Abstract
Background & aims
Despite its high prevalence in the western world metabolic dysfunction-associated steatotic liver disease (MASLD) does not benefit from targeted pharmacological therapy. We measured healthcare utilisation and identified factors associated with high-cost MASLD patients in France.
Methods
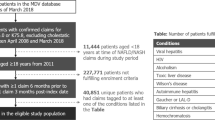
The prevalent population with MASLD (including non-alcoholic steatohepatitis) in the CONSTANCES cohort, a nationally representative sample of 200,000 adults aged between 18 and 69, was linked to the French centralised national claims database (SNDS). Study participants were identified by the fatty liver index (FLI) over the period 2015–2019. MASLD individuals were classified according as “high-cost” (above 90th percentile) or “non-high cost” (below 90th percentile). Factors significantly associated with high costs were identified using a multivariate logistic regression model.
Results
A total of 14,437 predominantly male (69%) participants with an average age of 53 ± SD 12 years were included. They mainly belonged to socially deprived population groups with co-morbidities such as diabetes, high blood pressure, mental health disorders and cardiovascular complications. The average expenditure was €1860 ± SD 4634 per year. High-cost MASLD cost €10,863 ± SD 10,859 per year. Conditions associated with high-cost were mental health disorders OR 1.79 (1.44–2.22), cardiovascular diseases OR 1.54 (1.21–1.95), metabolic comorbidities OR 1.50 (1.25–1.81), and respiratory disease OR 1.50 (1.11–2.00). The 10% high-cost participants accounted for 58% of the total national health care expenditures for MASLD.
Conclusion
Our results emphasize the need for comprehensive management of the comorbid conditions which were the major cost drivers of MASLD.
Graphical Abstract

Highlights
• MASLD is a prevalent but low cost condition
• Over 50% of NAFLD participants belong to the more deprived population group
• The low average cost may result from limited awareness about complications
• Higher healthcare costs for NAFLD treatments are associated with comorbid conditions, in particular psychiatric disorders, diabetes, cardiovascular and respiratory diseases.
Lay summary
Metabolic dysfunction-associated steatotic liver disease (MASLD) is the most common chronic liver disease in European countries, affecting 4–50% of the European population. Confirmation of diagnosis requires liver biopsy which is an invasive procedure. We studied the healthcare costs of patients with MASLD in order to identify cost predictors and cost drivers. We found that patients cost on average €1860 per year. Conditions associated with high-cost were mental health disorders, cardiovascular diseases, metabolic comorbidities, and respiratory disease.
Similar content being viewed by others
Introduction
Non-alcoholic fatty liver disease (MASLD) is the most common chronic liver disease in European countries, affecting 25.10% (20.55–30.28%) of the Western European population with a rapidly increasing prevalence [1,2,3,4]. In a study based on the CONSTANCES (CONSulTANts des Centres d’Examens de Santé) cohort, using the Fatty Liver Index (FLI), an algorithm based on body mass index, waist circumference, triglycerides and gamma glutamyl transferase, the estimated prevalence of MASLD in France was 18.2% [5].
MASLD is considered a “silent” disease, as many patients do not show specific symptoms, are not diagnosed and do not seek healthcare until they are at an advanced stage. In many cases, symptoms are attributed to metabolic comorbidities (including diabetes mellitus (DM), hyper-lipidaemia and dyslipidaemia, which are associated with increased risk of cardiovascular disease (CVD) and chronic kidney disease) commonly associated with MASLD. Confirmation of the diagnosis of MASLD is by liver biopsy, which is not routinely performed in the absence of approved therapies to treat diagnosed patients.
Given the increasing prevalence of MASLD, the economic burden is undoubtedly considerable despite the low cost per patient. In a Markov modelling study, the economic impact of MASLD in France was estimated at €784 per patient per year [6]. However, this study was built on several modelling assumptions including a 23% prevalence and expert opinion to estimate healthcare resource use. Circumventing these limitations, another study conducted in adults diagnosed with MASLD/ non-alcoholic steatohepatitis (MASH) from the French hospital claims database between 2009 and 2015 estimated annual hospitalization costs per patient at €7736 [7]. Although this study provided direct cost data, it included only patients with a hospital admission and therefore at more advanced stages of liver disease and comorbid conditions including cardiovascular or renal disease.
