Abstract
Background
The value of Epstein–Barr virus (EBV) DNA assay during posttreatment follow-up of the patients with nasopharyngeal carcinoma (NPC) presenting with different pretreatment plasma EBV DNA levels remains unclear. In the present study, we aimed to evaluate the prognostic value of plasma EBV DNA assay during posttreatment follow-up in the patients with NPC who have undergone intensity-modulated radiotherapy.
Methods
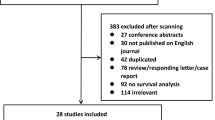
The medical records of 385 NPC patients treated with intensity-modulated radiotherapy between November 2009 and February 2012 were reviewed. All patients underwent plasma EBV DNA assays before treatment, within 3 months after treatment, and then every 3–12 months during posttreatment follow-up period. The recurrence rates for patients with different pretreatment and posttreatment follow-up plasma EBV DNA levels were analyzed.
Results
Of the 385 patients, 267 (69.4%) had detectable pretreatment plasma EBV DNA (> 0 copy/mL) and 93 (24.2%) had detectable posttreatment EBV DNA during a median follow-up of 52.8 months (range 9.3–73.8 months). Detectable EBV DNA during posttreatment follow-up was found in 14.4% (17/118) and 28.5% (76/267) of patients with undetectable and detectable pretreatment EBV DNA, respectively, and was significantly associated with tumor recurrence in both patient groups. EBV DNA was detectable in 12.8% (40/313) of patients who remained disease-free, 56.4% (22/39) of patients with locoregional recurrence alone, and 93.9% (31/33) of patients with distant metastasis as the first recurrence event (P < 0.001); 6.5% (19/292) of patients with undetectable EBV DNA and 57.0% (53/93) of patient with detectable EBV DNA during posttreatment follow-up experienced tumor recurrence. Compared with other cut-off values, the cut-off value of 0 copy/mL for EBV DNA during posttreatment follow-up had the highest area under the ROC curve (AUC) value (0.804, 95% confidence interval 0.741–0.868) for predicting tumor recurrence (sensitivity, specificity, and accuracy: 73.6%, 87.2%, and 84.7%, respectively).
Conclusion
Plasma EBV DNA level during posttreatment follow-up is a good marker for predicting distant metastasis but not locoregional recurrence in the patients with NPC irrespective of the pretreatment EBV DNA levels.
Similar content being viewed by others
Background
Nasopharyngeal carcinoma (NPC) is a common head and neck cancer in China, with 60,600 new cases reported in 2015 [1]. The incidence varies in different areas of China; the highest risk areas are South China, especially Guangdong Province; low rates of NPC are generally observed in North China [2]. Epstein–Barr virus (EBV) infection is an important etiological factor in NPC. Recent studies indicated that circulating EBV DNA originates from tumor lesions and associates with tumor load, and the plasma EBV DNA assay is widely used for screening, prognostic prediction, and post-treatment surveillance of patients with NPC [3, 4]. Pretreatment plasma EBV DNA was detectable (> 0 copy/mL) in 69%–97% of patients with NPC and was closely related to clinical stage and treatment outcome [5,6,7,8,9,10,11,12,13,14,15,16,17]. On the other hand, plasma EBV DNA detected within 3 months after treatment was found in 4.3%–30% of patients with NPC and was associated with short survival [6, 12,13,14,15,16,17,18,19,20,21,22].
The plasma EBV DNA assay has also be used to monitor tumor recurrence during posttreatment follow-up of NPC patients. It has been reported that patients with NPC who remained in remission after radiotherapy had consistently undetectable or extremely low levels of plasma EBV DNA, whereas patients who developed recurrence exhibited significantly elevated plasma EBV DNA levels [4, 9, 14, 23,24,25,26,27,28,29,30]. If plasma EBV DNA levels remain elevated after treatment or initially dropped but subsequently increased, the patients are suggested to take a positron emission tomography/computed tomography (CT) (PET/CT) scan to locate the potential site of recurrence [27]. Moreover, it has been reported that in patients with undetectable EBV DNA levels during posttreatment follow-up period but with radiographic evidence of disease recurrence, recurrence was not detected using histologic examination [27, 28]. Therefore, some investigators indicated that applying an EBV DNA screening followed by a PET/CT scan may be a cost-effective follow-up examination for patients with NPC [27].
