Abstract
Background
Only low-quality evidence is currently available to support the effectiveness of different traction modalities in the treatment of lumbar radiculopathy (LR). Yet, traction is still very commonly used in clinical practice. Some authors have suggested that the subgroup of patients presenting signs and symptoms of nerve root compression and unresponsive to movements centralizing symptoms may benefit from lumbar traction. The aim of this study is to conduct a systematic review of randomized controlled trials (RCTs) on the effects of vertical traction (VT) on pain and activity limitation in patients affected by LR.
Methods
We searched the Cochrane Controlled Trials Register, PubMed, CINAHL, Scopus, ISI Web of Science and PEDro from their inception to March 31, 2019 to retrieve RCTs on adults with LR using VT to reduce pain and activity limitation. We considered only trials reporting complete data on outcomes. Two reviewers selected the studies, extracted the results, and performed the quality assessment using the Risk of Bias and GRADE tools.
Results
Three studies met the inclusion criteria. Meta-analysis was not possible due to the heterogeneity of the included studies. We found very low quality evidence for a large effect of VT added to bed rest when compared to bed rest alone (g = − 1.01; 95% CI = -2.00 to − 0.02). Similarly, VT added to medication may have a large effect on pain relief when compared to medication alone (g = − 1.13; 95% CI = -1.72 to − 0.54, low quality evidence). Effects of VT added to physical therapy on pain relief were very small when compared to physical therapy without VT (g = − 0.14; 95% CI = -1.03 to 0.76, low quality evidence). All reported effects concerned short-term effect up to 3 months post-intervention.
Conclusions
With respect to short-term effects, VT may have a positive effect on pain relief if added to medication or bed rest. Long-term effects of VT are currently unknown. Future higher quality research is very likely to have an important impact on our confidence in the estimate of effect and may change these conclusions.
Similar content being viewed by others
Background
Low back pain (LBP) is a common musculoskeletal disorder [1]. Most LBP are non-specific, and only 3–5% of the general population is affected by lumbar radiculopathy (LR) [2], that is a pain syndrome caused by compression and/or irritation of lumbar nerve roots [3]. LR is a common reason for physician consultations and imaging referrals [4]; typical symptoms are radiating pain, often with numbness, paresthesia, and/or muscle weakness [4].
The initial management for LR is conservative treatment, as recommended by the North American Spine Society [5]. Among different interventions [6], lumbar traction has been used for decades in the treatment of acute or chronic LBP [7], with or without sciatica [8, 9]. Delitto [10] and Fritz [11] have suggested that the subgroup of patients presenting signs and symptoms of nerve root compression and who are unresponsive to movements that centralize symptoms may benefit from lumbar traction.
On the contrary, previous reviews have not confirmed the effectiveness of traction for LBP, with or without LR [6, 12, 13]. Judging the state of the literature as a whole, only low-quality evidence is currently available supporting the effectiveness of different traction modalities in the treatment of LR [12]. Despite this gap in knowledge, it is very commonly used in clinical practice [7, 14].
Traction can be manual or mechanical, and traction forces may be applied continuously (maintained for 20 min or more) or intermittently (alternating traction and relaxation with cycles of a few minutes each) [12]. Traction rhythm, force, and patient position can also vary.
Vertical traction (VT) exerts a distractive force by suspending the patient while held in a vertical or seated position using a belt around the chest or placing the patient in an upside down position from the ankles (the so-called inverted lumbar traction) [15]. Patients may also be asked to perform traction independently by using a pull-up bar to suspend the trunk in vertical position. Finally, VT may be done in water, using the same modalities previously described with the addiction of an external weight placed on the patient’s ankles [16]. As a result, traction force can vary from upper half patients’ body weight plus gravity to a patient’s full body weight plus gravity and/or external weight [17].
Traction forces in VT are likely to be more consistent and tailored to each patient than manual traction. In fact, they are linearly proportional to the weight of the patient’s lower body. Using the second law of Newton, the force exerted on the lower disk spaces while in suspension can be calculated with the formula F = m x g, where F is force with the unit of Newton, m is the weight of the lower body in kilograms, and g is a constant for the gravity of earth, which is equal to 9.8 [18]. Gravitational traction produces a greater widening of the individual disc space than the static supine lumbar traction and may result in decreased intradiscal pressure and pain [19]. However, most traction devices are available only in physical therapy clinics, which places a burden on patients to receive treatment.
