Abstract
Silicone breast implants are commonly used for cosmetic and oncologic surgical indications owing to their inertness and being nontoxic. However, complications including capsular contracture and anaplastic large cell lymphoma have been associated with certain breast implant surfaces over time. Novel implant surfaces and modifications of existing ones can directly impact cell-surface interactions and enhance biocompatibility and integration. The extent of foreign body response induced by breast implants influence implant success and integration into the body. This review highlights recent advances in breast implant surface technologies including modifications of implant surface topography and chemistry and effects on protein adsorption, and cell adhesion. A comprehensive online literature search was performed for relevant articles using the following keywords silicone breast implants, foreign body response, cell adhesion, protein adsorption, and cell-surface interaction. Properties of silicone breast implants impacting cell-material interactions including surface roughness, wettability, and stiffness, are discussed. Recent studies highlighting both silicone implant surface activation strategies and modifications to enhance biocompatibility in order to prevent capsular contracture formation and development of anaplastic large cell lymphoma are presented. Overall, breast implant surface modifications are being extensively investigated in order to improve implant biocompatibility to cater for increased demand for both cosmetic and oncologic surgeries.
Similar content being viewed by others
Background
Breast augmentation is one of the most common plastic surgical procedures performed to correct breast volume and shape abnormality for both cosmetic and oncologic indications. Estimates put the number of breast implants at around 8 million worldwide [1]. According to the International Society of Aesthetic Plastic Surgery (ISAPS) statistics report of 2019 [2], approximately half of the total annual breast procedures in the world were breast augmentations, with 89% using silicone implants [2]. Since 1963, silicone breast implants have been utilised increasingly for both plastic and reconstructive surgical indications. Indeed, significant improvements have been observed in terms of their biocompatibility and safety [3, 4]. For example, Choi and colleagues demonstrated that the presence of micro-textures on silicone implants suppress foreign body response (FBR) and capsular contracture [5]. However, significant problems continue to exist, and various strategies have been utilised to improve silicone implant performance which continues to remain under investigation. These strategies are aimed at improving implant biocompatibility and enhancing implant integration in the human body as well as the prevention of silicone implant ‘bleeding’ and stimulation of FBR [6, 7].
Silicone, with the most common being polydimethylsiloxane (PDMS), has many diverse uses including incorporation in medical devices such as implants and catheters [8, 9]. As an inert material, silicone does not degrade and displays great properties ranging from low toxicity, as well as being gas permeable [10, 11]. Despite its appealing properties, silicone materials also exhibit a hydrophobic nature [12]. Silicone hydrophobicity leads to poor anti-fouling activities and this can impact on its efficacy in medical devices [13]. Implantation of ‘foreign material’ in the body causes the host tissue to initiate a defence mechanism known as FBR, characterised by a series of humoral and cellular activities. The extent of host response depends on several factors including the foreign material’s biocompatibility and the host tissue’s response.
Adsorption of proteins onto the implant surface facilitates the attachment of various cells including immune cells and fibroblasts as well as the activation of signalling cascades leading to formation of a capsule around the implant. Excessive FBR may result in enhanced extracellular matrix (ECM) synthesis leading to the formation of a dense contracting capsule which prevents the proper implant-breast tissue integration ultimately leading to structural deformation of the implant and continuous pain and discomfort to patients [12, 14]. This necessitates the replacement of the old implant. Implant surface properties play key roles in the adsorption of proteins and ultimately the attachment of cells to the implant. Thus, a large portion of research has been dedicated to investigating implant surface properties and modifications and effects on integration into the body [15,16,17,18,19,20,21,22]. For instance, of note macro-textured silicone breast implants have been linked to the development of anaplastic large cell lymphoma (ALCL) [1].
Several in vitro and in vivo studies on silicone breast implants have revealed insight into the role of implant surface in mediating cellular and tissue behaviour or function (Table 1) [15,16,17,18,19,20,21,22,23,24]. These studies demonstrated that implant properties including topography can influence implant integration and their ultimate fate in vivo [17,18,19,20, 22]. A number of studies have shown that breast-derived fibroblasts are affected by the physical and chemical characteristics of the silicone shells and over time adapt to the specific topographies of the material after being stressed [25,26,27]. Interestingly, in an in vitro study carried out by Kyle et al., the effect of silicone implant surfaces compared with biomimetically engineered silicone surfaces was evaluated using breast-derived fibroblasts [18]. This study demonstrated that a biomimetic-engineered implant surface was superior in attenuating FBR in terms of development of an inflammatory response compared with most common commercially available silicone implant surfaces [18]. Furthermore, Doloff et al. studied the effect of silicone breast implant surface topography on capsule formation and FBR in human and other animal models [15]. The authors discovered, using both animal and human studies, that biomimetic surfaces with the roughness of around 4 μm provoked the least amount of inflammation as well as FBR. In another study using both animals and humans, Chung and colleagues were able to identify immune regulators of FBR after implantation of implants including silicone breast implants [21]. An in vivo study by Brigaud and co-workers investigated ECM and inflammatory gene expression in capsules from human patients using textured implants and showed that implant surface topography provide ‘cues’ that impact gene expression [28].
The aim of this review is to present recent advances in implant surface technology including surface topography and chemistry, and to demonstrate how these impact silicone implant biocompatibility and biointegration. We demonstrate that roughness and wettability influence the type and number of proteins adsorbed onto the implant surface and therefore can affect the FBR. Overall, we show that modifications of implant surfaces are important in enhancing biocompatibility.
Methodology
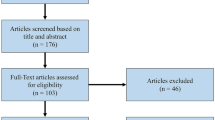
We performed an electronic search on Scopus, PubMed and Web of Science to identify articles to be included using specific search strings including keywords silicone breast implants, host response, cell adhesion, protein adsorption, and cell-surface interaction. This comprehensive literature search was performed for relevant manuscripts on the evolution of breast implants and origins of theories. Abstracts and titles of studies were screened by authors and included if they met the inclusion criteria. Duplicate articles were removed.
Past and current silicone-gel breast implants used in surgical practice
Silicone gel implants have been used widely since the 1960s (Fig. 1). Interestingly, the first generation of silicone-gel breast implants consisted of a teardrop pre-shaped prosthesis composed of a thick (0.75 mm), smooth silicone elastomer shell filled with Silastic™ and a dacron mesh backing, which became anchored in the underlying pectoral fascia [29]. Due to high cases of capsular contracture and firmness of these original silicone gel-filled implants, new types of silicone-gel filled implants emerged, with thinner (0.13 mm) and seamless shells, which were introduced in 1970s. The new silicone gel filled implants had low viscosity to provide a more natural feel, and the fixation patches were eliminated [30]. However, several reports showed that these second-generation implants suffered from increasing firmness, shell rupture and bleeding of the silicone gel [31, 32]. Therefore, third-generation implants with high-performance multi-layered shells and a much more cohesive gel were introduced [33, 34].
Historical evolution of silicone breast implants. Important breakthroughs in silicone implants technologies starting with implants with Dacron patches on the posterior side to the latest implants with biocompatible shells and radio frequency identification technologies. First generation silicone breast implants were made from thick smooth silicone elastomer shell filled with Silastic. Second generation implants consisted of thinner and seamless shells, with the fixation patches removed. Third generation implants were introduced from 1982 onwards and consisted of high-performance multi-layered shells with a cohesive gel. The introduction of texturing saw the entrance of fourth generation implants from 1987. From 1993, fifth generation implants were introduced, and these have an anatomical shape with a highly cohesive gel. From 2010, sixth generation implants were introduced, and these have a biocompatible shell and a rheological gel. Other technologies such as radio frequency identification are associated with sixth generation silicone implants
Aiming to prevent the development of capsular contracture, double-lumen implants consisting of an inner silicone gel-filled lumen surrounded by an outer saline inflatable shell were designed [35]. In addition, the reverse type of implants, with an outer silicone gel-filled shell surrounded an inner inflatable shell, have been investigated. The reverse double-lumen was shown to provide better properties including no wrinkling of the outer shell, a more natural breast feel, and a nonpalpable self-sealing posterior valve compared to the inflatable saline-filled breast [36]. Concerns related to biocompatibility and safety use of silicone gel implants led to provisional restrictions on some specific implants from the American market in 1992 by the Food and Drug Administration (FDA) until 2006. In turn, core studies to assess overall implant safety profiles have been carried out [37,38,39,40] and led to development of silicone gel-filled implants focusing on shell properties, gel cohesiveness, and anatomical shape.
