Abstract
Background
The epiretinal membrane (ERM) is a nonvascular fibrocellular tissue formed by cellular metaplasia and proliferation at the vitreoretinal surface and is generally treated by pars plana vitrectomy (PPV) with or without internal limiting membrane (ILM) peeling. This network meta-analysis aimed to compare the efficacy of all available ERM removal interventions and assessed the use and efficacy of surgical dyes in managing idiopathic ERMs.
Methods
MEDLINE, EMBASE, Cochrane CENTRAL, and the US National Library of Medicine were searched (June 28, 2023). Clinical studies that included patients with ERMs were included. Randomized controlled trials (RCTs) were also appraised using Cochrane risk of bias (ROB).
Results
Ten RCTs and ten non-RCTs were included in this study. A pairwise meta-analysis between ERM removal and combined ERM and ILM removal showed no significant difference in visual outcome (change in BCVA) 1 year postintervention (MD = − 0.0034, SE = 0.16, p = 0.832). Similarly, there was no significant difference in the central macular thickness postoperatively between the two groups (MD = − 4.95, SE = 11.11, p = 0.656) (Q = 4.85, df = 3, p = 0.182, I2 = 41.21%). The difference in ERM recurrence between the groups was also not statistically significant (OR = 4.64, p = 0.062, I2 = 0). In a network meta-analysis, there was no significant difference in visual outcomes between ERM removal only and other treatment modalities: combined ILM and ERM removal (MD = 0.039, p = 0.837) or watchful waiting (MD = 0.020, p = 0.550). In a network meta-analysis, there was no significant difference in the visual outcomes between ERM removal alone and dye-stained combined ERM and ILM peeling (MD = 0.122, p = 0.742 for brilliant blue G; BBG and MD = 0.00, p = 1.00 for membrane blue-dual; MBD). The probability of being a better surgical dye for better visual outcomes was 0.539 for the MBD group and 0.396 for the BBG group. The recurrence of ERM was not significantly different when the ILM was stained with any of the dyes. No study was judged on ROB assessment as having low ROB in all seven domains.
Conclusion
The two types of surgical modalities provided comparable efficacy, with no significant differences between the outcomes. Among the dye-assisted ILM peeling methods, the membrane blue-dual dye was the most effective in providing better structural and functional outcomes.
Similar content being viewed by others
Background
The epiretinal membrane (ERM) proliferation is a nonvascular fibrocellular tissue formed by cellular metaplasia and proliferation at the vitreoretinal surface [1]. It causes symptomatic visual disturbances due to retinal wrinkling and distortion [2]. ERM may occur without antecedent ocular conditions or surgical procedures and is termed idiopathic or primary ERM. It may also be associated with retinal vascular diseases, trauma, or surgery and is termed secondary ERM. ERM secondary to retinal vascular diseases is very common and has been reported to be strongly associated with diabetic retinopathy [1]. The pooled age-standardized prevalence estimates of early ERM, advanced ERM, and any ERM have been reported to be 6.5%, 2.6%, and 9.1%, respectively [3]. There have been reports of ethnicity-specific prevalence rates for ERMs, with Chinese ethnicity reported to be at higher risk of contracting the disease [1]. Reported risk factors associated with the development of primary ERMs include old age, longer axial length, smoking, ethnicity, and cataracts [1].
ERM is generally treated by pars plana vitrectomy (PPV) with or without internal limiting membrane (ILM) peeling [2]. Removal of the ILM during ERM surgery has been reported to be useful in preventing subsequent recurrences [4]. However, this maneuver can cause structural and functional macular damage or endanger the macula with iatrogenic complications (tears, bleeding, and retinal pigment epithelium (RPE) damage due to microscope coaxial light or adjuvant dye toxicity). Therefore, some clinicians prefer not to remove the ILM to avoid these complications.