However, in the clinic, some patients with consistently undetectable plasma EBV DNA during posttreatment follow-up period also develop tumor recurrence, whereas some patients with elevated EBV DNA levels remain disease-free even after long-term follow-up [29]. Thus, the recurrence rates for patients with undetectable or detectable plasma EBV DNA during posttreatment follow-up period remain unclear. Moreover, the value of plasma EBV DNA follow-up in patients with undetectable or detectable pretreatment EBV DNA has not yet been assessed. Therefore, we performed this retrospective study to further investigate the value of plasma EBV DNA for predicting tumor recurrence in patients with NPC.
Patients and methods
Patients
Medical records of 1811 patients with newly-diagnosed, non-distant metastatic, histologically proven NPC treated with radical intensity-modulated radiotherapy (IMRT) at Sun Yat-sen University Cancer Center (Guangzhou, China) between November 2009 and February 2012 were retrospectively analyzed. All patients underwent physical examination, endoscopy, and conventional imaging scans before treatment, and were restaged according to the 7th edition of the Union for International Cancer Control and American Joint Committee on Cancer (UICC/AJCC) staging system [31]. During the study, institutional guidelines recommended only IMRT for stage I NPC and concurrent chemoradiotherapy with or without neoadjuvant and/or adjuvant chemotherapy for stage II to IVB diseases [17]. Only patients who underwent plasma EBV DNA assays before treatment, within 3 months after treatment, and then every 3–12 months during posttreatment follow-up period were included in this study, and all records of the plasma EBV DNA levels were collected. The authenticity of this article has been validated by uploading the key raw data onto the research data deposit (RDD) public platform (http://www.researchdata.org.cn), with the approval RDD number as RDDA2017000230.
Quantification of plasma EBV DNA
Samples of peripheral blood (5 mL each) were collected and centrifuged at 1600×g for isolation of plasma. DNA from plasma samples was extracted with the QIAamp Blood Kit (Qiagen, Hilden, Germany). In total, 500–1000 µL of each plasma sample were used for DNA extraction per column, with a final elution volume of 50 µL from the extraction column [8]. Plasma EBV DNA levels were measured using a real-time quantitative polymerase chain reaction (qPCR) assay amplifying the BamH I-W region of the EBV genome, as previously described [5, 8]. The sequences of the forward and reverse primers were 5′-GCCAG AGGTA AGTGG ACTTT-3′ and 5′-TACCA CCTCC TCTTC TTGCT-3′, respectively. A dual fluorescence-labelled oligomer 5′-(fluorescein amidite, FAM) CACAC CCAGG CACAC ACTAC ACAT (tetramethylrhodamine, TAMRA)-3′ served as a probe. The plasma EBV DNA level was calculated using the following formula: C = Q × (V DNA/V PCR) × (1/V EXT), in which C represents the target level in plasma (copies/mL), Q represents the target quantity (copy number) determined by PCR, V DNA represents the total volume of DNA obtained after extraction (typically 50 µL per Qiagen extraction), V PCR represents the volume of DNA solution used for PCR (typically 2 µL), and V EXT represents the volume of plasma extracted (typically 0.5 mL). A plasma EBV DNA level of higher than 0 copy/mL was considered detectable, whereas a level of 0 copy/mL was considered undetectable.
Follow-up and assessments
Patients were recommended to undergo examinations at least every 3 months during the first 2 years after IMRT and every 6 months thereafter (or until death). The routine follow-up workup included physical examination, plasma EBV DNA assay, nasopharyngeal fiberoptic endoscopy, nasopharyngeal and neck magnetic resonance imaging (MRI), chest X-ray or CT, liver ultrasound or CT, and whole-body bone scan. If possible, tumor recurrence (locoregional recurrence or distant metastasis) was confirmed by fine needle aspiration or biopsy. For recurrences at sites not accessible, clinical diagnosis was accepted if classical changes were observed using at least two imaging methods with or without clinical symptoms, including 18F-fluorodeoxyglucose (18F-FDG) PET/CT, MRI, CT, abdominal sonography and/or a whole-body bone scan. To increase diagnostic accuracy in the present study, the diagnoses of tumor recurrence were retrospectively confirmed by two experienced doctors on the basis of abnormal imaging findings and the response to treatment.