The clinical and economic impact of comorbidities among MASLD participants cannot be neglected because of the poor health outcomes and the multiple expenses incurred, either due to a higher prevalence of hospitalizations and clinic visits or due to an increase in the number of drugs used. The objectives of this study were to: 1) evaluate the use of healthcare resources by MASLD patients; 2) evaluate which factors are associated at a higher cost in MASLD patients.
Methods
A prevalence-based cost study was performed using 2019 French health administrative databases.
Database
The study sample was derived from the CONSTANCES cohort, a population-based prospective cohort study that included 220,000 volunteers aged from 18 to 69 years at 21 health examination centers throughout France between 2012 and 2020 [8]. Participants in the cohort were randomly selected within the National Health Insurance Fund beneficiaries. In France, all salaried and self employed workers—whether active or retired—and their families, are affiliated to the National Health Insurance Fund (“Caisse Nationale d’Asssurance Maladie des travailleurs salaries”, CNAMTS) which covers approximately 97% of the French population. At inclusion, a health examination was performed by a physician, and self-administered questionnaires with items on lifestyle, health status, medical history, socio-economic status, occupational exposures and lifetime employment history were completed by the eligible participants at home. Each participant visits 1) a health screening centre for a full assessment including a physical examination and laboratory tests; and 2) one of CONSTANCES’s recruitment centers for a comprehensive evaluation including a physical examination and laboratory tests. Health data from CONSTANCES cohort is linked at the individual level to healthcare reimbursement data recorded in the French national health insurance information system (SNDS). The SNDS contains the data on claims submitted for all healthcare resources: primary care (types and dates of procedures performed by private physicians, dentists, etc.; medical devices and associated services, reimbursed drugs, etc.); private and public hospitalizations; cash benefits (sick leave, disability pensions, workers’ compensation, occupational disease, or death benefits).
Patient population
We studied the prevalent population of MASLD (including MASH) in participants in CONSTANCES, aged ≥18 years on December 31, 2019, identified by the fatty liver index (FLI), over the period 2015 to 2019, having claimed at least one healthcare reimbursement during the year 2019 and still alive as of December 31, 2019 [9].
Patient characteristics
Factors assessed for association with healthcare utilization included demographics, socioeconomic characteristics (e.g. age, sex, educational level, social deprivation index), Charlson Comorbidity Index (CCI) and comorbidities [10]. Presence of comorbidities (56 treated diseases, episodes of care, chronic treatments) was identified by algorithms combining inpatient diagnoses international classification of diseases 10th revision (ICD-10) code, long-term disease code used by the social health insurance, pharmacy, laboratory tests and medical procedures reimbursement claims. The detailed methodology of the Diseases Mapping algorithms are publicly available in French [11]. Exclusion criteria or hierarchical rules apply to some algorithms, and some conditions are therefore mutually exclusive (e.g., acute ischemic heart disease is prioritized over chronic ischemic heart disease and, for a given location, currently treated cancer over history of cancer).
Outcome
The total healthcare cost was calculated as the sum of medical claims over a one-year period. It included all claims submitted. The French national health insurance information system database records the total cost of each claim, regardless of the reimbursement rate applied. MASLD individuals were classified as high cost (above 90th of the total healthcare cost) or “non-high cost” (below 90th of the total healthcare cost [12]. Costs were expressed in 2022 euros.
Statistical analysis
We described demographic, socioeconomic and clinical characteristics using means, and standard deviations for continuous variables, and frequency and percent for categorical variables. Patients were grouped in percentile of health care expenditures, high cost was defined as the 90th percentile and we used logistic regression to identify predictors of high cost. We first selected the variables corresponding to identified risk factors and complications (e.g. diabetes, hypertension, cardiovascular disease, mental health disorders) or homogeneous groups of conditions (e.g. inflammatory bowel diseases).
To combine highly correlated conditions within disease categories, we performed pairwise and multivariate correlation analyses. This procedure helps to prevent multicollinearity, without information loss. We also excluded conditions with very low explained variance (comorbidities with a prevalence < 0.1%). A logistic regression model with a logit link was used to identify the demographic, socioeconomic and clinical characteristics significantly associated with high costs, performed. On the demand side, we tested age, sex, comorbidities and socioeconomic characteristics; to describe the effect of supply or access to healthcare, we used the healthcare utilization of the previous year. Coefficients were exponentiated to express effects as rate ratio estimates. Variables for which a p-value lower or equal to 0.2 was observed in the bivariate analysis were included in the regression model. Models were generated iteratively using a forward building approach to ensure convergence could be attained. To generate the most parsimonious model, we excluded factors associated with a p-value greater than or equal to 0.05.
