Abstract
Hypertension is an important modifiable risk factor for morbidity and mortality associated with cardiovascular disease. The incidence of hypertension is increasing not only in Korea but also in many Western countries due to the aging of the population and the increase in unhealthy lifestyles. However, hypertension control rates remain low due to poor adherence to antihypertensive medications, low awareness of hypertension, and numerous factors that contribute to hypertension, including diet, environment, lifestyle, obesity, and genetics. Because artificial intelligence (AI) involves data-driven algorithms, AI is an asset to understanding chronic diseases that are influenced by multiple factors, such as hypertension. Although several hypertension studies using AI have been published recently, most are exploratory descriptive studies that are often difficult for clinicians to understand and have little clinical relevance. This review aims to provide a clinician-centered perspective on AI by showing recent studies on the relevance of AI for patients with hypertension. The review is organized into sections on blood pressure measurement and hypertension diagnosis, prognosis, and management.
Graphical Abstract

Similar content being viewed by others
Introduction
Hypertension is a highly prevalent chronic disease affecting approximately 1.28 billion people worldwide [1]. Despite increases in awareness and treatment rates, hypertension and its complications are still a significant clinical burden [1, 2]. This may be because hypertension is a heterogeneous phenotype caused by many factors, including age, sex, body mass index, lipid profiles, personal habits (stress, smoking, physical activity, etc.), socioeconomic status, environment, and genetics [2,3,4].
Artificial intelligence (AI) may represent a breakthrough in understanding and treating hypertension and an important tool for overcoming the current problems associated with managing patients with hypertension. AI is increasingly impacting our daily lives, not only in the areas of advertising, finance, law, and education but also in medicine, where AI technologies are now being applied to the field of hypertension. However, AI research is limited to exploratory techniques with minimal clinical implications and can be difficult to understand for clinicians who are not experts in machine learning (ML) or deep learning (DL).
Before generating this review article, we conducted a detailed search of journal databases, including PubMed, EMBASE, and Web of Science, for applications of AI in hypertension from 2015 to 2023. Search terms included AI, artificial neural network, DL, ML, hypertension, blood pressure (BP), and BP measurement. We included clinical trials involving hypertensive patients rather than healthy individuals. To narrow our focus, we excluded exploratory technical studies, validation studies, and community-based primary health care studies. In this article, we review recently published studies of AI applications to BP measurement, hypertension diagnosis and prognostication, and management of hypertensive patients to clarify the current clinical implications of AI in hypertension from a clinician-centered perspective.
Clinical implications of AI
BP measurement
Accurate BP measurement is a cornerstone of hypertension diagnosis and management. The originally recommended method for measuring BP is the oscilloscopic method [2]. Noninvasive BP estimation devices include the traditional sphygmomanometer using an inflatable cuff, stethoscope, and manometer using Korotkoff sound, which was introduced in 1905 [5, 6]. Nevertheless, it is difficult and time consuming to measure BP. Moreover, oscilloscopic measurement has significant interoperator differences. Compared to the conventional oscilloscopic method, automatic monitors have become popular in recent years because they can easily measure BP and can be used to measure BP at home. Home BP monitoring can be the key to better BP control [7]. To improve the accuracy of BP measurement, many new algorithms or devices have been developed using AI technology to improve the precision, accuracy, and reproducibility of BP measurement. Automatic noninvasive BP estimation devices can be divided into oscillometric, auscultatory, and cuffless methods.
AI algorithms have been used for many years to improve the accuracy of BP measurement with automatic oscillometric BP monitors, and several experimental studies on the performance of these algorithms have been published recently [8]. In several clinical studies, auscultatory waveform studies have been published mainly for inflated cuff-based BP measurement [9]. Furthermore, Chu et al. [10] developed a smartphone app with an auscultatory waveform analysis algorithm to simultaneously evaluate the accuracy of an automated oscillometric BP device.
