Abstract
Background
Over many decades, the treatment of Dupuytren’s disease, a fibroproliferative disease of the hand, is the centre of various studies and publications. Surgical intervention has always been the method of choice, with fasciectomy being today’s state of the art. Nevertheless, researchers also focused on conservative non-operative treatment methods of which collagenase Clostridium histolyticum (CCH) turned out to be very promising. With the release of CCH under the name Xiapex in 2010, its use increased steadily. The aim of this work is to survey the current state of the treatment with CCH and the status of Xiapex treatment in Austria.
Methods
On behalf of the Division of Plastic, Aesthetic and Reconstructive Surgery at the Medical University of Graz, a questionnaire was sent out to departments and doctors in Austria that are treating Dupuytren’s disease. Based on this expert interrogation data concerning treating patterns, complications, outcome, etc. has been collected.
Results
The questionnaires were sent out since February 2016 and were evaluated until January 2017. Every single participant considered Xiapex to play an ‘integral part’ in the treatment of Dupuytren’s disease. According to 85%, the treatment of the MCP joint provides the highest success rate. Eighty-five percent indicated a faster return to work for patients being treated with collagenase than for those undergoing surgery.
Conclusion
The present work indicates a positive perception of treating patients suffering from Dupuytren’s disease with collagenase Clostridium histolyticum, respectively, Xiapex. It depicts this technique to be a widely accepted treatment method and a promising alternative to surgery. However, the call for further research is still present.
Similar content being viewed by others
Background
Dupuytren’s disease is a benign disease of the palmar fascia, a fibromatosis that was first mentioned in descriptions by Plater 400 years ago and later named after the French surgeon Baron Guillaume Dupuytren who lengthy described this disease in the 1830s.
Dupuytren’s contracture is the result of increased proliferation of myofibroblasts and collagen matrix organisation leading to a formation of nodules and cords and ultimately a flexion contracture of the thickened palmar fascia. Due to the progressive flexion of the fingers, especially in the metacarpophalangeal (MCP) and the proximal interphalangeal (PIP) joint, a normal function of the affected fingers and hand is severely restricted [1, 2].
Even today, the aetiology, pathophysiology and the ideal treatment have yet to be fully understood. Trauma, inflammation, ischemia, environmental factors, a genetic predisposition and a variable expression of proteins and growth factors in local tissue are all thought to be part of a multifactorial pathogenesis [1].
Dupuytren’s disease is most prevalent among elder men of Northern European descent and is thought to be inherited autosomal dominantly with variable penetrance [2, 3].
The treatment of Dupuytren’s contracture consists of various surgical techniques such as fasciectomy, dermofasciectomy, fasciotomy, or aponeurotomy or the less invasive percutaneous needle fasciotomy. Since the introduction of collagenase Clostridium histolyticum as a promising treatment method for Dupuytren’s contracture, there now exists an alternative minimal invasive, non-surgical treatment [1, 2].
Dupuytren’s contracture
Dupuytren’s contracture is a connective tissue disease affecting the palmar fascia and is listed under the superficial fibromatoses with the ICD-10 Code M72.0. Thus, it is also referred to as palmar fibromatosis. Fibromatoses emerge from fibrous proliferation, and due to their interaction with surrounding tissue are to be found in an intermediate position between benign fibrous tumours and fibrosarcomas. They are characterised by an infiltrative growth, a tendency for recurrence and the inability of metastasizing [4,5,6].
Epidemiology
Predominately Caucasian men of Northern European descent are affected. According to The Reykjavik Study, the prevalence of Dupuytren’s disease in the Icelandic population increased from 7.2% in 45- to 49-year-old men to 39.5% among those aged 70 to 74 years. Patients younger than 30 years rarely are affected [6,7,8].
In 5 to 20%, the fibromatosis of the palm and fingers is associated with fibromatous lesions of the planta pedis (plantar fibromatosis, Morbus Ledderhose), in 4% with a penile fibromatosis (induratio penis plastica, Peyronie’s disease) [6].
