Abstract
Multiple sclerosis (MS) is a chronic inflammatory disease of the central nervous system with a very high economic impact. Peginterferon beta-1a is the first approved pegylated interferon beta-1a for the treatment of relapsing-remitting multiple sclerosis (RRMS). Its efficacy and safety were demonstrated in the placebo-controlled ADVANCE trial. A complete path to the assessment of a new health technology requires, in addition to a clinical evaluation, also an economic evaluation. In Italy, two economic evaluations were conducted and recently published.
The objective of this article is focused on the two Italian economic analyses in order to describe the methods used, to summarize the main results, and to give a comprehensive picture of the pharmacoeconomic profile of peginterferon beta-1a in Italy in approved indication.
The two analyses were conducted to evaluate such profile; the former was a cost-effectiveness analysis, the latter was a budget impact analysis:
-
1)
The cost-effectiveness analysis – developed through a lifetime Markov model – compared peginterferon beta-1a with injectable first-line treatments for RRMS in Italy from the perspective of the Italian National Healthcare Service (NHS) and from the societal perspective. Efficacy data were derived from a published Network Meta-analysis. Unit costs were based on current prices and tariffs, and the published literature.
From the Italian NHS perspective, peginterferon beta-1a was dominant in one case, while in all others its incremental cost-effectiveness ratio (ICER) was between €10,580/QALY and €22,023/QALY. From the societal perspective, peginterferon beta-1a was dominant versus every comparator.
-
2)
The budget impact analysis estimated – using a simple decision analytic model from the perspective of the Italian NHS – the financial impact due to the introduction of peginterferon beta-1a on the Italian drug market. The cumulative budget impact over 3 years was a cost saving of approximately €3.1 million.
Based on the results of both analyses, the adoption of peginterferon beta-1a for the treatment of RRMS is not only clinically effective, but also economically efficient and financially sustainable from the Italian NHS perspective.
Similar content being viewed by others
Background
Multiple sclerosis (MS) is a chronic inflammatory disease of the central nervous system, entailing a progressive disability. In 85% of patients with multiple sclerosis (MS) the onset form is relapsing–remitting MS (RRMS) [1].
MS affects 2.1 to 2.3 million people all over the world, including 600,000 in Europe and 75,000 in Italy (where an incidence is estimated of about 2000 cases/year) [2, 3].
The disease onset in full working age, its chronicity and its progression all heavily impact patients’ quality of life and societal costs [4].
The annual societal cost of MS is estimated in Italy at €2.7 billion [3], 29% of which is for direct medical costs (hospitalizations, drugs, diagnostics), 29% for indirect costs (productivity losses), and 42% for direct non-medical costs (informal care, transportation, aids) [5].
The estimated average cost per patient/year from the perspective of the Italian society (i.e., including direct and indirect costs) amounts to €38,000 ca. It varies from €23,000 ca. in patients with mild disability (Expanded Disability Status Scale [6] (EDSS) score: 0–3), to €44,000 ca. in patients with moderate disability (EDSS: 4–6.5), to €63,000 ca. in patients with severe disability (EDSS ≥7) [7].
The correlation between disease severity and cost significance was reported in several sources [3,4,5,6,7,8,9]. The Disease Modifying Therapies (DMTs) reduce the frequency of clinical relapses and delay disability progression.
Interferon (IFN) beta-1a, IFN beta-1b and glatiramer acetate (GA) are among the DMTs used in the first line treatment of patients with RRMS in Italy. They are available in injectable formulations (subcutaneous [SC] or intramuscular [IM]), with a variable administration frequency from once a day to once a week.
The European Commission granted marketing authorization to peginterferon beta-1a (Plegridy®) on July 18, 2014. This is the first pegylated formulation for the treatment of RRMS and the only therapy administered with the frequency of one SC injection every 2 weeks.
In the randomized, double-blind, phase 3 clinical trial ADVANCE [10, 11] the efficacy and safety of peginterferon beta-1a were evaluated on a 2-year time horizon. The primary endpoint was the annualized relapse rate (ARR) at 48 weeks.
In the first year patients were treated with peginterferon beta-1a, administered every two (Q2W) or 4 weeks (Q4W) or with placebo; in the second year all patients were treated with peginterferon beta-1a, as placebo patients were re-randomized to be treated with either peginterferon beta-1a Q2W or Q4W. In the first year, patients treated with peginterferon beta-1a reported on average fewer relapses than those taking placebo (0.26 for the Q2W group [p = 0.0007], 0.29 for the Q4W group [p = 0.0114]. The confirmed disability progression 24 weeks decreased significantly (p = 0.0069) in patients treated with peginterferon beta-1a Q2W compared with placebo.
In the second year peginterferon beta-1a efficacy was maintained, with greater effects for the Q2W vs Q4W dosing.
Moreover, in both administration regimens the ADVANCE study indicated a good safety and tolerability profile of peginterferon beta-1a, similar to the profile of the currently available IFN beta-1a therapies.
A complete path to the assessment of a new health technology requires, in addition to a clinical evaluation, also an economic evaluation.
The economic profile of peginterferon beta-1a versus other injectable first line therapies for the treatment of RRMS was recently evaluated In Italy with two different analyses: cost-effectiveness analysis and budget impact analysis [12, 13].
Both analyses are published in Italian language, on a journal mostly addressed to pharmacoeconomists; a purpose of the present article is to provide with new data a wider area of readers, since it is written in English, on a journal which is read mainly by clinicians.
The primary objective of the present article is focused on the two cited analyses [12, 13], in order to describe the methods used, to summarize the main results, and to give a comprehensive, unified picture of the pharmacoeconomic profile of peginterferon beta-1a in Italy in the approved indication.
Materials and methods
Economic evaluations reflect the need to rationalize the allocation of the available resources (scarce by definition), offering the decision-maker some criteria (on the basis of the information available and their reliability) such as to make justifiable choices [14]. Normally, such evaluations follow two steps.
The first (fundamental) step is aimed at estimating the economic efficiency in the allocation of healthcare resources, assuming they are invested in a given technology instead of another. The technique preferably used is the cost-effectiveness analysis (CEA) [15], with the objective of quantifying (as far as possible, consistent with the specificity of the assessed technology) how much the new technology costs in order to gain one additional benefit (typically, a life year, LY) as compared to a competitor. Such measure, on which many economic evaluations are based in healthcare, is named incremental cost-effectiveness ratio (ICER). In the decision process, the ICER is compared to an acceptability threshold value, an acknowledged (not necessarily official) benchmark to which the meaning may be given of how much the society or the National Healthcare Service (NHS) is willing to pay (willingness to pay, WTP) for one additional benefit gained (for example, as above, a life year). When the new technology is more effective and less expensive than the standard, then it is named dominant.