Recently, noninvasive automated cuff-less BP monitors have been developed and are commercially available [11]. Various methods have been proposed for cuff-less BP estimation, including methods based on the pulse transit time (PTT) and the pulse arrival time (PAT) using photoplethysmograms (PPGs) and electrocardiograms (ECGs) [12, 13]. A PPG is a noninvasive optical recording used to detect changes in blood volume in tissue, particularly in the microvascular bed. The PPG sensor detects changes in the amount of transmitted or reflected light and generates a PPG waveform. The volume and dilation of the arteries can be related to the pressure in the arteries, so the PPG signal produces a pulse waveform similar to the pressure waveform produced by a tonometer. The collected signal and data can be fed into an ML model to obtain estimates of SBP and DBP from the raw signal [13].
The PAT is more commonly used to describe the time from the R-wave of the ECG to the arrival of the arterial pulse at the peripheral site. The PTT, on the other hand, is a more general concept that includes the time it takes for the pulse to travel between two selected points. It is well known that there is a positive correlation between the PTT or PAT and BP because arterial stiffening resulting from increased BP leads to a rise in the pulse wave velocity and a decrease in the PTT [12,13,14]. These methods are used in cuff-less noninvasive automated BP monitors, which are suitable for taking measurements at any time and can be used for continuous monitoring.
Recently, several clinical studies of multiple DL algorithms for BP estimation using PPGs [15], calibration-free measurement [16], smartphone apps [17, 18], and wrist-worn cuff-less devices [19, 20] have been published. In one study, retinal fundus photographs were used to measure BP, rather than the presence of complications of hypertension, but the accuracy was not as good as a direct BP measurement [21]. Nevertheless, the fact that BP can be measured with imaging data is an example of how various methods of BP measurement may be tested in the future (Table 1).
Diagnosing hypertension
Many studies have been published using AI to diagnose [22, 23] or predict the occurrence of hypertension [24,25,26] in the general population. As this article focuses on studies in hypertensive patients, recent studies that have attempted to use AI to identify subtypes of hypertension in hypertensive patients were reviewed (Table 2).
BP variability (BPV) is known to be an independent risk factor for cardiovascular disease (CVD), but the diagnostic criteria are vague. Tsoi et al. [27] reanalyzed previous randomized controlled trials, including the SPRINT trial, and established patient clusters based on low, medium, and high BPV levels using traditional quantile clustering and 5 ML algorithms. K-means clustering showed the most stable and reliable results. It showed that approximately one-seventh of the population with a high level of BPV correlated with a higher risk of stroke and heart failure [27]. BPV data are time series and address different time scales; thus, Koshimizu et al. [28] predicted BPV using a multi-input multi-output deep neural network. The dataset in this study included cardiovascular risk factors and home BP readings every day for 2 years or more.
Recent studies have shown that DL or ML algorithms can be used to diagnose clinically important conditions such as masked uncontrolled hypertension or secondary hypertension using not only big data from electronic health records (EHRs) but also easily identified clinical features such as office BP, pulse pressure, use of beta-blocker, and high-density lipoprotein-cholesterol (HDL-C) level [29, 30]. Furthermore, there have been several attempts to diagnose hypertension using the amplitude and voltage of ECG waves [23, 31] (Fig. 1).
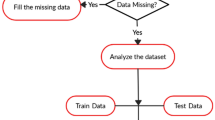
Big data commonly used in each category of hypertension research, and the algorithms that use it to implement individualized approaches for hypertensive patients. BP, blood pressure; CVD, cardiovascular disease; DNN, deep neural network; ECG, electrocardiography; EHRs, electronic health records; LSTM, long short-term memory; PPG, photoplethysmogram; RCT, randomized controlled trial; SVM, support vector machine; XGboost, extreme gradient boost
Prediction of prognosis in hypertensive patients
As BP is a complex multifactorial phenotype that is influenced by many factors, including genomic, demographic, lifestyle and environmental factors, the prognosis of hypertensive patients is also influenced by many factors. In analyzing multimodal data, AI provides the opportunity to conduct integrated analyses of hypertension as a newer analytic method and provides more insight into the prognosis and risk stratification of hypertensive patients [32, 33]. Louca et al. [34] analyzed the multimodal data from TwinsUK with concurrent BP, metabolomics, genomics, biochemical measures, and dietary data. The features tested in this study were then probed using the same algorithm in an independent dataset of 2,807 individuals from the Qatar Biobank. They found that the most predictive features of BP are the traditional risk factors, metabolites, and diet, while genetics (single nucleotide polymorphisms) did not appear to play a major role in predicting prognosis.
