Abstract
Background
Uveal metastasis is reported to be the most common intraocular malignancy. The most common site of origin of ocular metastases in females is the breast. In some cases, uveal metastatic lesions respond to systemic chemotherapy. We report a case of a patient who developed choroidal metastasis, while on endocrine therapy with selective estrogen receptor modulator (SERM), tamoxifen, for estrogen receptor (ER) positive, progesterone receptor (PR) positive and (human epidermal growth factor receptor 2) HER2 negative primary breast carcinoma, which then regressed following systemic chemotherapy with palbociclib.
Case description
An 83-year-old female, with a history of modified radical mastectomy, chemotherapy and radiation therapy for infiltrating duct carcinoma of the breast, presented with a choroidal metastatic lesion in the left eye along with liver and lung metastases, 3 years after the primary carcinoma was treated. At the time of presentation, she was on tamoxifen. The choroidal tumor showed regression after the introduction of palbociclib, a cyclin-dependent kinase 4/6 (CDK4/6) inhibitor.
Conclusion
This report highlights the use of palbociclib, in the palliative treatment of choroidal metastasis from primary breast cancer. The use of chemotherapy for choroidal metastasis can help avoid external beam radiation therapy and its concurrent side effects. Although there are a few reports involving the use of palbociclib for metastatic breast carcinoma, all of those have been in conjunction with and/or following non-response to other treatment modalities. Ours is the first report wherein palbociclib has been used as the first-line palliative chemotherapy and helped in regression of choroidal metastasis.
Similar content being viewed by others
Background
Breast cancer is the most common neoplastic disorder diagnosed in females [1]. The most common site of origin of ocular metastases in females is the breast [2]. Uveal metastasis is reported to be the most common intraocular malignancy and often the first sign of tumor dissemination [3]. Uveal metastases frequently involve the choroid (88%) and uncommonly the iris (9%) or ciliary body (2%) [4]. The rich vascularity of the choroid and microenvironmental factors account for its highest metastatic efficiency index relative to all body tissues [5, 6].
Following surgical resection of the primary breast cancer, patients often receive adjuvant systemic chemotherapy with the aim of eradicating clinically and radiologically occult micrometastatic disease that may advance into frank metastatic disease if left untreated. Selection of adjuvant systemic therapies is based on classifying disease burden (number of lymph nodes, size of the primary tumor) and disease biology as determined by hormone receptor (HR) status [ER (estrogen receptor), PR (progesterone receptor)] and HER2 (human epidermal growth factor receptor 2) status, in addition to genomic assays [7]. Herein we report a case of an 83-year-old female who developed choroidal metastasis, while on endocrine therapy with selective estrogen receptor modulator (SERM), tamoxifen, for ER positive, PR positive and HER2 negative primary breast carcinoma, which then regressed following first-line palliative systemic chemotherapy with palbociclib.
Case description
An 83-year-old female presented in August 2020 with complaints of gradual diminution of vision in the left eye (OS) for two weeks. She had a history of infiltrating duct carcinoma of the breast (Stage IIIA T2N2M0), for which she had undergone modified radical mastectomy followed by chemotherapy with epirubicin and radiation therapy in 2017. On immunohistochemistry, the carcinoma was found to be ER positive, PR positive and HER2 negative. At the time of presentation to us, she was on hormonal therapy in the form of oral tamoxifen 20 mg daily.
