Abstract
Background
Postpartum intrauterine contraceptives device (PPIUCD) offers an effective means of providing contraceptive services to women in countries with high rates of unmet needs for family planning services. However, scientific literature estimating the long-term retention rates is scarce. We estimate the factors affecting acceptance and retention of PPIUCD and explore the risk factors against PPIUCD Discontinuation at six months”.
Material and method
: This prospective observational study was conducted between 2018 and 20 at a tertiary care institute in North India. PPIUCD was inserted following a detailed counseling session and consent. The women were followed up for six months. Bivariate analysis was done to depict the association between socio-demographic characteristics and acceptance. Logistic regression, cox regression, and Kaplan Meier analysis were applied to explore factors affecting acceptance and retention of PPIUCD.
Results
Of the 300 women counseled for PPIUCD, 60% accepted them. The majority of these women were between 25 and 30 years (40.6%), primigravida (61.7%), educated (86.1%), and from urban areas (61.7%). Retention rates at six months were about 65.6%, while 13.9% and 5.6% were either removed or expelled. Women declined PPIUCD due to refusal by spouses, partial knowledge, inclination towards other methods, non-willingness, religious beliefs, and fear of pain and heavy bleeding. Adjusted logistic regression depicted that higher education, housewife status, lower-middle and richest SES, Hinduism, and counseling in early pregnancy promoted acceptance of PPIUCD. The most common reasons for removal were AUB, infection, and family pressure (23.1%). Adjusted hazard ratio depicted religion other than Hinduism, counseling in late stages of pregnancy, and normal vaginal delivery were significant predictors for early removal or expulsion. While education, higher socio-economic status favoured retention.
Conclusion
PPIUCD is a safe, highly effective, low-cost, long-acting, and feasible method of contraception. Skill enhancement of healthcare personnel for insertion techniques, adequate antenatal counseling, and advocacy of PPIUCD can help increase the acceptance of PPIUCD.
Similar content being viewed by others
Introduction
India has been experiencing exponential growth in population in recent decades, mainly driven by progress in the socio-economic and medical fields. This burgeoning population exerts colossal pressure on the already constrained resources, which have proved limited over time. As per the fourth round of the National Family Health Survey- an Indian counterpart for the Demographic Health Survey- Intrauterine devices have a meager contribution of just 1.5% among all the methods of contraception practiced for family planning. However, IUCD services are offered free of cost at all government facilities [1]. This is mainly attributed to the low level of knowledge, myths, and misconceptions, particularly for copper T, which has resulted in its low utilization and discontinuation [2].
Consecutive pregnancies occurring within 24 months of a previous birth have a higher risk of adverse outcomes [3, 4]. This calls for reliable and effective long-term contraception in the postpartum period. IUCD is a highly recommended method of contraception due to its safety, efficacy, coitus independence, rapidly reversible, and long-acting nature with relatively few side effects [5]. Also, women are highly motivated during the postpartum period and have minimal need for additional hospital visits [6]. Insertion of IUCD in the immediate postpartum period (PPIUCD) is a technique of insertion of IUCD within 48 h of vaginal delivery or cesarean section after removal of the placenta. The copper ions released from the IUCD offer long-term contraception by interfering with the ability of sperm to survive and ascend the fallopian tube where fertilization occurs. It also stimulates a sterile foreign body reaction in the endometrium potentiated by copper [7].
In India, PPIUCD is still emerging as a new contraceptive choice where delivery may be the only time a healthy woman comes in contact with health care personnel. It has been observed that the expulsion rate of PPIUCD varies according to the clinician’s skill. In addition, follow-up care of the PPIUCD is critical to ensure client satisfaction and the continuation of the accepted method [8]. Limited studies have been conducted so far in India about the safety, follow-up data on complications, decision-making, perception, and satisfaction among the women who accepted PPIUCDs [7, 9,10,11]. In this context, we did the present study to estimate the factors affecting acceptance and retention of PPIUCD and explore the risk factors against PPIUCD discontinuation at six months” in women undergoing delivery in our institution.
Methods
Study area and period
The study was conducted between 2018 and 20 in a tertiary care teaching health facility in the Malwa region of Punjab, India’s northern state. It is a private facility where family planning, Antenatal care (ANC), and delivery services are provided at a nominal charge. It serves as a referral center for complicated ante-natal cases by offering state-of-the-art blood banks, operation theatre, and intensive care for the mother and child. Modern contraceptive methods (injectables, pills, implants, male condoms) are offered to clients in need after proper counseling and assessing their medical eligibility using the Medical Eligibility Criteria for Contraceptive Use (MEC) wheel as recommended by the World Health Organization.