Globally, researchers emphasize the need to identify targeted delivery methods of traction that match appropriate parameters and patient populations [12]. For all these reasons, we conducted a systematic review to investigate the effectiveness of each different type of VT compared with or added to other conservative treatments on pain and activity limitations, in patients with LR.
Main text
Methods
This systematic review protocol was registered in the PROSPERO database (code CRD42019136591) and followed PRISMA recommendations (see Additional file 1).
Data sources and searches
The authors undertook a multiple database electronic search of articles in the following databases: Cochrane Controlled Trial Register, PubMed, CINAHL, Scopus, ISI Web of Science, and PEDro. The following search terms in various combinations were utilized: “sciatica”/"radiculopathy”/"radicular syndrome”/“nerve root pain”/"leg pain/"low back pain”; “traction”/"physical therapy modalities” and adapted for the search in all databases (see Additional file 2).
Databases were searched from their inception until March 31, 2019. Additional records were explored by manually searching reference lists of selected articles, systematic reviews and Guidelines on LBP and LR, and personal records of the authors. If necessary, authors were contacted for missing information. Two independent blinded reviewers (AP, LT) conducted study selection. They first imported all results on EndNote X9 to search for and delete duplicates [20], and then they screened titles, abstracts and full texts using Rayyan QRCI [21]. Systematically the two authors compared their results; when disagreement occurred, a third expert author (CV) was consulted.
Studies selection
We included in this systematic review randomized controlled trials (RCT) on humans, in all languages and published in every date. We included only studies on adults (≥18 years) with LR confirmed by the presence of at least two of the following criteria:
-
1.
radicular symptoms: LBP with pain and/or numbness radiating below the knee.
-
2.
≥1 radicular signs:
-
a.
sensory loss/paresthesia in any of the L4-S1 dermatomes;
-
b.
diminished Patellar/Achilles reflex;
-
c.
muscle strength deficit in any of the L4-S1 myotomes.
-
a.
-
3.
positive imaging (MRI/CT) [5].
Trials including patients without signs and symptoms of LR were excluded; trials involving patients with other specific diagnoses/current pregnancy/early postpartum period were also excluded. We included RCTs in which every type of VT was applied alone or in combination with other conservative or pharmacological treatments. Only trials with complete data regarding traction (patient position, traction type, rhythm, force, duration and frequency; and number of sessions) were considered for inclusion. We considered every type of non-traction therapy, including other conservative treatment, placebo, sham treatment, minimal care, or no intervention, a control/comparison group as long as traction was the main contrast between intervention and control group. We excluded studies comparing different traction types or traction parameters.
We considered as primary outcome the intensity of pain perceived in lumbar and/or sciatic areas, measured with a Numerical Rating Scale (NRS) or a Visual Analogue Scale (VAS), In case of separate data concerning lumbar and sciatic pain, we selected those about leg pain. Secondary outcomes were: physical functioning, measured with the Oswestry Disability Index (ODI) or the Roland & Morris Disability Questionnaire (RMDQ); lumbar/leg mobility; psychological parameters (e.g. fear-avoidance beliefs, depression, anxiety); quality of life; changes in neurological function (e.g. Straight Leg Raising, Herniation Index, etc.); and treatment adherence. In cases in which data were lacking, we contacted the authors to obtain them. When they were impossible to obtain, we estimated unreported standard deviations borrowing them from one or more other studies [22].
Adverse effects, when reported, were collected.
Outcome measures were collected at short-time (up to 3 months), mid-time (from three to 6 months), and long-time (more than 6 months) follow-ups.
Data extraction and quality assessment
Two reviewers (AP, LT) independently conducted data extraction and collection of the following data:
-
population: total number of participants; number of participants of treatment/control groups; proportion of male/females; mean age; previous episodes of LBP; mean pain intensity; mean physical functioning; number of patients taking drugs;
-
interventions: setting and geographical area where the intervention was conducted; type of intervention, with frequency, intensity, number/duration of sessions;
-
comparisons: type of control, including frequency, intensity, number/duration of sessions;
-
outcomes: measurement tools used to record each outcome; means and standard deviations of each outcome at the baseline and each follow-up for all groups; measurement scales/questionnaires and their direction for each outcome.