Aetiology and pathogenesis
A combination of various risk factors and a multifactorial pathogenesis are responsible for the development of Dupuytren’s disease. Especially, alcohol abuse and alcohol-induced liver diseases, smoking, diabetes, previous traumata of the hand and exposition to vibration are thought to play a role in the emergence of this disease. Furthermore, a genetic cause appears to have an impact as many affected patients show a significant family history. Various proteins appear to be a factor in the development of this disorder, such as the cytokine transforming growth factor-β (TGF-β) which has an impact on proliferation and differentiation of myofibroblasts. Further proteins are platelet-derived growth factor (PDGF), fibroblast growth factor (FGF), epidermal growth factor (EGF) and interleukin-1 (IL-1), as well as the cell matrix proteins Tenascin and Periostin that also affect differentiation, growth and contractility of myofibroblasts. However, the exact pathogenesis and pathology have yet to be decrypted [1, 9,10,11,12].
In the development of Dupuytren’s disease, the first asymptomatic manifestation is an isolated palmar nodule. It originates from fibroblast proliferation, myofibroblast differentiation and fibrosis of the superficial palmar aponeurosis. In the process of the disease, cordlike indurations or bands are being formed in between further nodules. This ultimately leads to skin pitting and thickening and a flexion contracture of the fingers [1, 6].
Prognosis
The diathesis for Dupuytren’s disease is described as a combination of various criteria such as Northern European descent, male sex, onset before age 50, one or more affected siblings or parents, bilateral manifestation and knuckle pads. The presence of one or more of these criteria indicates points towards an inferior prognosis and a higher recurrence rate. In case of all these factors being present, the risk for recurrence is 71% compared to 23% in patients without a risk factor [1].
Examination, diagnosis and classification
Patients usually approach a physician once the disease has already proceeded to an advanced and serious stage, and they are obviously handicapped in certain daily activities. The diagnosis is a clinical one and is made through inspection and palpation. Further, the angle of the palmar and digital contracture is measured by use of a goniometer (active and passive range of motion). A quick and useful test to stage the disease is the Hueston table top test. This test is positive when the patient is not able to put his or her hand flat on the table [1, 13,14,15].
Classification
Various classification models and assessment methods can be found in the existing literature. The typical classification is the Tubiana staging system that mainly focuses on the extension deficit. In this system, the hand is subdivided in five digito-palmar segments. The sum of the angles of the extension deficit in all three joints (MCP, PIP and DIP) of one longitudinal segment represents the total contracture, respectively, the total flexion deformity:
-
Stage 0: no lesion
-
Stage N: palmar nodule without finger contracture
-
Stage 1: total flexion deformity between 0° and 45°
-
Stage 2: total flexion deformity between 45° and 90°
-
Stage 3: total flexion deformity between 90° and 135°
-
Stage 4: total flexion deformity greater than 135° [16,17,18]
Another staging system is the Iselin classification (1951) that consists of five stages of Dupuytren’s contracture:
-
Stage 0: small nodules, no hand function disability
-
Stage 1: nodules and cords, slight contracture of the MCP
-
Stage 2: MCP flexion contracture up to 30° and early PIP involvement
-
Stage 3: interphalangeal joint contracture more than 30°
-
Stage 4: severe digital flexion contracture plus sensory and circulatory impairment [19, 20]
Treatment of Dupuytren’s contracture
Since the seventeenth century, various surgical techniques have been established and described. Since the last century, research focused particularly on non-surgical treatment options.
The most popular surgical techniques are fasciotomy, limited and radical fasciectomy, dermofasciectomy, the open-palm technique and the percutaneous needle aponeurotomy. Still, surgical intervention is the gold standard in the treatment of progressive Dupuytren’s disease and functionally impaired patients with contractures more than 30° in the MCP joint and an affected PIP joint [2, 14].
According to Bainbridge et al., the overall complication rate during surgery is at 4% with the most frequent being injury of nerves, arteries or the volar plate [21].
The most frequent postoperative complications are hematoma (8%), wound healing disorder or delay (6%), inflammation and infection (6%) and pain (6%) [21]. These are seen particularly in more invasive surgical techniques. Non-invasive treatment methods come with a lower complication rate compared to invasive interventions. However, their recurrence rate is inferior to invasive surgical methods.
Because of the interplay of genetic predisposition, environmental factors and its special pathophysiology, a surgical excision can never be curative [1,2,3, 21,22,23].
Alternative treatment options
Although surgical intervention has always been the method of choice in the treatment of Dupuytren’s disease, various conservative treatment options have been under investigation. Most of them, however, turned out to be inferior to surgery [10].