The adjusted odds ratios (ORs) were calculated and displayed with their respective 95% confidence intervals (95% CI).
All statistical analyses were conducted R statistical software version 4.1.3 (R studio).
Results
Study population and characteristics
We identified 14,437 prevalent individuals with MASLD in 2019 (Fig. 1) out of a total population of 92,313 (after excluding subjects with a history of chronic viral hepatitis or excessive alcohol consumption. This assessment made at the baseline recruitment visit and allow to avoid misclassification of MASLD diagnosis.) or 15.6%. The average age (mean ± standard deviation) was 53 ± 12 years; 39% were aged > 58 years. Of the total individuals, ~ 69% were males, and CCI scores were 0.8 ± 1.3. Characteristics of MASLD individuals are shown in Table 1.
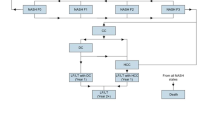
Half of the MASLD individuals belonged to the two worst deprivation quintiles, despite the fact that over 60% of the population reported high school or university education. Metabolic risk factors and diabetes were the most prevalent comorbidities, followed by mental health disorders. Figure 2 describes the association between MASLD/ MASH and risk factors/ cardiovascular complications. While not a longitudinal study, it shows the frequent association of MASLD with metabolic disease and mental health disorders. We also examined the combinations of comorbidities and risk factors (Fig. S2) and found that the most frequent were metabolic and metal health disorders, followed by cardiovascular and respiratory disease.
Healthcare costs in participants with MASLD
The mean healthcare expenditure per participant with MASLD was €1860 in 2019 (Table 2). Hospitalization represented the leading expenditure item with a mean of €673 representing 36% of all healthcare expenditure. Only 27% of MASLD individuals were hospitalised with primary diagnoses of diabetes, cardiovascular disease or mental health disorders. Of note, the mean length of stay was 0.6 ± 6 days. Pharmacy was also a substantial expenditure driver, representing 21% of all healthcare expenditure for 94% of MASLD patients. More specifically, about 35% of individuals with MASLD were treated for hypertension, 21% for dyslipidaemia, 15% for respiratory disease, and 9% for diabetes. Medical fees and paramedical visits accounted for 25% of healthcare expenditure (Table 2). 92% of patients visited the general practitioner in 2019, with a mean of 5 ± 4 visits. Nurses and physiotherapists were the main paramedical professionals consulted, by 46 and 32% of patients, respectively. Medical devices’ expenditure was driven by 10% of patients receiving ventilation at home including continuous positive airway pressure and oxygen therapy. Only 4 patients out of the 14,437 population had a procedural code for liver biopsy during the 2015–2019 period. For a total adult population of 53 million in France the estimated total healthcare cost was 15,7 billion €.
Characteristics of high-cost and non-high cost patients
Among MASLD individuals, 1444 were identified as being above the 90th percentile of the cost distribution (more than €4086 per year). Differences found between high cost and non-high cost individuals are described in Table 3. High cost individuals were older, more frequently female, and with multiple comorbidities, mostly metabolic (49.2% vs. 31.2%), mental health disorders (27.1% vs. 11.1%), cardiovascular diseases and stroke (19.3% vs. 5.8%), and respiratory disease (12.9% vs. 5.1%). No differences were found between high and non-high costs regarding social deprivation and education level. High-cost patients spent an average 5.6 days in the hospital, while non-high cost patients were barely hospitalized.
Distribution of healthcare expenditure
Table 4 shows the cost distribution for patients in the high cost and non-high cost groups. The total mean annual cost was €859 in the non-high cost and €10,863 in the high-cost group or a 12.6-fold increase. Hospital cost contributed to ∼51% of total cost in high-cost vs 16% in non-high cost. The 10% most expensive individuals incurred 58% of total MASH expenditures.