For any disagreement, another expert author (CV) was consulted.
The same two authors conducted the risk of bias assessment using the Cochrane Collaboration’s Risk of Bias (RoB) Tool [23, 24]. This tool comprises 13 items, each item was scored as “YES” if it fulfilled the criterion, “NO” if there was a clear RoB, and “UNSURE” if there was insufficient information. To summarize the overall RoB for a study, according to Gianola and colleagues, items related to allocation concealment, blinding of outcome assessment, and incomplete outcome data were considered [25]. Studies were classified as at “low risk of bias” when all three criteria were met, at “high risk of bias” when at least one criterion was unmet, and at “moderate risk of bias” in the remaining cases.
We evaluated the overall quality of evidence using the Grading of Recommendation, Assessment, Development and Evaluation (GRADE) framework [26]. GRADE is a systematic and explicit approach to make judgments about quality of evidence and strength of recommendations. Using GRADE, we rated the evidence not by individual study, but across studies for specific clinical outcomes. We considered the five GRADE domains:
-
1)
study limitations for RoB assessment was defined “serious” if studies were classified as “high risk of bias” or “not serious” if studies were classified as “moderate/low risk of bias” using the Cochrane Collaboration’s Risk of Bias (RoB) Tool [23, 24];
-
2)
inconsistency, in case of conflicting results;
-
3)
indirectness, to describe comparisons of the characteristics of population, setting and outcomes to those of our clinical practice;
-
4)
imprecision, identifying studies that include relatively few patients and few events and thus have a wide confidence interval around the estimate of the effect [27];
-
5)
publication bias, describing the possibility that a systematic under-estimation or over-estimation of the underlying beneficial or harmful effect is due to selective publication [28].
We planned to perform the assessment of publication bias using the Egger t test only if ten or more studies have been included in our systematic review. The test proposed by Egger in 1997 may be used to test for funnel plot asymmetry. General considerations suggest that the power will be greater in the continuous outcomes than for dichotomous outcomes, but that use of the method with substantially fewer than 10 studies is unwise [22].
We decided to evaluate the quality of the evidence using GRADE approach [29], even in the case when only a single RCT addressed a comparison, by careful scrutiny of all relevant issues (risk of bias, imprecision, indirectness, and publication bias) as suggested by GRADE Guideline [30].
Data synthesis and analysis
To calculate the effects of interventions, separate analyses were made according to traction type, patient position (vertical, sitting) and force delivered. We did not take into consideration the stage of LR, so that studies on subjects in acute (less than four weeks duration), subacute (from four to 12 weeks duration), or chronic (more than 12 weeks duration) stages of LR were analyzed together. Likewise, no differences in the statistical analysis were made regarding period of application of the traction therapy (continuous or intermittent).
We provided a descriptive synthesis of the findings and estimated the effects of interventions from the included studies. When possible, we calculated Hedge’s g using a random effects model to give a more conservative estimate of effect. We chose a priori to use the random effects method because it is a more conservative approach that also allows generalization of findings beyond the studies included in the synthesis. We used the Q and I-square statistics to assess heterogeneity across studies [31].
For statistical analysis we used the software ProMeta v.2.0 (Internovi by Scarpellini Daniele s.a.s., Cesena [FC], Italy; now owned by Idostatistics) [32]. We calculated standardized mean differences (SMDs) with 95% confidence intervals (95% CIs) for continuous data. To interpret effect size calculated with SMD, we used Cohen’s interpretations of d thresholds as a guide to identify very small (< 0.20), small (≥0.20 < 0.50), medium (≥0.50 < 0.80), or large (≥0.80) effects [32]. We calculated the effect size based on the reported data (means/standard deviations/sample sizes of intervention and control groups). We excluded the studies for which these or other essential data were not reported or obtainable by contacting authors.
Results
Characteristics of the selected studies
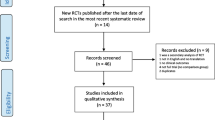
We identified 3673 records through database searching and 30 additional studies through other sources, for a total of 3703 records. After we removed duplicates, we assessed 2995 records by title and abstract, of which 94 studies were eligible to be assessed by full text reading to verify the eligibility for inclusion in this systematic review. Of these 94, we excluded another 91 studies for different reasons (see Additional file 3), resulting in three studies available for quantitative synthesis (Fig. 1).