Several studies have shown that ML algorithms are better in the prediction of the 10-year risk of cardiovascular events than an established risk prediction approach such as the Framingham score or ACC/AHA CVD Risk Calculator (Table 3) [35,36,37,38,39].
The features most strongly associated with CVD vary across studies, depending on the algorithm or input dataset. Lee et al. [39] reported characteristics such as age, sex, income, body mass index, BP, smoking, physical activity, lipid profile, and fasting plasma glucose level associated with CVD. Lacson et al. [40] reported that age, the urine albumin/creatinine ratio, the estimated glomerular filtration rate, serum creatinine, history of subclinical CVD, total cholesterol, a variable representing time-series SBP signals using wavelet transformation on HDL‐C, the 90th percentile SBP, and triglyceride were significantly associated with CVD. Wu et al. [30] extended predictions from CVD to end‐stage renal disease and all‐cause mortality in 508 young patients by using several clinical variables, namely, the left atrial diameter, HDL‐C level, cholesterol level, big endothelin‐1 level, right arm DBP, right leg SBP, left leg SBP, right leg DBP, left arm SBP, mean nocturnal arterial oxygen saturation, past maximum SBP, and blood urea level.
The prognostication of hypertensive patients is a highly dynamic domain in AI research, leading to the emergence of diverse AI algorithms. Hybrid or multiple algorithms have been applied to improve the accuracy of prognostic models and analyze multimodal datasets, such as those based on EHRs containing textural descriptions and discrete physical indicators [37, 38]. In addition, to overcome biases arising from differences in race/ethnicity or primary/tertiary healthcare systems, existing large international prospective cohorts or randomized controlled trials have been reanalyzed and used for external validation [35, 36].
Management of hypertension
AI could play a role in novel digital interventions, such as promoting patient awareness, self-monitoring, healthy behaviors, and medication adherence. In other words, AI can be integrated into health coaching apps that automatically analyze patients’ BP or activity data from wearable BP devices and/or social media and then provide personalized feedback, including suggestions for BP medications and lifestyle modifications. Recently, randomized clinical trials (RCTs) of mobile apps for managing BP have been reported. One RCT found a small improvement in self-reported adherence with no change in SBP compared to the control group when using a smartphone app to improve medication adherence [41]. However, another RCT utilizing a mobile self-monitoring BP app in conjunction with a feedback algorithm showed a significant improvement in BP control [42].
AI could be useful for personalized hypertension management in terms of antihypertensive drug selection or BP control strategies, such as intensive BP control. Several RCTs have demonstrated the beneficial effects of intensive BP control, and recent ACC/AHA hypertension guidelines recommend intensive BP control [3, 43, 44]. However, intensive BP control may sometimes be difficult to apply to all patients. Therefore, it is important to define which patients can benefit from intensive BP control. AI can be used to define personalized benefit through phenotypic representation in clinical trials. Oikonomoun et al. developed a practical tool for individualized selection of intensive versus standard SBP control in patients without and with type 2 diabetes mellitus [45]. In addition, a study was recently conducted for personalized optimal antihypertensive drug selection. Data mining methods utilizing data from successful and unsuccessful cases were applied to reveal the spectrum of clinical characteristics or important clinical attributes (sensitizers) of five commonly used drugs (irbesartan, metoprolol, felodipine, amlodipine, and levo-amlodipine) [46].
By analyzing big data using ML, Koren et al. [47] showed that drug options that are not reflected in the latest guidelines, such as beta-blockers, proton pump inhibitors and statins, improve the success rate of hypertension treatment. This shows that AI can be used to consider new indications for already marketed drugs.