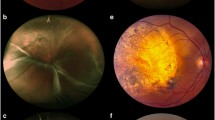
Best corrected visual acuity (BCVA) was 6/9 in the right eye (OD) and 6/24p in the left eye (OS). Intraocular pressure was normal in both eyes (OU). Anterior segment examination revealed pseudophakia OU. Fundus examination was within normal limits OD. The left eye showed a solitary yellowish elevated choroidal lesion along the superotemporal arcade, measuring approximately 3DD (disc diameters) by 3DD, with mottled hyperpigmentation on its surface (Fig. 1a). Subretinal fluid (SRF) was present at the macula. Autofluorescence (Heidelberg Retina Angiograph, Heidelberg Engineering, Heidelberg, Germany) showed alternate areas of speckled hyperautofluorescence and hypoautofluorescence within the lesion (Fig. 1b). Fundus fluorescein angiography (FFA) (Heidelberg Retina Angiograph, Heidelberg Engineering, Heidelberg, Germany) showed early hypofluorescence with late hyperfluorescence and pinpoint leakage at the borders of the lesion (Fig. 1c, d), while indocyanine green angiography (ICGA) showed early and late hypocyanescence. (Fig. 1e, f). Spectral domain optical coherence tomography (SD-OCT) (Optovue RTVue XR Avanti, Optovue Inc., Fremont, CA) revealed an elevated choroidal hyporeflective lesion, with thickened, undulating ("lumpy-bumpy") overlying retinal pigment epithelium (RPE). SRF with overlying elongated "shaggy" receptors were also seen (Fig. 1g). Bearing in mind her significant past history of breast carcinoma and the characteristic features on multimodal imaging, a provisional diagnosis of choroidal metastasis OS was made.
Multimodal imaging of choroidal metastasis in the left eye from primary breast carcinoma. At the first visit—a Multicolor fundus imaging showing a solitary yellowish elevated choroidal lesion along the superotemporal arcade with mottled hyperpigmentation on the surface. b Short wave fundus autofluorescence showing alternating areas of hyperautofluorescence and hypoautofluorescence within the lesion. c, d Fundus fluorescein angiography (FFA) showing early hypofluorescence with late hyperfluorescence and pinpoint leakage at the borders of the lesion. e, f Indocyanine green angiography (ICGA) showing early and late hypocyanescence. g Spectral domain optical coherence tomography (SD-OCT) showing an elevated choroidal hyporeflective lesion, with "lumpy-bumpy" overlying retinal pigment epithelium (RPE) and subretinal fluid with elongated "shaggy" photoreceptors
An urgent oncology clinic review was advised. Computed tomography (CT) scan of the chest and abdomen revealed mediastinal lymphadenopathy, right pleural effusion and multiple heterogeneously enhancing lesions in the liver, highly suggestive of metastases. Palliative chemotherapy for metastatic breast cancer was initiated by the oncologist in the form of oral palbociclib (cyclin-dependent kinase 4/6 (CDK4/6) inhibitor) 125 mg administered orally in 4-week cycles (3 weeks of treatment followed by 1 week off), in combination with oral letrozole (non-steroidal aromatase inhibitor) 2.5 mg daily (continuous treatment).
Three weeks after initiation of the palliative chemotherapy, her BCVA improved to 6/9 OS. Although a clinically appreciable reduction in size of the choroidal lesion OS was not visible, the tumor surface showed RPE alteration. SD-OCT showed regression of subretinal fluid and reduction in height of the choroidal lesion. At the 3-month follow up visit, BCVA was maintained at 6/9 OS. Fundus examination revealed reduction in height of the choroidal lesion OS (Fig. 2a). Autofluorescence showed stippled hyperautofluorescence and hypoautofluorescence (Fig. 2b). Repeat FFA showed early hypofluorescence and late stippled hyperfluorescence (Fig. 2c, d). Repeat ICGA (Figs. 2e, f) showed regression of hypocyanescence that was noted prior to initiation of treatment. Corresponding resolution in SRF and reduction in height of the choroidal elevation was seen on OCT (Fig. 2g). Thus, a gradual regression of the choroidal lesion on OCT was documented over 12 months of follow-up (Fig. 3a–c). At the end of the year-long follow-up in the ophthalmology clinic, she maintained status quo.