Attempts with the cytokine TNF as a therapeutic target or the application of interferon gamma should have led to the inhibition of fibroblast and collagen proliferation. Further injections with the steroid Triamcinolon Acetonide into affected cords has brought some promising results, as shown in a study by Ketchum et al. in which a regression of nodules (flattening and softening) was achieved. However, this technique is accompanied with certain adverse effects, such as a depigmentation or temporary subcutaneous atrophy at the site of the injection and a recurrence rate of 50% [14, 24,25,26,27,28]. Also, the impact of radiotherapy and shockwave therapy on Dupuytren’s contracture has been investigated [14, 29,30,31,32]. A target for future therapies could be the dysregulation of IGF-II and IGFBP-6 in the development of Dupuytren’s disease as well as metalloproteases [33, 34].
In the year 2010, however, a very promising, minimal invasive and non-operative treatment option has been approved by the US FDA: the treatment with the enzyme collagenase Clostridium histolyticum. It was later released under the name of Xiaflex, respectively, Xiapex in Europe and has also been introduced in the treatment of Dupuytren’s contracture in Austria [2].
Treatment with collagenase Clostridium histolyticum
Collagenases are zinc-dependent matrix metalloproteases produced by clostridial bacterial species and are able to cleave collagen, an insoluble matrix protein consisting of three polypeptide helices. The proteases are subdivided into two classes: collagenase class I attacks the terminal end of the collagen molecule, class II cleaves inner sections [35].
This new minimal invasive, non-surgical treatment option for Dupuytren’s contracture does not require anaesthesia and can be performed in the doctor’s office.
At first, the Xiapex powder (0.58 mg of collagenase Clostridium histolyticum (CCH)) is diluted in the supplied Ca2+-containing diluent (0.39 ml in MCP, 0.31 ml in PIP joints). Where the affected cord is least adhered to the skin, it is then punctured three times in three contiguous areas. Twenty-four hours (up to 1 week) after the injections, a passive finger extension is performed under local anaesthesia to rupture the affected cord according to a four-step manipulation technique.
The patients may return to daily activities right away. For a better outcome, they are instructed to wear a night splint for up to 4 months and perform daily extension and flexion exercises. Follow-up visits take place on the 1st, 7th and 30th day after the injection [35,36,37,38].
Although one positive aspect of the treatment with CCH is its low complication rate compared to invasive treatment methods, a notable risk for specific adverse events does exist. Most common complications are contusion, hematoma, pain, swelling and itching on the injection site and peripheral oedema. Severe adverse events are nerve injury and flexion tendon rupture [39].
Various studies have described the outcome of collagenase treatment as beneficial, especially in terms of patient satisfaction due to the simplicity of the procedure and the quick recovery of full hand function [40, 41].
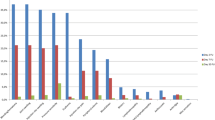
Concerning procedure frequencies of various treatment options, the number of CCH procedures has steadily increased since its release in 2010 [42].
The aim of the present work is to evaluate the status of the treatment of Dupuytren’s contracture with collagenase Clostridium histolyticum in Austria.
Methods
The evaluation of the status of Xiapex treatment in Austria was conducted on the basis of an expert survey by use of a questionnaire (Fig. 1). Starting in February 2016, the questionnaires were sent out by the Division of Plastic, Aesthetic and Reconstructive Surgery at the Medical University of Graz to 100 hospitals, medical centres and doctor’s offices in Austria. After a 2-month response period, the collected data was evaluated.
Inclusion criteria for respondents were that the doctors were specialised hand surgeons, plastic surgeons or orthopaedists who encounter Dupuytren’s contracture on a regular basis.
At first, participants were asked for their name, department and name and location of the facility. All data was of course anonymized and treated confidentially. In the following, the doctors were asked 15 questions concerning Xiapex treatment consisting of yes–no questions, single and multiple choice questions as well as open questions. Some of the questions contain an ancillary question.
Statistical analysis
A descriptive analysis and presentation of data were conducted.
Results
In total, 100 questionnaires were sent out to hospitals, medical centres and doctors with a response rate of 25%.
One hundred percent of participants declare the treatment with Xiapex as a fixture in the treatment of Dupuytren’s contracture (Fig. 2).