Statistical analysis
Overall survival (OS) was calculated from the end of radiotherapy to death from any cause or censored at last follow-up. Disease-free survival (DFS) was calculated from the end of radiotherapy to the date of locoregional recurrence or distant metastasis, whichever occurred first. Distant metastasis-free survival (DMFS) and locoregional recurrence-free survival (LRRFS) were calculated from the end of radiotherapy to the date of distant metastasis or first locoregional recurrence, respectively. EBV failure-free survival was calculated from the end of radiotherapy to the date of first emergence of plasma EBV DNA during follow-up, which was defined as the first emergence of EBV DNA after radiotherapy to the date of first tumor recurrence or the last follow-up in patients with undetectable or persistently detectable EBV DNA after radiotherapy, or the re-emergence of EBV DNA in patients with transiently detectable EBV DNA after radiotherapy followed by a rapid regression to undetectable levels. Living patients without an event corresponding to any endpoint were censored at the date of last follow-up.
All statistical analyses were performed using SPSS v13.0 (SPSS Inc., Chicago, IL, USA). The Chi square test was used to compare categorical variables (or Fisher’s exact test, if the expected number was < 5 in at least 1 cell) and test the association between EBV DNA levels and recurrence. Receiver operating characteristic (ROC) curves were generated, and the area under the ROC curve (AUC) and 95% confidence interval (CI) was calculated to determine the optimal cut-off value of plasma EBV DNA for predicting tumor recurrence with the best trade-off between sensitivity and specificity. Survival rates were calculated using the Kaplan–Meier method, and the differences were compared using the log-rank test. Two-tailed P values < 0.05 were considered statistically significant.
Results
Treatment outcomes
A total of 385 patients were included in this study, and the clinical characteristics of these patients are shown in Table 1. The median follow-up time was 52.8 months (range 9.3–73.8 months). Seventy-two (18.7%) patients experienced tumor recurrence. The first recurrence was locoregional recurrence alone in 39 (10.1%) patients and distant metastasis with or without locoregional recurrence in 33 (8.6%) patients. The 5-year DFS, OS, LRRFS, and DMFS rates were 80.6%, 89.7%, 86.8%, and 89.3%, respectively. Plasma EBV DNA was detected in 267 (69.4%) patients before treatment and 93 (24.2%) patients during posttreatment follow-up. The 5-year EBV failure-free survival rate was 74.4%. The Kaplan–Meier survival curves for DFS and EBV failure-free survival are shown in Fig. 1.
Association between plasma EBV DNA status and tumor recurrence
Detectable EBV DNA during posttreatment follow-up was found in 14.4% (17/118) of patients with undetectable pretreatment EBV DNA and 28.5% (76/267) of patients with detectable pretreatment EBV DNA (P = 0.003). The plasma EBV DNA status during posttreatment follow-up was significantly associated with tumor recurrence in both patient groups stratified by the pretreatment EBV DNA status (detectable or undetectable) (Table 2). In all, EBV DNA was detectable during posttreatment follow-up in 12.8% (40/313) of patients who remained disease-free and 73.6% (53/72) of patients who experienced tumor recurrence (P < 0.001). The posttreatment follow-up plasma EBV DNA status was also associated with the site of first recurrence. Posttreatment follow-up plasma EBV DNA could be detected in 93.9% (31/33) of patients who developed distant metastasis with or without locoregional recurrence, but only in 56.4% (22/39) of patients with locoregional recurrence alone (P < 0.001).
Failure patterns in patients with undetectable EBV DNA during posttreatment follow-up
Of the 292 patients with undetectable EBV DNA during posttreatment follow-up, 19 (6.5%) experienced tumor recurrence; the first recurrence included locoregional recurrence alone in 17 patients and distant metastasis in 2 patients (Table 2). All 17 cases of locoregional recurrence were histologically confirmed, with the exception of one case that was diagnosed by MRI and PET/CT. Two patients developed lung metastasis: one was confirmed by surgical pathology, and the other was diagnosed by chest CT and PET/CT.