The ERM, ILM, and vitreous humor are semitransparent structures that are difficult to visualize without using vital dyes. Therefore, dyes are commonly used in vitreoretinal surgeries [5]. Different dyes have been used in ERM surgeries to stain the ERM, ILM, or both. However, the efficacy of these dyes in improving the structural and functional outcomes of surgery has not yet been clearly established.
Few systematic reviews have compared different surgical techniques in ERM management; however, these reviews have pooled both randomized and nonrandomized studies [6,7,8]; therefore, they have been subjected to bias or used a conventional pairwise meta-analysis yielding only one pooled effect estimate [9, 10]. Therefore, the present network meta-analysis (NMA) was conducted to compare the efficacy of all available ERM removal interventions and to assess the use and efficacy of surgical dyes in the management of idiopathic ERM.
Methods
Search strategy
The present systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) extension for Network Meta-analysis (PRISMA-NMA) guidelines [11]. A comprehensive search strategy (Additional file 1) was developed to identify articles that reported interventions for the surgical management of ERM. The review protocol was developed before the literature search and strictly followed. The MEDLINE, Embase, Scopus, and Cochrane Library databases were systematically searched from their inception to July 28, 2023, and the search results were limited to English-language articles.
Study eligibility criteria
The inclusion criteria are listed in Table 1. This review included studies published in English that used surgical procedures to manage idiopathic ERMs in patients aged ≥ 18 years. Meta-analyses were performed for randomized controlled trials (RCTs), in which individuals were randomly assigned to the two treatment groups. Nonrandomized trials (non-RCTs), defined as interventional studies that included investigator-controlled treatment allocation of participants, and case studies, defined as interventional studies that reported descriptive data of individuals, are summarized in tabulated form. Given the potential for bias in case studies and the fact that more rigorous study designs offering stronger evidence were included in this review, the case studies were not synthesized. Conference abstracts, retrospective studies, and reviews were also excluded.
Selection of studies and data extraction
Citations retrieved from different databases were imported into the Covidence [12], a systematic review tool used for screening, selection, and data extraction. Two reviewers (MAQR and EAQG) independently screened the articles based on their titles and abstracts, followed by a full-text review. Any discrepancy in the inclusion of articles was resolved through consensus, or a third reviewer (MAQG) was consulted when consensus could not be reached.
Two independent review authors (MAQR and VLG) extracted the data. The extracted data were recorded using a specially designed data-extraction form. The extracted data included the study’s first author and year of publication, study location, study design, mean age, standard deviation (SD) of the participants in each group, sample size, follow-up period (months), type of intervention(s), adjuvant dyes used, and outcome measures.
Data analysis
Data analysis was performed using R software version 4.3.1, which consists of a traditional pairwise meta-analysis using the meta [13] and metafor [14] packages, whereas a network meta-analysis (NMA) was performed using the netmeta package [15]. The results are presented using forest plots. The interventions were ranked using P scores, and the corresponding surface under the cumulative ranking curve scores (SUCRA) values were also recorded [16]. Summary estimates for continuous outcomes were reported as the mean difference (MD), while categorical outcomes were reported using the odds ratio (OR). Statistical significance was set at p < 0.05.
Assessment of heterogeneity
A random effects model was used to conduct the NMA, and heterogeneity was assessed using the Cochrane Chi-square and I2 statistics. An I2 value greater than 50% indicated substantial heterogeneity, as described in the Cochrane Handbook of Systematic Reviews [17]. In addition, the design inconsistency in the network was assessed using the decomposition of Cochrane’s Q statistic into between (inconsistency) and within design (heterogeneity) variability in the effect sizes using the netmeta package.
Assessment of risk of bias
Risk of bias (ROB) assessment was independently performed for the RCTs by two authors (MAQR and VLG). Disagreements were resolved through consensus. The Cochrane ROB tool [18] was used to appraise RCTs (Additional file 2). The Cochrane ROB tool comprises seven domains; each domain was judged as having i) low, ii) unclear, or iii) high ROB.