The total number of patients treated by the polled physicians was 1697. In 2% (n = 35) of these patients, an affected cord needed to be infiltrated more than once. According to 90% of the participating doctors, the most frequently noted adverse events were bleeding, pain, swelling, tenderness and haematoma. Eighty-five percent thought skin tears to be quite common. As for 45% of the doctors, lymph node swelling and lymphangitis were frequent events. Forty percent of the doctors noticed joint swelling and pain and 25% efflorescence of the skin. Fifteen percent of the participating surgeons thought pruritus to be a common adverse event. Only 5% observed tendon rupture.
Sixty-five percent of the polled physicians evaluate treatment success by means of objectifiable techniques and methods. Primarily, the doctors take measurement by use of a goniometer. For time between injection and cord rupture, 65% of the participants wait 1 day, 35% wait 2 days or more. Thirty percent infiltrate one cord per therapy session and 60% two cords. Ten percent did not give an answer to that question.
Asked how many cords needed to be affected for surgeons to favour surgery over treatment with Xiapex, 30% said two cords and 60% three cords. Ten percent did not give an answer to that question. Ninety-five percent of the doctors deny the question if there was a longer follow-up care period after treating with Xiapex compared to surgery.
Twenty percent of the participants stated a lower recurrence after Xiapex treatment compared to surgical options. Seventy-five percent, however, did not make that observation. Five percent did not give an answer to that question.
Asked about patient satisfaction and if it was higher with Xiapex treatment in comparison to surgery, 85% of participating doctors answered in the affirmative, whereas 15% denied this question (Fig. 3).
Eighty-five percent stated that treatment success is depending on which joint is affected. Of these 85%, every single one considers treatment success to be greater in the MCP joint than in the PIP joint.
When questioned about which setting the participants prefer, 40% stated to perform the intervention in an outpatient setting and 25% in the day clinic. Thirty-five percent favour an inpatient procedure in the hospital. Most frequent explanation for outpatient or day clinic procedures was accounting-related and organisational benefits.
According to 85% of the polled doctors, patients treated with Xiapex returned to work earlier than those who underwent surgery. Fifteen percent disagreed (Fig. 4).
Asked about whether there was sufficient evidence for the Xiapex infiltration therapy, 90% approved. In total, however, 30% of the questionnaire’s participants wish for further studies and research on issues such as long-term results, recurrence rate, cost and health economic studies, duration of sick leave and the need for physiotherapy.
Discussion
Several conclusions about the status of collagenase treatment in Austria can be drawn from the answers and result of the questionnaire in the present work.
Already, the results to question number 1 show an unambiguous trend as 100% of the questionnaire participants consider Xiapex an important armamentarium in the treatment of Dupuytren’s contracture. This is also seen in several other studies, including a work by Zhao et al. (2016) showing the increase of the trend line of collagenase treatment since its release, whereas the number of surgical encounters is decreasing [42].
The answers to the most frequent adverse events and side effects (90% of the participants observed bleeding, pain, swelling, tenderness and haematoma, 85% skin tears, 45% lymph node swelling and lymphangitis, 40% joint swelling and pain, 25% efflorescence of the skin, 15% pruritus and 5% tendon rupture) are also comparable with the existing literature such as the CORD I and II studies [35, 36, 39].
Sixty-five percent of the polled physicians evaluate treatment success by means of objectifiable techniques and methods. Primarily, the doctors take measurements by use of a goniometer. This is also seen in several studies including the ones by Gilpin et al. (2010) and Peimer et al. (2013), in which the range of motion (ROM) was one of the most important postoperative outcome measures [3, 36, 43].
Of all 1697 patients treated by the questionnaire participants, in 2% (n = 25), the same cord needed to be infiltrated twice. According to literature, the injection can be repeated up to three times at 30-day intervals [3, 36].
Asked about time between injection and cord rupture, 65% of the participants wait 1 day and 35% wait 2 days or more. The majority of the studies taken into account confirm our result, as usually the cord is ruptured 24 h postinjection [35].
Thirty percent of the participants infiltrate one cord per therapy session, 60% two cords. According to Gaston et al., treatment of two cords per therapy session is easily possible without an increase in complication rate [44].
The question how many cords needed to be affected for surgeons to favour surgery over treatment with Xiapex was answered with two cords by 30% and three cords by 60%. The established literature as well as the European Medicines Agency (EMA) and the Xiapex-producing company itself declare two cords per therapy session as the maximum [44,45,46].