Failure patterns in patients with detectable EBV DNA during posttreatment follow-up
Of the 93 patients with detectable EBV DNA during posttreatment follow-up, 53 (57.0%) experienced tumor recurrence; the first recurrence were locoregional recurrence alone in 22 patients and distant metastasis with or without locoregional recurrence in 31 patients (Table 2). Of the 53 patients with tumor recurrence and detectable EBV DNA during posttreatment follow-up, 25 (47.2%) were histologically confirmed, whereas 28 (52.8%) were diagnosed by combined radiologic imaging methods. The other 40 patients with detectable posttreatment follow-up EBV DNA remained disease-free after a median follow-up of 29.2 months (range 0.7–65.9 months); none of these patients received preventative chemotherapy or other therapeutic interventions during posttreatment follow-up period.
Of the 53 patients with tumor recurrence and detectable posttreatment follow-up EBV DNA, 29 (54.7%) had elevated posttreatment follow-up EBV DNA levels prior to clinical recurrence, with a median interval between the observation of elevated EBV DNA level and first recurrence of 9.1 months (range 2.2–35.7 months). The median plasma EBV DNA level was 3940 copies/mL (range 40–2,420,000 copies/mL) at the time of first detection after radiotherapy, and 16,500 copies/mL (range 180–8,010,000 copies/mL) at the time of recurrence. For the 40 patient who were disease-free, the median EBV DNA level was 805 copies/mL (range 30–8840 copies/mL). Transiently detectable EBV DNA followed by a rapid regression to undetectable levels was observed in 9.4% (5/53) of patients with tumor recurrence and 97.5% (39/40) of those who were disease-free (P < 0.001, Table 3).
Optimal plasma EBV DNA cut-off level for predicting tumor recurrence
The plasma EBV DNA level at the time of first detection during posttreatment follow-up was analyzed as a dichotomous variable using different cut-off values (0, 500, and 1000 copies/mL). The AUC, sensitivity, specificity, accuracy, positive predictive value, and negative predictive value for each cut-off value of EBV DNA level for prediction of tumor recurrence are shown in Table 4. Compared with other cut-off values, an EBV DNA value of > 0 copy/mL had the highest AUC value (AUC, 0.804; 95% CI 0.741–0.868), with corresponding sensitivity, specificity, and accuracy of 73.6%, 87.2%, and 84.7%, respectively.
Discussion
The results of the present study showed that detectable plasma EBV DNA during posttreatment follow-up could be found in NPC patients with undetectable pretreatment EBV DNA, and was significantly associated with tumor recurrence, especially distant metastasis, in patients with either detectable or undetectable pretreatment EBV DNA. Compared with other cut-off values, EBV DNA > 0 copy/mL during posttreatment follow-up had the strongest association with tumor recurrence.
Elevated levels of EBV DNA during posttreatment follow-up have been shown to associate with tumor recurrence, and play an important role in detecting and monitoring recurrence in NPC [4, 9, 14, 23,24,25,26,27,28,29,30]. However, the role of posttreatment follow-up EBV DNA assay on NPC patients with undetectable pretreatment EBV DNA has not been reported yet. In the present study, detectable EBV DNA during posttreatment follow-up was found in 14.4% of patients with undetectable pretreatment EBV DNA and was significantly associated with tumor recurrence in these patients. Our results suggested that the posttreatment follow-up plasma EBV DNA assay is also valuable in patients with undetectable pretreatment EBV DNA.