Study design
A facility-based prospective observational study design was employed.
Study participants
Pregnant women between 28 and 42 weeks of gestation willing to use IUCD for postpartum contraception within 48 h of delivery were included in the study after explaining the purpose of the research and taking informed written consent to participate in the study. Pregnant women who did not fulfill World Health Organization medical eligibility criteria for IUCD insertion like those with HIV, antepartum hemorrhage, fever during labor and delivery, delivery at less than 28 weeks and with PROM more than 18 h, who had a previous history of genital tuberculosis, known allergy to copper, history of uterine abnormalities and not willing to participate were excluded from the study.
The Counseling and process of having consent were done per the guidelines by the Government of India [12]. During the process of giving counseling and obtaining informed consent from the participants, they were explicitly told about the possible benefits of using the PPIUCD, potential side effects and complications, the process of getting the PPIUCD removed, precautions to be taken, how to observe the PPIUCD and other available options of contraception in the postpartum period. Specifically, we ensured that she knows that menstrual changes are a common side effect among PPIUCD users and that the PPIUCD does not protect against STIs. Also, we described the medical assessment required before PPIUCD insertion and the procedures for PPIUCD insertion and removal. Concurrently, we encouraged her to ask questions throughout the process and provided any other additional information and reassurance as needed.
Sample size and sampling
A sample size of 289 was calculated using the single population proportion formula after considering the overall acceptance of PPIUCD to be around 25%[13], with a 95% confidence interval and a margin of error of 5%. We included a total of 300 participants in the study. Eligible pregnant women were recruited from the OPD or emergency labor room using a systematic random sampling technique.
Data collection
The structured and pre-tested questionnaire was prepared first in English from peer-reviewed articles and then translated into Hindi and Punjabi (local languages), using the standard WHO methodology for questionnaire translation. The tool consisted of three sections: Part A included questions to collect information regarding the socio-demographic factors (age, education, occupation, socio-economic status, religion, residence) and obstetric history (parity, timing of PPIUCD insertion, client perception of pain during and after PPIUCD insertion and time since last childbirth); while part B had questions about the acceptance of PPIUCD, decision making about PPIUCD ( Period of counseling, decision making in PPIUCD as family planning method, reasons for acceptance and declining of PPIUCD, Time of the decision taken to choose PPIUCD as family planning method), and Part C collected data from the follow-up visits (acceptance of PPIUCD, side-effects, reason for removal and satisfaction). The study tool was pilot tested in 30 pregnant women and incorporated necessary changes in the final version. The authors collected data after ensuring the study subjects’ confidentiality and privacy, maintaining a non-judgemental attitude to minimize bias.
After taking universal precautions, a procedure was carried out on patients who consented to participate in the study. In women who had a normal vaginal delivery, after the expulsion of the placenta, the IUCD was held in suitably long forceps without a lock (Kelly’s forceps). The instrument was taken to the uterine fundus, and the IUCD was released. While in a cesarean section, the IUCD was introduced through the uterine incision after removal of the placenta and placed at the uterine fundus. This was done manually or using artery forceps, and the strings were directed towards the os.
Women who accepted PPIUCD insertion were advised to follow up routinely after six weeks, three months, and six months on an outpatient basis. On follow-up visits, the position of IUCD was verified by per speculum and vaginal examination. If the participant did not feel the threads, pelvic ultrasound or radiography of the pelvis was done. The findings on their follow-up visit like expulsion, reasons for removal, continuation rate, loss to follow up, and any complications like menstrual problems, infection/discharge per-vaginum, pyrexia, abdominal pain or backache, lost or missing thread, perforation, and pregnancy were noted.
Data analysis
Data was entered in the Microsoft Excel sheet and checked for completeness and inconsistencies by the principal investigator. It was analyzed using SPSS version 21( IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp). We conducted a bivariate analysis to assess any association between independent variables (the socio-demographic characteristics and counseling process) and the dependent variable (PPIUCD acceptance). Further, we did a multivariable logistic regression analysis to explore factors affecting the acceptance of the PPIUCD. At the same time, a Cox proportional hazard model was used to estimate hazard ratios (HRs) of variables associated with discontinuation. Independent variables with a significant association (p < 0.2) in the bivariable analysis were entered into the multivariable analysis. The final model declared a significant association at a p < 0.05. The results were presented in tables with adjusted odds ratio (AOR) and the corresponding 95% confidence interval. Kaplan-Meier survival function was used to estimate the continuation rates for the PPIUCD at six months after insertion.