Breast tissue response to implant
The insertion of an implant into the breast tissue results in an inflammatory reaction by the body referred to as FBR which is characterised by the release of immune factors such as chemokines and cytokines. Enhanced levels of chemokines and cytokines result in excessive inflammation as well as increased synthesis of several ECM proteins [41, 42]. This section briefly describes the breast tissue wound healing response to the placement and presence of the implant.
Breast anatomy and histology: implications on implant placement
The human breast is composed of five components: 1) skin 2) superficial fascia, 3) breast parenchyma 4) nipple (areola complex) and 5) deep fascia [43] (Fig. 2). The parenchyma can be divided into three tissue types: glandular epithelium, fibrous stroma, and supporting structures and fat (adipose tissue) [44]. The glandular epithelium forms a system of branching ducts connected to the nipples and lobules where the milk is produced. Other parts of the breast provide a substrate for glandular epithelium development and functions [45]. The neovascular and lymphatic structures of the breast provide nutrition for breast cells and drain fluid into lymph nodes, respectively [46]. Anatomically, two-thirds of the breast is placed anterior to the pectoralis muscle with the rest elongating from the margin of sternum out to the midaxillary line. The tail of breast tissue known as the ‘axillary tail of spence’, is prolonged into the axilla [45]. The breast contains various cells including epithelial cells, fibroblasts, and immune cells. Epithelial cells grow from the nipple into a fat pad, formed by adipocytes, and infiltrated by vascular endothelial cells [47].
Insertion of an implant into the breast cavity depends on various factors such as the patient ‘s breast size and anatomy. An incision (infra-mammary, peri-areolar, trans-axillary, or trans-umbilical) is made to place the implant either in the sub-glandular (Fig. 2a) or dual-plane/ partial under the muscle or sub-pectoral [48] (Fig. 2b). If the patient has enough natural breast tissue the sub-glandular placement is the obvious choice for surgeons as it is easier for surgery and has better outcomes in terms of patient satisfaction [48]. However, placement of the implant in the sub-glandular position is more palpable and studies have indicated that the risk of capsular contracture is higher [49].
Implant-host tissue dynamics following implantation
Following surgical incision and implantation, the local release of chemical mediators by injured cells results in a wound healing process characterised by an early inflammatory response and subsequent wound healing events [41, 42] (Fig. 3). Vasoactive substances cause changes in blood flow and vascular permeability leading to extracellular fluid and cells moving from the circulatory system to the injured tissue in a process called exudation [41, 42]. Both the extracellular fluid and migrating cells interact dynamically with the implant surface (Fig. 3).
Protein adsorption and provisional matrix formation
Immediately after implantation, mixtures of proteins, lipids, ions, and carbohydrates from the blood and wound bed competitively adsorb onto the implant’s surface [50,51,52]. This mixture may desorb, displace, or change conformation as well as denature until an enriched layer of stable proteins is formed [53, 54]. The rapid exchange of proteins on the implants’ surfaces was first described by Vroman and Adams in 1969, and it is commonly mentioned as a Vroman effect [55, 56]. Concentration, rate of diffusion, and affinity of proteins are influential in the adsorption of proteins on the implant surface. Small proteins found in a high concentration such as albumin, tend to adsorb on the implant first, but are gradually replaced by larger and higher affinity proteins such as fibrinogen and collagen [57, 58].
Various mechanisms have been proposed to describe the exchange of proteins adsorbed on solid surfaces and these include i) adsorption/desorption, ii) competitive exchange, and iii) exchange via transient complex formation [59, 60]. In vivo, however, protein adsorption is a highly complex process and not yet wholly understood as a vast number of proteins are involved. Importantly, various proteins are continuously secreted by cells including the ECM proteins. For instance, in a proteomic study of adsorbed proteins, Barr and colleagues identified 822 proteins on silicone implants’ surfaces after breast implantation [61]. Furthermore, the affinity of proteins to the implant surface is altered by various other parameters, including the physio-chemical properties of the implant’s surface and other proteins’ presence on the surface.
Local and recruited cells at the implantation site are much larger than proteins and thus move much more slowly. Cells encounter a dynamic layer of proteins covering the implant’s surface allowing attachment to occur. Some of these proteins, like von Willebrand’s factor, fibrinogen, vitronectin, and fibronectin, have specific peptide segments (e.g., arginine–glycine–asparagine (RGD) and proline-histidine-serine-arginine-asparagine (PHSRN) sequence) recognised by adhesion receptors on various cells. These cell recognition sequences facilitate cell attachment and subsequent tissue regeneration [62, 63]. Cell-surface interactions involving ECM proteins regulate cell behaviour through interactions with cell-surface receptors, such as integrin, and this results in tissue-specific cell spreading, migration, tissue assembly, and differentiation, as well as cell-to-cell communications (Fig. 4) [64]. Proteins prone to denature may induce the innate immune system whilst proteins in their native conformation do not [65].
Schematic illustration of the cell-implant interactions via adhesion-mediating proteins and receptors. During attachment and spreading on the implant, the cell adheres to proteins adsorbed on the implant surface including collagen and fibronectin through transmembrane integrins units. Focal complexes are formed termed focal adhesion complexes consisting of molecular components such as paxillin, talin and vinculin
One large protein known to bind to the implant surface is fibrinogen. Fibrinogen has a large size of 330 kDa and is one of the most abundant proteins involved in promoting adhesion of platelets, neutrophils as well as macrophages bonding to each other via αIIbβ3 (cluster of differentiation 41 (CD41)/CD61, GPIIb/IIIa), αMβ2 (CD11b/CD18, Mac‐1, and Cr3), and αXβ2 (CD11c/CD18, p150,95) integrin [66, 67]. Additionally, fibrinogen plays a crucial role in the blood clotting process by forming a fibrin network through the coagulation cascade [68].
As a result of protein-implant interactions, a provisional matrix with three-dimensional structural integrity develops at the tissue-implant interface, consisting of fibrin, inflammatory mediators, trapping cells, proteins, and platelets. This matrix is the initial ‘blood clot’ or ‘thrombus’ from the wound healing process formed through the conversion of fibrinogen to fibrin which is mediated by the initiator of activated factor XII/ Hageman factor (intrinsic pathway) or factor III/ tissue factor (extrinsic pathway) [41, 42, 69]. Macrophage-derived interleukin-10 (IL-10) has been shown to be involved in the cleavage of fibrinogen into fibrin, the major component of the provisional matrix [15]. Production of interleukin-10 by macrophages occurs concurrently with inhibition of tumour necrosis factor-alpha production [15]. Simultaneously, platelets secrete platelet factor 4 (PF4), platelet-derived growth factor (PDGF), and transforming growth factor beta (TGF-β), which play a part in leukocyte, fibroblast, and platelet recruitment [70].
To summarise, protein adsorption on the implant’s surface is necessary for wound healing. However, from the cell and histocompatibility perspective, if the thickness of the protein layer increases or specific protein conformation enhances cellular adhesion, this can lead to excessive capsule formation.