Ninety-five percent of the participating physicians deny the question about collagenase therapy requiring a longer follow-up care compared to surgical methods. This answer is quite comprehensible since invasive approaches lead to much bigger wounds and a higher infection risk, respectively, require multiple bandage changes as well as the removal of the stitches. Gilpin et al. (2010) and several other publications scheduled their patients for three visits on the 1st, 7th and 30th day postinjection. Additionally, the patients were told to wear a night splint and perform daily flexion and extension exercises at home for the next 4 months [35,36,37,38].
In our study, 20% of the questionnaire’s participants observed a lower recurrence rate in Xiapex treatment in comparison with surgery. According to Henry (2014), however, the recurrence rate in minimal-invasive procedures, albeit their many advantages, is by far higher compared to surgical methods, especially fasciectomy [3].
A vast majority of the polled surgeons (85%) stated a higher patient satisfaction in Xiapex treatment than in surgical approaches. The less complex procedure, less complications and adverse events and a faster return of hand function and return to work are definite benefits of the Xiapex therapy. Among others, Zhou et al. report a higher patient satisfaction concerning, for example, strength and sensation 6 to 12 weeks after CCH therapy compared to fasciectomy [40, 47].
Eighty-five percent stated that treatment success is depending on which joint is affected. All of these 85% consider treatment of the MCP joint more promising than treatment of the PIP joint. These results mostly fall in line with the existing literature. Hurst et al. (2009) show a decisive superiority of the MCP location regarding clinical improvement or contracture reduction. Peimer et al. displayed the benefit of the MCP location concerning recurrence rate in their CORDLESS study [3, 35, 38, 48].
Asked about which setting the participants prefer, 40% stated to perform the intervention in an outpatient setting and 25% in the day clinic. Thirty-five percent favour an inpatient procedure in the hospital. The most frequent explanation for outpatient or day clinic procedures was accounting-related and organisational benefits. Because of the minimal-invasive procedures and thus the possibility of performing the treatment in an outpatient setting, Xiapex therapy represents a cost-effective alternative to surgery. Therefore, also in existing literature, there is mostly talk of outpatient procedures [49, 50].
According to 85% of the polled surgeons, patients treated with Xiapex returned to work earlier than those who underwent surgery, while 15% disagreed. A study by Naam et al. (2014) is showing similar results with average return-to-work after Xiapex therapy was at 1.9 days, whereas it was 37.4 days following fasciectomy [51].
Although the majority (90%) of the participants thought there was sufficient evidence for the infiltration therapy with Xiapex, still 30% requested further studies and research on issues such as long-term results, recurrence rate, cost and health economic studies, duration of sick leave and the need for physiotherapy. This result is in line with most of the literature, where publications call for further studies in a specific topic concerning treatment of Dupuytren’s disease with Xiapex. Thus, for example, Thomas and Bayat (2010) postulate further data on long-term results, recurrence rate and complications, whereas Ball et al. (2016) demand clear definitions of the disorder or objective, reproducible methods for outcome measurement [19, 35].
A publication similar to the present work concerning the state of the treatment of Dupuytren’s contracture with collagenase Clostridium histolyticum or Xiapex in Austria using an expert survey could not be found when searching PubMed. The international study The Impact of Collagenase Clostridium histolyticum Introduction on Dupuytren Treatment Patterns in the United States by Zhao et al. (2016) is comparable to the present one and showed similar results. However, Zhao et al. used a database to collect the data to evaluate the impact of collagenase treatment in the USA, whereas the present study uses a questionnaire for data collection.
Several results in this study reveal a certain discordance in treatment modalities, especially seen in the questions about time between injection and rupture, number of fingers treated per session and number of affected fingers per hand for favouring surgery over collagenase injection. Also, the fact that only 65% of the questionnaire’s participants evaluate treatment success by use of objectifiable methods shows that there is no consistent and standardised approach for classification and evaluation. As it can be also taken from the results to the last question in the survey, there is still a call and a necessity for further studies on various aspects of Dupuytren’s contracture, such as its development, its pathophysiology, the ideal treatment and follow-up care.