It is commonly assumed that the absolute risk reduction (ARR) of a treatment-induced cardiovascular event is proportional to baseline risk, with the greatest benefit in high-risk patients. Using individual participant data from the SPRINT and ACCORD-BP trials, Duan et al. showed that an X-learner correctly observed that individualized treatment effects were often not proportional to baseline risk. This study demonstrated that ML methods can be used to improve the identification and calibration of individualized treatment effect estimates from clinical trial data [48]. Li et al. [49] evaluated nonadherent patients’ characteristics from the New York City Community Health Survey using the ML segmentation approach as exhaustive chi-square automatic interaction detection. The study revealed that the most significant predictors of nonadherence for young adults aged 18 to 44 years were no diabetes and white, Asian or Hispanic race. Moreover, uninsured status, no diabetes mellitus, and moderate or high neighborhood poverty were predictors of nonadherence among adults aged 45 to 65 years. Older adults aged 65 years and older were more likely to be nonadherent if they had a low household income or lived in neighborhoods with moderate to high levels of poverty.
Population segmentation analysis can help interpret complex interactions or correlations between variables and offer targeted and effective population health interventions for each segment. This approach is more effective than regression analysis.
Limitations of applying AI in hypertension
There are several challenges to the implementation of AI for managing patients with hypertension. Several regulatory healthcare systems, such as the United States Food and Drug Administration (FDA) and Korean Ministry of Food and Drug Safety, have announced approval guidelines [50,51,52,53]. However, there is still a lack of expert consensus or guidelines. In addition, there are legal and ethical concerns about processing large volumes of data. AI research requires large-scale data for training, testing, and validating.
AI algorithms are trained on previous datasets, which can reflect selection bias based on factors such as sex, race, and socioeconomic status. These biases can be encoded into the algorithm, leading to discriminatory outcomes. Therefore, researchers should develop techniques to debias datasets and algorithms, such as using diverse training data and implementing fairness-aware algorithms. One issue associated with AI research is the lack of transparency and explainability. AI models are often opaque and difficult to understand, creating a ‘black box’ problem. This makes it challenging to explain how the algorithm arrives at its decisions, raising concerns about accountability and trust [32, 54, 55]. Researchers should investigate methods to increase the interpretability of AI models. Techniques such as importance maps or attention mechanisms can be used to emphasize the data components that have the most significant impact on the algorithm’s output. Because AI systems often require access to large amounts of personal data to function effectively. This raises concerns about data privacy, security and the potential for misuse. Thus, it is essential to ensure robust data privacy regulations and advocate responsibility in the data collection practice.
Also, an AI algorithm and the accuracy of the algorithm depend on the amount of data. Many AI studies have reanalyzed existing cohorts or published clinical trials to confirm superiority over statistical analysis and gain new insights. There are only a few reliable RCTs in hypertension AI research, such as those assessing mobile apps for hypertension management and new BP measuring devices (Tables 1 and 4). Recently, various AI algorithms have been developed by many institutions. The lack of standardization and interoperability, such as overfitting, is inevitable, although most AI studies validate their algorithms in separate datasets [56, 57]. AI can make decisions about the diagnosis, treatment, and prognosis of hypertension, thereby mimicking a clinician but is not considered able to replace the physician. AI is based on automated learning from data, so if the data are biased, the algorithm could generate the wrong data-driven decision [58]. Because AI draws conclusions in the most efficient way for its purpose without regard to medical ethics, clinicians with some insight into medical ethics or clinical settings must become involved in the development and implementation of algorithms [32].
Conclusions
Most AI studies on hypertension have remained exploratory technology assessments or have reanalyzed data from retrospective cohorts or RCTs focused on other topics. To date, only a few RCTs have tested AI algorithms in hypertension, such as algorithms for mobile apps or BP measuring devices. Nevertheless, with the innovative development of AI technology, AI has the potential to overcome the stagnation in hypertension and all aspects of hypertension clinical practice, including BP measurement, diagnosis, prognostication, and management. Collaboration with medical professionals, particularly in the field of hypertension research, is crucial during the development and validation process of the AI model to ensure clinical relevance.
Data availability
Not applicable.
