Abstract
Background
Literature is satiated with studies focusing on knowledge, attitude, and practices of family planning (FP) among the female population, conversely, the gaps in sex-disaggregated data on FP continue to exist. This study sought to report sex differences existing in FP knowledge, attitude, and use in Uganda.
Methods
This study uses data from a household survey that covered 16 districts in Uganda. Multi-stage cluster randomized sampling was employed for participant selection. Bivariate analysis for categorical data was conducted. Multilevel logistic regression model was applied to model the effects of socio-demographic characteristics on the use of modern FP methods.
Results
Data from 4,352 respondents in the ratios of 70 % females and 30 % of males were analyzed. The mean age was 28.7 SD (8.5) and was not significantly different between males and females. More male respondents had secondary or higher level of education (44 %) than females (36 %). Knowledge of at least one modern FP method was high, but small significant differences were revealed between males (96 %) and females (98 %). Significant knowledge differences were seen in specific FP methods. A higher proportion of females (71 %) than males (67 %) perceived modern FP methods as always available in the community whereas more males (40 %) believed that modern FP methods can result in infertility than females (35 %). There was high self-efficacy about family planning methods use in both males and females. The proportion of married females that reported using or their partner using a modern FP method was 39 % compared to 45 % reported by the married males. Approx. 53 % of the males compared to 37 % of the females that reported condom use also cited STI/HIV prevention as the main reason for condom use suggesting dual protection as a driver for use. Males, young adults, the more educated, and those in marriage or active relationships were more likely to use modern FP methods.
Conclusions
Our study found significant sex differences in knowledge, attitudes, and use of FP methods. The young adults and more educated respondents were more likely to use FP methods. The high self-efficacy observed for both males and females is a signal that both sexes can use FP methods. Project strategies and implementation should take into consideration the existing differences by sex and devise sex-tailored approaches to improve FP knowledge, attitudes, and use in this population. There was increased reporting of condom use as an FP and STI/HIV prevention method, follow-up studies aiming at succinctly measuring dual protection, and its drivers for both sex should be done.
Similar content being viewed by others
Background
Use of family planning (FP) methods by women and men can improve the health, economic, and social domains of their lives [1]. As such, FP continues to be a key focus of the global agenda for improving maternal, sexual and reproductive health. According to the Uganda Demographic and Health Survey (UDHS) report 2016, some knowledge of FP methods is nearly universal in Uganda, with 99 % of both women and men having heard of at least one method of FP [2]. However, the use of modern FP and any form of FP among married women in Uganda stood at only 35 and 39 % respectively. FP methods use among sexually active unmarried women was slightly higher with 51 % using any FP method and 47 % using a modern method, and the total unmet need for FP among the sexually active women of reproductive age stood at 28 % among currently married women, and 32 % among the sexually active unmarried women.
In the FP Costed Implementation Plan 2015–2020 [3], the Uganda Ministry of Health (MoH) acknowledged that several innovative FP service delivery models have been successfully implemented by Non-Governmental Organizations (NGOs) in Uganda in an effort to remove access barriers for FP. For instance, community-based distribution of certain FP commodities has been successful at expanding access, and task shifting of injectable FP to Village Health Teams (VHTs)/Community Health Workers (CHWs). Over the past 2 decades, government-supported VHTs have provided a broad service package including family planning. However, key challenges still exist, limiting the effectiveness of the community health program; CHWs not adequately equipped with commodities and skills to deliver FP, absence of supervision, no compensation, and suboptimal use of reporting and decision support tools. In 2018, Living Goods, an international organisation piloted the implementation of comprehensive CHW led FP services model while addressing these gaps in the two districts of Wakiso and Mpigi in Uganda. The FP services provided to the clients mainly comprised of counseling, and provision of condoms, DMPA-SC (commonly known by the brand Sayana Press® or simply Sayana) and oral FP and as well as referral for long-term methods. The pilot program results suggested that by working through CHWs, it is possible to address the binding constraints to the uptake and utilization of FP including social opposition, misinformation and fear of side effects, among others[4].