A LY takes the name of QALY (quality-adjusted life year) when it is weighted with the patient’s quality of life. One QALY is a measure unit “equivalent” to the benefit provided by one LY in full health. When QALYs are used, the evaluation technique may be called cost-utility analysis (CUA) – “utility” because the quality of life is converted into a synthetic coefficient which can be related, in economics, to a concept of utility such as “the degree of personal satisfaction”, with values varying from 1 (full health) to 0 (death). CEAs/CUAs are preferably conducted on a medium to long term time horizon.
No economic acceptability threshold has been officially defined in Italy to date. Some proposals have been formulated by Italian authors [16,17,18]. In other countries official thresholds are used [19], or thresholds are proposed by authors or organizations [20, 21]). Based on data from these sources, an ICER value was assumed to be economically acceptable in Italy when it is less or equal to a range from €30,000 to €50,000 per QALY gained.
The second (complementary) step of an economic evaluation is aimed at answering a more immediate and frequent question from the decision-maker, regarding the financial sustainability of a new technology in the short term (1–3 years). Such objective is pursued with the budget impact analysis (BIA), with a view to estimate how and how much a change in the mix of therapies (following the introduction and spread of the new technology) used in the treatment of a given health condition will impact on the trend of the expenditure for such condition [22] from the perspective of the National Healthcare Service.
In the next sections we describe the methods which were followed to perform the two steps (CEA and BIA [12, 13]) to evaluate the economic performance of peginterferon beta-1a for the treatment of RRMS in Italy.
The cost-effectiveness analysis (CEA) of peginterferon beta-1a in Italy
The analysis was conducted using a Markov model (a tool particularly useful when a decision problem involves risk that is continuous over time, when the timing of events is important, and when important events may happen more than once – such as the transitions that a patient performs from one health state to another, often in a recursive way [23]). The model was based on a previously published one [24], reviewed and accepted by – among several agencies – the National Institute for Health and Clinical Excellence (NICE) in the UK [25].
General description of the model
The economic perspective of the Italian National Health Service (NHS) is adopted, with an additional scenario taking into consideration the perspective of the whole Italian society. The time horizon is lifetime; costs and outcomes are discounted at the annual rate of 3.5% (to account for the effect of time on current cost and outcomes values).
Peginterferon beta-1a is compared to other injectable DMTs used in the first line therapy of RRMS:
-
IFN beta-1a, 30 μg, intramuscular (IM), once a week (Avonex®)
-
IFN beta-1a, 22 μg, subcutaneous (SC), three times a week (Rebif 22®)
-
IFN beta-1a, 44 μg SC, three times a week (Rebif 44®)
-
IFN beta-1b, 250 μg SC, every other day (Betaferon® and Extavia®)
-
GA, 20 mg SC, once a day (Copaxone®).
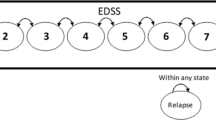
The model simulates the mortality, the disease progression between EDSS levels, the relapse frequency and the transition to secondary progressive multiple sclerosis (SPMS), estimating the survival (LYs), the survival adjusted for quality of life (QALYs), the overall costs, the incremental cost per QALY gained (ICER).
Twenty-one health states are included in the model (Fig. 1):
-
10 states in the RRMS form (EDSS levels 0; 1–1.5; 2–2.5; ….; 9–9.5)
-
10 states in the SPMS form (EDSS levels 0; 1–1.5; 2–2.5; ….; 9–9.5)
-
Death
The simulation starts with a hypothetical cohort distributed in the different EDSS levels of RRMS, according to the initial distribution and demographic characteristics of the patients in the ADVANCE study [10, 11]. At each (annual) simulation cycle the patients can progress/regress between the EDSS levels or remain in the same EDSS level in the RRMS form, progress to the SPMS form, have a relapse according to the specific probability in each level, or die. Patients cannot return from SPMS to RRMS, nor regress to lower EDSS levels in the SPMS form.
The treatments included in the model exert their effect both slowing down the disability progression (compared to the natural history of the disease) and reducing the relapse incidence in the RRMS form. Such effects persist over the long term [26,27,28,29,30]. No effect is considered on the progression from RRMS to SPMS, on the transition between EDSS levels in the SPMS form and on mortality.
It is assumed that patients stop therapy, with the DMTs included in the analysis, when reaching an EDSS level ≥ 7 in the RRMS form or when passing to the SPMS form.
In respect to each treatment adverse events are simulated.
Clinical data
The annual transition probabilities between EDSS scores of RRMS patients were obtained on the basis of data from the ADVANCE study [10, 11] (for levels 0–5), together with data from the London database, Ontario [31, 32] (for levels 6–9). The annual transition probabilities from RRMS to SPMS, and between EDSS scores of SPMS patients, were derived only from the London database (patients with SPMS were not enrolled in the ADVANCE study).
Annual relapse incidence data were obtained from the ADVANCE study [10, 11], pooled with more data from literature [33,34,35].
The death probability was estimated for each cycle considering the general mortality of the Italian population broken down by age and gender [36], adjusted for the specific relative risk (RR) in each EDSS score (risk obtained by fitting data reported in the literature [37]).
The treatment efficacy was simulated reducing the disability progression and the relapse incidence, using data derived from the recently published comprehensive Network Meta-analysis [38].
The adverse events (AEs) for all therapies included in the model were those occurred with an incidence ≥5% for peginterferon beta-1a 125 mcg in the ADVANCE study as well as AEs that occurred at an incidence of ≥3% in the overall peginterferon beta-1a group compared to the placebo group (even if the overall incidence in the peginterferon beta-1a arms was <5%). The serious adverse events were excluded, considering their very low frequency in the ADVANCE study. Annual incidences for comparators were obtained from several sources [39,40,41,42,43,44,45,46].
The utility (related to the quality of life) in the EDSS scores of RRMS patients was assessed by Kobelt et al. [5], together with a disutility (a decrement of utility, due to a health worsening) equal to 0.18 for each relapse (independent from the EDSS score). The utility in the EDSS scores of SPMS patients was estimated subtracting a disutility equal to 0.045 from the utility in the same level in RRMS [32].
The disutilities of the adverse events were obtained from literature or based on expert opinion [47,48,49,50,51].
A zero utility value was assumed when subtracting disutility gave a negative value.