Inflammation
Injury to the skin and breast tissue followed by insertion of the implant induces FBR and sets in motion a series of events known as inflammation. Inflammation allows the body to clean up any cellular debris and infectious organisms and initiate repair [42]. The first stage of inflammation referred to as acute inflammation begins with the infiltration of polymorphonuclear leukocytes (PMNs) such as neutrophils, and mast cells to the injured tissue in response to diverse endogenous damage-associated molecular patterns (DAMPs) released from necrotic cell death [71].
Chemo-attractants produced by activated complement products, platelets, endothelial cells, and bacteria during implant insertion induce inflammation [72,73,74,75]. In turn, PMNs and later monocytes migrate to the injured tissue to phagocytose invading pathogens and cellular debris. Adsorption of ECM proteins such as fibronectin on the surface of the implant can increase neutrophil extracellular traps (NET) that are involved in elimination of infection agents through the action of proteases attached to chromatin filaments [76]. Over time, neutrophils are depleted via apoptosis either spontaneously or via the action of macrophages (efferocytosis process) [77, 78]. Breast implants cannot be engulfed by phagocytic cells due to their large size (> 10 µm) and this leads to secretion of mediators of degradation, such as reactive oxygen intermediates, degradative enzymes, and acids that may damage the implant and the surrounding healthy tissue [79,80,81].
The implant surface properties, type of adsorbed proteins, and the extent and duration of inflammatory responses may lead to chronic inflammation. In addition, infection and movement of the implant within the breast pocket (tribology) may additionally prolong the process of acute inflammation leading to chronic inflammation [82, 83]. Single macrophages fuse to form the multi-nucleated giant cells, known as foreign body giant cells (FBGCs) that attempt to phagocytose the implant. The inability to engulf implants [84], causes FBGCs to change to a “frustrated phagocytosis” state and remain on the implant’s surface via podosome adhesion (not focal contacts) [85]. Several inflammatory associated cytokines including IL-4 and IL-13 produced by immune cells at the injury site cause macrophage fusion [86,87,88]. Furthermore, chemo-attractants such as the chemokine (C–C motif) ligand 2 (CCL2) are also involved in directing macrophages towards each other [89].
Various pieces of evidence show that the von Willebrand factor, which was already adsorbed onto the surface, can reduce macrophages’ adhesion to the implants, leading to a decrease in FBGCs formation. In contrast, Immunoglobulin G (IgG) adsorption on the implant surface strongly provokes macrophage adhesion in the long term [90]. McNally and colleagues [87] demonstrated that vitronectin, interacting with integrin adhesion receptors of integrin alpha V beta-1 (αVβ1) and integrin alpha M beta-2 (αMβ2), can considerably promote macrophage adhesion and IL-4-induced FBGC formation. It has been demonstrated that the involvement and interaction of specific cell types, adsorbed proteins, cytokines, and chemokines can lead to induction of both acute and chronic inflammation at the injury site after implant insertion [87].
Fibrotic encapsulation
Adherent FBGCs/ macrophages and accumulation of collagen from fibroblast causes the persistence of FBR. Several reports indicate that when cells attach to the implant and release several cytokines, this influences FBR and induces signalling transduction [18, 91]. Many of the induced signalling cascades are involved in stimulating ECM synthesis and release of cytokines and growth factors [18, 82, 91, 92]. Fibroblasts are known to occupy most spaces on the material/ implant surface where they deposit several ECM proteins such as type I collagen [93,94,95]. ECM proteins deposited on traditional smooth implant surfaces are aligned nicely, whilst those deposited on rough implant surfaces may not be optimally oriented [96, 97]. The alignment of ECM proteins such as collagens, facilitates implant isolation in a fibrous capsule [98]. In addition, if apoptosis of granulation tissue does not occur, fibrotic encapsulation of the implant occurs [99].
Dolores and colleagues demonstrated that the fibrous capsule removed from patients at various times after silicone breast implant surgery is mainly composed of three layers; (i) a layer touching the silicone implant, mainly composed of macrophages and fibroblasts (ii) an intermediate layer of connective tissue with internal vascular vessels, and (iii) an outer layer of dense connective tissue with external vascular vessels [90]. Moreover, T-lymphocytes CD4 + and dendritic cells (CD1a/CD208 + cells) are present in the inner layer in contact with the silicone implant and contribute toward immune response in the fibrous capsule. A high amount of fibronectin and tenascin were also detected in the first layer that mediates cellular and ECM protein interactions [90]. Within days of implant insertion, granulocytes, lymphocytes, and fibroblasts surround the implant and contribute towards the formation of a provisional matrix (Fig. 5). Over time, more fibroblasts and dendritic cells are also recruited to the implant site. Type III collagen in the initial provisional matrix is replaced with type I collagen as a fibrous capsule form around the implant (Fig. 5) [100,101,102,103].
The development of a capsule over time after breast implant insertion. Days after insertion of the implant, cells such as granulocytes, lymphocytes, and fibroblasts surround the implant and contribute towards the formation of a normal and thin capsule. Over time, more fibroblasts and dendritic cells can be recruited to the implant site, leading to synthesis of more ECM proteins. Type III collagen in the initial provisional matrix is replaced with type I collagen as more fibrous ECM is formed around the implant. Encapsulation is part of the normal physiologic FBR, however, excessive deposition of fibrous ECM around the implants contracts the implant and cause capsular contracture
Whilst encapsulation is part of the physiologic FBR, excessive deposition of fibrous material around the implants contracts the implant and leads to progressive capsular contracture. Silicone implant-related capsular contracture is associated with pain, discomfort, and hardness, and deformation of breast tissue. The amount of capsule around the implant varies and is linked to implant features such as surface topography and wettability. A histological analysis by Glicksman and colleagues demonstrated that textured implants as well as the continued presence of shearing forces are linked to enhanced development of FBR leading to the formation of double capsules [104]. Various studies have shown that implants of different roughness and hydrophobicity influence implant biocompatibility/integration and may play a key role in the development of complications post-implant augmentation [15, 105, 106].
Silicone breast implant-related complications
Silicone breast implants have received both conflicting reviews since their first use decades ago. Despite the great benefit derived from silicone implants, their use and the resulting issues have led to increased scrutiny [107]. Questions about the safety of silicone breast implants arose following concerning reports on the possible link between certain types of textured silicone breast implants and specific neoplastic changes. Definitive studies showing the determining factors for someone to develop these complications are still lacking. Textured implants were introduced to increase the integration of the implants in the human body [1, 108]. However, textured implants were significantly associated with increased of development of anaplastic large cell lymphoma [109, 110]. Furthermore, other adverse effects include capsular contracture formation, implant leakage/rupture, site-specific complications and silicone particulate migration to different body tissues including the lung and skin [111]. Particulate debris and gel leakage can result in migration of silicone to other parts of the body which can also interfere with the detection of cancer. To overcome some of these problems, new and novel silicone implants are being introduced including the introduction of the Motiva SmoothSilk® / SilkSurface®. Some of these new implants have more than one layer of silicone in addition to a blue seal layer which prevents silicone gel leakage through the shell [112].
Implant-related capsular contracture
Breast augmentation has been associated with several complications and these include bacterial infection, scarring, hematoma, capsular contraction, and a rare cancer known as breast implant associated ALCL [109, 110]. Of these, capsular contracture is the most common complication associated with breast augmentation and in most cases requires surgical correction [109, 110]. Several reports indicate that thousands of implants are either removed or replaced each year globally [113]. Although estimates differ, a minimum of a fifth of breast augmentations will require corrections within the first 10 years after placement of the implant [114]. Capsular contracture is the main reason for surgical corrections post-breast implant augmentation [39], as the risk of developing and recurrence of capsular contracture continues to be relatively high [115, 116]. Ideally, the protective capsule formed must be a thin layer of fibrous proteins. However, a persistent fibrotic process can lead to a thicker capsule which hardens into the pathogenic capsular contracture [98, 117]. Bacterial infection (mostly opportunistic during surgery) can result in persistent presence of inflammatory cells around the inserted implant [118]. The resulting inflammation cause the body to synthesize ECM molecules in a bid to isolate the affected area [119]. Chronic inflammation can lead to excessive ECM synthesis and formation of capsular contracture [120]. Furthermore, bacteria can easily attach to adsorbed proteins on the implant surface via adhesins [121]. Whilst the early stages of capsule formation do not show any physical distortions to the breast, the continual tightening associated with capsular contracture eventually results in complications including malposition and discomfort for the patient [116, 122]. In this scenario, a regular check-up and replacement of the implant is recommended to detect the onset and treatment of capsular contracture formation [123, 124]. Implants of different textures and roughness have been associated with varying degrees and severity of capsular contractures [125, 126].