Ethical considerations
Ethical approval was obtained from the research review committee of Adesh Institute of Medical Sciences and Research, Bathinda, Punjab (AU/EC/FM/133/ 2018). We obtained written informed consent from each study participant. We also ensured the confidentiality of the information to all participants throughout the study, and the data was made anonymous for analysis. Withdrawal from the study at any point was assured to all the participants.
Results
Of the 300 women counseled for PPIUCD, 60% accepted using it as a contraceptive method in their postpartum period. (Table 1) Acceptance of PPIUCD was significantly higher (p-value < 0.05) in educated women, homemakers, higher socio-economic status, following Sikhism and Hinduism, rural areas of residence, positive history of family planning usage in the past, and even the types of methods used in the past. However, the participant’s age, gravidity, and time since the last childbirth did not affect the chances of accepting PPIUCD. Further, we assessed the effect of counseling on the prospects of acceptance (Table 2). It was seen that the acceptance was significantly higher when counseling was provided in the ante-natal period when the respondent was the sole decision-maker and those who ended up having a cesarean section. All of the respondents who were counseled (n = 180) and finally accepted PPIUCD reported satisfaction with the counseling services. The most common reason for PPIUCD acceptance in the present study was its long lifetime period (42.2%), non-hormonal action (16.1%), non-interference with breastfeeding (15.6%) as seen with hormonal pills, the safety of usage (10.6%), need for fewer follow-ups (8.3%) and reversibility of fertility after removal (7.2%). However, women who declined (n = 120) PPIUCD cited reasons of either refusal by their husbands (23.33%), concern about the partial/incomplete knowledge (18.3%), preference for other methods (17.5%), non-willingness to adopt any contraception immediately (15.8%), religious beliefs (15%) and due to fear of pain and heavy bleeding after insertion (10%). Nevertheless, in our study, 67.2% of participants perceived no pain at the time of PPIUCD insertion (immediately following the delivery), while only 8.3% admitted it to be very painful (data not tabulated).
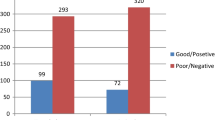
By the end of 3 months, the proportion of respondents who retained their PPICUD was 65% and remained the same even at six months. Among those non-compliant, 6.7% and 3.3% of respondents got their PPICUD removed by the end of six weeks and six months, respectively. In 3.3% and 5.6% of cases, IUCD got expelled spontaneously, while 6.7% and 15% could not be contacted and were lost to follow-up (Table 3; Fig. 1). We also explored the reasons for removing PPIUCD from 12 to 13 women who got Cu T removed at six weeks and three months. At six weeks, the main reasons included AUB (66.67%) and infection (16.67%), while at three months, the reasons included AUB (53.84%), and family pressure (23.1%). We also recorded the complications following PPIUCD insertion at the three follow-up visits. At six weeks, 62 women reported complications which mainly included AUB (10.7%), missing threads (9.5%), and infection/per-vaginal discharge (8.3%). At the end of 3 months, the most common complication was AUB (10.2%), while infection and per-vaginal discharge (3.8%) were most commonly reported at six months.
Further, unadjusted binary logistic regression depicted that the most common factors for acceptance of PPIUCD included age between 26 and 35 years, education, employed or housewife, from the lower middle or richest SES, Hindu and Muslim religion, urban residence, primigravida, and counseling in the immediate postpartum period (Table 4). However, adjusted logistic regression depicted education, housewife, lower-middle and richest SES, Hinduism, and counseling in the antenatal and immediate postpartum period as final predictors of acceptance of PPIUCD during counseling sessions. Then, a bivariate analysis of the participants who received a PPIUCD with different socio-demographic variables depicted that type of occupation, religion, and time of counseling for PPIUCD affected retention significantly. Cox hazard regression analysis illustrated that the chances of the event (removal and expulsion) happening were significantly higher in women following religion other than Hinduism, those who had received counseling for the first time during the intrapartum period or had undergone normal vaginal delivery, while education, unorganized labor class, higher socio-economic status emerged as protective factors against the removal or expulsion. (Table 5). Figure 2 shows Kaplan-Meier survival estimates for PPIUCD retention at the end of six months.