Economic data
The analysis from the Italian NHS perspective identified, measured and quantified the direct medical costs relative to the health management of patients with MS.
The annual treatment cost per patient was calculated based on the ex-factory price per pack, net of temporary low reductions and any negotiated hidden discounts, multiplied by the number of units needed to cover 1 year. For all DMTs included in the model, adherence to treatment was considered equal to 100%.
Administration costs were not considered, since all DMTs in the model can be self-administered subcutaneously or intramuscularly, i.e. at zero cost from the perspective of the Italian NHS.
Annual monitoring costs were calculated based on MS healthcare regional recommendations adopted in Emilia-Romagna [52] and Lazio [53]; resources consumption was valued according to current tariffs [54]. For peginterferon beta-1a, the same consumption was assumed as for non pegylated IFN beta-1a therapies.
The direct medical management cost per relapse was calculated on the basis of an elaboration of the societal cost of one relapse assessed by Kobelt et al. [5], inflated to December 2014 with the Italian consumption price index [36].
The management cost of adverse events was calculated multiplying the annual incidence rates of the adverse events associated to each DMT included in the model by the unit cost of each event. It was assumed that adverse events included in the analysis were managed in the outpatient setting, by a general practitioner [55] or by a specialist [54].
Disease management costs (hospitalizations, outpatient care, visits and lab tests, drugs except DMTs) in the different EDSS scores of RRMS and SPMS patients were estimated processing data reported in the MS cost of illness analysis by Karampampa et al. [56].
In the additional scenario where the Italian society perspective was adopted, indirect costs due to productivity losses (sick leaves, early retirements) caused by MS were also valued, together with direct non-medical costs, e.g. for informal care (from relatives and/or friends) [56].
Sensitivity analysis
The sensitivity analysis was conducted in order to check the robustness of the results and the impact of uncertainties in the data used, considering that the clinical and economic parameters of the model might – in the real life and over time – take values both more or less favorable as compared to those adopted in the basic configuration of the model.
In the one-way sensitivity analysis (OWSA) the value of each parameter was separately varied, and the impact was calculated and registered of such change on the results. For each parameter the low and high value of its uncertainty interval were given. Such interval was defined as the 95% statistical confidence interval (95%CI) when available or as ±10% of the parameter basic value.
The probabilistic sensitivity analysis (PSA) was performed by simultaneously and randomly varying (through 1000 replications) the values of all parameters. To each of them a probability distribution was assigned, centered on the parameter base value and with a variance derived from the 95%CIs reported in the cited Network Meta-analysis [38] (for relapse and progression parameters) or with a standard error assumed equal to 25% of the base value (in all other cases).
The budget impact analysis (BIA) of peginterferon beta-1a in Italy
A simple decision analysis model was used in order to evaluate the potential financial impact of the introduction of peginterferon beta-1a in the Italian drug market for the treatment of RRMS, from the perspective of the Italian NHS, on a 3-year time horizon.
General description of the model
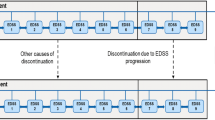
The overall treatment costs were analyzed of a population with RRMS (target population) in Italy, by comparing two different scenarios (Fig. 2):
-
A scenario in which the target population is treated with the injectable first line DMTs available in Italy (IFNs beta, GA) excluding peginterferon beta-1a (base scenario)
-
A scenario including peginterferon beta-1a among the injectable first line DMTs available in Italy (alternative scenario)
BIA Model structure. NHS: National Health Service; Adapted from Iannazzo et al. [13]
By processing drug consumption data in Italy [57], the number of patients treated with a first line injectable DMT (target population) in the first year of observation was estimated at 35,472. To this number, the number of naïve patients (2000 per year [3]) was added for the following years. The mortality was not taken into account in the budget impact analysis, in view of the short period of observation.
The treatment mix in the base scenario was derived from estimated market shares [57], assuming it remains constant during the three observed years.
In the alternative scenario, the number was initially estimated of the patients that might start the treatment with peginterferon beta-1a in the first 3 years after launch. The number of equivalent patients per year was then calculated (such number allows to consider that every patient is treated for 1 year). Based on the similarity between active principles, it was assumed that peginterferon beta-1a could compete mainly with IFN beta-1a therapies, and only marginally with IFN beta-1b and GA (considering other characteristics too: ways of use in the clinical practice, action mechanism, etc.).
Clinical data
Efficacy data – in terms of relapse incidence rate without treatment, and of relapse relative risk reduction associated to the drug treatments of the RRMS – were derived from the recently published Network Meta-analysis [38].
With the objective of maintaining a simple cost structure, among the adverse events only those related to the injection site necrosis and flu-like syndrome were considered. The respective incidences were derived from the Prescribing Information of each DMT included in the analysis [58,59,60,61,62,63].
Economic data
The treatment cost (for which a general adherence of 85% was assumed [64]), the annual monitoring costs and the management cost per relapse were valued with the same criteria adopted in the cost-effectiveness model (see point 2.1.3). The management cost of adverse events was assumed equal to the cost of an outpatient specialist visit [54].
The sensitivity analysis
An OWSA was performed, based on the same criteria adopted in the cost-effectiveness evaluation (see point 2.1.4). The analysis was focused on the maximum budget impact occurring in the third year.
Results
Similarly to the order followed in the Methods section, results are presented sequentially in the two steps of the economic evaluation of peginterferon beta-1a: CEA and BIA respectively.
The cost-effectiveness analysis (CEA) of peginterferon beta-1a in Italy
The comparison of peginterferon beta-1a with IFN beta-1a in the NHS perspective
Results of the analysis indicated that peginterferon beta-1a appeared more effective than IFN beta-1a, in terms both of survival (LYs, discounted) and of survival adjusted for quality of life (QALYs, discounted) (Table 1).
The (discounted) total direct medical cost of a patient treated with peginterferon beta-1a was slightly higher than that of a patient treated with IFN beta-1a 30 μg or with IFN beta-1a 22 μg; in fact, the higher drug and monitoring cost is only partially offset by lower costs for relapses, adverse events and disease management (as compared with the two comparators). On the contrary, the total direct medical cost of peginterferon beta-1a was lower than that of IFN beta-1a 44 μg (Table 1).
Peginterferon beta-1a was dominant vs IFN beta-1a 44 μg because it was more effective and with lower costs. The ICER of peginterferon beta-1a vs IFN beta-1a 30 μg and vs IFN beta-1a 22 μg resulted equal to €11,112 and €12,604 per QALY respectively. In both cases, the ICER is below the acceptability threshold of €30,000–50,000/QALY (Table 1).