The three included studies were published from 1998 to 2015 and conducted in Iran [33], Nederland [34], and United Kingdom [35]. The total number of patients enrolled in the studies was 90; the total number of patients who completed the assessments was 85 (range 16–50), with a mean of 28.3 participants.
The different types of traction used were VT [33, 34] and inversion traction [35], which was considered a different type of VT for statistical analysis purposes. Two studies used intermittent traction [33, 35] and one study [34] used continuous traction. The duration of the treatments ranged from 1 week to 2 months and the duration of each treatment ranged from 10 to 45 min. Traction force ranged from upper half of patient’s bodyweight to patient’s bodyweight. Interventions with which traction were compared were physical therapy (PT) [35], medications [33], and bed rest [34].
Given the aims of this study, pain was considered as primary outcome measure. Concerning secondary outcome measures, we considered only activity limitation for quantitative analyses because it was reported in most of the selected studies [34, 35]. We included other outcomes collected in single studies (i.e. lumbar range of motion, global perceived recovery, Herniation Index, etc.) only in qualitative analyses.
All studies evaluated pain and activity limitation only at short-term follow-up. All the details regarding characteristics of the studies are shown in Table 1.
Quality assessment
Risk of bias assessment according to the Cochrane Collaboration’s Risk of Bias Tool [22] showed that two studies had moderate RoB [33, 35], and one had high RoB [34]. A complete description on RoB assessment is shown in Fig. 2.
Risk of Bias of included studies according to the summarizing proposed by Gianola S. et al. [25]
Effects of interventions
Table 2 shows the study findings for pain and activity limitation with respect to the effect size for intervention outcomes, with 95% CI values.
First comparison: intermittent inversion traction combined with physical therapy versus physical therapy alone
Pain
Only one study [35] assessed this outcome and only at short-term follow-up. The effect size of VT was very small and non-significant (g = − 0.14) with a 95% CI from − 1.03 to 0.76. Following GRADE criteria this outcome provides low-quality evidence.
Activity limitation
Only one study [35] assessed this outcome and only at short-term follow-up. The effect size of VT was small and non-significant (g = − 0.31) with a 95% CI from − 1.21 to 0.58. Following GRADE criteria this outcome provides low-quality evidence.
Second comparison: continuous VT combined with bed rest versus bed rest alone
Pain
Only one study [34] assessed this outcome and only at short-term follow-up. The effect size of VT was large and significant (g = − 1.01) with a 95% CI from − 2.00 to − 0.02. Following GRADE criteria this outcome provides very low-quality evidence.
Activity limitation
Only one study [34] assessed this outcome and only at short-term follow-up. The effect size of VT was medium and non-significant (g = − 0.56) with a 95% CI from − 1.50 to 0.39. Following GRADE criteria, this outcome provides very low-quality evidence.
Third comparison: intermittent VT combined with routine medication versus routine medication alone
Pain
Only one study [33] assessed this outcome and only at short-term follow-up. The effect size of VT was large and significant (g = − 1.13) with a 95% CI from − 1.72 to − 0.54. Following GRADE criteria this outcome provides low-quality evidence.
The certainty of the evidence (GRADE) for each comparison is shown in Table 3.
Adverse effects
Among the selected studies, only the study of Moret [34] cited adverse effects. One patient reported hyperventilation complaints and had to stop traction before the end of the therapy period and another reported discomfort from the traction belt, which was easily resolved by correcting the belt position and giving extra instructions about how to fasten the belt around the chest. No other complaints were reported.
Discussion
This systematic review aimed to investigate the effectiveness of VT in the treatment of LR. Among all the studies assessed, only three studies met the criteria to be included in our systematic review, i.e., having used VT in a well-defined population and having reported complete data.
The included studies showed large statistically significant results on pain in favor of VT only when traction was combined with a passive treatment (bed rest or medications) and compared with the same treatment alone. These results are based on very low and low quality evidence respectively. According to these results, we could infer initially that VT might be effective on pain with LR. However, when we look subsequently at the results of inversion traction combined with PT and compared with PT alone, we cannot find statistically significant results either on pain or on activity limitation. Notably, these results are based on low quality evidence.