Abbreviations
- AI:
-
artificial intelligence
- ARR:
-
absolute risk reduction
- BP:
-
blood pressure
- CVD:
-
cardiovascular disease
- DBP:
-
diastolic blood pressure
- DL:
-
deep learning
- EHR:
-
electronic health records
- HDL-C:
-
high-density lipoprotein-cholesterol
- ML:
-
machine learning
- PAT:
-
pulse arrival time
- PPG:
-
photoplethysmogram
- PTT:
-
pulse transit time
- RCT:
-
randomized controlled trial
- SBP:
-
systolic blood pressure
References
Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. 2021;18:785–802.
Kim HL, Lee EM, Ahn SY, Kim KI, Kim HC, Kim JH, Lee HY, Lee JH, Park JM, Cho EJ, Park S, Shin J, Kim YK. The 2022 focused update of the 2018 Korean Hypertension Society Guidelines for the management of hypertension. Clin Hypertens. 2023;29:11.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr., Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA, Sr., Williamson JD, Wright JT Jr, 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines. Hypertension. 2018;71:1269–324.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I. 2018 ESC/ESH guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36:1953–2041.
Semret M, Zidehsarai M, Agarwal R. Accuracy of oscillometric blood pressure monitoring with concurrent auscultatory blood pressure in hemodialysis patients. Blood Press Monit. 2005;10:249–55.
Landgraf J, Wishner SH, Kloner RA. Comparison of automated oscillometric versus auscultatory blood pressure measurement. Am J Cardiol. 2010;106:386–8.
Ihm S-H, Park J-H, Kim JY, Kim J-H, Kim K-I, Lee EM, Lee H-Y, Park S, Shin J, Kim C-H. Home blood pressure monitoring: a position statement from the Korean Society of Hypertension Home blood pressure forum. Clin Hypertens. 2022;28:38.
Argha A, Celler BG, Lovell NH. Artificial Intelligence based blood pressure estimation from Auscultatory and Oscillometric Waveforms: a methodological review. IEEE Rev Biomed Eng. 2022;15:152–68.
Argha A, Celler BG, Lovell NH. A Novel Automated blood pressure estimation algorithm using sequences of Korotkoff sounds. IEEE J Biomed Health Inf. 2021;25:1257–64.
Chu G, Zhang Z, Xu M, Huang D, Dai Q. Validation of a smartphone auscultatory blood pressure kit Accutension XYZ-110 in adults according to the ANSI/AAMI/ISO 81060-2: 2013 standard. Blood Press Monit. 2017;22:290–4.
Lee HY, Lee DJ, Seo J, Ihm SH, Kim KI, Cho EJ, Kim HC, Shin J, Park S, Sohn IS, Chung WJ, Ryu SK, Sung KC, Kim J, Kim DH, Pyun WB. Smartphone / smartwatch-based cuffless blood pressure measurement: a position paper from the Korean Society of Hypertension. Clin Hypertens. 2021;27:4.
Kwon Y, Wiles C, Parker BE, Clark BR, Sohn MW, Mariani S, Hahn JO, Jacobs DR, Stein JH, Lima J, Kapur V, Wellman A, Redline S, Azarbarzin A. Pulse arrival time, a novel sleep cardiovascular marker: the multi-ethnic study of atherosclerosis. Thorax. 2021;76:1124–30.
Elgendi M, Fletcher R, Liang Y, Howard N, Lovell NH, Abbott D, Lim K, Ward R. The use of photoplethysmography for assessing hypertension. NPJ Digit Med. 2019;2:60.
Kounalakis SN, Geladas ND. The role of pulse transit time as an index of arterial stiffness during exercise. Cardiovasc Eng. 2009;9:92–7.
Esmaelpoor J, Moradi MH, Kadkhodamohammadi A. A multistage deep neural network model for blood pressure estimation using photoplethysmogram signals. Comput Biol Med. 2020;120:103719.
Samimi H, Dajani HR. A PPG-Based calibration-free Cuffless blood pressure estimation method using Cardiovascular dynamics. Sens (Basel). 2023;23.
Matsumura K, Rolfe P, Toda S, Yamakoshi T. Cuffless blood pressure estimation using only a smartphone. Sci Rep. 2018;8:7298.