Comparing peginterferon beta-1a with IFN beta-1a 30 μg and with IFN beta-1a 22 μg, the OWSA showed that the parameters which most impact on the cost-effectiveness results are the disability progression hazard rates and the outcomes discount rate. However, only the variation in the hazard rates can give rise to ICERs exceeding the €30,000/QALY threshold. Also in the comparison between peginterferon beta-1a and IFN beta-1a 44 μg, where the former was dominant (Table 1), the most impacting parameters are the same – but in no case the ICER exceeds €30,000/QALY.
The PSA primarily showed that the results are robust to variations in the input parameters, in all cases. Moreover, over the 1000 simulations where parameters were varied from the base-case assumptions, in the comparison with IFN beta-1a 22 μg, the probability that peginterferon beta-1a was cost-effective when WTP is assumed to be €30,000/QALY was 74.1% (79.8% if WTP is €50,000/QALY). In the comparison with IFN beta-1a 30 μg, the analogous probability was 79.7% for peginterferon beta-1a when WTP is assumed to be €30,000/QALY (85.1% when WTP is €50,000/QALY).
Finally, in the comparison with IFN beta-1a 44 μg, the PSA showed that peginterferon beta-1a is dominant in 76.2% of cases and cost-effective in 97.6% when WTP is €30,000/QALY.
The comparison of peginterferon beta-1a with other injectable first line DMTs in the NHS perspective
Peginterferon beta-1a was more effective than IFN beta-1b and GA (in terms both of LYs and of QALYs), with a total medical direct cost per patient slightly higher (Table 2).
The ICER of peginterferon beta-1a was €10,580, €16,702, and €22,023 per QALY vs IFN beta-1b 250 μg (Betaferon), IFN beta-1a 250 μg (Extavia), and GA 20 mg, respectively – below the acceptability threshold of €30,000–50,000/QALY in all comparisons (Table 2).
The results of the OWSA are in line with those relative to the comparisons between peginterferon beta-1a with IFN beta-1a (reported above).
In the PSA, the comparisons show trends analogous to those described for IFN beta-1a. In particular, the probability for peginterferon beta-1a to be cost-effective is 74.7% vs GA, 81.4% vs IFN beta-1b 250 μg (Extavia) and 87.0% vs IFN beta-1b 250 μg (Betaferon) when WTP is €50,000/QALY.
The analysis in the societal perspective
The total societal cost of a patient treated with peginterferon beta-1a was lower than those of all the comparators included in the analysis (Table 3).
Peginterferon beta-1a was dominant vs all injectable first line DMTs (IFN beta-1a, IFNβ-1b, GA) because it is more effective, in terms both of survival (LYs) and of survival adjusted for quality of life (QALYs) and with a lower total societal cost (Table 3).
The PSA showed peginterferon beta-1a dominant vs all comparators, with probabilities between 76.3% (vs IFN beta-1a 44 μg) and 85.8% (vs IFN beta-1b 250 μg).
The budget impact analysis (BIA) of peginterferon beta-1a in Italy
In the base scenario (without peginterferon beta-1a), the total medical cost of the target population was equal to €321,530,021, €339,658,686, and €357,787,352 in the first, second, third year of the observation period, respectively (Table 4). In the alternative scenario (with peginterferon beta-1a) the analogous costs were lower: €321,118,561, €338,559,367, and €356,201,191, respectively. Therefore, from the perspective of the Italian NHS, the introduction of peginterferon beta-1a to the Italian market of first line injectable therapies for the treatment of RRMS resulted in a 3-year cumulative impact of about €3.1 million savings (−0.3% of the expenditure).
The comparison of the detailed cost items in the two scenarios showed that the reduction of the total expenditure in the alternative scenario was mainly due to the reduction of the overall acquisition cost for the pharmacological therapy and to the lower costs for the relapse management thanks to the reduction of the total number of relapses.
The OWSA, focused on the cumulative impact of the 3 years, showed that the acquisition cost of peginterferon beta-1a is the most relevant parameter, the variation (±10%) of which can result in an impact with a positive value (i.e. in a cost to the Italian NHS). The result is influenced, albeit to a lesser extent, also by the efficacy parameters of the treatments (in terms of relapse increase or reduction) and by the cost per relapse; the variation of these parameters, however, can never give rise to a sign change in the result, which remains consistently favourable in the alternative scenario (with peginterferon beta-1a).
Discussion
The economic profile of peginterferon beta-1a in the treatment of RRMS in Italy was assessed with two analyses.
In the cost-effectiveness analysis (CEA), peginterferon beta-1a was compared with other injectable first line DMTs on a lifetime horizon, and was found to be the most effective. From the NHS perspective, peginterferon beta-1a was dominant versus IFN beta-1a 44 μg. The ICER of peginterferon beta-1a versus IFN beta-1a, IFN beta-1b and GA was consistently below the acceptability threshold adopted (€30,000–50,000/QALY [16,17,18,19,20,21]) – or, from another point of view, well below the level considered acceptable in another jurisdiction like UK [19]. From the societal perspective, peginterferon beta-1a was always dominant versus all the alternatives included in the cost-effectiveness model.
The analysis of the budget impact (BIA) from the NHS perspective showed that the introduction of peginterferon beta-1a results in a health expenditure reduction over the three analysed years, starting from the first year.
In both the CEA and the BIA, the sensitivity analysis confirmed the reliability of the base case results.
On the other hand, it is worth highlighting the major limitations associated to these assessments, starting from those which are common to both the CEA and the BIA of peginterferon beta-1a.
The first limitation is due to the unavailability of a head-to-head study comparing peginterferon beta-1a with the alternatives included in the analysis. As a consequence, for clinical data about the efficacy of the treatments the Network Meta-analysis [38] was used, which provides indirect comparisons. This is likely acceptable, however, considering that such analyses are numerically grown very much in the last years [65] and that their use in pharmacoeconomic evaluations is now well established [66, 67].
The second limitation lies in not having captured, in the design of the models, all the features that might be differentiating for peginterferon beta-1a, such as the administration frequency and the degree of immunogenicity.
In fact, peginterferon beta-1a is administered subcutaneously once every 2 weeks. Considering that the number of administrations per month of comparator first line injectable DMTs currently available in Italy is between 4 and 28, a reduction in administration frequency between 50% and 94% can be achieved with peginterferon beta-1a. Such a reduction might result in better adherence to treatment, with clinical and economic benefits for both patients and NHS. The adherence to therapies for MS has proved inversely correlated to the relapse incidence and to the total direct and indirect costs; in particular, the comparison between adherent and non-adherent patients showed that in the former the incidence of serious relapses is significantly lower (12.4% vs 19.9%, p < 0.013), and the average total direct and indirect costs are also significantly lower ($14,095 vs $16,638, p < 0.048) too [68].