Our results showed that plasma EBV DNA could be detected in 12.8% of patients who remained disease-free during posttreatment follow-up and in 73.6% of patients who experienced tumor recurrence. The EBV DNA levels during follow-up were usually low (≤ 1000 copies/mL) and transiently detected in patients who remained disease-free, but high (> 1000 copies/mL) and detected on consecutive occasions in patients who had tumor recurrence. In the study by Hsu et al. [29], approximately 30% of patients with disease free had transiently elevated EBV DNA levels of < 400 copies/mL or no < 400 copies/mL of EBV DNA load with fluctuation. The reasons explaining transiently detectable EBV DNA remain unknown, and none of the patients with detectable EBV DNA during posttreatment follow-up in the present study had preventative chemotherapy or other therapeutic interventions before clinical diagnosis of tumor recurrence; other EBV-related diseases [29] and false-positive EBV DNA levels [32] could be the possible factors.
We found that, in patients with undetectable plasma EBV DNA during posttreatment follow-up, 6.5% of patients experienced tumor recurrence, with locoregional recurrence as the major failure pattern. Moreover, plasma EBV DNA could be detected in 93.9% of patients who had distant metastasis with or without locoregional failure, but only in 56.4% of patients who suffered locoregional recurrence as the first recurrence event (P < 0.001). These results indicate that plasma EBV DNA assay has a significantly lower sensitivity for detection of locoregional recurrence than for that of distant metastasis. Similar findings have been reported in previous studies: plasma EBV DNA was detected in 86%–96% of patients who experienced distant metastasis and 51%–67% of patients who suffered locoregional recurrence [4, 9, 14, 23,24,25,26, 29, 30].
One possible explanation for this phenomenon is that plasma EBV DNA levels reflects the tumor load in NPC [5, 7], and patients with locoregional recurrence usually have a lower tumor burden than patients with distant metastasis. A second explanation is that locoregionally recurrent tumor cells often regrow from irradiated tumor sites, and post-irradiation changes such as stromal fibrosis and decreased vascularity may interfere with the efflux of EBV DNA into the plasma [24]. Distant metastatic tumor cells are derived from micro-metastasis from the pre-irradiated primary tumor; thus, the release of EBV DNA from these sites is not affected by post-irradiation changes [24]. Thus, plasma EBV DNA assay is not superior to imaging modalities such as MRI scans for detecting locoregional recurrence, but may be advantageous for the early detection of metastatic disease in comparison with imaging modalities that cannot detect micro-metastasis.
The optimal threshold of posttreatment follow-up EBV DNA level for detecting tumor recurrence in NPC patients remains unclear. Hsu et al. [29] found that with the cut-off value of 400 copies/mL of EBV DNA, the sensitivity was 46%, and the specificity was 94%. Cao et al. [25] recommended 0 copy/mL as the optimal cut-off value for detecting recurrence of NPC. In the present study, we found that higher EBV DNA cut-off values had higher specificity but lower sensitivity for detecting recurrence, and the EBV DNA value of more than 0 copy/mL yielded the highest AUC in predicting tumor recurrence, with sensitivity, specificity, and accuracy of 73.6%, 87.2%, and 84.7%, respectively. The sensitivity of EBV DNA assay for predicting NPC recurrence in the present study was lower than the 74.7%–81.5% reported in other studies which also used 0 copy/mL as the cut-off value [26, 29, 30]. The possible explanation is that plasma EBV DNA assay has a high sensitivity for the prediction of distant metastasis, but not locoregional recurrence. Thus, the sensitivity for predicting tumor recurrence depends on the ratio of distant metastasis to all recurrences. In the present study, distant metastasis accounted for a relatively small portion of total recurrences (45.8%, 33/72), which lowered the sensitivity of EBV DNA in predicting tumor recurrence.
The present study has several limitations. First, the records of plasma EBV DNA levels during posttreatment follow-up were retrospectively collected, and the intervals of 3–12 months were relatively long and irregular, which could confound the results. Second, not all of the patients with tumor recurrence underwent histologic examinations or PET/CT scans. Third, selection bias may have been introduced as only patients who underwent plasma EBV DNA assays every 3–12 months during posttreatment follow-up period were recruited to this study. However, consecutive enrollment was mandated to minimize bias.