Factors associated with high-cost
The results of the bivariate logistic regression analysis are presented in Table S3. Based on these results, we included the following variables, presenting a p-value was lower than 0.2, in the multivariate logistic regression: sex, age, HC in 2018, Charlson Comorbidity Index score, metabolic comorbidities, cardiovascular diseases and stroke, mental health disorders, cancer, respiratory disease, HIV infection or AIDS, chronic inflammatory disease, and neurological and neurodegenerative disease.
Table 5 presents the multivariate logistic regression analysis results. After adjustment for other independent variables, of the comorbidities with a prevalence ≥5%, the highest odds for being a high-cost patient were associated with cardiovascular diseases and stroke (OR = 1.59, 95% CI: 1.25–2.03, p < 0.001), diabetes and other cardiovascular risk factors constitutive of metabolic syndrome (OR = 1.47, 95% CI: 1.22–1.78), respiratory disease (OR = 1.48, 95% CI: 1.10–1.98), and mental health disorders (OR = 1.77, 95% CI: 1.43–2.20); prostate cancer and colonic cancer were not selected because of their low prevalence. Additionally, the historical /supply effect measured by the health care utilization during the previous year had the highest impact, participants who were high users of healthcare in 2018 remained high users in 2019 (OR = 5.80 95% CI: 4.80–7.03). On the contrary, demographic characteristics did not have a significant impact on high-cost. While belonging to the most deprived population groups was associated with the risk of MASLD (Table 1), deprivation was no predictive of high cost, which might point to reduced access to care in this population. Patients in the two most deprived deciles had the same resource use as the average, both in terms of ambulatory and hospital care (Table S2).
Discussion
Main results and interpretation of the findings
We investigated the healthcare costs of individuals with MASLD and examined the characteristics of high-cost patients. MASLD is a high-prevalence but low-cost condition due in part to the lack of specific diagnostic tests and treatments, which leaves the patient population largely unattended. In our analysis of a representative sample of the French population, we found a prevalence of 15.6% and an average yearly cost of 1860€ (2676 US$), which is lower than the average yearly per capita healthcare expenditures in the French, or EU 27 populations (from €5000 in Germany to just below €2000 in Greece) and lower than the average cost of diabetic patients in France (2300€). Patients were treated by their general practitioners (92% had a consultation) and specialists, high-cost patients were referred to specialists and admitted to hospitals, but that may be for any of their other conditions. In this French population, the costs of laboratory tests was low (71€ per patient per year), which suggests no excessive use of liver function tests or other procedures: this might be the result of either good compliance with guidelines, or ignorance altogether of the disease [13].
The linkage with the national claims database provided quasi certainty that the diagnosis of MASLD was nearly never confirmed by a liver biopsy. We confirmed that high cost MASLD was associated with metabolic syndrome and a number of comorbid conditions, including mental health disorders [13]. In terms of other comorbidities, cardiovascular diseases, metabolic comorbidities, and respiratory diseases represented the most prevalent conditions. The 10 % most expensive patients with MASLD and other comorbid conditions incurred 58% of healthcare expenditures which is in accordance with the published range of 55–77% for high cost patients in general [14].
The drivers of high costs were hospital admissions and drugs; part of the utilization may be explained by a supply-induced demand or failure to coordinate the care for shared risk factors between diabetes, cardiovascular disease, respiratory disease and mental health disorders. It is however impossible to separate legitimate from overuse of healthcare during a short follow up. Symmetrically, while we identified that patients in the most deprived groups had the highest risk of MASLD, we did not find association between deprivation and use of healthcare services. The simplest explanation on the supply side is the limited access to specialized care in this population, or lack of diagnostic awareness among general practitioners, absence of coordinated care pathways, or ‘one stop shops’ which could manage the risk factors and comorbidities. On the demand side, we saw that nearly all patients attend GP consultations and other health professionals, and use medications, which is in a way reassuring as it means some degree of health literacy and trust in the healthcare system.