A clinical grading system approved by the Food and Drug Administration, referred to as the Baker grading system, is commonly used to describe the extent or degree of capsular contracture [127]. The Baker grading system groups the capsular contracture into four grades, with grade I used for breasts with a natural feel which physically looks normal [127, 128]. In this grade both the capsule and breast are normal. Grade II is when there is minimal capsular contracture and the breast is slightly firm when touched [127]. Both grade III and grade IV display symptoms. Grade III is characterised by moderate contracture with the breast feeling hard to touch whilst grade IV is used for severe contracture which is felt by the patient as well as displaying physical deformities seen by the doctor [127]. Reports show that the development of new and improved implants has resulted in decreased cases of capsular contracture [129,130,131]. Several reports indicate that certain types of texturisation of implant surfaces may have played a role in reducing the rate of capsular contracture formation [130, 131]. Randomised clinical trials, however, have shown that certain textured implants were associated with lower cases of capsular contracture compared to traditional smooth surface implants [132, 133]. Controlled clinical trials involving many patients demonstrated that patients receiving the traditional smooth surface implants are likely to develop capsular contracture compared to those receiving certain textured implants within 5 years [134, 135].
Conflicting reports are available with other reports suggesting that the placement position of textured implants matter. For example, the placement of implant under the glandular tissue is associated with capsular contracture whilst placement of implant under the pectoral muscle do not show any link to development of capsular contracture [136, 137]. In addition, improvements in surgical techniques and modifications that decreased biofilm development have helped decrease cases of capsular contracture [49]. Furthermore, prevention of gel bleeds as well as rupture of the implants, also aided in decreasing cases of capsular contracture [138, 139]. One of the issues associated with many clinical studies is the lack of long-term outcomes as well as providing adequate follow-up details about the study itself [140, 141].
Implant-related anaplastic large cell lymphoma
About a decade ago, the Food and Drug Administration reported a possible association between a cancer of the breast called ALCL and the use of textured breast implants [142, 143]. ALCL is a rare T-cell non-Hodgkin lymphoma that occurs within 10 years of implant insertion [143, 144]. Although ALCL was first described in 1997, the World Health Organization (WHO) only recognised it as a cancer of the breast in 2016 [113]. Most of the cases reported so far occur in countries with high usage of breast implants including the USA and Australia [145, 146]. Although the number of cases of ALCL is low, this may be due to under-reporting.
ALCL is characterised as a persistent fluid with cancer cells or a mass of cancer cells attached to the fibrous capsule and mostly occurs in one breast [147]. In some cases, ALCL can spread to lymph nodes. Reports show that ALCL is linked closely to the use of textured breast implants with high surface areas [146, 148,149,150]. Various theories have been presented on the origin of ALCL, from bacterial contamination to extreme inflammation linked FBR. ALCL can cause pain and discomfort to patients. Most reported studies linking ALCL to bacterial inflammation are based on the association [151,152,153]. Importantly, many studies have suggested a multifactorial cause for the development of ALCL ranging from bacterial infection [154], implant surface texture [155, 156], genetic factors [157], and mechanical friction [158]. Removal of the neoplastic and fibrotic tissue, as well as the implant itself are some of the ways to effectively treat ALCL [149]. Chemotherapy may be given to patients with advanced disease as well as those with a possibility of metastasis [159, 160].
Cancerous cells found within the ALCL seroma display horseshoe-shaped nuclei in addition to being anaplastic lymphoma kinase negative [161]. These cells are also CD30-positive and express T-cell markers including CD3 and CD4. Other markers expressed by these cancerous cells include CD25, CD80, and Interleukin 6 (IL-6) [162,163,164]. It is suggested that inflammation can cause T-cells to proliferate excessively [163] and together with cytokines involved in lymphocyte division, this may lead to some cells becoming tumorigenic. This tumorigenic process is then driven further by cytokines such as IL-6. Together with TGF-β and IL-10, IL-6 is thought to induce immune suppression, further promoting tumorigenesis by inhibiting host anti-tumour immunity [163, 165]. Another unproven theory is the association with development of biofilm infection in addition to a person’s genetic background that may trigger cell proliferation, which is acted upon by selection pressure to yield proliferation of a cell with proliferative advantage, leading to ALCL [165].
Several studies have supported the theory that biofilm infection can cause ALCL [150, 157, 166]. Silicone implants’ hydrophobicity can cause non-specific adsorption of various blood and wound fluid proteins leading to fouling. This in turn promotes growth of several bacterial strains on the implant surface [167]. For example, it was shown that Helicobacter pylori infection can cause inflammation over time, which is now recognised as a causal agent in the development of lymphoma of the gut [168]. Staphylococcus epidermis contamination on the implant surface can cause enhanced fibrosis [169]. A recent study reported high levels of Ralstonia picketti in ALCL-linked breast implants [151]. In addition, antibiotics are known to cause remission of the disease in many patients. Doxycycline treatment of Chlamydophila psittaci causes regression of adnexal marginal zone lymphoma [170]. Several studies have shown that textured implants may promote bacterial growth more than smooth surface implants. Bacterial growth on textured implants can cause inflammation, leading to tumorigenesis and the development of T-cell lymphoma [166, 171, 172]. More lymphocytes have been observed to attach to textured implants versus smooth surface implants and a positive link has been found between bacterial growth and lymphocytes attached to implants [166, 171, 172]. Most importantly, biofilm has been detected on clinical samples of ALCL via quantitative polymerase chain reaction (qPCR) as well as visual analysis using scanning electron microscopy and fluorescent in situ hybridisation [151]. A large proportion of the bacteria in ALCL were identified by sequencing studies as Gram-negative [151].
The described complications associated with silicone breast implants suggest that the implant properties (physical and chemical) impact on biocompatibility. An optimised silicone surface via modifications would enhance the implant biocompatibility and reduce the occurrence of complications.
Silicone implant properties
The implant’s physio-chemical properties mainly influence the type and number of proteins adsorbed onto its surface and the subsequent inflammatory cell adhesion and FBR. Importantly, silicone surface implant properties can determine the fate of the breast implant in the body (Fig. 6). To ensure that silicone breast implants have optimal biocompatibility and display a desirable biological response, researchers have investigated strategies that minimise FBR by focusing on improving shell and gel properties. This review discusses recent modifications and advances in implant surface properties aimed at improving cell adhesion and enhanced implant integration in the body.
Surface topography
Implant’s surface topography, including profile shape and roughness influence the types of proteins that adsorb onto the implant surface as well as their conformation and ultimately impact cell orientation alongside the implant [173]. In addition, the orientation of collagen fibres deposited around the implant is impacted by the implant surface topography [136, 174].
Extensive research has been performed on the surface topography of breast implants aiming to control cellular response and ultimately influence implant fate in the body. For example, coating fine-cell polyurethane, a technique invented by William J Pangman [175], on the implants’ surface, formed open-pore texture leading to better tissue ingrowth and supposedly low tendency to capsular contracture [176]. However, polyurethane-foam-covered silicone implants gradually degraded in-vivo, producing toxic hydrolysis material, and caused delayed FBR [177, 178]. These silicone breast implants were therefore withdrawn from the United States of America implant market [179]. Soon after, modifications of silicone surfaces resulted in surfaces showing better biointegration and reduced FBR with each surface having a distinct microenvironment influencing cell shape and, thus, bio-integration depending on their texturising method [22, 179]. Various methods are used to achieve texturisation and these include imprinting, salt-loss, and gas expansion technique. Whilst the main aim of texturisation is to prevent implant malposition as well as easy maintenance, biointegration of silicone implants remains an issue requiring further investigations.