Conclusions
Plasma EBV DNA level during posttreatment follow-up is a good marker for predicting distant metastasis, but not locoregional recurrence, in patients with NPC irrespective of the pretreatment EBV DNA status. Thus, we suggest that plasma EBV DNA assay plus nasopharyngeal and neck MRI could be an effective follow-up strategy for patients with NPC, and whole body examinations (e.g., PET/CT) should be recommended for patients with detectable EBV DNA during posttreatment follow-up. Close follow-up is needed for patients with elevated levels of EBV DNA during posttreatment follow-up but negative findings on imaging studies. The conclusions of this study require further validation in large-scale prospective studies.
Abbreviations
- NPC:
-
nasopharyngeal carcinoma
- EBV:
-
Epstein–Barr virus
- PET:
-
positron emission tomography
- IMRT:
-
intensity-modulated radiotherapy
- UICC:
-
Union for International Cancer Control
- AJCC:
-
American Joint Committee on Cancer
- MRI:
-
magnetic resonance imaging
- PFS:
-
progression-free survival
- OS:
-
overall survival
- DMFS:
-
distant metastasis-free survival
- LRRFS:
-
locoregional recurrence-free survival
- AUC:
-
area under curve
References
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–32. https://doi.org/10.3322/caac.21338.
Zhang LF, Li YH, Xie SH, Ling W, Chen SH, Liu Q, et al. Incidence trend of nasopharyngeal carcinoma from 1987 to 2011 in Sihui County, Guangdong Province, South China: an age-period-cohort analysis. Chin J Cancer. 2015;34(8):350–7. https://doi.org/10.1186/s40880-015-0018-6.
Chan KC. Plasma Epstein–Barr virus DNA as a biomarker for nasopharyngeal carcinoma. Chin J Cancer. 2014;33(12):598–603. https://doi.org/10.5732/cjc.014.10192.
Yip TT, Ngan RK, Fong AH, Law SC. Application of circulating plasma/serum EBV DNA in the clinical management of nasopharyngeal carcinoma. Oral Oncol. 2014;50(6):527–38. https://doi.org/10.1016/j.oraloncology.2013.12.011.
Lo YM, Chan LY, Lo KW, Leung SF, Zhang J, Chan AT, et al. Quantitative analysis of cell-free Epstein–Barr virus DNA in plasma of patients with nasopharyngeal carcinoma. Cancer Res. 1999;59(6):1188–91.
Chan AT, Lo YM, Zee B, Chan LY, Ma BB, Leung SF, et al. Plasma Epstein–Barr virus DNA and residual disease after radiotherapy for undifferentiated nasopharyngeal carcinoma. J Natl Cancer Inst. 2002;94(21):1614–9.
Lin JC, Wang WY, Chen KY, Wei YH, Liang WM, Jan JS, et al. Quantification of plasma Epstein–Barr virus DNA in patients with advanced nasopharyngeal carcinoma. N Engl J Med. 2004;350(24):2461–70. https://doi.org/10.1056/NEJMoa032260.
Shao JY, Li YH, Gao HY, Wu QL, Cui NJ, Zhang L, et al. Comparison of plasma Epstein–Barr virus (EBV) DNA levels and serum EBV immunoglobulin A/virus capsid antigen antibody titers in patients with nasopharyngeal carcinoma. Cancer. 2004;100(6):1162–70. https://doi.org/10.1002/cncr.20099.
Fan H, Nicholls J, Chua D, Chan KH, Sham J, Lee S, et al. Laboratory markers of tumor burden in nasopharyngeal carcinoma: a comparison of viral load and serologic tests for Epstein–Barr virus. Int J Cancer. 2004;112(6):1036–41. https://doi.org/10.1002/ijc.20520.
Leung SF, Zee B, Ma BB, Hui EP, Mo F, Lai M, et al. Plasma Epstein–Barr viral deoxyribonucleic acid quantitation complements tumor-node-metastasis staging prognostication in nasopharyngeal carcinoma. J Clin Oncol. 2006;24(34):5414–8. https://doi.org/10.1200/JCO.2006.07.7982.
Bortolin MT, Pratesi C, Dolcetti R, Bidoli E, Vaccher E, Zanussi S, et al. Clinical value of Epstein–Barr virus DNA levels in peripheral blood samples of Italian patients with undifferentiated carcinoma of nasopharyngeal type. Cancer Lett. 2006;233(2):247–54. https://doi.org/10.1016/j.canlet.2005.03.015.