Conclusion
The benefits of collagenase Clostridium histolyticum for the treatment of Dupuytren’s contracture when compared to traditional treatment options are well known and established in existing literature. Aspects, such as a lower complication rate, a quicker return to work and a higher patient satisfaction, show the superiority of this technique. Especially patients with one or two palpable cords and a flexion in the MCP and/or the PIP of more than 20° (Tubiana stages I and II) benefit the most from Xiapex treatment.
This study was able to show the impact of collagenase treatment and its role as an important armamentarium in the treatment spectrum of Dupuytren’s contracture in Austria.
Abbreviations
- CCH:
-
Collagenase Clostridium histolyticum
- DIP:
-
Distal interphalangeal joint
- EGF:
-
Epidermal growth factor
- EMA:
-
European Medicines Agency
- FGF:
-
Fibroblast growth factor
- IGFBP-6:
-
Insulin-like growth factor-binding protein 6
- IGF-II:
-
Insulin-like growth factor 2
- IL-1:
-
Interleukin 1
- MCP:
-
Metacarpophalangeal joint
- PDGF:
-
Platelet-derived growth factor
- PIP:
-
Proximal interphalangeal joint
- ROM:
-
Range of motion
- TGF-β:
-
Transforming growth factor-β
- TNF:
-
Tumour necrosis factor
- US FDA:
-
United States Food and Drug Administration
References
Black EM, Blazar PE. Dupuytren disease: an evolving understanding of an age-old disease. J Am Acad Orthop Surg. 2011;19:746–57.
Desai SS, Hentz VR. The treatment of Dupuytren disease. J Hand Surg. 2011;36(5):936–42. doi: https://doi.org/10.1016/j.jhsa.2011.03.002
Henry M. Dupuytren’s disease: current state of the art. Hand. 2014;9(1):1–8. doi: https://doi.org/10.1007/s11552-013-9563-0
Böcker W, Denk H, Heitz PU, Höfler G, Kreipe H, Moch H, et al. Pathologie. 5., vollst. Elsevier, Urban & Fischer: München; 2012.
Riede U-N, Bianchi L. Allgemeine und spezielle Pathologie. 5., komple. Stuttgart: Thieme; 2004. p. 1174f.
Fletcher CDM, K. Unni FM. World Health Organization classification of tumours pathology and genetics of tumours of soft tissue and bone. Cancer. 2002;177(3):81f.
Gudmundsson KG, Arngrímsson R, Sigfússon N, Björnsson Á, Jónsson T. Epidemiology of Dupuytren’s disease: clinical, serological, and social assessment. The Reykjavik Study. J Clin Epidemiol. 2000;53(3):291–6.
McFarlane RM. On the origin and spread of Dupuytren’s disease. J Hand Surg. 2002;27(3):385–90.
Larsen S, Krogsgaard DG, Larsen LA, Iachina M, Skytthe A, Frederiksen H. Genetic and environmental influences in Dupuytren’s disease: a study of 30,330 Danish twin pairs. J Hand Surg (European Volume). 2015;40(2):171–6.
Rehman S, Goodacre R, Day PJ, Bayat A, Westerhoff HV. Dupuytren’s: a systems biology disease. Arthritis Res Ther. 2011;13(5):238.
Forrester HB, Temple-Smith P, Ham S, de Kretser D, Southwick G, Sprung CN. Genome-wide analysis using exon arrays demonstrates an important role for expression of extra-cellular matrix, fibrotic control and tissue remodelling genes in Dupuytren’s disease. PLoS One. 2013;8(3):e59056.
BURKE FD, PROUD G, LAWSON IJ, MCGEOCH KL, MILES JNV. An assessment of the effects of exposure to vibration, smoking, alcohol and diabetes on the prevalence of Dupuytren’s disease in 97,537 miners. J Hand Surg (European Volume). 2007;32(4):400–6.
Guilhen TA, Vieira ABM, de Castro MC, Hirata HH, Machado IR. Evaluation of surgical treatment of Dupuytren’s disease by modified open palm technique. Rev Bras Ortop (English Edition). Sociedade Brasileira de Ortopedia e Traumatologia. 2014;49(1):31–6.
Mafi R, Hindocha S, Khan WS. Recent surgical and medical advances in the treatment of Dupuytren’s disease—a systematic review of the literature. Open Orthop J. 2012;6(1):77–82.