It has been shown that collagen fibrils around textured breast implants have multiplane conformation that causes more flexible and thinner capsules and are less likely to cause contraction [180]. In comparison, collagen fibres are organised longitudinally and parallel to the traditional smooth implants during early inflammation, and gradually change their orientations in the long term [181, 182]. Capsule formation is enhanced when fibres are aligned longitudinally. Contrasting data on histologic tissue responses and clinical outcomes on textured shells demonstrated the superiority of textured surfaces over smooth surfaces in decreasing capsular contracture and reoperation [125, 126, 136, 183,184,185,186]. For example, Poeppl and colleagues demonstrated that patients with textured breast implants showed reduced degree of symptoms for capsular contracture than patients who had smooth-surfaced implants [125]. Fischer and co-workers showed that textured silicone implants resulted in temporarily thicker but overall less dense fibrotic capsules compared with smooth surfaces in an animal model [187]. Moreover, Bergman and co-workers showed that textured implants can enhance bacterial contamination leading to increased risk of capsular contracture [188].
Properties of textured implant surfaces including size and shape influence soft tissue adhesion. Deep pores (> 350 µm) have demonstrated increased fibrous capsule disruption and enhanced tissue ingrowth into textures than smaller pores, leading to decreasing the risk of capsular contracture and implant movement respectively [22, 181]. Furthermore, textured implant surfaces, increased surface area for attachment compared to smooth surfaces, allowed tissue ingrowth and more adherence than smooth surfaces [22]. Tolksdorf and co-workers [189] recently investigated the effect of different pore sizes of silicone textured surfaces produced by the salt-loss technique on human fibroblast behaviour in an in vitro model. The authors’ results showed that textured surfaces with fine (< 65 µm) and medium (> 250 µm) pore size leads to a compact uniform cell layer with good adhesion. In contrast, the fibroblasts could not bridge the coarse texture with larger pores (> 500 µm), causing irregular growth and finger-shaped cell extension missing the intracellular contact. Moreover, the expression of TGFβ1, a key molecule for differentiation of fibroblast to myofibroblast and creation of capsular contracture, was lower on fine and medium texture compared with coarse ones [189].
Topographical features may provide areas that are desirable for focal adhesion formation [190]. A one-week examination of fibroblast cytoskeleton orientation on different smooth and microtextured surfaces has shown that microfilaments and the vinculin-containing attachment aggregations could orient toward several directions on the surfaces with large ridges (5 and 10 µm). In contrast, on surfaces with the small size of ridges (2 µm), they attached only in the direction of ridges [190].
To understand the effect of surface topography on cell behaviour, it is important to consider the topographical aspect ratio (depth/width) instead of one feature dimension (width, depth, or pitch). The increase in the aspect ratio of textures on the surface increases cell alignment and elongation regardless of material and cell type [191]. Depending on the texturising method, the shapes of textures are different [28, 192]. The cross-section and surface topographical examination of 17 types of breast implants have shown they typically fit into three categories; i) regular peak and valley structures with heights of low amplitude (PV-patterned surfaces) ii) curve-shaped open cavities features of amplitude ranging from 50 µm to 300 µm (OC-patterned surfaces), iii) repetitive and regularly distributed unsealed cuboid-like patterns of high amplitude (> 400 μm) (semi-opened cavities (SOC)-patterned surfaces) [28]. The respective cross-section of these categories is given in Table 2. Overhanging features of some cuboid structures can help fix the position of ingrowing tissue and device [17]. The coated-salt-loss technique or salt-loss technique followed by brushing can generate this structure [28, 193].
An animal study of capsule formation and tissue adherence of different breast implant surfaces at six weeks after implantation revealed that surfaces with larger surface area textures develop unstructured alignment of collagen fibrils at their tissue-implant interface and need stronger force for detachment of the implant tissue [22].
Another important parameter to characterise surface topography is surface roughness. The surface is considered rough if the actual surface’s vertical deviations against its ideal form are large and smooth if the deviations are small [194]. Surface roughness parameters include height descriptors (e.g., arithmetic mean height (Ra), surface skewness (Ssk), and kurtosis value (Sku)) can manipulate friction and cell adhesion and eventually tissue response. Surface roughness is associated with increased surface area [14], and contact angle (hydrophobicity) [195], but this depends on the nature of the material analysed. Increased implant surface area is linked to enhanced cell adhesion, in particular adhesion of fibroblasts [19, 196]. Prasad et al. [197] showed that in the sub-micron scale (88–650 nm), an increase in the roughness of silicone elastomer substrates decreases fibroblast growth. Rough surfaces also induce macrophage (M1) activation to (M2) by up-regulating macrophage inflammatory proteins 1a (MIP-1a) and monocyte chemoattractant protein-1 (MCP-1) and downregulating the secretion of chemokine C-X-C motif chemokine ligand 10 (CXCL10) [198]. Surface topography plays a key role in directing extracellular matrix related gene expression [28]. A study involving the use of breast implants with semi-opened cavities-patterned surfaces demonstrated that metalloproteinase inhibitor 4 (TIMP4) and tumour necrosis factor ligand superfamily member 11 (TNSFS11) expression were remarkably down-regulated. In addition, matrix metallopeptidase 9 (MMP9), matrix MMP12, TIMP1, and IL-8 were drastically up-regulated compared to other surfaces with peak and valleys and open cavities patterned surfaces [28]. Overall, evidence shows that the progression of FBR is dependent on many factors including cytokines and MMPs. These soluble factors are secreted by various cells including fibroblasts, macrophages, and inflammatory cells. Chemokines and MMPs cause a series of cellular events associated with FBR such as invasion, blood vessel formation, migration and fibrosis. Constant changes that occur during FBR means that the amounts and type of soluble mediators available differs at various time points.
The International Organization for Standardization (ISO) in ISO 14607:2018 [199] has defined three categories based on the value of average surface roughness; smooth: < 10 μm; microtexture: 10–50 μm, and macrotexture: > 50 μm and given guidance on the assessment of the physical surface characteristics of silicone implants. Many scientists within the materials field have suggested alternative classifications of texturisation. As a result, many studies have used surface topography parameters including roughness [17, 28], and surface area [22, 192] in order to classify textured breast implants (Table 2).
Despite displaying several advantages, studies on textured implants report long-term complications such as late seroma, double capsule, and anaplastic large cell lymphoma (ALCL) [200,201,202,203]. As a result, new breast implants with smooth surfaces have been introduced and shown fewer complications [112, 204]. The three-dimensional (3D) imprinting technology is used for these novel implants to create low roughness features and micro/nano topographical structures with high contact points on PDMS [112]. Since the surface topographic properties of these new implants are less than the cellular level, tissue ingrowth is impossible [17]. Furthermore, the surface’s high contact points prevent fibroblast clumping, presumably decreasing capsular contracture risk [112]. In addition, immunophenotypic characterisation has shown that on these surfaces, the secretion of tumour necrosis factor α (TNF-α) and IL-1β (inflammatory cytokines) by cells is lower than when cells are cultured on other surfaces [23].