In the pivotal study peginterferon beta-1a showed a low immunogenicity. This results in a low risk of producing neutralizing antibodies (NAbs), which reduce treatment efficacy. Patients with NAbs show a significant increase of the relapse incidence rate ratio (IRR = 1.38; p = 0.0247) and a significant decrease of the time to the first relapse (IRR = 1.51; p = 0.0111) [69]. This means that a low immunogenicity results in a low economic impact from the perspective of both the NHS and the society: the annual increment of the management cost of a patient who develops NAbs is equal to €1111 from the perspective of the Italian NHS and to €3100 from the perspective of the Italian society [70].
In any case, it should be noted that assuming an equal adherence to treatment (100% in the CEA and 85% in the BIA) in all the DMTs included in the analysis, and not considering a different immunogenicity degree among the IFNs, is a conservative approach in assessing peginterferon beta-1a.
Another limitation is represented by the value used for the relapse cost from the perspective of the Italian NHS: not having found ad hoc data in the literature, such value was calculated processing the societal cost estimated by Kobelt et al. [5]. Moreover, this source is not recent and the relapse management mode has meantime changed in the clinical practice, with a reduction of the number of relapses associated to a hospitalization. To keep into consideration the potential weakness of the adopted value, its variation interval was extended to −30% of the basic value in the OWSA.
Among the limitations specific to peginterferon beta-1a CEA only, the first one regards the model configuration, which is limited to the first line of treatment and cannot simulate possible further treatments. This is due to the fact that no therapeutic algorithm is reported in the Italian guidelines for the MS treatment.
Finally, the analysis does not capture the patient’s satisfaction/dissatisfaction effects nor the effects of increment/decrement of the quality of life associated to a MS therapy as compared with another. Due to the unavailability of data in the literature to this purpose, the utilities adopted to assess the quality of life do not keep into account the possible preferences of patients for the individual drugs.
As to the budget impact analysis, not including costs due to disability progression is a specific limitation. On the other hand, this choice was made because a three-year time horizon looked too short to appreciate the possible economic consequences of a slowing in the disability progression.
Some evidence and confirmations could be given in addition to the results of this study.
The first one regards the cost-effectiveness analysis where the average proportion between the total lifetime per patient cost from the NHS perspective (direct medical costs) and the society perspective (direct and indirect costs) is about 28% (Tables 1–3). This percentage is in line with the estimated proportion of direct medical costs in the Kobelt study [5]. The second one regards the budget impact analysis where the cost per patient per year which can be derived from Table 4 (about € 9200) looks comparable with the mean direct medical cost per patient per year reported in the Kobelt study [5] (€ 11,100) considering also that in the BIA were not considered all costs included in the Kobelt study (such as: physical visits, over the counter drugs, rehabilitation).
Further supports are available for CEA only. They show how the results from the Italian analysis are in line with those reported for US, Scotland, and Ireland.
A study was conducted in the US assessing the cost-effectiveness of peginterferon beta-1a vs IFN beta-1a (44 μg SC three times per week) and GA (20 mg SC once daily) in the treatment of RRMS from the perspective of a US payer [71].
The Markov model used for the analysis is the same (both in structure and in assumptions) as that above described in Section 2, only differing in some options (e.g., time horizon: 10 years in the base case instead of lifetime; annual discount rate: 3% instead 3.5%) and in the data concerning the US demographic and economic environment (mortality, medical costs) instead of the Italian one.
Compared with IFN beta-1a 44 μg and GA 20 mg, peginterferon beta-1a was associated with a slower rate of disability progression during RRMS and of progression to SPMS. This resulted in peginterferon beta-1a being dominant over both competitors, with cost savings of $ 22,070 (€ 19,424) and $ 19,163 (€ 16,865) respectively and additional 0.06 and 0.07 QALYs gained respectively (original monetary values were converted from $ to € @0.88 [72]).
A comparison of results from Italian and USA analyses – specific data are not reported here – shows that LYS and QALYs are fewer in the former, due to the shorter time horizon adopted in the US model. However, all (but one) cost items are higher (in particular, the cost for drugs and monitoring) than in Italy, which might be explained by a positive difference between the unit prices in the respective health systems.
The only cost item which appears higher in Italy is the cost for disease management: a kind of cost particularly increasing with the worsening of the disease, which can be better assessed in a longer time horizon.
The probabilistic sensitivity analysis showed that peginterferon beta-1a was dominant over both competitors in >90% of 5000 replications and was cost-effective in 95% of the replications when using a WTP threshold equal to $50.000 (€ 44,000) per QALY gained.
The study [67] showed that peginterferon beta-1a has a favorable cost-efficacy profile relative to its comparators, confirming the results from the Italian CEA [12].
In Scotland, the cost-effectiveness evaluation of peginterferon beta-1a vs IFNs beta and GA from the NHS perspective showed peginterferon beta-1a dominant vs IFN beta-1a 30 μg, IFN beta- 1a 22 μg and IFN beta-1b and cost-effective (assuming a WTP equal to £20,000) vs IFN beta- 1a 44 μg and GA 20 mg [73].
Also in Ireland, in the cost-effectiveness evaluation of peginterferon beta-1a vs IFNs beta and GA from the perspective of a third payer, peginterferon beta-1a resulted dominant vs all comparators [74].
Conclusions
In conclusion, the results from the cost-effectiveness analysis show that peginterferon beta-1a in the treatment of RRMS in Italy is a cost-effective alternative, vs both IFN beta- 1a and other injectable first line treatments (IFN beta- 1b and GA) from the perspective both of the Italian NHS and of the Italian society. In the light of the budget impact analysis, the introduction of peginterferon beta-1a among the first line injectable available alternatives does not result in additional costs but, on the contrary, it generates savings for the NHS.
Overall, reading together the results from two analyses (CEA and BIA), peginterferon beta-1a is a cost-effective and financially sustainable alternative from the NHS perspective and a valid option in the treatment of patients with RRMS in Italy.
References
Compston A, Coles A. Multiple Sclerosis. Lancet. 2008;372:1502–17.
MSIF - Multiple Sclerosis International Federation. Atlas of MS 2013. http://www.msif.org/wp-content/uploads/2014/09/Atlas-of-MS.pdf. Accessed 29 Feb 2016.