Sagirova Z, Kuznetsova N, Gogiberidze N, Gognieva D, Suvorov A, Chomakhidze P, Omboni S, Saner H, Kopylov P. Cuffless Blood pressure measurement using a smartphone-case based ECG Monitor with Photoplethysmography in Hypertensive patients. Sens (Basel). 2021;21.
Sayer G, Piper G, Vorovich E, Raikhelkar J, Kim GH, Rodgers D, Shimbo D, Uriel N. Continuous monitoring of blood pressure using a wrist-worn Cuffless device. Am J Hypertens. 2022;35:407–13.
Juri T, Suehiro K, Kanematsu R, Takahashi K, Fujimoto Y, Tanaka K, Mori T. Validation of continuous noninvasive blood pressure monitoring using Error Grid Analysis. Anesth Analg. 2022;134:773–80.
Poplin R, Varadarajan AV, Blumer K, Liu Y, McConnell MV, Corrado GS, Peng L, Webster DR. Prediction of cardiovascular risk factors from retinal fundus photographs via deep learning. Nat Biomed Eng. 2018;2:158–64.
López-Martínez F, Núñez-Valdez ER, Crespo RG, García-Díaz V. An artificial neural network approach for predicting hypertension using NHANES data. Sci Rep. 2020;10:10620.
Soh DCK, Ng EYK, Jahmunah V, Oh SL, San TR, Acharya UR. A computational intelligence tool for the detection of hypertension using empirical mode decomposition. Comput Biol Med. 2020;118:103630.
Völzke H, Fung G, Ittermann T, Yu S, Baumeister SE, Dörr M, Lieb W, Völker U, Linneberg A, Jørgensen T, Felix SB, Rettig R, Rao B, Kroemer HK. A new, accurate predictive model for incident hypertension. J Hypertens. 2013;31:2142–50. discussion 50.
Ye C, Fu T, Hao S, Zhang Y, Wang O, Jin B, Xia M, Liu M, Zhou X, Wu Q, Guo Y, Zhu C, Li YM, Culver DS, Alfreds ST, Stearns F, Sylvester KG, Widen E, McElhinney D, Ling X. Prediction of Incident Hypertension within the Next Year: prospective study using Statewide Electronic Health Records and Machine Learning. J Med Internet Res. 2018;20:e22.
Kanegae H, Suzuki K, Fukatani K, Ito T, Harada N, Kario K. Highly precise risk prediction model for new-onset hypertension using artificial intelligence techniques. J Clin Hypertens. 2020;22:445–50.
Tsoi KKF, Chan NB, Yiu KKL, Poon SKS, Lin B, Ho K. Machine learning clustering for blood pressure variability Applied to systolic blood pressure intervention trial (SPRINT) and the Hong Kong Community Cohort. Hypertension. 2020;76:569–76.
Koshimizu H, Kojima R, Kario K, Okuno Y. Prediction of blood pressure variability using deep neural networks. Int J Med Inf. 2020;136:104067.
Hung MH, Shih LC, Wang YC, Leu HB, Huang PH, Wu TC, Lin SJ, Pan WH, Chen JW, Huang CC. Prediction of masked hypertension and masked uncontrolled hypertension using machine learning. Front Cardiovasc Med. 2021;8:778306.
Wu X, Yuan X, Wang W, Liu K, Qin Y, Sun X, Ma W, Zou Y, Zhang H, Zhou X, Wu H, Jiang X, Cai J, Chang W, Zhou S, Song L. Value of a machine Learning Approach for Predicting Clinical outcomes in Young patients with hypertension. Hypertension. 2020;75:1271–8.
Angelaki E, Barmparis GD, Kochiadakis G, Maragkoudakis S, Savva E, Kampanieris E, Kassotakis S, Kalomoirakis P, Vardas P, Tsironis GP, Marketou ME. Artificial intelligence-based opportunistic screening for the detection of arterial hypertension through ECG signals. J Hypertens. 2022;40:2494–501.