Results
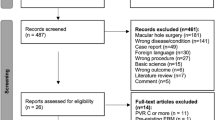
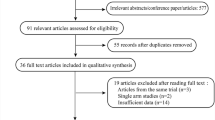
The literature search yielded 1053 articles (146 from MEDLINE, 16 from Embase, 889 from Scopus, 1 from the Cochrane Library, and 1 from the gray literature search), of which 19 were eligible for inclusion. A PRISMA flowchart is presented in Fig. 1. Ten RCTs [19,20,21,22,23,24,25,26,27,28], one prospective comparative nonrandomized trial [29] and eight prospective interventional studies [30,31,32,33,34,35,36,37] were included in this qualitative synthesis. However, only RCTs were included in this meta-analysis.
In the included prospective studies, the interventions mainly included PPV with ERM peeling only, with or without the use of a surgical dye, or combined ERM and ILM peeling with an adjuvant surgical dye. In the included RCTs and nonrandomized comparative studies, ERM peeling was compared to combined ERM and ILM peeling. One RCT [20] compared ERM removal with watchful waiting for ERM for a year. A range of surgical dyes have been used in these studies, including indocyanine green (ICG), infracyanine green (IFCG), trypan blue (TB 0.06 or 0.15%), brilliant blue G (BBG), triamcinolone acetonide (TA), view ILM, and combination dyes, such as membrane blue-dual (MBD).
Different outcome measures were assessed for the included studies. The outcome measures were best-corrected visual acuity at different follow-up periods, central macular thickness (CMT), metamorphopsia, and ERM recurrence. The characteristics of the included RCTs are presented in Table 2A, and those of the non-RCTs are presented in Table 2B.
Efficacy of interventions
Comparison of different modalities of ERM peeling
In the included studies, there were three types of interventions for the surgical management of ERM: PPV with ERM removal, PPV with ERM along with ILM removal, and watchful waiting of ERM for 1 year.
There were four RCTs [20, 22,23,24] from which complete data could be extracted to assess the visual outcome between 6 months and 1 year postintervention. A pairwise meta-analysis between ERM removal and combined ERM and ILM removal showed no significant difference in visual outcome (change in BCVA) 1 year postintervention (MD = − 0.0034, SE = 0.16, p = 0.832). There was no significant heterogeneity among studies (Q = 3.82, df = 3, p = 0.281, I2 = 0.07%). Similarly, there was no significant difference in the central macular thickness postoperatively between the two groups (MD = − 4.95, SE = 11.11, p = 0.656) (Q = 4.85, df = 3, p = 0.182, I2 = 41.21%). The difference in ERM recurrence between the groups was not statistically significant (OR = 4.64, p = 0.062, I2 = 0).
In a network meta-analysis, there was no significant difference in visual outcomes between ERM removal only and other modalities of treatment, namely, combined ILM and ERM removal (MD = 0.039, p = 0.837) or watchful waiting (MD = 0.020, p = 0.550). No significant heterogeneity (I2 = 22.2%) was observed in the network. The probability of each intervention being the best was 0.653, 0.540, and 0.307 for ERM alone, ERM with ILM, and 0.307 for watchful waiting, respectively. Based on 1000 simulations, the SUCRA values were 0.645, 0.544, and 0.310, respectively. Similarly, CMT was not significantly different between the ERM-only and ERM-with-ILM groups (MD = 5.24, p = 0.628), whereas a significant difference was observed in the watchful waiting group (MD = 41.00, p < 0.006, I2 = 38.2%). The probabilities of each intervention being the best were 0.841, 0.643, and 0.015 for the ERM-only, ERM-with-ILM, and watchful waiting groups, respectively. The corresponding SUCRA values are 0.837, 0.654, and 0.009, respectively. Forest plots for the ranking of each intervention (ERM with ILM and watchful waiting) compared with ERM peeling only (reference group) for visual outcome and changes in CMT are presented in Fig. 2.