Men’s knowledge, attitudes, and behaviors around FP impact uptake and unmet need because men are not only women’s partners, but individuals with distinct reproductive histories and desires of their own. A 2020 Tanzania study [5] found that knowledge of modern contraception was a crucial factor in influencing the use of modern FP among men and suggested that targeting of men with FP awareness programs would improve the use of FP among men. The UDHS 2016 findings [2] showed that 12 % of married women were refused to use FP by their partners while 44 % made the decision jointly with their husbands. The literature on the role and attitude of men in decision-making is mixed. A study in Uganda revealed that men were greatly interested in modern contraception, albeit they possessed little knowledge about it [6] while a related study in Tanzania showed that men expressed little interest in the use of modern FP methods, and yet were considered by women as key decision-makers in their use of FP[7]. Another study conducted in Uganda using nationally representative data revealed that the use of FP was significantly higher among men that had discussions with a health worker, desired for few children, belonged to a higher wealth index, and highly educated [8], and these factors are similar to factors that affect FP among women. Male inclusion in FP has been encouraged by various international and national initiatives including providing incentives for men who escort their partners for FP. However, gaps in data continue as FP data in programs and reports is rarely disaggregated by sex if men are included at all [9]. Where data on utilization of modern contraception were reported among men, FP methods use was found to be high[5].
Whereas there is paucity of literature on men’s statistics, collection, analysis, and reporting of sex-disaggregated data are critical to fully understand the specific needs of men and women. This study sought to explore sex variations existing in the knowledge, attitudes, and use of FP services in selected districts of Uganda.
Methods
Study design
This was a cross-sectional survey, conducted as a baseline to a larger research project. The paper focuses on the results from the quantitative household survey. Data collection was conducted in August 2019.
The study setting
Data collection was undertaken in sixteen (xvi) districts of Uganda. The study did not seek to be nationally representative as the selection of study districts took into consideration Living Goods Uganda’s current catchment area for the FP intervention. Figure 1 shows a map of Uganda with survey districts marked “Yes” with a pink color.
Study population
Participants in the household (HH) baseline survey comprised of women and men in the reproductive age of 15 to 49 years.
Sample size
The Cochran (1963) formula for two independent samples with a dichotomous outcome was used to determine the sample size (n). To achieve a maximum sample size, a proportion of 0.5 per sample group was used. A sample of 4,380 respondents was derived with a statistical power of 90 %, a precision level of 5 %, a design effect is 1.5, and a 95 % confidence level. The sample was distributed equally among sampled districts and villages.
Household sample selection
The selection of the households for the survey utilized a four-stage sampling approach. The first stage involved a purposive selection of districts for the survey and the second stage involved a random selection of sub-counties per district (2 to 6 sub-counties per district). The third stage involved the random selection of four villages within each sub-county using the computer-based Random Draw Method. The fourth and last stage involved systematic random sampling of households to be interviewed. To ensure all eligible households had an equal chance of participating in the survey, the survey team worked with local leaders to conduct a household listing of households with persons in the age range of 15–49 years (male and female). The desired ratio of 3 females to 1 male was used. The sample size was not adjusted for non-response and consequently, the household replacement was assumed to be feasible where a HH refused to participate or was not available at the time of interview. For the latter non-response, the replacement was done after making three [3] call-backs to the household. For each HH selected, only one person was needed for an interview. Therefore, simple random sampling using the raffle/lottery method without replacement was used to select a respondent from all eligible members of the desired sex in the household. The sex of the respondent was predetermined before arriving at the household.
Data collection methods
The quantitative household survey data collection was done through face-to-face interviews using a structured questionnaire. The questionnaire was programmed using the Open Data Kit (ODK) software and uploaded on electronic devices (smartphones).
Quality assurance
Before the study was started, a data quality assurance protocol was developed and this included constituting a strong and dynamic team with experience in conducting similar assignments, recruiting and training experienced research assistants and field supervisors to handle data collection. The ODK data collection tool was also designed with controls to limit data entry errors. Field supervisors did spot checks on 5 % of the respondents to validate the information collected by the interviewers and feedback was analyzed to improve the process. Also, the research team organized routine internal meetings to review progress on the data collection against set targets per district per cluster.