Comparison with other studies
Our results align well with prior studies in the USA and Europe where the low cost of diagnosis and treatment of MASLD have been reported on population samples [15, 16]. The prevalence of MASLD reported in a previous study based on the CONSTANCES cohort after adjustment to ensure full representativeness of the French adult population was 18.2%, lower than the 25% worldwide estimate [5]. The total healthcare costs estimated at 15.7 billion € by our study also come close to the estimated 11.4 € billion in the model-based study of MASLD costs by Younoussi with 2015 cost data [6]. Regarding estimates for the MASH population, our results align well with prior studies in the USA and Europe where the low costs of diagnosis and treatment have been reported on population samples [15, 16]. We found a pattern of resource utilization of general practitioners and specialists consistent with the results of the National Health and Wellness Survey, albeit lower as can be expected for MASLD vs MASH patients [17]. Lower costs of € 699–771 for healthcare were reported for the MASH population in France, based upon prevalence estimates and literature data [16]. This was unexpected because the CONSTANCES cohort identifies also patients who are not diagnosed and therefore not actively monitored, however the cost of illness study by Schattenberg et al. estimated a ‘pure’ cost for MASH, without the additional resource use unrelated to the liver disease such as the metabolic syndrome and MASH complications, which affect roughly half of the MASLD population in our study (Fig. 2) [18].
Strengths
These results on the high prevalence of MASLD, combined with our data on the drivers of high resource utilization suggest the need to better identify and monitor patients requiring the more expensive care, a group likely to include patients with significant comorbidities [13]. We also confirmed that MASLD affects predominantly low income patients [19]. However, being in the two most socially deprived quintiles did not result in fewer consultations with healthcare professionals or lower use of hospital care, possibly because the use of healthcare resource is already low. The fact that cardiovascular diseases, metabolic comorbidities and respiratory disease were strong predictors of high-cost is consistent with the pathology of MASLD. These comorbidities are common resource-intensive conditions and hare risk factors. Similarly, psychiatric disorders were significantly more common in the high-cost group. Another important finding is the recurrence of high costs in the same cluster of patients, which could allow targeting a group of persistent high-healthcare users for specific interventions on the comorbidities and the care pathways.
Limitations
The major limitation of this study was the potentially existing selection bias. Participants selected in the CONSTANCES cohort are volunteers whose characteristics are different from the general population, particularly in terms of education and lifestyle (despite adjustment on demographic characteristics). Better lifestyle in CONSTANCES participants lead to a lower prevalence of metabolic diseases and, therefore, to a loss of power in statistical measures of association. Identification of MASLD patients used the fatty liver index, in the absence of a better marker and in particular the near total absence of liver biopsies. However, the diagnostic performance of this surrogate marker has been re assessed by a meta analysis, with a sensitivity 0.67 (CI 95% 0.62, 0.72) and specificity 0.78 (CI 95% 0.74, 0.83), it was considered the marker with highest diagnostic accuracy for MASLD [20]. Patients were not extracted from the CONSTANCES database using the newer cardiometabolic risk factors that are now part of the MAFLD definition [21]. Another limitation was that the relationships between clinical characteristics and medical costs does not allow causal interpretation due to the observational nature of data. This cost study was undertaken on a French population, which limits its external validity outside Europe (in the USA for example), but not inside Europe, as shown by the GAIN study [16]. Finally, our cost calculations excluded non-medical direct and indirect costs, which have been shown to amount to roughly the same as medical costs [16].
Conclusion
The objective of the QUID MASH (Quantitative imaging in diabetic non-alcoholic steatohepatitis) project was to advance better care pathways for patients with MASLD and MASH, by understanding their unmet needs. We found that a majority of patients with MASLD do not have biopsies and therefore no diagnostic confirmation.
Metabolic and mental health comorbid conditions drove the use of healthcare resources. Given the lack of targeted pharmacological therapy for MASLD, the overall management of the MASLD patients requires interventions that holistically address the need of patients with multimorbidity risk factors, such as lifestyle services, educational programmes, and obesity programmes, or increased MASLD pathway capacity [19]. Regular physical activity has been shown to reduce the risk of developing MASLD and should become part of the integrated patient management particularly in view of the possible prescription and reimbursement of supervised formal exercise programs [20].
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- CONSTANCES:
-
CONSulTANts des Centres d’Examens de Santé; patients recruited in primary care centers
- FLI:
-
Fatty Liver Index
- QUID-NASH:
-
Quantitative imaging in diabetic non-alcoholic steatohepatitis
- SNDS:
-
système national des données de sante; French national health claims data base
References
Younossi ZM, Golabi P, Paik JM, Henry A, Van Dongen C, Henry L. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Hepatology. 2023;77(4):1335–47.