Network meta-analysis for the most appropriate surgical dye for ERM removal
In the RCTs included in the analysis, ILM was stained with BBG, ICG, and MBD dyes. In a network meta-analysis, there was no significant difference in the visual outcomes between ERM removal alone and dye-stained ERM combined with ILM peeling (MD = 0.122, p = 0.742 for BBG and MD = 0.00, p = 1.00 for MBD). The probability of being a better surgical dye for better visual outcomes were 0.539 and 0.396 in the MBD and BBG groups, respectively. The corresponding SUCRA values were 0.528 and 0.406, respectively. Similarly, there was no significant difference in CMT when the ILM was stained with BBG (MD = 5.49, p = 0.705) or MBD (MD = − 2.00, p = 0.939, I2 = 54.1%). The probability score for MBD was 0.564, whereas for BBG, it was 0.377.
In a network meta-analysis, the recurrence of ERM was not significantly different when the ILM was stained with any of the dyes, namely, MBD (OR = 0.12, p = 0.172), BBG (OR = 0.27, p = 0.179), or ICG (OR = 0.77, p = 0.653). There was no evidence of heterogeneity (I2 = 0) in the network. The probabilities of being the best dye for nonrecurrence of ERMs were 0.817, 0.687, and 0.327 for MBD, BBG, and ICG, respectively. The corresponding SUCRA values based on 1000 simulations were 0.806, 0.689, and 0.345, respectively. Forest plots showing the effects of different dyes on the visual outcome, change in CMT, and recurrence of ERMs are presented in Fig. 3.
Complications
Intraoperative or postoperative complications related to ERM with or without ILM surgery were reported in six studies: two RCTs, one nonrandomized comparative study, and three prospective studies. The reported complications are summarized in Table 3. Retinal breaks and/or retinal detachment (RD), cystoid macular edema (CME), ocular hypertension, and cataract progression are commonly reported complications. We were unable to perform a meta-analysis due to insufficient data.
Risk of bias assessment
Figure 4 summarizes the ROB assessments of the RCTs. No study was judged to have low ROB in any of the seven domains. The domains with a lower risk of bias across all studies were ROB due to other sources of bias (10/10 studies), blinding of outcome assessors (10/10 studies), and attrition bias (10/10 studies). The domain with the highest risk of bias was ROB because of masking of participants and personnel (9/10 studies). A summary of the RCTs’ ROB judgments is provided in Additional file 2.
Discussion
The present systematic review and network meta-analysis aimed to assess the different surgical modalities of treatment and the use and efficacy of adjuvant dyes for idiopathic ERMs. The review identified three major treatment modalities: PPV with ERM removal alone, PPV with combined ERM and ILM removal, and watchful waiting for ERM. Similarly, a range of surgical dyes have been used in previous studies. The dyes used to stain ERM or ILM included TB at concentrations of 0.06% or 0.15%, ICG/IFCG, ILM view, BBG, and MBD dyes.
The NMA showed that both structural (evidenced by changes in CMT and/or recurrence of ERM) and functional (evidenced by visual outcomes) outcomes were not significantly different when the ERM was removed in isolation or when it was removed along with the ILM. However, the CMT increased significantly when no intervention (watchful waiting) was introduced. Although ERM recurrence was lower in the combined ERM and ILM peeling group, the difference was not statistically significant. The ranking of different treatment modalities suggests that although ERM alone and ERM in combination with ILM produced comparable outcomes, watchful waiting for ERM was the least effective modality of treatment for idiopathic ERM. These results of visual outcome and CMT changes in our NMA are in accordance with the pairwise meta-analyses conducted by Far et al. [9], Sun et al. [10] and an umbrella review conducted by Zhang et al. [38] However, unlike these three reviews, we did not find a significant difference in the recurrence of ERM between the groups. Previous meta-analyses had significant limitations because they pooled data from both randomized and nonrandomized studies, including retrospective studies [6,7,8].