Data analysis
Descriptive analysis using proportions was conducted to show the distribution of FP knowledge, attitudes, and use of FP. Bivariate analysis using Pearson’s Chi-square and Fisher’s exact tests for categorical data was done. Additionally, a multilevel logistic regression model [10] was used to model the effects of socio-demographic characteristics on the use of family planning methods. The sex of the respondent was included in the model as a fixed factor to model sex differences. To model the associations of respondents within the different districts, sub-counties, and villages, the study considered a four-level analysis model with three high-level cluster variables (random effects equations) i.e. district, sub-county, and village treated as random effects factors to account for within-cluster correlations (intra-cluster correlation). This assumes that observations nested in a cluster share common characteristics in terms of access to community services and this may affect the use of family planning methods. All quantitative analysis was done in STATA version 15 software and statistical significance was considered at 5 %.
Ethical considerations
The study received ethical clearance from Mildmay Uganda Research and Ethics Committee (MUREC) and Uganda National Council for Science and Technology (UNCST). All members of the survey team were trained on the protection of human subjects. In the field, all members of the survey team obtained written informed consent, upheld the principles of voluntary participation, confidentiality, anonymity, and respect of the privacy of respondents, and the obligation to not do any harm. Identifiers such as names of respondents were not tagged on an interview recorded on the smartphones further improving the privacy and confidentiality of survey data.
Results
The quantitative study achieved an overall response rate of 99 % (100 % for women and 99 % for men) by reaching 4,352 respondents out of the targeted 4,380 respondents. The study managed to achieve the ratios of 70 % female and 30 % male representation in the quantitative survey. All 4,352 respondents had complete data on socio-demographic characteristics and main outcomes hence no missing data handling approaches were used.
Socio-demographic characteristics of respondents
Table 1 shows the distribution of the socio-demographic characteristics of the study participants disaggregated by sex. The distribution of respondents differed by sex on the following variables; age group, education level, marital status, the main source of income, and the number of children. Although there were observed significant differences in age groups for males and females starting at the age of 30, the overall mean age of respondents was 28.7 SD (8.5) and was not significantly different between males and females. Overall 39 % of the respondents had not achieved at least a primary leaving certificate with a higher proportion of females (41 %) than males (35 %). Approximately one-quarter of respondents were not married, with the percentage unmarried was higher among males (44 %) than females (21 %). A significantly lower percentage of females (16 %) than males (38 %) reported having no children.
Knowledge of FP methods
Table 2 shows the results of the respondent’s knowledge of FP methods. Both sexually active and inactive respondents were included in the analysis. The findings revealed that overall 97 % of the respondents had heard of at least one modern FP method and there was a small, but significant difference between males (96 %) and females (98 %). There were also significant differences in knowledge of specific FP methods by sex. Women were most likely to know injectables, pills, implants, and IUDs. Male knowledge was highest for male condoms, followed by the same three methods as for females. Overall, the study observed higher levels of knowledge in hormonal birth control FP methods (implant, IUD, Injectable, Pills) than the natural methods (Lactational Amenorrhea, Withdrawal, Periodic abstinence) and permanent methods (female and male sterilization). Knowledge of male condoms was higher for both males and females than the female condoms.
Use of contraception methods
Use of contraception was assessed by looking at the proportion of sexually active respondents that were not currently pregnant that reported using the different FP methods (84 % of the total respondents). Table 3 shows the proportion of respondents that reported the use of FP methods. The use of modern FP stood at 38.7 % overall and this was significantly higher among the males (45 %) than the females (36 %). The main methods of FP reported by females were Depo (37 %), withdrawal (22 %), and male condoms (9 %) compared to male condoms (46 %), Depo (19 %), and withdrawal (12 %) reported by males. Overall the use of the permanent FP methods was higher (6 %) than long-term methods (3 %). For permanent use, there were significant differences between males and females, but, no significant sex differences were observed among the long-term methods.