Discussion
We highlight the effect of adequate counseling services on the long-term retention of PPIUCD and thus harness their actual potential as a practical family planning method. The revival of PPIUCD by the Ministry of Health and Family Welfare, Government of India, with technical assistance from Jhpiego in 2010, led to conscious efforts to provide the benefits of this long-term reversible postpartum contraception [14]. In our study, 60% of women accepted PPIUCD as a method of contraception during their postpartum period. This is higher than the acceptance observed by Agarwal N al et al. (41.1%) and Gautam R et al. (21.8%) [11, 15]. The origin of these studies was from the low-performing states of India in terms of Family planning. To add, in our institute, Cu T 380 A is available free of cost with support from the Government of India. Therefore, numerous advantages supplemented by no-cost contraceptive makes pregnant women more receptive to PPIUCD. Many socio-demographic factors are responsible for higher acceptance and are discussed in the subsequent parts of the manuscript.
We observed that the acceptance of PPIUCD as a long-term family planning method is significantly affected by education, SES, religion, and appropriate counseling, especially in the antenatal period. Similar results were seen in a study by Rajni Gautam et al., Kanhere AV et al., and Pandher et al. [15,16,17]. Nearly 77% of our acceptors were educated women, similar to other studies [11, 17]. Most of them belonged to urban areas, which was in concurrence with the study conducted by Patel J et al. (93.14%) and Mule VD et al. (62.5%)[18, 19]. This reveals that women’s education status and urban residence significantly influence the acceptance of PPIUCD. This also highlights the need for targeted interventions for better acceptance among less-educated women and those in rural areas where healthcare services are relatively deficient and inaccessible. We observed that acceptance for PPIUCD was highest in the wealthiest economic group. However, Agarwal N et al. noted higher acceptance in those with lower socioeconomic status [11]. The difference needs further evaluation to account for undue disparities based on SES. We also observed that the acceptance was not affected by the parity of women. However, primiparous women were more inclined towards the spacing method, while multipara women were interested in the permanent form of contraception. Similar results were seen in the study by Garuda L et al. (67.3%) and Mishra et al. (20.7%)[8, 20].
Acceptance increased when the respondent was the sole decision-maker or counseled during a cesarean section. Anecdotally, it is seen that it is easy to guide and convince about the benefits of PPIUCD usage the educated women who have a say in the decision-making process. However, the decision-making among uneducated women is primarily influenced by their family members and guided by societal norms—most of the PPIUCD acceptors who were counseled decided after discussing it with their husbands. The involvement of husbands during the counseling session increases the chances of acceptance of PPIUCD as contraception[20,21,22]. However, men must be engaged in counseling through tailor-made approaches[23]. We also counseled the women adequately about the benefits of PPIUCD during their intrapartum period, which essentially convinced them to choose PPIUCD as a family planning method, similar to observations made in previous studies [24, 25]. Women undergoing cesarean section showed a higher acceptance rate of PPIUCD, similar to other studies from India and abroad[7, 15, 26, 27]. This can be attributed to fear of post-cesarean conception over the scarred uterus. Previous systematic reviews have reported that post-placental placements during cesarean delivery are associated with lower expulsion rates than post-placental vaginal insertions without increasing rates of postoperative complications.
[28, 29] Satisfaction from the counseling services is also a significant determinant of acceptance and long-term retention. As per WHO, the role of counseling cannot be ignored as it supports a woman and her partner in choosing the method of family planning that best suits them. It also involves them in making an informed decision and addresses any concerns with the selected contraceptive method. Thus, if a woman can make an informed choice about any contraceptive method, it increases her acceptance, satisfaction, and usage [30].
The most common reasons for PPIUCD acceptance that emerged in our study align with the existing literature [16, 24, 31,32,33]. Immediate postpartum period is the appropriate time to begin contraception as women are highly motivated and not known to be pregnant. There is no need for additional hospital visits for insertion, which also has the advantage of being convenient for both women and health care providers. We observed that the most common reasons for declining PPIUCD were resistance from the family members, notably the husband, insufficient knowledge about PPIUCD, preference for other less invasive methods of contraception, and fear of side effects, similar to other studies [16, 24, 31,32,33]. Nigam A et al. have also pinpointed ineffective counseling as a crucial factor for refusal [34]. In our hospital, women were not accompanied by their partners during the antenatal visits, which deprives male spouses of understanding the PPIUCD benefits. Thus, partner refusal was the most common reason for denying PPIUCD. This again highlights the importance of partner involvement during counseling and decision-making, as stressed by previous studies [21,22,23].