AISM – Associazione Italiana Sclerosi Multipla. Bilancio Sociale 2014. http://bilanciosociale.aism.it/wp-content/uploads/2014/05/AISM-Bilancio-2014.pdf. Accessed 29 Feb 2016.
Kobelt G, Pugliatti M. Cost of multiple sclerosis in Europe. Eur J Neurol. 2005;12(Suppl 1):63–7.
Kobelt G, Berg J, Lindgren P, Battaglia M, Lucioni C, Uccelli A. Costs and quality of life of multiple sclerosis in Italy. Eur J Health Econ. 2006;7(Suppl 2):S45–54.
Kurtzke JF. A new scale for evaluating disability in multiple sclerosis. Neurology. 1955;5(8):580–3.
Ponzio M, Gerzeli S, Brichetto G, Bezzini D, Mancardi GL, Zaratin P, et al. Economic impact of multiple sclerosis in Italy: focus on rehabilitation costs. Neurol Sci. 2015;36(2):227–34.
Amato MP, Battaglia MA, Caputo D, Fattore G, Gerzeli S, Pitaro M, et al., Mu. S. I. C. Study Group. The costs of multiple sclerosis: a cross-sectional, multicenter cost-of-illness study in Italy. J Neurol. 2002;249(2):152–63.
Berto P, Amato MP, Bellantonio P, Bortolon F, Cavalla P, Florio C, et al. Multiple sclerosis in Italy: cost-of-illness study. Neurol Sci. 2011;32(5):787–94.
Calabresi PA, Deykin A, Arnold DL, Balcer L, Boyko A, Pelletier J, Hung S, Sheikh S, Seddighzadeh A, Zhu Y, Liu S, Kieseier BC - analysis of 2-year clinical efficacy and safety of Peginterferon Beta-1a in patients with relapsing-remitting multiple sclerosis: data from the pivotal phase 3 ADVANCE study - American Academy of Neurology, 66th annual meeting 2014.
Calabresi PA, Kieseier BC, Arnold DL, Balcer LJ, Boyko A, Pelletier J, et al., ADVANCE Study Investigators. Pegylated interferon beta-1a for relapsing-remitting multiple sclerosis (ADVANCE): a randomised, phase 3, double-blind study. Lancet Neurol. 2014;13(7):657–65.
Iannazzo S, Santoni L, Saleri C, Puma E, Vestri G, Giuliani L, et al. Analisi di costo-efficacia dell’utilizzo di peginterferone β-1a nel trattamento della sclerosi multipla recidivante remittente in Italia. Farmeconomia. Health Econ Therapeut Pathways. 2016;17(Suppl 2):13–36.
Iannazzo S, Santoni L, Saleri C, Puma E, Vestri G, Giuliani L, et al. Valutazione dell’impatto economico di peginterferone beta-1a nel trattamento della sclerosi multipla recidivante remittente in Italia. Farmeconomia. Health Econ Therapeut Pathways. 2016;17(Suppl 2):37–48.
Fantelli V, van de Vooren K, Garattini L, Budget Impact Analysis: stato dell’arte in letteratura e proposta per una definizione in Italia. QF 2011;15.
Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. Third edition. Oxford University Press 2005, pp. 379.
Gruppo di lavoro AIES coordinato da Fattore G. Proposta di linee guida per la valutazione economica degli investimenti sanitari in Italia. Pharmaco Economics Italian Res Articles. 2009;11(2):83–93.
Lucioni C, Ravasio R. Come valutare i risultati di uno studio farmacoeconomico? Pharmaco Economics Italian Res Articles. 2004;6(3):121–30.
Messori A, Santarlasci B, Trippoli S, Vaiani M. Controvalore economico del farmaco e beneficio clinico: stato dell’arte della metodologia e applicazione di un algoritmo farmacoeconomico. Pharmaco Economics Italian Res Articles. 2003;5(2):53–67.
National Institute for Clinical Excellence (NICE). Guide to the Methods of Technology Appraisal 2013. https://www.nice.org.uk/process/pmg9/resources/guide-to-the-methods-of-technology-appraisal-2013-pdf-2007975843781 Accessed 15 Mar 2016.
Jönsson B. Changing health environment: the challenge to demonstrate cost-effectiveness of new compounds. PharmacoEconomics. 2004;22(Suppl 4):5–10.
World Health Oranisation. Cost effectiveness and strategic planning (WHO-CHOICE). http://www.who.int/choice/costs/CER_levels/en/. Accessed 14 Mar 2016.
Tarricone R. Valutazione economica: definizioni, principali tecniche di valutazione e ruolo della Budget Impact Analysis. Giornale Italiano di Farmacoeconomia e Farmacoutilizzazione. 2012;4(2):5–24.
Sonnenberg FA, Beck JR. Markov models in medical decision making: a practical guide. Med Decis Mak. 1993;13(4):322–38.
Gani R, Giovannoni G, Bates D, Kemball B, Hughes S, Kerrigan J. Cost-effectiveness analyses of Natalizumab (Tysabri®) compared with other disease-modifying therapies for people with highly active relapsing-remitting multiple sclerosis in the UK. PharmacoEconomics. 2008;26(7):617–27.
Peninsula Technology Assessment Group (PenTAG). The effectiveness and cost-effectiveness of natalizumab for multiple sclerosis: an evidence review of the submission from Biogen. Evidence Review Group Report commissioned by NHS R&D HTA Programme on behalf of: NICE. 2007. https://www.nice.org.uk/guidance/ta127/documents/multiple-sclerosis-natalizumab-evaluation-report-evidence-review-group-report2. Accessed 20 Apr 2016.
Fiore D, Hung TW, Cui Y, You X, Shang S, Scott T. ADVANCE phase 3 extension study (ATTAIN): Peginterferon Beta-a 125 mcg every 2 weeks demonstrated sustained efficacy in RRMS patients treated up to 5 years. AAN Annual Meeting. 2016;P4:010.
Kappos L, Kuhle J, Multanen J, Kremenchutzky M. Verdun di Cantogno E, Cornelisse P, Lehr L, Casset-Semanaz F, Issard D, Uitdehaag BM. Factors influencing long-term outcomes in relapsing-remitting multiple sclerosis: PRISMS-15. J Neurol Neurosurg Psychiatry. 2015;86(11):1202–7.
Ford C, Goodman AD, Johnson K, Kachuck N, Lindsey JW, Lisak R, et al. Continuous long-term immunomodulatory therapy in relapsing multiple sclerosis: results from the 15-year analysis of the US prospective open-label study of glatiramer acetate. Mult Scler. 2010;16(3):342–50.