Figure 2 shows the use of modern FP methods among women by marital status and sex. The findings indicated that the proportion of married/cohabiting females that reported using or their partner using a modern FP was 39 % lower than 45 % reported by the male counterparts. Modern FP use was highest for both males and females that were in a relationship but married/ cohabiting and lowest for both males and females that were single or separated.
Condom use as a dual protection method
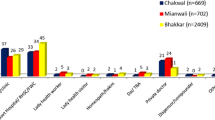
Figure 3 shows that half of the males and a third of the female respondents that reported condom use as the current method of FP used it as a prevention measure of STI/HIV infection. The study did not establish whether the primary objective was STI/HIV protection or protection against pregnancy or both, and this is a limitation to accurately measure the differentiated effect of condom use on the results reported among males.
Respondent perceptions, beliefs, and self-efficacy about FP services
Table 4 shows the respondent’s perceptions on the availability, affordability, self-efficacy, and beliefs about the FP methods disaggregated by sex. The results in this section were restricted to men (92 %) and women (96 %) respondents that were in-union or sexually active singles. The results are explained in the following sub-sections.
Perceived availability of FP services
Overall, more than half of the respondents (69.9 %) perceived modern FP as always available in the community whenever they were needed, and this was significantly higher among the females (71.1 %) than the males (66.7 %).
Perceived affordability of FP Services
The results in Table 4 further suggest that over half of the respondents (53 %) perceived modern FP methods to be affordable within their communities. There were no significant sex differences.
Perceived quality of FP services
The study results also revealed that overall almost three-quarters (73 %) of the respondents perceived public health facilities to be providing high-quality FP services, and this was significantly higher among the females (75.0 %) than males (68.5 %).
Beliefs about FP services
Beliefs about FP were assessed by exploring the respondent’s perceptions about the side-effects of FP considering; beliefs about modern FP and infertility, cancer, and the effects of FP use on sexual pleasure. Table 4 shows that more males (40 %) significantly perceived modern FP to result in infertility than females (35 %). For specific methods, overall 42 % of the respondents believed that the use of IUDs can result in cancer, and no significant sex differences were revealed. Overall, also, 11 % of the respondents believed that using Sayana Press reduces sexual pleasure, and this was lower among males (8.6 %) than females (12.5 %).
Perceived role of CHWs in FP service delivery
The study sought to establish the sex-disaggregated perception of the involvement of CHWs in FP services provision in communities. The results are presented in Fig. 4. Overall, there was perceived low involvement and quality of CHWs in FP services. Approximately only 3 in 10 of the respondents agreed that CHWs were available in the community to offer FP services and agreed that FP services provided were of high quality. There were no significant sex differences observed.
Decision-making regarding FP use
Decision-making regarding FP use is a critical factor in the adoption of FP services. The results presented in Fig. 5 suggested that a larger proportion of females (53 %) decided for the couple to take on FP than 33 % reported by males. More males reported that the decision for the couple to use FP was joint compared to females. Even though half of the women reported deciding to use FP themselves, majority of them indicated that their partners were aware of the FP use.
Effect of socio-demographic characteristics on modern FP use
Table 5 shows findings from the adjusted multilevel logistic regression to assess the effect of socio-demographic characteristics on modern FP use. The findings indicated that females were 35 % less likely to use FP compared to males (Adjusted odds ratio (AOR) = 0.65, P = 0.000). Respondents aged 40–44 and 45–49 were 36 and 69 % less likely to use modern FP compared to those aged 15–19. No significant differences were observed for other age groups in comparison to the 15–19 age group. For education level, those that completed primary were 43 % more likely to use modern FP (AOR = 1.43, P = 0.041) compared to those with no education while those that achieved secondary or higher were 45 % more likely to use modern FP compared to those with no education (AOR = 1.45, P = 0.030). After adjusting for sex and other socio-demographic characteristics, those in a relationship were approximately two times (AOR = 2.48, P = 0.000) more likely to use FP compared to those in no/ single relationships. The married respondents were also 88 % more likely to use modern FP compared to those in no relationship. No significant differences were revealed for religion, place of residence, source of income, and the number of children.