At the 3-month follow-up visit (post palliative chemotherapy with palbociclib)—a Multicolor fundus imaging showing flattening of the choroidal lesion and alteration in surface pigmentation. b Corresponding short-wave fundus autofluorescence showing prominent stippled hyperautofluorescence and hypoautofluorescence. c, d Fundus fluorescein angiography showing early hypofluorescence and late stippled hyperfluorescence. e, f Indocyanine green angiography (ICGA) showing normalization of hypocyanescence noted previously. g Spectral domain optical coherence tomography (SD-OCT) showing reduction in height of the choroidal hyporeflective lesion with resolution of overlying subretinal fluid
Serial optical coherence tomography (OCT) of our patient with choroidal metastasis in the left eye. a At the first visit, OCT showing an elevated choroidal hyporeflective lesion, with thickened, undulating, "lumpy-bumpy" overlying retinal pigment epithelium (RPE) and subretinal fluid (SRF) with elongated "shaggy" photoreceptors. b At the 3-week visit, after initiation of palbociclib, OCT showing reduction in height of choroidal lesion and regression of overlying SRF. c At the final visit (12-month follow-up), OCT showing flattening of the choroidal lesion and regressed SRF
Discussion
The prognosis and treatment options of primary breast carcinoma are guided by its clinicopathological characteristics, the presence or absence of hormone receptors (HR), the expression of the HER2 oncogene and multiparameter genomic assays [7]. 75% of breast carcinomas are ER and PR positive, and such tumors demonstrate a good response to endocrine therapy [7, 8]. SERMs such as tamoxifen are used in premenopausal and postmenopausal women; aromatase inhibitors (anastrozole, letrozole, and exemestane) are only used in postmenopausal women and are generally preferred over tamoxifen as adjuvant therapy, but may also be prescribed successively with tamoxifen [9]. Our postmenopausal patient developed a choroidal metastasis in an ER positive, PR positive and HER2 negative infiltrating duct carcinoma while on hormone therapy with tamoxifen. The aim of treatment being largely palliative at this advanced stage, the patient was offered conservative management in the form of palbociclib.
Management of patients with choroidal metastases depends on their systemic status in addition to the number, location, multifocality and laterality of the ocular tumors. Treatment options comprise of systemic chemotherapy, immunotherapy, hormone therapy, whole eye radiotherapy, plaque radiotherapy, indocyanine green augmented transpupillary thermotherapy (TTT), anti-VEGF injections, photodynamic therapy (PDT), surgical resection and enucleation [10]. It has been reported in literature that uveal metastatic lesions may respond to systemic chemotherapy [11–15], with corresponding regression of subretinal fluid documented on OCT [16, 17]. This may reduce the need for local radiation therapy [13, 15].
On 31st March, 2017, the U.S. Food and Drug Administration (FDA) granted regular approval to palbociclib (IBRANCE®, Pfizer Inc.) for the treatment of ER positive, PR positive and HER2 negative advanced or metastatic breast cancer in combination with an aromatase inhibitor as initial endocrine-based therapy in postmenopausal women [18, 19]. The PALOMA-2 [A Study of Palbociclib (PD-0332991) + Letrozole vs. Letrozole For 1st Line Treatment Of Postmenopausal Women With ER + /HER2- Advanced Breast Cancer] and PALOMA-3 [Palbociclib (PD-0332991) Combined With Fulvestrant In Hormone Receptor + HER2-Negative Metastatic Breast Cancer After Endocrine Failure] clinical trials have proven that concomitant use of palbociclib to standard endocrine therapy significantly improved outcomes in treatment of ER-positive, HER2-negative advanced breast cancer [20, 21]. There have been a few reports involving the use of palbociclib in conjunction with other treatment modalities for metastatic breast carcinoma. In a case series of 3 patients with late-onset choroidal metastasis that presented more than 20 years after diagnosis of the primary breast cancer, one of the patients was administered palbociclib for slowly progressive hepatic metastases [22]. Arya and Duker reported the regression of a choroidal metastatic lesion after the initiation of vinorelbine following failure to respond to various treatment modalities. The primary tumor was Stage IIIA T3N1M0 infiltrating duct carcinoma of the breast with ER positive, PR positive, HER2 negative expressivity. The primary malignancy was treated with surgical resection and adjuvant chemoradiation, followed by hormone therapy with numerous agents (including palbociclib) in combination with kinase inhibitors for ER resistance [23]. In another case report of ER positive, PR positive, HER2 negative breast carcinoma in a 38-year-old woman treated with right mastectomy and axillary lymph node dissection, followed by four cycles of docetaxel and cyclophosphamide and adjuvant radiation, the patient developed multiple bone metastases in addition to mediastinal lymphadenopathy, two years after the primary diagnosis [24]. The patient underwent bilateral salpingo-oophorectomy and was started on gemcitabine with denosumab. Two months later, she developed bilateral choroidal metastases, which regressed following treatment with four intravitreal injections of bevacizumab 1.25 mg and orbital radiation of 37.5 Gy in 14 fractions. After completion of bevacizumab and radiation therapy, their patient was started on palbociclib and letrozole—unlike our patient who responded to palbociclib and letrozole as first-line chemotherapy for the choroidal metastasis. In a recent case series, Beddok et al., reported that concomitant administration of palbociclib with locoregional and/or symptomatic irradiation at a metastatic site was reasonably well tolerated in a cohort of 30 women with metastatic breast cancer [25].