The efficacy of the surgical dyes used for staining ILM did not produce statistically significant differences in the outcomes. However, the MBD dye produced better visual outcomes and lower ERM recurrences rates than the BBG and ICG dyes. Although limited by the number of trials included in the review, this NMA provides an important indication that MBD is a potentially more effective dye for the surgical management of ERM. This finding is concurrent with the published literature about the potential efficacy of MBD in the intraoperative identification of ERMs and ILMs from the surrounding intraocular structures [39]. Similarly, in another recent study, an improved identification of ILM at retinal breaks with MBD was reported [40]. Our findings and concurrent literature indicate a potential role of MBD in managing ERM surgery. Further studies comparing the different dyes are required to confirm these results.
All ten RCTs examining the treatment outcomes of ERM surgeries were identified as having a high risk of performance and detection biases. Surgical intervention in retinal diseases is likely to vary across patients owing to the nature of individual conditions, causes of the disease and many other factors beyond the control of a surgeon. Therefore, masking participants and personnel is difficult because clinicians and patients are typically involved in clinical decision making. Although there was a high risk of bias across the four domains (sequence generation, selection process, masking, and blinding of outcome measures), three other domains (attrition, reporting, and other biases) were judged to be at a low risk. Therefore, the validity of the current NMA results can be useful in making judgments during ERM management surgical planning.
The strength of our NMA is that we included only RCTs in the quantitative synthesis. We assessed the structural and functional outcomes only in idiopathic ERMs. ERMs due to other causes were purposefully excluded so that participants with similar inclusion criteria were included in the NMA, which helped to satisfy the assumption of transitivity. However, this study has several limitations. The number of RCTs included in the review was small, with varying outcome measures. We could not assess the heterogeneity on some occasions because of the limited number of studies.
Conclusion
A systematic search of the literature identified three treatment modalities for ERM: PPV with ERM removal alone, PPV with ERM and ILM removal, and watchful waiting for ERM. The two types of surgical modalities provided comparable efficacies, with no significant differences between the outcomes. Among the dye-assisted ILM peeling techniques, the MBD dye was the most effective in providing better structural and functional outcomes. Further multicentric RCTs comparing multiple dyes are required to confirm these findings.
Availability of data and materials
The datasets used in this study have been included in the main text. Photographs and figures from this study may be released via a written application to the Photographic Laboratory and Clinical Archives Retina Department at the Oftalmologia Integral ABC Medical and Surgical Assistance Institution (Nonprofit Organization) Av. Paseo de las Palmas 735 suite 303, Lomas de Chapultepec, Mexico City 11000, Mexico, and the corresponding author upon request. The search strategy for the data analysis and ERM-ROB analysis can be found in Additional files 1 and 2, respectively.