Discussion
Literature is replete with studies focusing on knowledge, attitude, and use of FP services among the female population, conversely, the disaggregation of results by males and females has been less of a focus and not emphasized in reporting [9]. This paper’s findings add to a growing body of literature on sex-disaggregated FP knowledge and use. The results from the study revealed significant sex differences in the knowledge, attitudes, and use of FP services in selected districts in Uganda.
The finding that knowledge of FP was equally high for both males and females, despite the small differences is an indication that males and females have been equally targeted and engaged with information on FP in Uganda. It is not surprising that men were more aware of condoms as an FP method than any other method while women were more aware of the longer-term FP methods. It may be argued that whereas men may be more focused on the dual protection they can get from condoms, women are usually more concerned about the prevention of unplanned pregnancy and this explains why men may be more informed more about condom use. These findings contradict those found in Mwanza region Tanzania [7], Mpigi district Uganda[6], Mbeya region Tanzania [11], and Nigeria [12] which all found that men had little knowledge on the subject.
Whereas females had more knowledge on FP and its availability within their communities, their attitudes, and fears about the possible side effects were significantly different from those of males. The study found out that more males were worried that modern FP methods can result in infertility while females were on the other hand more concerned about reduced sexual pleasure or their partners being angry if they found out. Whenever such fears exist, it becomes difficult for people to embrace FP methods. The mismatch in fears between men and women related to FP may also affect couples’ communication on FP matters and result in lower uptake of FP and or discontinuation. The negative effect of fear of side effects on FP uptake has been reported by previous research studies [6, 7, 13,14,15,16].
Findings revealed that half of the males that reported condom use as the current FP method also cited STIs/HIV prevention as the reason for its use. This finding revealed that most of the males preferred condom use dual protection compared to a third of the females resulting in a potential overestimation of reported FP use among males. Whereas almost half of the males in this study commonly reported condoms as their FP method of use, other studies have associated condom use with HIV prevention and protection efforts [17] or casual sexual relationships rather than as an FP method [18]. Future research should establish the primary use of condoms whenever they are reported as the FP method to avoid overstating its use as an FP method. The findings further suggested that the use of short-term modern FP methods accounted for more than three-quarters of the total modern FP methods in this study and recent studies associated short-term methods use with high odds of discontinuation and switching affecting uptake and retention of clients on FP [2, 16]. Our study findings from the regression model suggested that males, the young adults, the highly educated, and those in marriage or active relationship were more likely to use modern FP services. These findings are consistent with other research studies that reported high FP among the educated [8], and the married [19]. Contrary to the recent studies [8, 20] our study finding revealed no significant variations in uptake of modern FP among respondents with no child and those with an increasing number of children.
Results from a recent randomized controlled trial study found that where CHWs were active in the provision of low-cost health products and basic child health services to low-income families, there were improved health outcomes among the community members like reduced morbidity and mortality [21]. Our study findings revealed low involvement of CHWs in the delivery of family planning services. Learning from findings on the RCT study [21], we think that there is a potential opportunity for research on how CHWs can be leveraged to provide FP services and follow-up of clients. The Living model that addresses some of the bottlenecks to effective CHW services delivery like inadequate tools, lack of supervision, and compensation is a learning opportunity on how CHWs can be supported to drive impact in the community in the sexual and reproductive health services domain.
Our findings are not indicative of the national picture and should not be decisively used to generalize the entire country’s situation since they are largely biased to a few selected districts where Living Goods Uganda has a presence. Albeit, the findings provide important sex-disaggregated insights into the knowledge, attitudes, beliefs, and use of FP and are thus important for improving the programming of future FP interventions. The results showed that females had a higher positive attitude and beliefs on availability, affordability, and beliefs of FP methods than males. Overall both males reported high self-efficacy and this can be leveraged to promote use of FP methods. The study couldn’t succinctly establish the reasons for condom use or the differentiated effect of condom use on modern contraception as a dual protection method for STIs/HIV and pregnancy. Follow-up studies will aim to measure this accurately. Given that this study was conducted as part of a baseline to an FP project, project strategies and implementation will take into consideration the existing differences by sex as documented in this paper and devise sex-tailored approaches to improve FP knowledge, attitudes, and use in this population.