The most common complications following PPIUCD insertion included AUB, missing thread, and infections, the most common reason for removal. Most of the missing thread complications were seen within six weeks in the women who had intra-cesarean insertion of PPIUCD because, at the time of insertion, there is the practice of leaving the entire length of IUCD string in the uterine cavity and not passing it through the cervical-os which leads to curling up of thread that is not visible at external-os. This may cause apprehension as the missing thread relates to expulsion, malposition, and perforation. However, there was no reported case of uterine perforation. None of the studies retrieved during the literature review has reported uterine perforation after PPIUCD insertion, except in one case report [35].
In the present study, we observed a continuation rate of about 80.6% and a removal rate of 13.9% at six months postpartum. This is similar to the results from previous studies by Ranjana et al. and Sunita Singhal et al. [36, 37]. Cox regression depicted that PPIUCD retention was affected by the type of occupation, religion, and normal vaginal delivery. About one-fifth of our respondents either got their PPIUCD removed, or it was expelled by the end of 6 months. We explored the reasons for the removal of PPIUCD. The main reasons for removal included pain, AUB, infection, and family pressure. These factors are in coherence with the existing literature [25, 34, 37,38,39,40,41]. Persistent pain was seen as a critical factor leading to removal. However, two-thirds of our participants perceived no pain during and after PPIUCD insertion, comparable with the study by Kumar S et al. [25]. This can be attributed to the use of the proper insertion technique by skilled health-care workers. Family pressure has been a critical determinant of retention of PPIUCD and a bottleneck for the effective implementation of women’s reproductive rights [8, 39, 40]. We observed a cumulative expulsion rate of 5.6% at the end of six months. In previous studies from India, the expulsion rate has been seen between 5 and 10% [8, 11, 25, 42, 43]. Expulsion rate can be minimized if PPIUCD is inserted by a trained health care provider and proper fundal placement by placental forceps. When the IUCD is inserted immediately after the third stage of labor, expulsion rates at six months range between 31 and 41% per a WHO multi-centric trial and from 12 to 22% in a Family Health International multicentre trial [4]. Insertion 1–7 days after delivery results in even higher expulsion rates and may vary between 5 and 10% [37, 41, 44]. Findings in the present study that expulsion is more common in post-placental insertion than intra-cesarean insertion is supported by many studies worldwide [8].
There are certain limitations in the present study that should be acknowledged. Being a time-bound study, we could not do a long-term follow-up of the participants and assess the actual impact of PPIUCD. Excessive bleeding may contribute to high removal rates of PPIUCD after six months of delivery, which warrants further long-term follow-up as the same was not possible due to feasibility issues during the study. We also could not record the patterns of bleeding that prompted women to request IUD removal, which can be done in future studies. We could not rate the quality of PPIUCD counseling services and compare it with existing literature regarding the acceptance rates of PPIUCD. Our study’s follow-up loss was high (15%), similar to observations made by previous researchers field[45]. The loss of patients to follow-up is a significant problem in low and middle-income countries like India. Patients with poor education, low socio-economic status, and poor access to health care facilities tend not to give adequate importance to health-related issues. Lastly, this study was conducted in a health facility; hence the findings might not adequately reflect the entire population.
There is a pertinent policy implication of this study. Our study highlights the need to focus on the continuation rates rather than just the initial acceptance rate of PPIUCD. In the long run, the number of women years counted free of unwanted pregnancy has long-term effects on decreased Total fertility rates and population stabilization. Even if the lower proportion of women accept PPIUCD as a contraceptive method of choice but continue to use it for a longer time, it can trade off the need for a more significant number of women initially to accept PPIUCD. Previous reports have stated that health professionals discourage IUD removals within a year of placement regularly and downplayed or offer to treat side effects instead of giving patients a choice to have their IUD removed immediately [46]. Forcing women to continue using contraceptive methods against their will can diminish trust in the health personnel and patient satisfaction with the technique. Also, such coercive dynamics are against medical ethics and violate the principles of reproductive rights, emphasizing that health professionals should respect a woman’s bodily autonomy and decision-making.