Conclusion
Infrequent spontaneous regression of choroidal metastatic lesions, without any therapy directed towards the primary tumor, has also been reported, although rare [26]. However, in our case, since regression of subretinal fluid and reduction in size of the choroidal lesion coincided with the initiation of palbociclib, it was the most probable contributor to the observed clinical response. The use of chemotherapy for choroidal metastasis can help avoid external beam radiation therapy and its concurrent side effects such as exposure keratopathy, radiation retinopathy, and optic neuropathy [27].
Previous reports involving the use of palbociclib for metastatic breast carcinoma have been in conjunction with and/or following non-response to other treatment modalities [22–25]. Ours is the first report wherein palbociclib has been used as the first-line palliative chemotherapy and helped in regression of choroidal metastasis. Therefore, we suggest the use of palbociclib as the initial palliative chemotherapy for choroidal metastasis following breast carcinoma.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- HR:
-
Hormone receptor
- ER:
-
Estrogen receptor
- PR:
-
Progesterone receptor
- HER2:
-
Human epidermal growth factor receptor 2
- SERM:
-
Selective estrogen receptor modulator
- BCVA:
-
Best corrected visual acuity
- OD:
-
Right eye
- OS:
-
Left eye
- OU:
-
Both eyes
- FFA:
-
Fundus fluorescein angiography
- ICGA:
-
Indocyanine green angiography
- SD-OCT:
-
Spectral-domain optical coherence tomography
- CT:
-
Computed tomography
- CDK:
-
Cyclin-dependent kinase
- TTT:
-
Transpupillary thermotherapy
- PDT:
-
Photodynamic therapy
- PALOMA-2:
-
A Study of Palbociclib (PD-0332991) + Letrozole vs. Letrozole For 1st Line Treatment Of Postmenopausal Women With ER + /HER2- Advanced Breast Cancer
- PALOMA-3:
-
Palbociclib (PD-0332991) Combined With Fulvestrant In Hormone Receptor + HER2-Negative Metastatic Breast Cancer After Endocrine Failure
References
Ban KA, Godellas CV. Epidemiology of breast cancer. Surg Oncol Clin N Am. 2014;23(3):409–22.
Freedman MI. Metastatic tumors to the eye and orbit. Arch Ophthalmol. 1987;105(9):1215.
Konstantinidis L, Rospond-Kubiak I, Zeolite I, Heimann H, Groenewald C, Coupland SE, et al. Management of patients with uveal metastases at the Liverpool Ocular Oncology Centre. Br J Ophthalmol. 2013;98(1):92–8.
Shields CL, Shields JA, Gross NE, Schwartz GP, Lally SE. Survey of 520 eyes with Uveal metastases. Ophthalmology. 1997;104(8):1265–76.
McCartney A. Intraocular metastasis. Br J Ophthalmol. 1993;77(3):133.
Weiss L. Comments on hematogenous metastatic patterns in humans as revealed by autopsy. Clin Exp Metas. 1992;10(3):191–9.
Moo T-A, Sanford R, Dang C, Morrow M. Overview of breast cancer therapy. PET Clinics. 2018;13(3):339–54.
Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, et al. American Society of Clinical Oncology/College Of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol. 2010;28(16):2784–95.
Burstein HJ, Temin S, Anderson H, Buchholz TA, Davidson NE, Gelmon KE, et al. Adjuvant endocrine therapy for women with hormone receptor–positive breast cancer: American Society of Clinical Oncology Clinical Practice Guideline focused update. J Clin Oncol. 2014;32(21):2255–69.