Conclusions
Our study found out that knowledge of at least one modern FP method was high, but small significant differences were revealed between males (96 %) and females (98 %). Large differences were however observed in FP-specific methods. There was high self-efficacy about family planning methods use in both males and females. Significantly, more males (40 %) believed that modern FP methods can result in infertility compared to females (35 %). A significantly lower proportion of married females reported using or their partner using a modern FP method (39 %) compared to 45 % reported by the married males. The young adults and more educated respondents were more likely to use FP methods. Project strategies and implementation should take into consideration the observed sex differences in attitudes, beliefs, and knowledge and devise sex-tailored approaches to improve FP uptake. There was increased reporting of condom use as an FP and STI/HIV prevention method, follow-up studies aiming at succinctly measuring dual protection, and its drivers in both males and females should be done.
Availability of data and materials
Data and study tools are available upon request from the corresponding author.
Abbreviations
- AOR:
-
Adjusted Odds Ratio
- CHW(s):
-
Community Health Worker(s)
- CI:
-
Confidence Interval
- FGDs:
-
Focus Group Discussion
- FP:
-
Family Planning
- HH:
-
Household
- IUDs:
-
Intra-Uterine Device
- LG :
-
Living Goods
- MCH:
-
Maternal and Child Health
- MOH:
-
Ministry of Health
- MUREC:
-
Mildmay Uganda Research and Ethics Committee
- ODK:
-
Open Data Kit
- UBOS:
-
Uganda Bureau of Statistics
- UDHS:
-
Uganda Demographic and Health Survey
- UNCST:
-
Uganda National Council for Science and Technology
References
Guttmacher Institute BMGF. ADDING IT UP: Investing in Contraception and Maternal and Newborn Health. Guttmacher Inst [Internet]. 2017;(June):1–4. Available from: http://www.gatesfoundation.org/What-We-Do/Global-Development/Family-Planning%0Ahttps://www.guttmacher.org/fact-sheet/adding-it-up-contraception-mnh-2017.
Uganda Bureau of Statistics and ICF. Uganda Demographic and Health Survey 2016 [Internet]. Kampala; 2018. Available from: https://dhsprogram.com/pubs/pdf/FR333/FR333.pdf.
Uganda Family Planning. Costed Implementation Plan, 2015–2020. Uganda: Kampala; 2014.
Allan E, Frank N, Phionah K. DIGITAL HEALTH PILOT. PROJECT IN UGANDA EXTENDS THE REACH OF FAMILY PLANNING CARE IN THE COMMUNITY [Internet]. 2021. Available from: https://knowledgesuccess.org/2021/01/15/digital-health-pilot-project-in-uganda-extends-the-reach-of-family-planning-care-in-the-community/.
Msovela J, Kessy AT, Rumisha SF, Simba DO, Urassa DP. Male partner approval on the use of modern contraceptive methods : factors determining usage among couples in Kibaha district, Tanzania. 2020;8:1–7. Available from: https://contraceptionmedicine.biomedcentral.com/articles/https://doi.org/10.1186/s40834-020-00107-8.
Kaida A, Kipp W, Hessel P, Konde-Lule J. Male participation in family planning: Results from a qualitative study in Mpigi District, Uganda. J Biosoc Sci. 2005;37(3):269–86.
Mosha I, Ruben R, Kakoko D. Family planning decisions, perceptions and gender dynamics among couples in Mwanza, Tanzania: A qualitative study. BMC Public Health [Internet]. 2013;13(1):1. Available from: BMC Public Health.