Bayat A, McGrouther DA. Management of Dupuytren’s disease—clear advice for an elusive condition. Ann R Coll Surg Engl. 2006;88(1):3–8.
Tubiana R. Evaluation of deformities in Dupuytren’s disease. Ann Chir Main. 1986;5(1):5–11.
Tubiana R. Dupuytren’s disease of the radial side of the hand. Hand Clin. 1999;15(1):149–59.
Hindocha S, Stanley JK, Watson JS, Bayat A. Revised Tubiana’s staging system for assessment of disease severity in Dupuytren’s disease-preliminary clinical findings. Hand (New York, NY). 2008;3(2):80–6.
Ball C, Verjee LS, Izadi D, Nanchahal J. A systematic review of non-surgical treatments for early dupuytren’s disease. Hand Ther BMC Musculoskelet Disord. 2016;21(1):39.
ISELIN M, DIECKMANN G. Our experiences in the treatment of Dupuytren’s disease. Mem Acad Chir(France). France. 1951;77(8–9):251–5.
Bainbridge C, Dahlin LB, Szczypa PP, Cappelleri JC, Guérin D, Gerber RA. Current trends in the surgical management of Dupuytren’s disease in Europe: an analysis of patient charts. Eur Orthop Traumatol. 2012;3(1):31–41.
Becker GW, Davis TRC. The outcome of surgical treatments for primary Dupuytren’s disease—a systematic review. J Hand Surg Eur Vol. 2010;35(8):623–6.
Denkler K. Surgical complications associated with fasciectomy for Dupuytren’s disease: a 20-year review of the English literature. Eplasty. 2010;10:e15.
Ketchum LD, Donahue TK. The injection of nodules of Dupuytren’s disease with triamcinolone acetonide. J Hand Surg. 2000;25(6):1157–62.
Trojian TH, Chu SM. Dupuytren’s disease: diagnosis and treatment. Am Fam Physician. 2007;76(1):86–9.
McMillan C, Binhammer P. Steroid injection and needle aponeurotomy for Dupuytren disease: long-term follow-up of a randomized controlled trial. J Hand Surg. 2014;39(10):1942–7.
Tanaka K, Sano K, Yuba K, Katsumura K, Nakano T, Tanaka K, et al. Inhibition of induction of myofibroblasts by interferon γ in a human fibroblast cell line. Int Immunopharmacol. 2003;3(9):1273–80.
Verjee LS, Verhoekx JSN, Chan JKK, Krausgruber T, Nicolaidou V, Izadi D, et al. Unraveling the signaling pathways promoting fibrosis in Dupuytren’s disease reveals TNF as a therapeutic target. Proc Natl Acad Sci U S A. 2013;110(10):E928–37.
Adamietz B, Keilholz L, Grünert J, Sauer R. Radiotherapy of early stage Dupuytren disease. Long-term results after a median follow-up period of 10 years. Strahlenther Onkol. 2001;177(11):604–10.
Betz N, Ott OJ, Adamietz B, Sauer R, Fietkau R, Keilholz L. Radiotherapy in early-stage dupuytren’s contracture long-term results after 13 years. Strahlenther Onkol. 2010;186(2):82–90.
Zirbs M, Anzeneder T, Bruckbauer H, Hofmann H, Brockow K, Ring J, et al. Radiotherapy with soft X-rays in Dupuytren’s disease—successful, well-tolerated and satisfying. J Eur Acad Dermatol Venereol. 2015;29(5):904–11.
Knobloch K, Kuehn M, Vogt PM. Focused extracorporeal shockwave therapy in Dupuytren’s disease—a hypothesis. Med Hypotheses. 2011;76(5):635–7.
Raykha C, Crawford J, Gan BS, Fu P, Bach LA, O’Gorman DB. IGF-II and IGFBP-6 regulate cellular contractility and proliferation in Dupuytren’s disease. Biochim Biophys Acta Mol basis Dis. 2013;1832(10):1511–9.
Wilkinson JM, Davidson RK, Swingler TE, Jones ER, Corps AN, Johnston P, et al. Biochimica et Biophysica Acta MMP-14 and MMP-2 are key metalloproteases in Dupuytren ’ s disease fi broblast-mediated contraction. BBA Mol Basis Dis. Elsevier B.V. 2012;1822(6):897–905.