Although pain management is a primary aim of treatment, other outcomes such as the improvement of activity limitation are relevant to a complete recovery [36]. In this study, no statistically significant results on activity limitation, albeit based on low quality evidence, were found even when VT was combined with bed rest and compared with bed rest alone.
Therefore, we conclude that the role of VT appears very limited in LR, since positive results were found only on pain and only when it was compared to medications or bed rest. Relative to the effects of medications in LR, there are conflicting conclusions on NSAIDs among who considered them as effective [8], who did not draw conclusions [6], and who did not recommend them [37, 38], while a recent systematic review suggested that corticosteroids were effective in LR [39]. Concerning the advice of bed rest or stay active in patients with sciatica, little or no difference emerged on pain and function, with moderate quality evidence [6, 40]. Therefore, better results for VT appear to emerge only when it was compared with treatments whose effectiveness is uncertain.
However, an interesting suggestion in favor of VT comes from the study of Prasad [35], where 76.9% of the patients in the traction group avoided surgery, while only 22.2% of the patient in the control group had this benefit. This might imply a relevant cost-effectiveness of VT if future research offers confirmatory evidence.
VT can be particularly appealing as a clinical tool due to some of the advantages of this kind of therapy; it is very easy to use and time sparing; and it could be applied at home more frequently and for longer duration, thereby increasing the dosage. Among the studies selected in this review, VT has been applied in very different ways. In the study of Moret [34] traction was delivered in sitting position with a belt around patient’s chest; in the study of Khani [33] patients were asked to perform an auto-traction in vertical position holding in suspension from a pull-up bar; and in the study of Prasad [35] traction was performed in inverted position. Even the ways of delivering traction force changed among the studies, with one using continuous [34] and two using intermittent [33, 35] forces. Treatment dosage was different, and control groups also received different treatments. These factors did not allow us to perform meta-analysis, so our results are based on singular analyses made per each trial.
Our results are in same direction of the systematic reviews of Cheng [41] and Zhang [39]. The first one [41] showed short-term results in favor of traction for the treatment of LBP with herniated intervertebral disks, but this review included studies on patients with and without LR. The second one [39] recommended traction in patients with radiculopathy, but it did not make any difference between patients with cervical or lumbar radiculopathy.
Other systematic reviews investigating the effectiveness of traction obtained different results, but we observe that they included studies comparing different types of traction [42,43,44,45,46] or the same type of traction with different force of application [47,48,49,50,51,52,53]. The lack of a control group, which did not receive traction, could generate a high risk of bias, especially if we assume that the effect of traction could not be only related to the delivered force [54].
Adverse effects were reported only in the study of Moret [34], but they were more related to the device than to the technique. Poor tolerance and anxiety due to inversion traction were reported by Güevenol [44]. However in this trial patients were inverted for 10 consecutive minutes, so anxiety may have been due to the treatment dosage. Static inversion may produce feelings of congestion that could be avoided delivering it in shorter periods within patient’s tolerance [55].
Strength and limitations
Our search was extensive, using many databases and carefully consulting all published reviews and guidelines on this topic. The selection and qualitative assessment were independently done by two authors on studies reflecting clear PICOS criteria: this method minimized the heterogeneity of study population and allowed us to exclude studies with critically important missing data, and thereby reduced reference biases.
A strong publication bias is unlikely because studies in all languages, from every country and for any year of publication were included. However, we cannot exclude that we could have missed potential records, due to the search strategies we adopted. Moreover, other small studies or studies with negative studies have not published. Using only RCTs may have influenced the potential publication bias, but this approach allowed us to derive our conclusions by more rigorous studies. We believe our review has external validity because traction is often used by physical therapists for the treatment of LR, mostly in combination with treatments similar to that employed in the included trials [7, 14].
The most important limitation is related to the small number of included studies, also due to the very restricted population we considered, and the small sample sizes of included studies. It did not allow a sensitivity analysis; however, we have tried to account for the RoB found in the different studies with the GRADE method. Only two studies considered physical functioning as outcome measure, and only one study separately measured lumbar and sciatic pain.