Nabi O, Lacombe K, Boursier J, Mathurin P, Zins M, Serfaty L. Prevalence and Risk Factors of Nonalcoholic Fatty Liver Disease and Advanced Fibrosis in General Population: the French Nationwide NASH-CO Study. Gastroenterology. 2020;159(2):791–793.e2.
Allen AM, Lazarus JV, Younossi ZM. Healthcare and socioeconomic costs of NAFLD: A global framework to navigate the uncertainties. J Hepatol. 2023;79(1):209–17.
Boursier J, Shreay S, Fabron C, Torreton E, Fraysse J. Hospitalization costs and risk of mortality in adults with nonalcoholic steatohepatitis: Analysis of a French national hospital database. EClinicalMedicine. 2020;25:100445.
Zins M, Goldberg M, CONSTANCES team. The French CONSTANCES population-based cohort: design, inclusion and follow-up. Eur J Epidemiol. 2015;30(12):1317–28.
Bedogni G, Bellentani S, Miglioli L, Masutti F, Passalacqua M, Castiglione A, et al. The fatty liver index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006;6(1):33.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Berkman ND, Chang E, Seibert J, et al. Characteristics of high-need, high-cost patients. A “best-fit” framework synthesis. Ann Intern Med. 2022;175:1728–41. https://doi.org/10.7326/M21-4562.
Pryke R, Guha IN. Time to focus on chronic liver diseases in the community: A review of primary care hepatology tools, pathways of care and reimbursement mechanisms. J Hepatol. 2023;78(3):663–71.
Wammes JJG, van der Wees PJ, Tanke MAC, Westert GP, Jeurissen PPT. Systematic review of high-cost patients' characteristics and healthcare utilisation. BMJ Open. 2018;8(9):e023113.
Geier A, Heinz S, Balp MM, Brass C, Pedrosa M, Cai J, et al. The cost of diagnosing and managing non-alcoholic steatohepatitis in Europe and the United States. J Gastrointestin Liver Dis. 2022;31(3):317–22.
O'Hara J, Finnegan A, Dhillon H, Ruiz-Casas L, Pedra G, Franks B, et al. Cost of non-alcoholic steatohepatitis in Europe and the USA: the GAIN study. JHEP Rep. 2020;2(5):100142.
Balp MM, Krieger N, Przybysz R, Way N, Cai J, Zappe D, et al. The burden of non-alcoholic steatohepatitis (NASH) among patients from Europe: a real-world patient-reported outcomes study. JHEP Rep. 2019;1(3):154–61.
Schattenberg JM, Lazarus JV, Newsome PN, Serfaty L, Aghemo A, Augustin S, et al. Disease burden and economic impact of diagnosed non-alcoholic steatohepatitis in five European countries in 2018: a cost-of-illness analysis. Liver Int. 2021;41(6):1227–42.
Ventura-Cots M, Bataller R, Lazarus JV, Benach J, Pericàs JM. Applying an equity lens to liver health and research in Europe. J Hepatol. 2022;77(6):1699–710.
Contreras D, González-Rocha A, Clark P, Barquera S, Denova-Gutiérrez E. Diagnostic accuracy of blood biomarkers and non-invasive scores for the diagnosis of NAFLD and NASH: systematic review and meta-analysis. Ann Hepatol. 2023;28(1):100873.
Castera L, Laouenan C, Vallet-Pichard A, Vidal-Trecan T, Manchon P, Paradis V, et al. High prevalence of NASH and advanced fibrosis in type 2 diabetes: a prospective study in 330 outpatients undergoing liver biopsies for elevated ALT using a low threshold. Diabetes Care. 2023;46(7):1354–62.
Lazarus JV, Mark HE, Allen AM, Arab JP, Carrieri P, Noureddin M, et al. Healthy lives collaborators. A global research priority agenda to advance public health responses to fatty liver disease. J Hepatol. 2023;79(3):618–34.
Stine JG, Long MT, Corey KE, Sallis RE, Allen AM, Armstrong MJ, et al. American College of Sports Medicine (ACSM) international multidisciplinary roundtable report on physical activity and nonalcoholic fatty liver disease. Hepatol Commun. 2023;7(4):e0108.
Rinella ME, Lazarus JV, Ratziu V, Francque SM, Sanyal AJ, Kanwal F, et al. NAFLD nomenclature consensus group. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. Hepatology. 2023;78(6):1966–86.