Surface stiffness
While more studies have focused on implant surface topography, the formation of implant-cell adhesion complexes rely on the softness and stiffness of the implant’s shell [205]. The stiffness of substrates is influenced by thickness and can be calculated through measuring the elastic modulus [19]. The elastic modulus (E) of various commercial breast implant shells was measured and shown to be around 600–3000 kPa, values higher than the elasticity of the human dermis (E < 10 kPa) and human mammary tissue (E < 0.5 kPa) [19, 205, 206]. Cells have been shown to spread more on substrates with high stiffness, with F-actin cytoskeleton networks being more organised. In contrast, cells assume a round shape with restricted F-actin complexes on soft substrates [207,208,209]. In addition, stiffness influences ECM protein secretions, thus, regulating ECM ligand depositions for cell attachment [210].
An in vitro assessment of neutrophil activities on silicone surfaces with different stiffness (0.2–32 kPa) revealed that stiffer surfaces evoke NET formation and more pro-inflammatory cytokines secretion [76]. Noskovicova et al. [205] recently investigated the effect of breast implant surfaces with different stiffness on development of fibrosis capsule in a mouse model and showed that a softer silicone layer (E ~ 2 kPa) on the breast implant reduce collagen deposition and myofibroblast activation. The reduced implant fibrosis was a result of less intracellular stress, decreased recruitment of αv and β1 integrins, and TGF-β1 signalling [205]. The same study showed that stiffness does not affect the numbers of macrophages and their polarization states in vitro [205].
Surface wettability
In terms of appropriate body response to implant and biocompatibility, wettability is a critical property of the surface. Wettability is defined as the capacity of a liquid solution to remain in contact with solid surfaces and is quantified through contact angle measurements [211]. Silicone devices have low wetting ability due to their chemical composition and are therefore considered hydrophobic. The helical structure of PDMS as well as the presence of protruding methyl groups results in a hydrophobic material. The contact angles of clinical breast implant surfaces have been measured between 108° and 142° which indicate all surfaces are hydrophobic [17, 19]. Textured implants depict 17–27% increase in contact angle and hydrophobicity compared the smooth surfaces [17, 19].
Wettability influence protein [212, 213], platelet [214], cell [215], and bacterial [216] adhesion. The more hydrophobic the surface is (shown by a contact angle > 90°), the more biomolecules such as proteins have an affinity to it [212, 213]. A surface with optimal wettability (not strongly hydrophilic or hydrophobic) adsorbs enough proteins with appropriate conformation and receptor-ligand accessibility to allow cell attachment [217]. The optimum contact angle of the surface for proper cell adhesion and cell growth is varied and depends on the kind of cell. For instance, A contact angle around 70° (moderately hydrophilic) is reported optimal for in vitro culturing fibroblasts [218], as the most abundant cell type in the breast tissue [219]. To improve wetting properties and biocompatibility of silicone implants, surface chemistry modifications of silicone have been the subject of many studies in recent decades [220,221,222,223,224,225,226].
Silicone surface coating and modifications
Silicone (PDMS) with repeating (CH3)2-Si–O- units has a hydrophobic character due to the nonpolar methyl group presence in its chemical structure. In turn, high amounts of proteins become adsorbed on the silicone and strongly interact with its surface, which leads to protein denaturation and loss of their biological activity. As a result, cell detachment occurs over time and cells cannot bind to the denatured proteins on the implant surface [227]. Moreover, bacteria and inflammatory cells readily adsorb on the silicone surface, causing biofilm formation and extensive fibrous encapsulation [12].
Immobilising polar groups on the surface of silicone can improve wettability. However, providing a homogeneous stable grafting on the surface in order to regulate the implant surface’s wettability of silicone is challenging since the silicone hydrophobic chains easily migrate to the interface and recover the surface due to silicone’s low glass transition temperature (Tg ≈ -123 °C) [12, 228]. Therefore, in most cases, modifications require pre-treatment steps.
Pre-treatments and silanization
Immobilising hydrophilic polymers on the surface requires activating the PDMS surface, which can be done using chemical oxidation, UV/ozone/γ-irradiation, plasma-induced techniques and laser treatment [220,221,222,223,224, 229]. Through these pre-treatment techniques, Si-CH3 groups will be oxidised to polar species such as Si–OH or Si-OOH groups for a limited period. Then the intended polymer can be grafted covalently to active sites provided. This paper briefly discusses pre-treatment techniques below.
The most common technique used to activate silicone surfaces is oxygen plasma treatment under vacuum. In this technique, reactive oxygen groups are introduced on the silicone surface resulting in a reactive silica layer with induced silanol groups [230]. The presence of the silanol groups enhances the silicone surface wettability for a limited time. To maintain activated silicone surface hydrophilicity for longer periods for example weeks, de-ionised water and Luria–Bertani broth can be used [106, 231]. Plasma activation has been shown to inhibit bacterial adhesion but has limitations as it can cause silicone surface cracking [232]. Importantly, oxygen plasma exposure can influence silicone surface roughness, as determined by atomic force microscopy. Another form of plasma activation is corona discharge. In this case, plasma treatment is localised and is performed under atmospheric pressure [233, 234]. Gas molecules are ionised and converted into radicals that react with the silicone surface. Corona plasma results in few molecules being oxidised but still adds polar groups to the silicone surface. Corona plasma treatment, similar to oxygen plasma, can also cause silicone surface cracking [235].
UV/ozone, via a mercury-vapor grid lamp, can be used to excite atoms on silicone surface. UV light at different wavelengths is used in a stepwise process to convert O2 to O3 and then into radicals or active species on the silicone surface. This results in the conversion of methyl groups into -OH groups [236, 237]. Further modifications can be performed on the activated surfaces with -OH groups to enhance surface wettability. A faster way to activate silicone surfaces is by using UV irradiation. In this process, the silicone material is irradiated with UV at 365 nm using a Lot Oriel mercury lamp in degassed water for about an hour [238]. Reports indicate that this technique can result in long lasting -OH groups on silicone surfaces as determined by FTIR analysis [106, 238]. The activation of silicone surface via UV irradiation is thought to involve the formation of -CH2 groups from the methyl group on silicone as well as -OH groups from water molecules. The -CH2 and -OH groups combine to form -CH2-OH on the silicone surface.
The use of ultra-short and short pulsed lasers for very short durations creates very high energy flux at a focal point and this causes plasma-mediated ablation of PDMS material. Due to the short duration of the pulse, minimum thermal breakdown is recorded. Both ultra-short and short lasers have been used in laser micromachining of PDMS surfaces [239, 240]. Precise control of PDMS laser treatment can result in a variety of micro- and nano-structures that mimic natural tissues [241]. The PDMS surface treated with lasers can then be modified further for example through immersion in various solutions of natural and synthetic polymers.
In addition to the use of energy sources for silicone surface activation, chemical oxidation, chemical vapor deposition, and sol–gel strategies can be used. Referred to as Piranha, chemical oxidation utilising a mixture of strong acids such as sulphuric acid and hydrogen peroxide has been used to activate silicone surfaces [242]. Care is needed during this activation process, as persistent exposure to the strong acids can lead to degradation of the silicone surface [238]. As reported by Yang and colleagues, cracks can appear on the PDMS surface due to over-exposure to strong acids [242]. A solution to this problem includes the use of less aggressive acids such as nitric acid [106, 238]. Wettability obtained via the use of chemical oxidation can last for weeks and sometimes months. When a silicone surface is heated, gas molecules can be transformed into solids under vacuum conditions, leading to the formation of a thin layer of material. This process is referred to as chemical vapor deposition and has been used to modify silicone surfaces with hexamethyldisilazane, for example [243]. One major disadvantage of chemical vapor deposition is the loss of hydrophilicity within minutes. This problem can be overcome by combining chemical vapor deposition and silanization [244]. Furthermore, the production of materials from other small molecules on the surface of silicone can result in a thin layer of ‘new’ material with properties influencing surface interactions with cells. This is what the sol–gel technique is based upon. For example, SiO2 can be generated on silicone surfaces via the reaction of tetraethoxysilane and water [245]. In situ formation of titanium oxide on silicone surfaces has been shown to enhance hydrophilicity over several months [246, 247].
