-377.e35.
Smith BE, Littlewood C, May S. An update of stabilisation exercises for low back pain: a systematic review with meta-analysis. BMC Musculoskelet Disord. 2014;15:416.
Saragiotto BT, Maher CG, Yamato TP, et al. Motor control exercise for chronic non-specific low-back pain. Cochrane Database Syst Rev. 2016. https://doi.org/10.1002/14651858.CD012004. Epub ahead of print 2016.
Steiger F, Wirth B, de Bruin ED, et al. Is a positive clinical outcome after exercise therapy for chronic non-specific low back pain contingent upon a corresponding improvement in the targeted aspect(s) of performance? A systematic review. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2012;21:575–98.
Lee H, Mansell G, McAuley JH, et al. Causal mechanisms in the clinical course and treatment of back pain. Best Pract Res Clin Rheumatol. 2017;30:1074–83.
Lee H, Hübscher M, Moseley GL, et al. How does pain lead to disability? A systematic review and meta analysis of mediation studies in people with back and neck pain. Pain. 2015;156:988–97.
Vibe Fersum K, O’Sullivan P, Skouen JS, et al. Efficacy of classification-based cognitive functional therapy in patients with non-specific chronic low back pain: A randomized controlled trial. Eur J Pain. https://doi.org/10.1002/j.1532-2149.2012.00252.x. Epub ahead of print 2012.
O’Sullivan PB, Caneiro J, O’Keeffe M, et al. Cognitive Functional Therapy: An Integrated Behavioral Approach for the Targeted Management of Disabling Low Back Pain. Phys Ther. 2018;98:408–23.
O’Keeffe M, O’Sullivan P, Purtill H, et al. Cognitive functional therapy compared with a group-based exercise and education intervention for chronic low back pain: A multicentre randomised controlled trial (RCT). Br J Sports Med. 2019;1–9.
Demoulin C, Halleux V, Darlow B, et al. Traduction en langue française de la version longue du « Back Pain Attitudes Questionnaire » et étude de ses qualités psychométriques. Mains Libr. 2017;4:19–27.
Bekkering GE, Hendriks HJM, Van Tulder MW, et al. Effect on the process of care of an active strategy to implement clinical guidelines on physiotherapy for low back pain: a cluster randomised controlled trial. Qual Saf Heal Care. 2005;14(2):107–12. https://doi.org/10.1136/qshc.2003.009357.
Bérubé MÈ, Poitras S, Bastien M, et al. Strategies to translate knowledge related to common musculoskeletal conditions into physiotherapy practice: a systematic review. Physiother (United Kingdom). 2018;104:1–8.
Grimshaw J, Eccles M, Tetroe J. Implementing clinical guidelines: current evidence and future implications. J Contin Educ Heal Prof. 2004;24(Suppl 1):S31–7. https://doi.org/10.1002/chp.1340240506.
Engers AJ, Wensing M, Van Tulder MW, et al. Implementation of the Dutch low back pain guideline for general practitioners: a cluster randomized controlled trial. Spine (Phila Pa 1976). 2005;30:595–600.
Krasny-Pacini A, Evans J. Single-case experimental designs to assess intervention effectiveness in rehabilitation: a practical guide. Ann Phys Rehabil Med. 2018;61(3):164–79. https://doi.org/10.1016/j.rehab.2017.12.002.
Acknowledgements
Not applicable.
Funding
This study was not funded.
Author information
Authors and Affiliations
Contributions
GC designed the study and collected data. All authors participated to the analysis and interpretation of data, contributed significantly to the manuscript and approved its final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The local Research Ethics Committee (CER-VD) confirmed that the project complied with Swiss ethical regulations on studies without identifying data collection (REQ-2018-00146). Participants received information about the study and the right not to participate, and gave their informed consent before completing the questionnaire.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Christe, G., Darlow, B. & Pichonnaz, C. Changes in physiotherapy students’ beliefs and attitudes about low back pain through pre-registration training. Arch Physiother 11, 13 (2021). https://doi.org/10.1186/s40945-021-00106-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40945-021-00106-1