Conclusion
We conclude that PPIUCD is well accepted by the women as a practical family planning method provided it is offered as an informed choice, followed up for the complications, and supported through adequate counseling. Our study highlights various modifiable and non-modifiable patient-related factors that affect acceptance and facilitates long-term retention. These factors should be discussed during the counseling sessions in the ante-natal periods. The spouse’s involvement is equally crucial to reap this highly effective contraceptive’s long-term benefits. Being a tertiary care center, we observed better retention rates that reiterate our emphasis on enhancing the skills of health care personnel through training, elaborate antenatal counseling, and public awareness campaigns to increase the acceptance of PPIUCD. Retention rates increase when women are adequately enquired about the side effects of PPIUCD in the post-partum period, which can be done during home-based post-natal care visits. At the same time, it is also essential to understand that to meet our targets; health workers should prevent engaging in inadvertent coercion, which may hamper the reproductive rights of the women, and dilutes the whole idea of empowering our women for a better future.
Data Availability
The datasets for the current study are available from the corresponding author upon reasonable request.
Abbreviations
- IUCD:
-
Intra-Uterine Contraceptive Device
- PPIUCD:
-
Post-Partum Intrauterine Contraceptive Device
- ANC:
-
antenatal care
- PROM:
-
Premature Rupture of Membranes
- HIV:
-
Human Immunodeficiency Virus
- WHO:
-
World Health Organization
- SES:
-
Socio-Economic Status
References
International Institute for Population Sciences. India-Key Indicators. National Family Health Survey (NFHS-4) 2015-16- India. 2017. https://www.rchiips.org/nfhs. http://www.iipsindia.org Accessed 10 Jul 2021.
Gbagbo FY, Kayi EA. Use and discontinuation of intrauterine contraceptive device in the Greater Accra Region of Ghana. Contracept Reprod Med. 2018;3:8.
Mahande MJ, Obure J. Effect of interpregnancy interval on adverse pregnancy outcomes in northern Tanzania: a registry-based retrospective cohort study. BMC Pregnancy Childbirth. 2016;16:1–9.
Nonyane BAS, Norton M, Begum N, Shah RM, Mitra DK, Darmstadt GL, et al. Pregnancy intervals after stillbirth, neonatal death and spontaneous abortion and the risk of an adverse outcome in the next pregnancy in rural Bangladesh. BMC Pregnancy Childbirth. 2019;19:62.
Kaneshiro B, Aeby T. Long-term safety, efficacy, and patient acceptability of the intrauterine copper T-380A contraceptive device. Int J Womens Health. 2010;2:211.
Iftikhar PM, Shaheen N, Arora E. Efficacy and Satisfaction Rate in Postpartum Intrauterine Contraceptive Device Insertion: A Prospective Study.Cureus. 2019;:e5646.
Hooda R, Mann S, Nanda S, Gupta A, More H, Bhutani J. Immediate Postpartum Intrauterine Contraceptive device insertions in caesarean and vaginal deliveries: a comparative study of Follow-Up outcomes. Int J Reprod Med. 2016;2016:1–5.
Mishra S. Evaluation of Safety, Efficacy, and expulsion of post-placental and intra-cesarean insertion of Intrauterine Contraceptive Devices (PPIUCD). J Obstet Gynecol India. 2014;64:337–43.
Yadav V, Balasubramaniam S, Das S, Srivastava A, Kumar S, Sood B. Comparison of outcomes at 6 weeks following postpartum intrauterine contraceptive device insertions by doctors and nurses in India: a case-control study. Contraception. 2016;93:347–55.
Vidyarama R, Nagamani T, Prasad U. PPIUCD as a long acting reversible contraceptive (LARC) – an experience at a tertiary care centre. Interantional J Sci Res. 2015;4:3–5.
Agarwal N, Gupta M, Agrawal A, Sharma A. Efficacy and safety of Post-Partum Intrauterine Contraceptive device (PPIUCD) insertion-A prospective study. Santosh Univ J Heal Sci. 2017;3:20–3.
2013; Family Planning Division; Ministry of Health and Family Welfare Government of India. IUCD Reference Manual for Medical Officers and Nursing Personnel, September. http://nhm.gov.in/images/pdf/programmes/family-planing/guidelines/IUCD_Reference_Manual_for_MOs_and_Nursing_Personne_-Final-Sept_2013.pdf. Accessed 6 Jul 2022.