Lastly, both micro- and nano-patterning have been used to introduce different patterns on silicone surfaces. To achieve nanopatterning, an electron beam lithography procedure is done. In the case of micro-patterning, an optical lithography procedure is performed. The flexibility of PDMS material allows textures to be introduced on its surface via the use of lithography technique [248, 249]. Using a silicone wafer as a foundation, a layer of photoresist is added on top, followed by the introduction of texture patterns by photolithography. Finally, etching will generate designs for PDMS moulding. A layer of PDMS is added on top of the patterned master, cured and finally removed from the master. Cells cultured on such patterned PDMS surfaces display characteristic shapes and morphologies [250,251,252]. A combination of photolithography and casting is used to produce nanopatterned PDMS. A layer of PDMS is made on polyester film mould, heated, and then peeled off to allow replicas to be made from the PDMS surface.
Silicone surface coating materials
A typical strategy to modify silicone hydrophobicity involves forming a passivating surface layer using hydrophilic material such as polyethylene glycol derivatives [225, 226]. Selected materials investigated for grafting on the silicone surface are summarised according to their chemical families (Table 3). These polymers are resista
nt to protein adsorption by increasing the wettability of the surface but may not resist bacteria and cell adhesion [225, 253]. Some of these materials, including high-molecular-weight hyaluronic acid (FDA-approved) and phosphorylcholine (PC), are biomimetic materials that could improve the implant’s in vivo stability and inhibit capsular contracture [254,255,256,257].
Various polymers have been utilised in coating procedures with the sole aim of enhancing silicone material biocompatibility. PDMS displays high hydrophobicity, and this negatively affect cell adhesion and growth and, in most cases, makes surface modification a necessity. Natural polymers including collagen, gelatine and hyaluronic acid are very good examples [25, 274, 275] whilst synthetic polymers include poly-lactic acid (PLA), poly-glycolic acid and poly-lactic-co-glycolic acid (PLGA) [276, 277]. Natural polymers have several advantages over synthetic polymers including having excellent biocompatibility and functional groups relevant for biological processes, they suffer from poor tensile strength. To overcome poor tensile strength, natural polymers can be combined with synthetic polymers that display good mechanical strength. Below, we briefly describe the use of various biopolymers in modifying the surface of silicone implants and the biocompatibility of the resulting surfaces.
Collagen
The connective tissue has an ECM mainly composed of collagens [278,279,280]. Although close to 28 proteins have been identified to belong to the collagen family, most of the collagens in the body are types I, II and III collagens [279]. Type I collagen is the most used collagen for coating silicone implants partly due to it being the dominant collagen within connective tissue and has been linked to enhanced fibroblast proliferation [281,282,283]. Being non-toxic as well as being biodegradable makes type I collagen a suitable material for coating silicone implant surfaces. Since collagen is biodegradable, over time the coating on the implant surface will be depleted resulting in bare silicone implant interacting with tissue. However, as the degradation of collagen happens over time, we speculate that biointegration would have occurred by then. A recent study by Sharma and colleagues showed that grafting collagen to silicone by means of polydopamine as a conjugator enhanced hydrophilicity resulting in better mesenchymal stem cell adhesion [268]. In another study, Li and co-workers showed that coating PDMS with collagen and polydopamine increased its biocompatibility enabling long culture of fibroblasts [284]. Gao and colleagues utilised L-3,4-dihydroxyphenylalanine to covalently immobilise collagen on the PDMS surface. The modified PDMS surface showed enhanced wettability and biocompatibility [285].
Hyaluronic acid
Also referred to as hyaluronan, hyaluronic acid is a viscous polysaccharide that has been utilised as a viscoelastic material in many processes [286]. Various reports have shown that hyaluronic acid is biocompatible, promotes cell adhesion and proliferation, processes that are important after implantation of silicone implants [287, 288]. Xue and colleagues demonstrated that modifying the surface of PDMS with hyaluronic acid conjugated to polydopamine increased surface compatibility and this allowed the resulting material to be used in medical implants [271]. Hung and colleagues demonstrated modifying the surface of PDMS with dopamine and hyaluronic acid increased its biocompatibility and allowed enhanced mesenchymal stem cell differentiation [272]. In another study, Yue and colleagues utilised both hyaluronic acid and collagen type I to functionalise the PDMS surface resulting in increased pheochromocytoma cell proliferation and differentiation [289]. In this work, the authors conjugated type I collagen onto the hyaluronic acid-modified PDMS leading to promotion of cell-substrate interaction [289]. Hyaluronic acid can be degraded by hyaluronidases and its long-term presence on silicone implant in the body is not guaranteed in vivo [290]. Studies investigating long-term in vivo stability of hyaluronic acid coating on silicone implants are not available.
Gelatin
Derived from collagen, gelatine is a biodegradable natural polymer that exists as type A and type B gelatine [291]. Several studies have shown that gelatine is biocompatible and promotes cellular adhesion to surfaces hence its use in tissue culture [253, 292]. Importantly, gelatine contains various functional groups that allow for cross-linking with other materials for many applications. Ai and colleagues investigated the crosslinking of gelatine with glutaraldehyde on silicone surface and revealed that this resulted in enhanced endothelial cell proliferation and adhesion [253]. Liu used proanthocyanidin-crosslinked gelatin on a silicone tube to investigate nerve fibre regeneration [293]. This study demonstrated that the proanthocyanidin-crosslinked gelatine on silicone surface promoted Schwann cell growth and promoted peripheral nerve regeneration [293]. Since gelatin is biodegradable its presence on the modified silicone breast implant in the body is not assured. Future studies need to investigate this concern.
Poly-glycolic acid and poly-lactic-co-glycolic acid
Poly-glycolic acid (PGA) has excellent strength and display great hydrophilicity as a polymer. However, its biggest disadvantage is that PGA can easily degrade causing a local increase in glycolic acid, a by-product of the degradation process. Elevated levels of glycolic acid result in local tissue damage which is undesirable if used on silicone breast implants. Hatton and Brook investigated the utility of reinforced silicone and biodegradable PGA in an in vitro study using a rat bone cell culture model [294]. The results demonstrated the osteoinductive properties of both silicone and PGA with bone cells showing increased proliferation and bone-like tissue formation within the weave of the PGA membrane [294]. When PGA is mixed with poly-lactic acid, poly-lactic-co-glycolic acid (PLGA) is formed. By controlling the amounts of its monomers, it is easy to control the hydrophilicity of PLGA. In most cases, PLGA is blended with other materials to develop products useful for tissue regeneration by encouraging cell proliferation. For example, combining PLGA and silicone was shown to enhance endothelial and smooth muscle cell proliferation in vitro [295].
Poly-vinyl alcohol (PVA)
A water-soluble polymer used in many applications, PVA has been shown to irreversibly bind to PDMS [296]. Trantidou and colleagues grafted PVA to the surface of plasma-treated PDMS and demonstrated that PVA deposition enhances PDMS surface hydrophilicity for increased time (above 30 days) [262]. By combining PVA coating and nano-patterning of PDMS together with exposure to air plasma, Li and colleagues demonstrated that the resulting hydrophilic PDMS surface was stable and promoted cell growth [263]. Using PDMS as an anchor, Huang and colleagues demonstrated that 3T3 fibroblasts on PVA-gelatin modified surface spread easily and had normal spindle shape than fibroblasts on PVA modified surface [297].