Acknowledgements
We thank the CONSTANCES participants for their commitment and the team of the “Population-based Cohorts Unit” (Cohortes en Population) that designed and manages the CONSTANCES Cohort Study.
A - QUID-NASH Research Group (conception).
Coordination of QUID-NASH project: Coordinateur du projet, Dominique Valla; Cheffe de projet, Angélique Brzustowski; Commissariat à l’Energie Atomique (CEA), Christophe Junot, Benoit Colsch, Francois Fenaille, Florence Castelli; Servier, Nathalie De Preville/Tania Baltauss / Philippe Delerive; BioPrédictive, Thierry Poynard; chefs de WP, Valérie Paradis (WP2), Bernard Van Beers (WP3), Christian Boitard (WP4), Cédric Laouénan (WP5), Isabelle Durand Zaleski (WP7).
B - QUID-NASH participants.
Hôpital Beaujon group (Université de Paris, Assistance Publique-Hôpitaux de Paris and Inserm CRI-UMR1149): service d’hépatologie, Dominique Valla, Laurent Castéra, and Pierre-Emmanuel Rautou; service de radiologie, Bernard Van Beers, Valérie Vilgrain, Philippe Garteiser, Marco Dioguardi-Burgio, and Sabrina Doblas; and service d’anatomie-pathologique, Valérie Paradis, Pierre Bedossa, Miguel Albuquerque and Adel Hammoutene.
Hôpital Lariboisière group (Université de Paris, Assistance Publique-Hôpitaux de Paris and Inserm U1138: Service de d’endocrinologie – Centre Universitaire du Diabète et de ses Complications CUDC: Jean-François Gautier, Tiphaine Vidal-Trécan, Jean-Pierre Riveline and Jean-Baptiste Julla.
Hôpital Cochin group (Université de Paris, Assistance Publique-Hôpitaux de Paris and Institut Cochin): service de diabétologie, Christian Boitard and Etienne Larger; service d’hépatologie, Stanislas Pol and Anaïs Vallet-Pichard; service d’anatomie pathologique, Benoît Terris; centre ressources biologiques, Béatrice Parfait; signalisation de l’insuline et du glucose, glucotoxicité, Catherine Postic; immunologie du diabète, Agnès Lehuen, Amine Toubal, Camille Rousseau, Blandine Fruchet, Pauline Soulard and Zouriatou Gouda; génomique, Michel Vidaud and Franck Letourneur; imagerie du vivant, Gilles Renault; and régulation des cellules béta pancréatiques Raphaël Scharfmann.
Hôpital Necker-Enfants Malades group (Université de Paris, Assistance Publique-Hôpitaux de Paris and Inserm): service de radiologie, Jean-Michel Corréas.
Hôpital Européen George Pompidou research group (Université de Paris, Assistance Publique-Hôpitaux de Paris and Inserm UMR1153): service de nutrition, Sébastien Czernichow, Claire Carette, and Charles Barsamian, Amel Ait-Boudaoud, Claire Rives-Lange, Alina Radu.
Hôpital Avicenne group (Université Paris 13, Assistance publique-Hôpitaux de Paris and Inserm U955, équipe 18, Université Paris-Est, Créteil): service de médecine interne, Dominique Roulot-Marullo; and service de diabétologie, Hélène Bihan and Emmanuel Cosson.
Physics for Medicine Paris group (Inserm, CNRS and Ecole supérieur de Physique et Chimie de Paris ESPCI): Mickael Tanter, Thomas Deffieux, Sofiane Decombas, and Thu-mai Nguyen
Laboratoire d’Imagerie Biomédicale (Inserm, Sorbonne Université and CNRS): Olivier Couture and Rachel Baida.
Département d’Epidémiologie, Biostatistiques et Recherche Clinique HUPNVS (Université de Paris, Assistance Publique-Hôpitaux de Paris Inserm IAME-UMR1137 and URC PNVS): Cédric Laouénan, Jimmy Mullaert, Delphine Bachelet, Nathalie Gault, Estelle Marcault,Nassima Si-Mohammed Pauline Manchon, Basma Basli-Baillet and Krishna Bhavsar.