Deshpande S, Gadappa S, Yelikar K, Wanjare N, Andurkar S, Professor A, et al. Awareness, acceptability and clinical outcome of post-placental insertion of intrauterine contraceptive device in Marathwada region, India. Indian J Obstet Gynecol Res. 2017;4:77–82.
Sood B, Asif R, Charurat E, Das S, Kumar S, McKaig C, et al. Revitalization of postpartum IUCD (PPIUCD) services: experience from India. Contraception. 2012;86:184–5.
Gautam R, Arya KN, Kharakwal S, Singh S, Trivedi M. Overview of immediate PPIUCD application in Bundelkhand region. J Evol Med Dent Sci. 2014;3:9518–26.
Kanhere A, Pateriya P, Jain M. Acceptability and feasibility of Immediate post-partum IUCD insertion in a tertiary care centre in Central India. Int J Reprod Contraception Obstet Gynecol. 2015;4:1.
Pandher DK, Rani S, Goel P. Two years follow up study of post placental insertion of IUCD during caesarean sections: safety, efficacy and complications. Int J Reprod Contraception Obstet Gynecol. 2018;7:981.
Patel J, Vyas R, Parikh P. Evaluation of PPIUCD insertion as a method of Contraception in India. J Dent Med Sci. 2017;16:49–53.
Mule VD, Rokade JV. Study the efficacy and compliance of postpartum intrauterine device. Int J Gynaecol. 2017;3:91–5.
Garuda L, Kambham S, Neelohita B. Clinical outcome of Ppiucd (Copper-380A)-Intracaesarean insertion. Indian J Obstet Gynecol Res. 2015;2:218.
Kanakuze CA, Kaye DK, Musabirema P, Nkubito P, Mbalinda SN. Factors associated with the uptake of immediate postpartum intrauterine contraceptive devices (PPIUCD) in Rwanda: a mixed methods study. BMC Pregnancy Childbirth. 2020;20:1–11.
Dixit A, Averbach S, Yore J, Kully G, Ghule M, Battala M et al. A gender synchronized family planning intervention for married couples in rural India: Study protocol for the CHARM2 cluster randomized controlled trial evaluation.Reprod Health. 2019;16.
El-Khoury M, Thornton R, Chatterji M, Kamhawi S, Sloane P, Halassa M. Counseling women and couples on Family Planning: a randomized study in Jordan. Stud Fam Plann. 2016;47:222–38.
Gonie A, Worku C, Assefa T, Bogale D, Girma A. Acceptability and factors associated with post-partum IUCD use among women who gave birth at bale zone health facilities, Southeast-Ethiopia. Contracept Reprod Med 2018 31. 2018;3:1–8.
Kumar S, Sethi R, Balasubramaniam S, Charurat E, Lalchandani K, Semba R, et al. Women’s experience with postpartum intrauterine contraceptive device use in India. Reprod Health. 2014;11:32.
Kant S, Archana S, Singh AK, Ahamed F, Haldar P. Acceptance rate, probability of follow-up, and expulsion of postpartum intrauterine contraceptive device offered at two primary health centers, North India. J Fam Med Prim care. 2016;5:770–6.
Çelen Ş, Sucak A, Yildiz Y, Danişman N. Immediate postplacental insertion of an intrauterine contraceptive device during cesarean section. Contraception. 2011;84:240–3.
Lopez LM, Bernholc A, Hubacher D, Stuart G, Van Vliet HA. Immediate postpartum insertion of intrauterine device for contraception.Cochrane Database of Systematic Reviews. 2015;2015.
Kapp N, Curtis KM. Intrauterine device insertion during the postpartum period: a systematic review. Contraception. 2009;80:327–36.
World Health Organization. Family Planning Counselling. Counselling for Maternal and Newborn Health Care: A Handbook for Building Skills. 2013;:233. https://www.ncbi.nlm.nih.gov/books/NBK304183/. Accessed 7 Jul 2021.
Gebremedhin M, Alemayehu A, Yihune M, Dessu S, Melis T, Nurahmed N. Acceptability and factors Associated with Immediate Postpartum Intrauterine Contraceptive device use among women who gave birth at Government Hospitals of Gamo Zone, Southern Ethiopia, 2019. Open access J Contracept. 2021;12:93–101.