Padmanabhan S, Tran TQB, Dominiczak AF. Artificial Intelligence in Hypertension seeing through a Glass darkly. Circ Res. 2021;128:1100–18.
Chaikijurajai T, Laffin LJ, Tang WHW. Artificial Intelligence and Hypertension: recent advances and future Outlook. Am J Hypertens. 2020;33:967–74.
Louca P, Tran TQB, Toit CD, Christofidou P, Spector TD, Mangino M, Suhre K, Padmanabhan S, Menni C. Machine learning integration of multimodal data identifies key features of blood pressure regulation. EBioMedicine. 2022;84:104243.
Weng SF, Reps J, Kai J, Garibaldi JM, Qureshi N. Can machine-learning improve cardiovascular risk prediction using routine clinical data? PLoS ONE. 2017;12:e0174944.
Kakadiaris IA, Vrigkas M, Yen AA, Kuznetsova T, Budoff M, Naghavi M. Machine learning outperforms ACC / AHA CVD risk calculator in MESA. J Am Heart Assoc. 2018;7:e009476.
Ren Y, Fei H, Liang X, Ji D, Cheng M. A hybrid neural network model for predicting kidney disease in hypertension patients based on electronic health records. BMC Med Inf Decis Mak. 2019;19:51.
Alaa AM, Bolton T, Di Angelantonio E, Rudd JHF, van der Schaar M. Cardiovascular disease risk prediction using automated machine learning: a prospective study of 423,604 UK Biobank participants. PLoS ONE. 2019;14:e0213653.
Lee SJ, Lee SH, Choi HI, Lee JY, Jeong YW, Kang DR, Sung KC. Deep learning improves prediction of Cardiovascular Disease-related mortality and admission in patients with hypertension: analysis of the Korean National Health Information Database. J Clin Med. 2022;11.
Lacson RC, Baker B, Suresh H, Andriole K, Szolovits P, Lacson E. Jr. Use of machine-learning algorithms to determine features of systolic blood pressure variability that predict poor outcomes in hypertensive patients. Clin Kidney J. 2019;12:206–12.
Morawski K, Ghazinouri R, Krumme A, Lauffenburger JC, Lu Z, Durfee E, Oley L, Lee J, Mohta N, Haff N, Juusola JL, Choudhry NK. Association of a Smartphone Application with Medication adherence and blood pressure control: the MedISAFE-BP Randomized Clinical Trial. JAMA Intern Med. 2018;178:802–9.
Choi DJ, Park JJ, Yoon M, Park SJ, Jo SH, Kim EJ, Kim SJ, Lee S. Self-monitoring of blood pressure and feed-back using APP in TReatment of UnconTrolled Hypertension (SMART-BP): a Randomized Clinical Trial. Korean Circ J. 2022;52:785–94.
Wright JT Jr., Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, Reboussin DM, Rahman M, Oparil S, Lewis CE, Kimmel PL, Johnson KC, Goff DC Jr., Fine LJ, Cutler JA, Cushman WC, Cheung AK, Ambrosius WT. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16.
Zhang W, Zhang S, Deng Y, Wu S, Ren J, Sun G, Yang J, Jiang Y, Xu X, Wang TD, Chen Y, Li Y, Yao L, Li D, Wang L, Shen X, Yin X, Liu W, Zhou X, Zhu B, Guo Z, Liu H, Chen X, Feng Y, Tian G, Gao X, Kario K, Cai J. Trial of intensive blood-pressure control in older patients with hypertension. N Engl J Med. 2021;385:1268–79.
Oikonomou EK, Spatz ES, Suchard MA, Khera R. Individualising intensive systolic blood pressure reduction in hypertension using computational trial phenomaps and machine learning: a post-hoc analysis of randomised clinical trials. Lancet Digit Health. 2022;4:e796–e805.
Chunyu L, Ran L, Junteng Z, Miye W, Jing X, Lan S, Yixuan Z, Rui Z, Yizhou F, Chen W, Hongmei Y, Qing Z. Characterizing the critical features when personalizing antihypertensive drugs using spectrum analysis and machine learning methods. Artif Intell Med. 2020;104:101841.