Goodin DS, Reder AT, Ebers GC, Cutter G, Kremenchutzky M, Oger J, et al. Survival in MS: a randomized cohort study 21 years after the start of the pivotal IFNβ-1b trial. Neurology. 2012;78(17):1315–22.
Bermel RA, Weinstock-Guttman B, Bourdette D, Foulds P, You X, Rudick RA. Intramuscular interferon beta-1a therapy in patients with relapsing-remitting multiple sclerosis: a 15-year follow-up study. Mult Scler. 2010;16(5):588–96.
Weinshenker BG, Bass B, Rice GP, et al. The natural history of multiple sclerosis: a geographically based study. 2.Predictive value of the early clinical course. Brain 1989;112:1419–1428.
Weinshenker BG, Bass B, Rice GP, et al. The natural history of multiple sclerosis: a geographically based study. I. Clinical course and disability. Brain. 1989;112:133–46. http://dx.doi.org/10.1093/brain/112.1.133
Orme M, Kerrigan J, Tyas D, Russell N, Nixon R. The effect of disease, functional status, and relapses on the utility of people with multiple sclerosis in the UK. Value Health. 2007;10(1):54–60.
Tyas D, Kerrigan J, Russell N, Nixon R. The distribution of the cost of multiple sclerosis in the UK: how do costs vary by illness severity? Value Health. 2007;10(5):386–9.
Patzold U, Pocklington PR. Course of multiple sclerosis. First results of a prospective study carried out of 102 MS patients from 1976–1980. Acta Neurol Scand. 1982;65(4):248–66.
ISTAT. Annuario statistico italiano 2015. http://www.istat.it/it/archivio/171864. Accessed 4 Mar 2016.
Pokorski RJ. Long-term survival experience of patients with multiple sclerosis. J Insur Med. 1997;29(2):101–6.
Tolley K, Hutchinson M, You X, Wang P, Sperling B, Taneja A, et al. A network meta-analysis of efficacy and evaluation of safety of subcutaneous Pegylated interferon Beta-1a versus other Injectable therapies for the treatment of relapsing-remitting multiple sclerosis. PLoS One. 2015:1–21. doi:10.1371/journal.pone.0127960.
Lublin FD, Cofield SS, Cutter GR, Conwit R, Narayana PA, Nelson F, et al. Wolinsky JS; CombiRx investigators. Randomized study combining interferon and glatiramer acetate in multiple sclerosis. Ann Neurol. 2013;73(3):327–40.
Schwid SR, Panitch HS. Full results of the evidence of interferon dose–response-European north American comparative efficacy (EVIDENCE) study: a multicenter, randomized, assessor-blinded comparison of low-dose weekly versus high-dose, high-frequency interferon beta-1a for relapsing multiple sclerosis. Clin Ther. 2007;29(9):2031–48.
Durelli L, Verdun E, Barbero P, Bergui M, Versino E, Ghezzi A, et al. Zaffaroni M; independent comparison of interferon (INCOMIN) trial study group. Every-other-day interferon beta-1b versus once-weekly interferon beta-1a for multiple sclerosis: results of a 2-year prospective randomised multicentre study (INCOMIN). Lancet. 2002;359(9316):1453–60.
Calabrese M, Bernardi V, Atzori M, Mattisi I, Favaretto A, Rinaldi F, et al. Effect of disease-modifying drugs on cortical lesions and atrophy in relapsing-remitting multiple sclerosis. Mult Scler. 2012;18(4):418–24.
Etemadifar M, Janghorbani M, Shaygannejad V. Comparison of Betaferon, Avonex, and Rebif in treatment of relapsing-remitting multiple sclerosis. Acta Neurol Scand. 2006;113(5):283–7.
Ebers GCR, Lesaux G, Paty J, Oger D, Li J, Beall DKB, et al. Randomised double-blind placebo-controlled study of interferon (beta)-1a in relapsing/remitting multiple sclerosis. Lancet. 1998;352(9139):1498–504.
Cadavid D, Wolansky LJ, Skurnick J, Lincoln J, Cheriyan J, Szczepanowski K, et al. Efficacy of treatment of MS with IFNbeta-1b or glatiramer acetate by monthly brain MRI in the BECOME study. Neurology. 2009;72(23):1976–83.
O'Connor P, Filippi M, Arnason B, Comi G, Cook S, Goodin D, et al., BEYOND Study Group. 250 microg or 500 microg interferon beta-1b versus 20 mg glatiramer acetate in relapsing-remitting multiple sclerosis: a prospective, randomised, multicentre study. Lancet Neurol. 2009;8(10):889–97.
National Institute for Clinical Excellence (NICE). Natalizumab for the treatment of adults with highly active relapsing-remitting multiple sclerosis. NICE technology appraisal guidance [TA127], 2007. https://www.nice.org.uk/guidance/TA127. Accessed 25 May 2016.
Parsons S, Carnes D, Pincus T, Foster N, Breen A, Vogel S, et al. Measuring troublesomeness of chronic pain by location. BMC Musculoskelet Disord. 2006;7:34.
National Institute for Clinical Excellence (NICE). Depression in adults: recognition and management. NICE guidelines [CG90]. 2009. http://www.nice.org.uk/guidance/cg90. Accessed 11 May 2015.
National Institute for Clinical Excellence (NICE). Irritable bowel syndrome in adults: diagnosis and management. NICE guidelines [CG61]. 2008. http://www.nice.org.uk/guidance/cg61. Accessed 11 May 2015.
van Hoek AJ, Underwood A, Jit M, Miller E, Edmunds WJ. The impact of pandemic influenza H1N1 on health-related quality of life: a prospective population-based study. PLoS One. 2011;6:e17030. http://dx.doi.org/10.1371/journal.pone.0017030
R Emilia-Romagna. Assessorato Politiche per la Salute. Percorso regionale (Emilia-Romagna) di diagnosi e terapia della sclerosi multipla. Versione 1.1, maggio 2011. http://salute.regione.emilia-romagna.it/documentazione/ptr/elaborati/128_sclerosi_multipla.pdf. Accessed 17 Mar 2016.
Regione Lazio. Decreto del Commissario ad acta (delibera del Consiglio dei Ministri del 21 marzo 2013) N. U00386 del 13/11/2014. Percorso Diagnostico Terapeutico Assistenziale Sclerosi Multipla. http://www.teresapetrangolini.it/wordpress-4/wp-content/uploads/2014/11/Decreto_sclerosi-multipla_13112014.pdf. Accessed 17 Mar 2016.