Gonie A, Worku C, Assefa T, Bogale D, Girma A. Acceptability and factors associated with post-partum IUCD use among women who gave birth at bale zone health facilities, Southeast-Ethiopia. Contracept Reprod Med. 2018;3:16.
Mohamed SA, Kamel MA, Shaaban OM, Salem HT. Acceptability for the use of postpartum intrauterine contraceptive devices: assiut experience. Med Princ Pract. 2003;12:170–5.
Nigam A, Ahmad A, Sharma A, Saith P, Batra S. Postpartum Intrauterine device refusal in Delhi: reasons analyzed. J Obstet Gynaecol India. 2018;68:208.
Gupta V, Kumari N, Goswami D, Maheshwari P. A rare case of Perforation following PPIUCD insertion. J Obstet Gynecol India. 2016;66:292–4.
Ranjana., Verma A, Chawla I. A follow up study of postpartum intrauterine device insertion in a tertiary health care centre. Int J Reprod Contraception Obstet Gynecol. 2017;6:2800.
Singal S, Bharti R, Dewan R, Divya, Dabral A, Batra A, et al. Clinical outcome of postplacental copper T 380A insertion in women delivering by caesarean section. J Clin Diagnostic Res. 2014;8:OC01–4.
Xess S, Sharma M, Rajoria L, Mehta S. A study to evaluate and compare the expulsion, removal and continuation of post placental insertion of Cu 375 and CuT 380A in indian women. Int J Clin Obstet Gynaecol. 2018;2:33–8.
Doley R, Pegu B. A retrospective study on acceptability and complications of PPIUCD insertion. J Evol Med Dent Sci. 2016;5:1631–4.
Nayak AK, Jain MK. Experience on Awareness, Acceptability, Safety, Efficacy, Complications and Expulsion of Post-partum Intrauterine Contraceptive Device Insertion.Int J Sci Study. 2017;:207.
Mishra S. Evaluation of Safety, Efficacy, and expulsion of post-placental and intra-cesarean insertion of Intrauterine Contraceptive Devices (PPIUCD). J Obstet Gynaecol India. 2014;64:337–43.
Mishra S. Tale of the tails, the Missing Postpartum IUCD Strings. J Obstet Gynaecol India. 2017;67:202–7.
Kant S, Archana S, Singh AK, Ahamed F, Haldar P. Acceptance rate, probability of follow-up, and expulsion of postpartum intrauterine contraceptive device offered at two primary health centers, North India. J Fam Med Prim Care. 2016;5:770.
Katheit G, Agarwal J. Evaluation of post-placental intrauterine device (PPIUCD) in terms of awareness, acceptance, and expulsion in a tertiary care centre. Int J Reprod Contraception Obstet Gynecol. 2013;2:539.
Khurshid N, Taing S, Qureshi A, Insha ·, Khanyari J. Post-placental intrauterine device insertion Versus delayed Intrauterine device insertion: an observational study. J Obstet Gynecol India. 2020;70:145–51.
University of California San Francisco. Provider support for IUDs can lead to coercive practices. Advancing New Standards in Reproductive Health. 2020. https://www.ansirh.org/research/research/provider-support-iuds-can-lead-coercive-practices. Accessed 6 Jul 2022.
Acknowledgements
Not applicable.
Funding
There was no funding to conduct this research.
Author information
Authors and Affiliations
Contributions
SG, RB, and PG conducted all the data analyses and drafted the manuscript. HKS, PS guided the literature review and helped draft the manuscript. SG conducted data management. PG suggested the literature review, analysis, and drafting of the manuscript. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethical approval
was obtained from the research review committee of Adesh Institute of Medical Sciences and Research, Bathinda, Punjab, India (AU/EC/FM/133/ 2018). Written informed consent was obtained from each study participant. Confidentiality of the information was ensured to all participants throughout the study process, and the data was made anonymous for analysis. Withdrawal from the study at any point was assured to all the participants.
Consent for publication
Not applicable.
Conflict of interest
There are no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gupta, S., Bansal, R., Shergill, H.K. et al. Correlates of post-partum intra-uterine copper-T devices (PPIUCD) acceptance and retention: an observational study from North India. Contracept Reprod Med 8, 25 (2023). https://doi.org/10.1186/s40834-023-00222-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40834-023-00222-2