The overall summarizing of RoB was different from current standards, having also used the “moderate risk of bias” classification, according to Gianola and colleagues [25]. The unreported standard deviations were derived from other similar studies: this may have led to an under-estimation or an over-estimation of the results.
No study was rated as “high quality,” and we did not find any published protocols, making it difficult to assess reporting bias. We cannot derive conclusions on what type of VT is better or which is the best patient’s position. Due to the heterogeneity in treatment dosage, both in terms of time of application and days of treatment, suggestions on this topic are not forthcoming.
Conclusions
VT may be an effective treatment only for reducing pain in LR at short-term, and may be preferred to passive treatments as bed rest and medications. VT does not demonstrate significant effects on activity limitation due to LR.
We have insufficient data to conclude that VT gives additional benefits when combined to or compared with PT treatments. Further research is very likely to have an important impact on our confidence in the estimate of effect and may change these conclusions. New large, high-quality studies are needed to investigate the effectiveness of VT and identify the most effective delivering, the best treatment dosage, or the pain stage that could benefit more by this intervention.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CIs:
-
Confidence Intervals
- CT:
-
Computed Tomography
- GRADE:
-
Grading of Recommendation, Assessment, Development and Evaluation
- LBP:
-
Low Back Pain
- LR:
-
Lumbar Radiculopathy
- MRI:
-
Magnetic Resonance Imaging
- NRS:
-
Numerical Rating Scale
- ODI:
-
Oswestry Disability Index
- PICO:
-
Patient, Intervention/Treatment, Control, Outcome
- PT:
-
Physical Therapy
- Rayyan QRCI:
-
Rayyan Qatar Computer Research Institute
- RCT:
-
Randomized Clinical Trial
- RMDQ:
-
Roland & Morris Disability Questionnaire
- RoB:
-
Risk of Bias
- SLR:
-
Straight Leg Raising
- SMDs:
-
Standardized Mean Differences
- VAS:
-
Visual Analogue Scale
- VT:
-
Vertical Traction
References
Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24(6):769–81.
Berry JA, Elia C, Saini HS, Miulli DE. A review of lumbar radiculopathy, diagnosis, and treatment. Cureus. 2019;11(10):e5934.
Van Boxem K, Cheng J, Patijn J, van Kleef M, Lataster A, Mekhail N, et al. Lumbosacral Radicular Pain. Pain Pract. 2010;10(4):339–58.
Iversen T, Solberg TK, Romner B, et al. Accuracy of physical examination for chronic lumbar radiculopathy. BMC Musculoskelet Disord. 2013;14:206.
Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 2014;14(1):180–91.
Luijsterburg PA, Verhagen AP, Ostelo RW, van Os TA, Peul WC, Koes BW. Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review. Eur Spine J. 2007;16:881–99.
Harte AA, Gracey JH, Baxter GD. Current use of lumbar traction in the management of low back pain: results of a survey of physiotherapists in the United Kingdom. Arch Phys Med Rehabil. 2005;86(6):1164–9.
Oliveira CB, Maher CG, Pinto RZ, Traeger AC, Lin CC, Chenot JF, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J. 2018;27(11):2791–803.
Van Tulder MW, Becker A, Bekkering T, Breen A, del Real MT, Hutchinson A, et al. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J. 2006;15(suppl):S169–91.
Delitto A, Erhard RE, Bowling RW. A treatment- based classification approach to low back syndrome: identifying and staging patients for conservative treatment. Phys Ther. 1995;75:470–85 discussion 485-479.
Fritz JM, Cleland JA, Childs JD. Subgrouping patients with low back pain: evolution of a classification approach to physical therapy. J Orthop Sports Phys Ther. 2007;37(6):290–302.
Alrwaily M, Almutiri M, Schneider M. Assessment of variability in traction interventions for patients with low back pain: a systematic review. Chiropr Man Therap. 2018;26:35.
Wegner I, Widyahening IS, van Tulder MW, Blomberg SE, de Vet HC, Brønfort G, et al. Traction for low-back pain with or without sciatica. Cochrane Database Syst Rev. 2013;8:CD003010.
Madson TJ, Hollman JH. Lumbar traction for managing low Back pain: a survey of physical therapists in the United States. J Orthop Sports Phys Ther. 2015;45(8):586–95.