Kabagenyi A, Ndugga P, Wandera SO, Kwagala B. Modern contraceptive use among sexually active men in Uganda: does discussion with a health worker matter?. BMC Public Health. 2014;14(1):1-8.
The importance of gender in family planning and reproductive health data [Internet]. 2017. Available from: https://www.measureevaluation.org/resources/publications/fs-17-205b/at_download/document.
Khan M, Shaw J. Multilevel Logistic Regression Analysis Applied to Binary Contraceptive Prevalence Data. J Data Sci 2011;9(No.1):93–110.
Mwageni EA, Ankomah A, Powell RA. Attitudes of men towards family planning in Mbeya region, Tanzania: A rural-urban comparison of qualitative data. J Biosoc Sci. 1998;30(3):381–92.
Blanc AK. The Effect of Power in Sexual Relationships on Sexual and Reproductive Health: An Examination of the Evidence. Stud Fam Plann. 2003;32(3):3–4.
Campbell M, Potts M. Barriers to Fertility Regulation: A Review of the Literature. Stud Fam Plann [Internet]. 2006;37(2). Available from: https://doi.org/10.1111/j.1728-4465.2006.00088.x.
Castle S. Factors Infuencing Young Malians’ Reluctance to Use Hormonal Contraceptives. Stud Fam Plann [Internet]. 2004;34(3). Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1728-4465.2003.00186.x.
Hall MAK, Stephenson RB, Juvekar S. Social and logistical barriers to the use of reversible contraception among women in a rural Indian Village. J Heal Popul Nutr. 2008;26(2):241–50.
Nuwasiima A, Nuwamanya E, Babigumira JU, Nalwanga R, Asiimwe FT, Babigumira JB. Acceptability and utilization of family planning benefits cards by youth in slums in Kampala, Uganda. 2019;2:1–11. Available from: https://rdcu.be/bXQnM.
Green EC, Halperin DT, Nantulya V, Hogle JA. Uganda’s HIV prevention success: The role of sexual behavior change and the national response. AIDS Behav. 2006;10(4):335–46.
Pranitha M, John C. Risk Perception and Condom Use Among Married Or Cohabiting Couples in KwaZulu-Natal, South Africa. Int Fam Plan Perspect. 2005;31(1):24–9.
Asiimwe JB, Ndugga P, Mushomi J, Menyenye Ntozi JP. Factors associated with modern contraceptive use among young and older women in Uganda; a comparative analysis. BMC Public Health. 2014;Sep 8(14):926.
D. W AM, F A, B. M. Determinants of modern contraceptive utilization among married women of reproductive age group in North Shoa Zone, Amhara Region, Ethiopia. Reprod Health [Internet]. 2014;11(1):1–7. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed12&NEWS=N&AN=2014111648.
Nyqvist MB, Guariso A, Svensson J, Yanagizawa-Drott D. Reducing child mortality in the last mile: Experimental evidence on community health promoters in Uganda. Am Econ J Appl Econ. 2019;11(3):155–92.
Acknowledgements
The authors for this study would like to acknowledge the Socio-Economic Data Centre Ltd Uganda consultants led by Professor Narathius Asingwire that designed the evaluation protocol, acquired ethical clearance and conducted data collection from which this study draws the data. The consultants however have no role in the manuscript writing for this paper.
Funding
The funding for the evaluation was drawn from the large project funding that was received from the John Templeton Foundation, Grant ID 61137. The funders had no role in the conceptualization and writing of this manuscript.
Author information
Authors and Affiliations
Contributions
AW and AN conceived the study. AN conducted the data analysis. AW and AN wrote the first draft. AE, PK, JL reviewed the draft manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received institutional ethics review approval from a recognized local review board. All study participants provided informed consent before participation on the study.
Consent for publication
Not Applicable.
Competing interest
There are no competing interests to report.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nuwasiima, A., Watsemba, A., Eyapu, A. et al. Sex differences in family planning knowledge, attitudes, and use in Uganda. Contracept Reprod Med 6, 23 (2021). https://doi.org/10.1186/s40834-021-00166-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40834-021-00166-5