Abbreviations
- BBG:
-
Brilliant blue G
- BCVA:
-
Best-corrected visual acuity
- CME:
-
Cystoid macular edema
- CMT:
-
Central macular thickness
- CST:
-
Central subfield thickness
- CRT:
-
Central retinal thickness
- ERM:
-
Epiretinal membrane
- FAZ:
-
Foveal avascular zone
- GC-IPL:
-
Ganglion cell-inner plexiform layer
- ICG:
-
Indocyanine green
- IFCG:
-
Infracyanine green
- ILM:
-
Internal limiting membrane
- logMAR:
-
Logarithm of the minimum angle of resolution
- MBD:
-
Membrane blue-dual
- MD:
-
Mean deviation
- MP:
-
Most-powerful test
- NMA:
-
Network meta-analysis
- OCT:
-
Optical coherence tomography
- OR:
-
Odds ratio
- PFD:
-
Papillo-foveal distance
- PICO:
-
Population, intervention, comparator, outcomes
- PPV:
-
Pars plana vitrectomy
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analysis
- PRISMA-NMA:
-
Preferred reporting items for systematic reviews and meta-analysis extensions for network meta-analysis
- PVD:
-
Posterior vitreous detachment
- RCT:
-
Randomized controlled trials
- RD:
-
Retinal detachment
- RNFL:
-
Retinal nerve fiber layer
- ROB:
-
Risk of bias
- RPE:
-
Retinal pigment epithelium
- SANFL:
-
Swelling of the arcuate nerve fiber layer
- SCP:
-
Superficial capillary plexus
- SE:
-
Standard error
- SD:
-
Standard deviation
- SD-OCT:
-
Spectral domain-optical coherence tomography
- SUCRA:
-
Surface under the cumulative ranking curse scores
- TA:
-
Triamcinolone acetonide
- TB:
-
Trypan blue
References
Cheung N, Tan SP, Lee SY, et al. Prevalence and risk factors for epiretinal membrane: the Singapore Epidemiology of Eye Disease study. Br J Ophthalmol. 2017;101:371–6. https://doi.org/10.1136/BJOPHTHALMOL-2016-308563.
Kwok AKH, Lai TYY, Yuen KSC. Epiretinal membrane surgery with or without internal limiting membrane peeling. Clin Experiment Ophthalmol. 2005;33:379–85. https://doi.org/10.1111/J.1442-9071.2005.01015.X.
Xiao W, Chen X, Yan W, et al. Prevalence and risk factors for epiretinal membranes: a systematic review and meta-analysis of population-based studies. BMJ Open. 2017. https://doi.org/10.1136/BMJOPEN-2016-014644.
Park DW, Dugel PU, Garda J, et al. Macular pucker removal with and without internal limiting membrane peeling: pilot study. Ophthalmology. 2003;110:62–4. https://doi.org/10.1016/S0161-6420(02)01440-9.
Farah ME, Maia M, Penha FM, Rodrigues EB. The use of vital dyes during vitreoretinal surgery—chromovitrectomy. Dev Ophthalmol. 2016;55:365–75. https://doi.org/10.1159/000438963.
Fang XL, Tong Y, Zhou YL, et al. Internal limiting membrane peeling or not: a systematic review and meta-analysis of idiopathic macular pucker surgery. Br J Ophthalmol. 2017;101:1535–41. https://doi.org/10.1136/BJOPHTHALMOL-2016-309768.
Azuma K, Ueta T, Eguchi S, Aihara M. Effects of internal limiting membrane peeling combined with removal of idiopathic epiretinal membrane: a systematic review of literature and meta-analysis. Retina. 2017;37:1813–9. https://doi.org/10.1097/IAE.0000000000001537.
Pierre-Jacques M, Safran DG, Zhang F, et al. Reliability of new measures of cost-related medication nonadherence. Med Care. 2008;46:444–8. https://doi.org/10.1097/MLR.0B013E31815DC59A.
Far PM, Yeung SC, Ma PE, et al. Effects of internal limiting membrane peel for idiopathic epiretinal membrane surgery: a systematic review of randomized controlled trials. Am J Ophthalmol. 2021;231:79–87. https://doi.org/10.1016/J.AJO.2021.04.028.
Sun Y, Zhou R, Zhang B. With or without internal limiting membrane peeling for idiopathic epiretinal membrane: a meta-analysis of randomized controlled trials. Retina. 2021;41:1644–51. https://doi.org/10.1097/IAE.0000000000003076.
Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84. https://doi.org/10.7326/M14-2385.
Covidence Systematic Review Software. Veritas Health Innovation, Melbourne, Australia. Accessed May 19, 2021. www.covidence.org.
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22:153–60. https://doi.org/10.1136/ebmental-2019-300117.
Viechtbauer W. Conducting meta-analyses in R with the metafor. J Stat Softw. 2010;36:1–48. https://doi.org/10.18637/jss.v036.i03.