Servier: Nathalie de Préville, Philippe Delerive, Tania Baltauss, Erwan Werner, Laura Xuereb, Julia Geronimi, Jessica Laplume, Valérie Duvivier, Pierre Barbier Saint Hilaire and Edwige-Ludiwyne Balzac.
Swiss Institute of Bioinformatics: Vital-IT Group, SIB Swiss Institute of Bioinformatics: Mark Ibberson, Olivier Martin, Florence Mehl, Robin Liechti and Manuela Pruess.
BioPrédictive: Thierry Poynard, Olivier Deckmyn.
Commissariat à l’Energie Atomique: Christophe Junot, François Fenaille, Florence Castelli and Benoit Colsch.
C – Supporting staff, research associates.
Vanessa Legrand, Dahia Sekour, Djamila Bellili, Miassa Slimani, Fatima Zohra Djelouat, Ouarda Bessadi, Benoit Girard, Manon Sens, Ouassila Zatout, Nathalie Neveux, Meriam Meziani, Charlene Da Silveira, Ludovic Roy.
Funding
RHU QUID-NASH is funded by Agence Nationale de la Recherche (ANR) under the reference ANR-17- RHUS-0009; implemented by Inserm, Université Paris Descartes, Université Paris Diderot, CNRS, CEA, Laboratoires Servier, Biopredictive, and AP-HP; and coordinated by Prof. Dominique Valla and Angélique Brzustowski.
The CONSTANCES Cohort Study was supported and funded by the French National Health Insurance Fund (“Caisse Nationale d’Assurance Maladie” (CNAM)). The CONSTANCES Cohort Study is an “Infrastructure Nationale en Biologie et Santé” and benefits from a grant from the French National Agency for Research (ANR-11-INBS-0002). CONSTANCES is also partly funded by Merck Sharp & Dohme, AstraZeneca, and L’Oréal. None of the funding sources had any role in the design of the study, the collection, analysis and interpretation of data, or in the writing of the report and decision to publish.
Author information
Authors and Affiliations
Contributions
All the authors listed in the contributors’ affiliations meet the ICMJE Authorship Criteria, that is, they substantially contributed to conception and design (MZ DV IDZ ANO), acquisition of funding (AB VP BVB CP CL SP LC JFG SC AVP EL MZ DV IDZ), acquisition of data (MZ IDZ ANO), drafting of the article, critical revision (AB VP BVB CP CL SP LC JFG SC AVP EL LS MZ DV IDZ), and final approval of the manuscript (AB VP BVB CP CL SP LC JFG SC AVP EL LS MZ DV IDZ).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This epidemiological study is based solely on data already collected. The CONSTANCES Cohort has obtained the authorization of the National Data Protection Authority (Commission nationale de l’informatique et des libertés—CNIL) on March 3, 2011 n°2011–067. This study was approved by CONSTANCES external scientific committee and conducted in accordance with the national data protection authority reference guideline (MR004).
Consent for publication
All authors gave their consent for publication.
Competing interests
Pr Castera has received lectures fees from Echosens and Novo Nordisk and has served as a consultant for Echosens, Novo Nordisk, Madrigal, MSD, Pfizer and Sagimet. Pr Pol has received consulting and lecturing fees from Janssen, Gilead, MSD, Abbvie, Biotest, Shinogui, Viiv, LFB and grants from Bristol-Myers Squibb, Gilead, Roche and MSD without relation to this manuscript. Pr Durand-Zaleski has received consulting and lecturing fees from Amgen, BMS, MSD, Sanofi, Pfizer, Takeda without relation to this manuscript. Pr Czernichow has received consulting and lecturing fees from Lilly, Fresenius, Novartis, Novo Nordisk, BMS, Boehringer, Bariatek without relation to this manuscript. Pr Jean-François Gautier received consulting and lecture fees from AstraZeneca, Bayer, Bristol-Myers Squibb, Eli Lilly, Gilead, Novo Nordisk, Pfizer, and Sanofi. Pr Valla has received lecture fees from Intercept. The other authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ossima, A.N., Brzustowski, A., Paradis, V. et al. Factors associated with high costs of patients with metabolic dysfunction-associated steatotic liver disease: an observational study using the French CONSTANCES cohort. Clin Diabetes Endocrinol 10, 9 (2024). https://doi.org/10.1186/s40842-023-00163-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40842-023-00163-4