Thomas A, Bayat A. The emerging role of Clostridium histolyticum collagenase in the treatment of Dupuytren disease. Ther Clin Risk Manag. 2010;6:557–72.
Gilpin D, Coleman S, Hall S, Houston A, Karrasch J, Jones N. Injectable collagenase clostridium histolyticum: a new nonsurgical treatment for Dupuytren’s disease. J Hand SurgElsevier Inc. 2010;35(12):2027–2038. e1.
Meals RA, Hentz VR. Technical tips for collagenase injection treatment for dupuytren contracture. J Hand SurgElsevier Inc. 2014;39(6):1195–1200.e2.
Hurst LC, Badalamente M a, Hentz VR, Hotchkiss RN, Kaplan FTD, Meals R a, et al. Injectable collagenase clostridium histolyticum for Dupuytren’s contracture. N Engl J Med 2009;361(10):968–979.
Badalamente MA, Hurst LC, Benhaim P, Cohen BM. Efficacy and safety of collagenase clostridium histolyticum in the treatment of proximal interphalangeal joints in Dupuytren contracture: combined analysis of 4 Phase 3 clinical trials. J Hand Surg. Elsevier Inc. 2015;40(5):975–83.
Bradley J, Warwick D. Patient satisfaction with collagenase. J Hand Surg. Elsevier Inc. 2016;41(6):689–97.
Watt AJ, Curtin CM, Hentz VR. Collagenase injection as nonsurgical treatment of Dupuytren’s disease: 8-year follow-up. J Hand Surg. Elsevier Inc. 2010;35(4):534–539.e1.
Zhao JZ, Hadley S, Floyd E, Earp BE, Blazar PE, Cline H, et al. The impact of collagenase Clostridium histolyticum introduction on Dupuytren treatment patterns in the United States. J Hand Surg. 2016;41(10):963–68. Elsevier Inc.
Peimer CA, Skodny P, Mackowiak JI. Collagenase clostridium histolyticum for dupuytren contracture: patterns of use and effectiveness in clinical practice. J Hand Surg. 2013;38(12):2370–6.
Glenn Gaston R, Larsen SE, Pess GM, Coleman S, Dean B, Cohen BM, et al. The efficacy and safety of concurrent collagenase clostridium histolyticum injections for 2 dupuytren contractures in the same hand: a prospective, multicenter study. J Hand Surg. Elsevier Inc. 2015;40(10):1963–71.
European Medicines Agency - Human medicines - Xiapex. 2016 [cited 2017 Mar 10]. Available from: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/002048/human_med_001423.jsp&mid=WC0b01ac058001d125#product-info
Xiapex - Simple, injectable procedure. 2016 [cited 2017 Mar 10]; Available from: http://www.xiapex.eu/about-xiapex/administration-preparation/
Zhou C, Hovius SER, Slijper HP, Feitz R, Van Nieuwenhoven CA., Pieters HJ, et al. Collagenase clostridium histolyticum versus limited fasciectomy for Dupuytren’s contracture. Plast Reconstr Surg. 2015;136(1):87–97.
Peimer CA, Blazar P, Coleman S, Kaplan FTD, Smith T, Tursi JP, et al. Dupuytren contracture recurrence following treatment with collagenase clostridium histolyticum (CORDLESS Study): 3-year data. J Hand Surg. Elsevier Inc. 2013;38(1):12–22.
Degreef I. Collagenase treatment in Dupuytren contractures: a review of the current state versus future needs. Rheumatol Ther. Springer Healthcare; 2016;3(FEBRUARY):43–51.
Mehta S, HJCR B. A single-centre cost comparison analysis of collagenase injection versus surgical fasciectomy for Dupuytren’s contracture of the hand. J Plast Reconstr Aesthet Surg. Elsevier Ltd. 2014;67(3):368–72.
Naam NH. Functional outcome of collagenase injections compared with fasciectomy in treatment of Dupuytren’s contracture. Hand. 2013;8(4):410–6.
Acknowledgements
Not applicable.
Funding
Not applicable.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Altziebler, J., Hubmer, M., Parvizi, D. et al. Dupuytren’s contracture: the status and impact of collagenase Clostridium histolyticum treatment in Austria. Saf Health 3, 12 (2017). https://doi.org/10.1186/s40886-017-0063-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40886-017-0063-8