Lin JC, Wang WY, Liang WM, Chou HY, Jan JS, Jiang RS, et al. Long-term prognostic effects of plasma Epstein–Barr virus DNA by minor groove binder-probe real-time quantitative PCR on nasopharyngeal carcinoma patients receiving concurrent chemoradiotherapy. Int J Radiat Oncol Biol Phys. 2007;68(5):1342–8. https://doi.org/10.1016/j.ijrobp.2007.02.012.
Twu CW, Wang WY, Liang WM, Jan JS, Jiang RS, Chao J, et al. Comparison of the prognostic impact of serum anti-EBV antibody and plasma EBV DNA assays in nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2007;67(1):130–7. https://doi.org/10.1016/j.ijrobp.2006.07.012.
Ferrari D, Codeca C, Bertuzzi C, Broggio F, Crepaldi F, Luciani A, et al. Role of plasma EBV DNA levels in predicting recurrence of nasopharyngeal carcinoma in a Western population. BMC Cancer. 2012;12:208. https://doi.org/10.1186/1471-2407-12-208.
Leung SF, Chan KC, Ma BB, Hui EP, Mo F, Chow KC, et al. Plasma Epstein–Barr viral DNA load at midpoint of radiotherapy course predicts outcome in advanced-stage nasopharyngeal carcinoma. Ann Oncol. 2014;25(6):1204–8. https://doi.org/10.1093/annonc/mdu117.
Liu LT, Tang LQ, Chen QY, Zhang L, Guo SS, Guo L, et al. The prognostic value of plasma Epstein–Barr viral DNA and tumor response to neoadjuvant chemotherapy in advanced-stage nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2015;93(4):862–9. https://doi.org/10.1016/j.ijrobp.2015.08.003.
Peng H, Guo R, Chen L, Zhang Y, Li WF, Mao YP, et al. Prognostic impact of plasma Epstein–Barr virus DNA in patients with nasopharyngeal carcinoma treated using intensity-modulated radiation therapy. Sci Rep. 2016;6:22000. https://doi.org/10.1038/srep22000.
Hou X, Zhao C, Guo Y, Han F, Lu LX, Wu SX, et al. Different clinical significance of pre- and post-treatment plasma Epstein–Barr virus DNA load in nasopharyngeal carcinoma treated with radiotherapy. Clin Oncol (R Coll Radiol). 2011;23(2):128–33. https://doi.org/10.1016/j.clon.2010.09.001.
Wang WY, Twu CW, Chen HH, Jiang RS, Wu CT, Liang KL, et al. Long-term survival analysis of nasopharyngeal carcinoma by plasma Epstein–Barr virus DNA levels. Cancer. 2013;119(5):963–70. https://doi.org/10.1002/cncr.27853.
Twu CW, Wang WY, Chen CC, Liang KL, Jiang RS, Wu CT, et al. Metronomic adjuvant chemotherapy improves treatment outcome in nasopharyngeal carcinoma patients with postradiation persistently detectable plasma Epstein–Barr virus deoxyribonucleic acid. Int J Radiat Oncol Biol Phys. 2014;89(1):21–9. https://doi.org/10.1016/j.ijrobp.2014.01.052.
Hui EP, Ma BB, Chan KC, Chan CM, Wong CS, To KF, et al. Clinical utility of plasma Epstein–Barr virus DNA and ERCC1 single nucleotide polymorphism in nasopharyngeal carcinoma. Cancer. 2015;121(16):2720–9. https://doi.org/10.1002/cncr.29413.
Wang WY, Lin TY, Twu CW, Tsou HH, Lin PJ, Liu YC, et al. Long-term clinical outcome in nasopharyngeal carcinoma patients with post-radiation persistently detectable plasma EBV DNA. Oncotarget. 2016;7(27):42608–16. https://doi.org/10.18632/oncotarget.9323.
Lo YM, Chan LY, Chan AT, Leung SF, Lo KW, Zhang J, et al. Quantitative and temporal correlation between circulating cell-free Epstein–Barr virus DNA and tumor recurrence in nasopharyngeal carcinoma. Cancer Res. 1999;59(21):5452–5.