Schwarzer G, Carpenter JR, Rücker G. Meta-analysis with R. Published Online; 2015. https://doi.org/10.1007/978-3-319-21416-0.
Rücker G, Schwarzer G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol. 2015;15:1–9. https://doi.org/10.1186/S12874-015-0060-8/TABLES/4.
Higgins J, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions version 6.3. Cochrane. Accessed October 4, 2022. https://training.cochrane.org/handbook/current/chapter-10.
Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ. 2011. https://doi.org/10.1136/BMJ.D5928.
Hillenkamp J, Saikia P, Herrmann WA, et al. Surgical removal of idiopathic epiretinal membrane with or without the assistance of indocyanine green: a randomized controlled clinical trial. Graefes Arch Clin Exp Ophthalmol. 2007;245:973–9. https://doi.org/10.1007/S00417-006-0485-1.
Kofod M, Christensen UC, La Cour M. Deferral of surgery for epiretinal membranes: Is it safe? Results of a randomized controlled trial. Br J Ophthalmol. 2016;100:688–92. https://doi.org/10.1136/BJOPHTHALMOL-2015-307301.
Solà DV, Nienow C, Jürgens I. Assessment of the internal limiting membrane status when a macular epiretinal membrane is removed in a prospective study. Retina. 2017;37:2310–6. https://doi.org/10.1097/IAE.0000000000001478.
Tranos P, Koukoula S, Charteris DG, et al. The role of internal limiting membrane peeling in epiretinal membrane surgery: a randomized controlled trial. Br J Ophthalmol. 2017;101:719–24. https://doi.org/10.1136/BJOPHTHALMOL-2016-309308.
De Novelli FJ, Goldbaum M, Monteiro MLR, et al. Surgical removal of epiretinal membrane with and without removal of internal limiting membrane: comparative study of visual acuity, features of optical coherence tomography, and recurrence rate. Retina. 2019;39:601–7. https://doi.org/10.1097/IAE.0000000000001983.
Russo A, Morescalchi F, Gambicorti E, et al. Epiretinal membrane removal with foveal-sparing internal limiting membrane peeling: a pilot study. Retina. 2019;39:2116–24. https://doi.org/10.1097/IAE.0000000000002274.
Aydin T, Kerci SG, Karti O, et al. Effect of internal limiting membrane peeling on macular structure and metamorphopsia scores in idiopathic epiretinal membrane surgery. Open Ophthalmol J. 2020;14:1–8. https://doi.org/10.2174/1874364102014010001.
Jatoi A, Shaikh FF, Rehman AU. Vitrectomy with epiretinal membrane peeling alone verses combined with internal limiting membrane peeling for idiopathic epiretinal membrane. J Ayub Med Coll. 2020;32:450–3.
Gabriel M, Djavid D, Innauer F, et al. Changes of optical coherence tomography angiography parameters after internal limiting membrane peeling compared with nonpeeling in epiretinal membrane surgery. Retina. 2022;42:1867–73. https://doi.org/10.1097/IAE.0000000000003567.
Ripandelli G, Scarinci F, Piaggi P, et al. Macular pucker: to peel or not to peel the internal limiting membrane? A microperimetric response. Retina. 2015;35:498–507. https://doi.org/10.1097/IAE.0000000000000330.
Garweg JG, Bergstein D, Windisch B, et al. Recovery of visual field and acuity after removal of epiretinal and inner limiting membranes. Br J Ophthalmol. 2008;92:220–4. https://doi.org/10.1136/BJO.2007.131862.
Arndt C, Rebollo O, Séguinet S, et al. Quantification of metamorphopsia in patients with epiretinal membranes before and after surgery. Graefes Arch Clin Exp Ophthalmol. 2007;245:1123–9. https://doi.org/10.1007/S00417-006-0505-1.