Konstantinidis L, Damato B. Intraocular metastases–A review. Asia-Pac J Ophthal. 2017;6(2):208–14.
Letson AD, Davidorf FH, Bruce RA. Chemotherapy for treatment of choroidal metastases from breast carcinoma. Am J Ophthalmol. 1982;93(1):102–6.
Brinkley JR. Response of a choroidal metastasis to multiple-drug chemotherapy. Cancer. 1980;45(7):1538–9.
Wong Z-W, Phillips SJ, Ellis MJ. Dramatic response of choroidal metastases from breast cancer to a combination of trastuzumab and Vinorelbine. Breast J. 2004;10(1):54–6.
Munzone E, Nolè F, Sanna G, Goldhirsch A. Response of bilateral choroidal metastases of breast cancer to therapy with trastuzumab. The Breast. 2005;14(5):380–3.
Manquez ME, Brown MM, Shields CL, Shields JA. Management of choroidal metastases from breast carcinomas using aromatase inhibitors. Curr Opin Ophthalmol. 2006;17(3):251–6.
Venkatesh P, Garg S. Regression of choroidal metastasis from breast carcinoma following letrozole therapy. Clin Experiment Ophthalmol. 2007;35(5):492–4.
Singh N, Kulkarni P, Aggarwal AN, Mittal BR, Gupta N, Behera D, et al. Choroidal metastasis as a presenting manifestation of lung cancer. Medicine. 2012;91(4):179–94.
Palbociclib [Internet]. National Center for Biotechnology Information. PubChem Compound Database. U.S. National Library of Medicine; https://pubchem.ncbi.nlm.nih.gov/compound/PalbocIclib. Accessed 9 Feb 2022.
Palbociclib (IBRANCE) [Internet]. U.S. Food and Drug Administration. 2022 . https://www.fda.gov/drugs/resources-information-approved-drugs/palbociclib-ibrance. Accessed 14 Feb 2022.
Finn RS, Martin M, Rugo HS, Jones S, Im S-A, Gelmon K, et al. Palbociclib and letrozole in advanced breast cancer. N Engl J Med. 2016;375(20):1925–36.
Turner NC, Slamon DJ, Ro J, Bondarenko I, Im S-A, Masuda N, et al. Overall survival with palbociclib and fulvestrant in advanced breast cancer. N Engl J Med. 2018;379(20):1926–36.
Levison AL, Erenler F, Zhao Y, Martin DF, Lowder C, Budd GT, et al. Late-onset choroidal metastasis from breast cancer. Retinal Cases Brief Rep. 2018;12(4):342–5.
Arya M, Duker JS. Vinorelbine-induced regression of a choroidal metastasis from primary breast carcinoma. Int J Retin Vitr. 2018. https://doi.org/10.1186/s40942-018-0121-3.
Nadiminti K, Leone JP. Intraocular bevacizumab in the treatment of choroidal metastases from breast cancer. BMJ Case Reports. 2016. https://doi.org/10.1136/bcr-2016-215719.
Beddok A, Xu HP, Henry AA, Porte B, Fourquet A, Cottu P, et al. Concurrent use of palbociclib and radiation therapy: single-centre experience and review of the literature. Br J Cancer. 2020;123(6):905–8.
Demirci H, Shields CL, Chao A-N, Shields JA. Uveal metastasis from breast cancer in 264 patients. Am J Ophthalmol. 2003;136(2):264–71.
Kanthan GL, Jayamohan J, Yip D, Conway RM. Management of metastatic carcinoma of the uveal tract: an evidence-based analysis. Clin Exp Ophthalmol. 2007;35(6):553–65.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to conceptualization and critical review of the brief report. The authors are alone responsible for the content of this article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The participant provided written consent for publication of this case.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Parakh, S., Das, S., Maheshwari, S. et al. Regression of choroidal metastasis from breast carcinoma with palbociclib. Int J Retin Vitr 8, 54 (2022). https://doi.org/10.1186/s40942-022-00398-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40942-022-00398-w