Leung SF, Lo YM, Chan AT, To KF, To E, Chan LY, et al. Disparity of sensitivities in detection of radiation-naive and postirradiation recurrent nasopharyngeal carcinoma of the undifferentiated type by quantitative analysis of circulating Epstein–Barr virus DNA1, 2. Clin Cancer Res. 2003;9(9):3431–4.
Cao SM, Min HQ, Gao JS, Hong MH, Xiao XB, Zhang CQ, et al. Significance of cell-free Epstein–Barr virus DNA in monitoring prognosis of nasopharyngeal carcinoma. Ai Zheng. 2003;22(3):302–6.
Hong RL, Lin CY, Ting LL, Ko JY, Hsu MM. Comparison of clinical and molecular surveillance in patients with advanced nasopharyngeal carcinoma after primary therapy: the potential role of quantitative analysis of circulating Epstein–Barr virus DNA. Cancer. 2004;100(7):1429–37. https://doi.org/10.1002/cncr.20129.
Wang WY, Twu CW, Lin WY, Jiang RS, Liang KL, Chen KW, et al. Plasma Epstein–Barr virus DNA screening followed by (1)(8)F-fluoro-2-deoxy-d-glucose positron emission tomography in detecting posttreatment failures of nasopharyngeal carcinoma. Cancer. 2011;117(19):4452–9. https://doi.org/10.1002/cncr.26069.
Liang FY, Sun W, Han P, Lu X, Lian YN, Huang XM. Detecting plasma Epstein–Barr virus DNA to diagnose postradiation nasopharyngeal skull base lesions in nasopharyngeal carcinoma patients: a prospective study. Chin J Cancer. 2012;31(3):142–9. https://doi.org/10.5732/cjc.011.10279.
Hsu CL, Chan SC, Chang KP, Lin TL, Lin CY, Hsieh CH, et al. Clinical scenario of EBV DNA follow-up in patients of treated localized nasopharyngeal carcinoma. Oral Oncol. 2013;49(6):620–5. https://doi.org/10.1016/j.oraloncology.2013.02.006.
Shen T, Tang LQ, Luo DH, Chen QY, Li PJ, Mai DM, et al. Different prognostic values of plasma Epstein–Barr virus DNA and maximal standardized uptake value of 18F-FDG PET/CT for nasopharyngeal carcinoma patients with recurrence. PLoS ONE. 2015;10(4):e0122756. https://doi.org/10.1371/journal.pone.0122756.
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC cancer staging manual. 7th ed. New York: Springer; 2010.
Le QT, Zhang Q, Cao H, Cheng AJ, Pinsky BA, Hong RL, et al. An international collaboration to harmonize the quantitative plasma Epstein–Barr virus DNA assay for future biomarker-guided trials in nasopharyngeal carcinoma. Clin Cancer Res. 2013;19(8):2208–15. https://doi.org/10.1158/1078-0432.CCR-12-3702.
Authors’ contributions
WFL and YZ contributed to study design, literature research, interpretation of findings, and writing of the manuscript. XBH, XJD, HP and RG contributed to data collection. LLT, LC and YS contributed to data analyses. JM contributed to critical review of data analyses and critical edit of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Approval for retrospective analysis of the patient data was obtained from the ethics committee of Sun Yat-sen University Cancer Center. Written consent was waived, while oral consent from the patients was obtained via telephone and documented by telephone recording.
Funding
This work was supported by grants from the Natural Science Foundation of Guangdong Province, China (No. 2015A030310033), the Health & Medical Collaborative Innovation Project of Guangzhou City, China (No. 201400000001), and the Key Laboratory Construction Project of Guangzhou City (No. 121800085). The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of this report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Li, WF., Zhang, Y., Huang, XB. et al. Prognostic value of plasma Epstein–Barr virus DNA level during posttreatment follow-up in the patients with nasopharyngeal carcinoma having undergone intensity-modulated radiotherapy. Chin J Cancer 36, 87 (2017). https://doi.org/10.1186/s40880-017-0256-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40880-017-0256-x