Kinoshita T, Imaizumi H, Miyamoto H, et al. Two-year results of metamorphopsia, visual acuity, and optical coherence tomographic parameters after epiretinal membrane surgery. Graefes Arch Clin Exp Ophthalmol. 2016;254:1041–9. https://doi.org/10.1007/S00417-015-3147-3.
Shahzadi B, Rizvi SF, Latif K, et al. Visual and anatomical outcomes following idiopathic macular epiretinal membrane surgery. J Coll Phys Surg Pak. 2016;26:971–4.
Ehlers JP, Khan M, Petkovsek D, et al. Outcomes of intraoperative OCT-assisted epiretinal membrane surgery from the PIONEER study. Ophthalmol Retin. 2018;2:263–7. https://doi.org/10.1016/J.ORET.2017.05.006.
Scupola A, Grimaldi G, Abed E, et al. Arcuate nerve fiber layer changes after internal limiting membrane peeling in idiopathic epiretinal membrane. Retina. 2018;38:1777–85. https://doi.org/10.1097/IAE.0000000000001768.
Jonna G, Jonna G, Thompson IA, et al. Five-year functional outcomes after epiretinal membrane surgery: a prospective, controlled study. Retina. 2019;39:2326–31. https://doi.org/10.1097/IAE.0000000000002323.
Zobor G, Sacu S, Hollaus M, et al. The postoperative course of choroidal and central retinal thickness in epiretinal membranes with respect to membrane severity. Ophthalmic Res. 2021;64:1020–8. https://doi.org/10.1159/000519272.
Datlinger F, Georgopoulos M, Aliyeva L, et al. Postoperative movement of the fovea after successful surgery in patients with idiopathic epiretinal membranes. Retina. 2021;41:510–5. https://doi.org/10.1097/IAE.0000000000002896.
Zhang B, Dong X, Sun Y. Effect of internal limiting membrane peeling for idiopathic epiretinal membrane. Heliyon. 2023;9:e14079. https://doi.org/10.1016/j.heliyon.2023.e14079.
Veckeneer M, Mohr A, Alharthi E, et al. Novel ‘heavy’ dyes for retinal membrane staining during macular surgery: multicenter clinical assessment. Acta Ophthalmol. 2014;92:339–44. https://doi.org/10.1111/AOS.12208.
Papavasileiou E. New application of membrane blue-dual dye for retinal or iatrogenic break staining in retinal detachment surgery. Hell J Nucl Med. 2019;22(Suppl 2):63–70.
Acknowledgements
We express our deep appreciation to the technical staff of the Retina Department of Oftalmologia Integral ABC (a Medical and Surgical Nonprofit Organization), Mexico City, Mexico, which is affiliated with The Postgraduate Division Studies at the National Autonomous University of Mexico.
Funding
No funding or grant support was received for this study.
Author information
Authors and Affiliations
Contributions
MAQR, study conception, writing the manuscript, dataset interpretation, statistical analysis interpretation, final revision, conclusions; EAQG, figure artwork, tables, material compilation; MAQG, figure and table construction; VLG, statistical analysis and final revision. All the authors have approved the manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study adhered to the tenets of the Declaration of Helsinki and received full approval from the appropriate research ethics committee, institutional review committee, and institutional teaching department (the institution did not provide reference numbers for the systematic review and network meta-analysis studies).
Institutional review board statement
This study was conducted in the Retina Department of the Oftalmologia Integral ABC Institution in Mexico City. The institutional review board approved the study according to the institutional guidelines.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Search strategy.
Additional file 2:
ERM_ROB analysis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Quiroz-Reyes, M.A., Quiroz-Gonzalez, E.A., Quiroz-Gonzalez, M.A. et al. Surgical management, use and efficacy of adjuvant dyes in idiopathic epiretinal membranes: a systemic review with network meta-analysis. Int J Retin Vitr 9, 77 (2023). https://doi.org/10.1186/s40942-023-00515-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40942-023-00515-3