MINISTERO DELLA SALUTE Remunerazione delle prestazioni di assistenza ospedaliera per acuti, assistenza ospedaliera di riabilitazione e di lungodegenza post acuzie e di assistenza specialistica ambulatoriale. DECRETO 18 ottobre 2012. Supplemento ordinario alla “Gazzetta Ufficiale„ n. 23 del 28 gennaio 2013 - Serie generale.
Garattini L, Castelnuovo E, Lanzeni D, Viscarra C. Durata e costo delle visite in medicina generale: il progetto DYSCO. Farmeconomia e Percorsi terapeutici. 2003;4(2):109–14.
Karampampa K, Gustavsson A, Miltenburger C, Teruzzi C, Fattore G. Treatment experience, burden and unmet needs (TRIBUNE) in MS study: results from Italy. Mult Scler. 2012;18(Suppl 2):29–34.
IMS Health. Aprile 2014 - Marzo 2015. Dati IMFO. ©IMS Health S.p.A. Tutti i diritti riservati.
Avonex Prescribing Information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/103628s5129s5177s5194s5224lbl.pdf. Accessed May 2016.
Plegridy Prescribing Information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/125499s000lbl.pdf. Accessed May 2016.
Rebif Prescribing Information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/103780s5178s5179lbl.pdf. Accessed May 2016.
Extavia Prescribing Information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/125290s0000lbl.pdf. Accessed May 2016.
Copaxone_Prescribing Information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/020622s057lbl.pdf. Accessed May 2016.
Betaferon_Prescribing Information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2015/103471s5186lbl.pdf. Accessed May 2016.
Furneri G, Scalone L, Ciampichini R, Cortesi PA, Fornari C, Madotto F, Chiodini V, Cesana G, Mantovani LG. Utilization of disease modifying agents in multiple sclerosis: analysis from an Italian administrative database. ISPOR 15th Annual European Congress. 2012.
Lee AW. Review of mixed treatment comparisons in published systematic reviews shows marked increase since 2009. J Clin Epidemiol. 2014;67(2):138–43.
Jansen JP, Fleurence R, Devine B, Itzler R, Barrett A, Hawkins N, et al. Interpreting indirect treatment comparisons and network meta-analysis for health-care decision making: report of the ISPOR task force on indirect treatment comparisons good research practices: part 1. Value Health. 2011;14(4):417–28.
Hoaglin DC, Hawkins N, Jansen JP, Scott DA, Itzler R, Cappelleri JC, et al. Conducting indirect-treatment-comparison and network-meta-analysis studies: report of the ISPOR task force on indirect treatment comparisons good research practices: part 2. Value Health. 2011;14(4):429–37.
Ivanova JI, Bergman RE, Birnbaum HG, Phillips AL, Stewart M, Meletiche DM. Impact of medication adherence to disease-modifying drugs on severe relapse, and direct and indirect costs among employees with multiple sclerosis in the US. J Med Econ. 2012;15(3):601–9.
Paolicelli D, D’Onghia M, Pellegrini F, Direnzo V, Iaffaldano P, Lavolpe V, et al. The impact of neutralizing antibodies on the risk of disease worsening in interferon b–treated relapsing multiple sclerosis: a 5 year post-marketing study. J Neurol. 2013;260(6):1562–8.
Paolicelli D, Iannazzo S, Santoni L, D’Onghia M, Direnzo V, Iaffaldano A, et al. The cost of patients with relapsing-remitting multiple sclerosis who develop Neutralising antibodies while treated with interferon Beta. Milano: ISPOR 2015. p. 2015.
Hernandez L, Guo S, Kinter E, Fay M. Cost-effectiveness analysis of peginterferon beta-1a compared with interferon beta-1a and glatiramer acetate in the treatment of relapsing-remitting multiple sclerosis in the United States. J Med Econ. Published online: 07 Mar 2016. Journal homepage: http://www.tandfonline.com/loi/ijme20
Data source: https://currency-conter.net/?gclid=CN2h_LnZmswCFRUTGwodElUEBg. Accessed 19 Apr 2016.
Hernandez L, Guo S, Toro-Diaz H, Carroll S, SFS F. Cost-effectiveness analysis of Peginterferon Beta-1a in the treatment of relapsing-remitting multiple sclerosis in Scotland. Milano: ISPOR 2015; 2015.
Hernandez L, Guo S, Toro-Diaz H, Carroll S, SFS F. Cost-effectiveness analysis of Peginterferon Beta-1a in the treatment of relapsing-remitting multiple sclerosis in Ireland. Milano: ISPOR 2015; 2015.
Acknowledgments
The authors thank Doctor Carlo Lucioni and Doctor Silvio Mazzi, professional pharmacoeconomists contracted to HPS (Health Publishing & Services Srl, Milan), for assistance in the preparation of the manuscript.
Funding
This manuscript was financially supported by Biogen Italia (Milan, Italy).
Availability of data and materials
Not applicable.
Authors’ contributions
All the authors are the same who published the two economic analyses [12, 13] which the present article is focused on. All authors read and approved the final manuscript.
Competing interests
• SI is a consultant that received fees by Biogen Italia for other projects
• DC is an Advisory Board member of Bayer Schering, Biogen, Merck-Serono, Teva and received honoraria for speaking or consultation fees from Almirall, Bayer Schering, Biogen, Genzyme, GW Pharmaceuticals, Merck Serono, Novartis, Sanofi-Aventis, Teva. He is also principal investigator in clinical trials for Bayer Schering, Biogen, Novartis, Merck Serono, Sanofi-Aventis, Teva
• PLC has received research grants, contributions and fees by the following pharmaceutical companies: Abbvie, Almirall, Amgen, A.C.R.A.F. – Angelini, Astellas, Astra Zeneca, Baxter, Bayer, Biogen, BioMarine, Bristol Mayers Squibb, Celgene, Chiesi, Daiichi Sankyo, Eli Lilly, Grunenthal, GSK, Hospira, Lundbeck, LeoPharma, Merck Serono, MSD, Menarini, Mundipharma, Novartis Consumer Health, Novartis Pharma, Otsuka, Pfizer, Roche, Sandoz, Sanofi, Sigma Tau, Takeda, Zambon
• LG received fee by Biogen Italia for other projects
• LS, CS, EP are employees of Biogen Italia
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Centonze, D., Iannazzo, S., Santoni, L. et al. The economic profile of peginterferon beta-1a in the treatment of relapsing-remitting multiple sclerosis in Italy. Mult Scler Demyelinating Disord 2, 13 (2017). https://doi.org/10.1186/s40893-017-0030-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40893-017-0030-6