Hahne AJ, Ford JJ, McMeeken JM. Conservative management of lumbar disc herniation with associated radiculopathy: a systematic review. Spine. 2010;35(11):E488–504.
Simmerman SM, Sizer PS, Dedrick GS, Apte GG, Brismée JM. Immediate changes in spinal height and pain after aquatic vertical traction in patients with persistent low Back symptoms: a crossover clinical trial. PM R. 2001;3(5):447–57.
Kaplan Y, Kaplan B. The effectiveness of aquatic vertical traction on lower back pain and associated sciatica. J Aquat Phys Ther. 2016;24(1):2–8.
Crowell B. Light and Matter. Section 4.2, Newton's First Law, Section 4.3, Newton's Second Law, and Section 5.1, Newton's Third Law; 2011.
Tekeoglu I, Adak B, Bozkurt M, Gurbuzoglu N. Distraction of lumbar vertebra in gravitational traction. Spine. 1998;23:1061–3.
End Note X9 software. https://endnote.com. Accessed 20 Apr 2019.
Rayyan QCRI software. https://rayyan.qcri.org. Accessed 21 Apr 2019.
Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]: The Cochrane Collaboration; 2011. Available from www.handbook.cochrane.org. Accessed 6 Aug 2020
Furlan AD, Malmivaara A, Chou R, Maher CG, Deyo RA, Schoene M, et al. 2015 updated method guideline for systematic reviews in the Cochrane Back and neck group. Spine. 2015;40(21):1660–73.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ. 2011;343:d5928.
Gianola S, Castellini G, Andreano A, Corbetta D, Frigerio P, Pecoraro V, et al. Effectiveness of treatments for acute and sub-acute mechanical non-specific low back pain: protocol for a systematic review and network meta-analysis. Syst Rev. 2019;8(1):196.
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490.
Schünemann HJ, Higgins JPT, Vist GE, Glasziou P, Akl EA, Skoetz N, Guyatt GH. Chapter 14: completing ‘summary of findings’ tables and grading the certainty of the evidence. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane handbook for systematic reviews of interventions version 6.0 (updated July 2019): Cochrane; 2019. Available from www.training.cochrane.org/handbook. Accessed 6 Aug 2020.
Schünemann H, Brożek J, Guyatt G, Oxman A (editors). The GRADE Working Group. GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations. 2013 Available from gdt.guidelinedevelopment.org/app/handbook/handbook.html. Accessed 6 Aug 2020.
Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P. GRADE guidelines: 4. Rating the quality of evidenced study limitations (risk of bias). J Clin Epidemiol. 2011;64:407e415.
Higgins J, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
ProMeta software. https://idostatistics.com. Accessed 10 Sept 2019.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: Lawrence Erlbaum Associates; 1988.
Khani M, Jahanbin S. A Randomized Controlled Trial on the Effect of Repeated Lumbar Traction By A Door-mounted Pull-up Bar on the Size and Symptoms of Herniated Lumbar Disk. Neurosurg Q. 2014;25:1. https://doi.org/10.1097/WNQ.
Moret NC, van der Stap M, Hagmeijer R, Molenaar A, Koes BW. Design and feasibility of a randomized clinical trial to evaluate the effect of vertical traction in patients with a lumbar radicular syndrome. Man Ther. 1998;3:203–21.
Prasad KS, Gregson BA, Hargreaves G, Byrnes T, Winburn P, Mendelow AD. Inversion therapy in patients with pure single level lumbar discogenic disease: a pilot randomized trial. DisabilRehabil. 2012;34(17):1473–80.
Grabovac I, Dorner TE. Association between low back pain and various everyday performances : activities of daily living, ability to work and sexual function. Wien Klin Wochenschr. 2019;131(21–22):541–9.
Vroomen PC, de Krom MC, Slofstra PD, Knottnerus JA. Conservative treatment of sciatica: a systematic review. J Spinal Disord. 2000;13(6):463–9.
Jordan J, Konstantinou K, O'Dowd J. Herniated lumbar disc.BMJ Clin Evid. 2011;2011:1118.