Koren G, Nordon G, Radinsky K, Shalev V. Machine learning of big data in gaining insight into successful treatment of hypertension. Pharmacol Res Perspect. 2018;6:e00396.
Duan T, Rajpurkar P, Laird D, Ng AY, Basu S. Clinical value of Predicting Individual Treatment effects for intensive blood pressure therapy. Circ Cardiovasc Qual Outcomes. 2019;12:e005010.
Li Y, Jasani F, Su D, Zhang D, Shi L, Yi SS, Pagán JA. Decoding nonadherence to Hypertensive Medication in New York City: a Population Segmentation Approach. J Prim Care Community Health. 2019;10:2150132719829311.
US Food and Drug Administration. Technical performance assessment of quantitative imaging in radiological device premarket submissions. Available at: https://www.fda.gov/media/123271/download. 2023 Accessed May 30 2023.
US Food and Drug Administration Guidance for the content. of premarket submissions for software contained in medical devices. Available at: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-content-premarket-submissions-software-contained-medical-devices. 2023 Accessed May 30 2023.
US Food and Drug Administration Artificial intelligence/machine. learning (AI/ML)-based software as a medical device (SaMD) action plan. Available at: https://www.fda.gov/media/145022/download. 2023 Accessed May 30 2023.
Korean Food and Drug Safety. Guidance on the Review and Approval of Artificial Intelligence(AI)-based Medical Devices. https://www.mfds.go.kr/eng/brd/m_40/view.do?seq=72627. Accessed January 8 2023.
Handelman GS, Kok HK, Chandra RV, Razavi AH, Huang S, Brooks M, Lee MJ, Asadi H. Peering into the Black Box of Artificial Intelligence: evaluation Metrics of Machine Learning methods. AJR Am J Roentgenol. 2019;212:38–43.
Emanuel EJ, Wachter RM. Artificial Intelligence in Health Care: will the Value Match the hype? JAMA. 2019;321:2281–2.
Nagendran M, Chen Y, Lovejoy CA, Gordon AC, Komorowski M, Harvey H, Topol EJ, Ioannidis JPA, Collins GS, Maruthappu M. Artificial intelligence versus clinicians: systematic review of design, reporting standards, and claims of deep learning studies. BMJ. 2020;368:m689.
Yusuf M, Atal I, Li J, Smith P, Ravaud P, Fergie M, Callaghan M, Selfe J. Reporting quality of studies using machine learning models for medical diagnosis: a systematic review. BMJ Open. 2020;10:e034568.
Kelly CJ, Karthikesalingam A, Suleyman M, Corrado G, King D. Key challenges for delivering clinical impact with artificial intelligence. BMC Med. 2019;17:195.
Mohammadi R, Jain S, Agboola S, Palacholla R, Kamarthi S, Wallace BC. Learning to Identify Patients at Risk of Uncontrolled Hypertension Using Electronic Health Records Data. AMIA Jt Summits Transl Sci Proc. 2019;2019:533– 42.
Wu L, Huang L, Li M, Xiong Z, Liu D, Liu Y, Liang S, Liang H, Liu Z, Qian X, Ren J, Chen Y. Differential diagnosis of secondary hypertension based on deep learning. Artif Intell Med. 2023;141.
Hae H, Kang SJ, Kim TO, Lee PH, Lee SW, Kim YH, Lee CW, Park SW. Machine learning-based prediction of post-treatment ambulatory blood pressure in patients with hypertension. Blood Press. 2023;32:2209674.
Acknowledgements
Not applicable.
Funding
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 5-20225A0154-00126).
Author information
Authors and Affiliations
Contributions
J-HP and JSC collected and analyzed the data. JSC wrote the original manuscript. J-HP reviewed and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflicts of interests
Jae-Hyeong Park serves on the editorial boards as a deputy editor in the Clinical Hypertension. Jung Sun Cho has no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cho, J.S., Park, JH. Application of artificial intelligence in hypertension. Clin Hypertens 30, 11 (2024). https://doi.org/10.1186/s40885-024-00266-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40885-024-00266-9