Zhang X, Zhang Z, Wen J, Lu J, Sun Y, Sang D. The effectiveness of therapeutic strategies for patients with radiculopathy: a network meta-analysis. Mol Pain. 2018;14:1744806918768972.
Dahm KT, Brurberg KG, Jamtvedt G, Hagen KB. Advice to rest in bed versus advice to stay active for acute low-back pain and sciatica. Cochrane Database Syst Rev. 2010;6:CD007612.
Cheng YH, Hsu CY, Lin YN. The effect of mechanical traction on low back pain in patients with herniated intervertebral disks: a systemic review and meta-analysis. Clin Rehabil. 2020;34(1):13–22.
Weber H, Ljunggren AE, Walker L. Traction therapy in patients with herniated lumbar intervertebral discs. J Oslo City Hosp. 1984;34:61–70.
Choi J, Lee S, Hwangbo G. Influences of spinal decompression therapy and general traction therapy on the pain, disability, and straight leg raising of patients with intervertebral disc herniation. J Phys Ther Sci. 2015;27(2):481–3.
Güevenol K, Tüzün Ç, Peker Ö, Göktay Y. A comparison of inverted spinal traction and conventional traction in the treatment of lumbar disc herniations. Physiother Theory Pract. 2000;16(3):151–60.
Shealy CN. Borgmeyer V. Decompression, reduction, stabilization of the Lumbar spine: A cost effective treatment for lumbosacral pain. AJPM. 1997;7(2):663–5.
Tesio L, Merlo A. Autotraction versus passive traction: an open controlled study. Arch Phys Med Rehabil. 1993;74(8):871–6.
Isner-Horobeti ME, Dufour SP, Schaeffer M, Sauleau E, Vautravers P, Lecocq J, et al. High-force versus low-force lumbar traction in acute lumbar sciatica due to disc herniation: a preliminary randomized trial. J Manipulative PhysiolTher. 2016;39(9):645–54.
Mathews JA, Hickling J. Lumbar traction: a double-blind controlled study for sciatica. RheumatolRehabil. 1975;14(4):222–5.
Murat S, Uzunca K, Erden N. The effect of lumbar traction with two different load on clinic and functional status of patients with subacute lumbar disc herniation. Medeniyet Med J. 2018;33(2):82–8.
Pal B, Mangion P, Hossain MA, Diffey BL. A controlled trial of continuous lumbar traction in the treatment of back pain and sciatica. Br J Rheumatol. 1986;25(2):181–3.
Reust P, Chantraine A, Vischer TL. Treatment of lumbar sciatica with or without neurological deficit using mechanical traction. A double-blind study. Schweizerischemedizinischewochenschrift. 1988;118(8):271–4.
van der Heijden G, Bouter L, Terpstra-Lindeman E, Essers A, Waltjè E, Köke A, et al. De effectiviteit van tractie bij lage rugklachten: de resultaten van een gerandomiseerde en geblindeerde pilotstudy. Ned T Fysiotherapie. 1991;101(2):37–41.
Weber H. Traction therapy in sciatica due to disc prolapse (does traction treatment have any positive effect on patients suffering from sciatica caused by disc prolapse?). J Oslo City Hosp. 1973;23(10):167.
Krause M, Refshauge KM, Dessen M, Boland R. Lumbar spine traction: evaluation of effects and recommended application for treatment. Man Ther. 2000;5(2):72–81.
Goldman RM, Tarr RS, Pinchuk BG, Kappler RE, Slick G, Nelson K. More on gravity inversion. West J Med. 1984;141:247.
Acknowledgments
None.
Funding
The authors declare that they have no funding.
Author information
Authors and Affiliations
Contributions
CV Designed the study, collected the data, analysed and interpreted the data, and wrote most of the text. LT Collected the data, analysed the data, and wrote part of the text. AP Collected the data, analysed the data, and wrote part of the text. AG Analysed and interpreted the data, checked and completed the text. LB Performed the statistical analysis and wrote part of the methods and results. PP Designed the study, checked and completed the text. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Based on the study design, no ethics approval was required.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Vanti, C., Turone, L., Panizzolo, A. et al. Vertical traction for lumbar radiculopathy: a systematic review. Arch Physiother 11, 7 (2021). https://doi.org/10.1186/s40945-021-00102-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40945-021-00102-5