2-hydroxyethylmethacrylate (HEMA), Oligo-ethylglycol-methylmethacrylate (OEGMA) and poly-ethylene glycol (PEG)
Most methods of chemical modification reported so far in order to improve wettability are laborious, and the final grafted surfaces are non-homogeneous which can affect the topography of silicone implants. Recently, Montoya-Villegas [220] introduced a method involving the use of reversible addition-fragmentation chain transfer (RAFT) to control graft distribution of HEMA and OEGMA on the surface of silicone rubber films oxidised with the γ-irradiation method. Their approach has potential in the modification of the wettability of silicone implants with control of grafting [220]. It has been shown that grafting hydrophilic groups increased the swelling of the modified PDMS leading to greater flexibility (low stiffness) in wet condition [220]. To improve the biocompatibility of silicone’s surface using PEG, Mikhail et al. [225] linked peptides and proteins to PEG and then introduced them to a pre-functionalised PDMS surface. Their method was reproducible, and the modified surface was durable [225].
Zwitterionic polymers
Zwitterionic materials with resistance to adhesion of bacteria and protein adsorption are the next generation of coating materials on silicone implants. They contain both positively and negatively charged groups, with water-binding capabilities, resulting in a highly hydrated surface [266]. Surface hydration is generally considered key to nonspecific protein adsorption resistance, as a tightly bound water layer forms a physical and energetic barrier to prevent protein adsorption to the surface [298, 299]. Moreover, zwitterionic polymers have strong salt bridge interactions, enhancing the coating’s stability [300]. Using 2-methacryloyloxyethyl phosphorylcholin, a zwitterionic PC-based polymer, Ham et al. [265] immobilised a durable coating on silicone breast implants which showed a significant decrease in the amount of inflammatory cytokines released by macrophages compare to uncoated implants. In addition, in vivo assessment of these coated implants showed a thinner, sparse capsule formation in a porcine model after six months implantation [265]. Hydrogel polymers are another possible option to improve the wettability of silicone using as a coating or composite with silicone rubber [264, 301]. Hydrogels entrap a high volume of water in their three-dimensional cross-linked network without dissolving in an aqueous solution. As a result, it has the potential to reduce foreign body reactions by decreasing protein adsorption on the surface [264].
Summary and perspectives
Breast augmentation is the most common plastic surgical procedure performed to correct breast abnormality for both cosmetic and oncologic reasons. One of the common materials used in breast implants is silicone due to its inherent properties including ease of fabrication, oxygen permeability, flexibility as well as low cost. However, most macro-textured and traditional smooth surfaced commercially available breast implants made from silicone have demonstrated limited biocompatibility. Thus, it is of great value to develop strategies to modify the properties of silicone surfaces to enhance the bio-integration of silicone breast implants. Silicone properties such as topography, stiffness, and wettability influence cell adhesion to the implant and therefore bio-integration. In this review, we provide a critical synthesis of advances in silicone surface modification techniques and strategies to enhance silicone breast implants biocompatibility. The review starts by discussing the biological processes involved when the implant is inserted into the breast. This is followed by the presentation of literature on the normal and aberrant formation of a capsule around the inserted silicone implant. Silicone implant fundamental properties that influence the formation of the capsule include topography and wettability. Various methods have been developed to modify the silicone implant surface properties including wettability and topography via chemical or physical means and this ultimately influence cell behaviour and tissue bio-integration. Whilst surface modification techniques such as UV/ozone and oxygen plasma activation are rapid and easy to use, they suffer from hydrophobic recovery. Current approaches overcome hydrophobic recovery through combining different modification techniques, in most cases involving a pre-treatment stage followed by a coating step. Natural polymers are an excellent choice for coating silicone surfaces as they mimic the natural ECM but suffer from lack of tensile strength. Synthetic polymers display great mechanical properties but suffer from lack of functional groups needed for interactions with cells and tissue. As shown in this review, recent work show that a combination of both natural and synthetic polymers may be the best way to overcome various challenges.
The work presented here demonstrates that following the insertion of a silicone implant into the breast cavity, the breast tissue undergoes repair. Soon after implant insertion the host tissue responds by the formation of a provisional matrix, initiation of acute inflammation, and finally fibrous capsule formation. Body fluids such as blood and wound fluid would soak the silicone implant first. Proteins within these fluids adsorb onto the implant surface. Typical proteins include vitronectin, collagens, albumin, and fibrinogen. The layer of proteins adsorbed onto the implant surface and the conformation of these proteins are influenced by implant surface properties such as surface topography and the hydrophilicity or hydrophobic nature of the implant surface. In addition, the adhesion of cells to the implant occurs via integrins interactions with the layer of proteins adsorbed on the implant.
Theories suggest that conditions such as ALCL may be caused by bacterial infection. Functionalisation of silicone implant surfaces via the use of UV/ozone and UV irradiation treatments adds reactive species on the surface of the implants rendering it unhabitable to bacteria. Coating the surfaces of silicone implants with various ECM proteins to modulate FBR and prevent pathological conditions such as ALCL is being investigated by various laboratories worldwide. In addition, the coating of silicone implant surfaces with nanoparticles is being investigated. New technologies including 3D printing can be harnessed to produce silicone surfaces with the right topography to modulate FBR and capsule formation after insertion of the implant.
Conclusions
Due to the inertness and other physical properties of silicone material, silicone implants may not integrate into the human body as well as other materials. To attach to the silicone implant, cells synthesize and release several biomolecules which adsorb onto the silicone surface, allowing cells to eventually bind to the implant. These adsorbed molecules thus influence gene expression, adhesion, proliferation, and spread of cells on the silicone surface. Several properties of the surface such as its roughness, wettability, and stiffness influence cellular adhesion and proliferation. Unmodified silicone material is highly hydrophobic and demonstrate poor cell adhesion and tissue biointegration. In turn, the amount and the conformation of the biomolecules adsorbed on the silicone implant surface can play a key role in determining the strength of cellular attachment to the silicone implant. The use of bio-mimetic engineered surfaces in addition to the presence of key biomolecules can help prevent complications such as capsular contracture and anaplastic large cell lymphoma formation. Future studies are needed to further study the influence of bio-inspired silicone implant surface modifications and their fate in vivo.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Change history
02 October 2023
A Correction to this paper has been published: https://doi.org/10.1186/s40824-023-00437-z
Abbreviations
- 3D:
-
Three-dimensional
- AA:
-
Alginic acid
- ALCL:
-
Anaplastic large cell lymphoma
- αMβ2:
-
Integrin alpha M beta-2
- αVβ1:
-
Integrin alpha V beta-1
- CCL2:
-
Chemokine C–C motif ligand 2
- CD:
-
Cluster of differentiation
- CMC:
-
Carboxymethyl cellulose
- CMD:
-
Carboxymethyl -1,3-dextran
- CXCL10:
-
Chemokine C-X-C motif chemokine ligand 10
- DAMPs:
-
Damage-associated molecular patterns
- E:
-
Elastic modulus
- ECM:
-
Extracellular matrix
- FBR:
-
Foreign body response
- FBGCS:
-
Foreign body giant cells
- FDA:
-
Food and Drug Administration
- HA:
-
Hyaluronic acid
- IgG:
-
Immunoglobulin G
- IL:
-
Interleukin
- ISAPS:
-
International Society of Aesthetic Plastic Surgery
- ISO:
-
International Organization for Standardization
- MCP-1:
-
Monocyte chemoattractant protein-1
- MIP-1a:
-
Macrophage inflammatory proteins 1a
- MKN:
-
Nε-myristoyl-lysine methyl ester
- MMP:
-
Matrix metallopeptidase
- NET:
-
Neutrophil extracellular traps
- OC:
-
Open cavities
- OEG:
-
Oligo (ethylene glycol)
- OEGMA:
-
Oligo (ethylene glycol) methyl ether methacrylate
- PAAm:
-
Poly(acrylamide)
- PC:
-
Phosphorylcholine
- pCBMA:
-
Poly carboxybetaine methacrylate
- PDGF:
-
Platelet-derived growth factor
- PDMS:
-
Polydimethylsiloxane
- PEG:
-
Poly (ethylene glycol)
- PEG-SBSi:
-
Polyethylene glycol sulfobetaine silane
- PEG-silane:
-
Methoxy(polyethyleneoxy) propyltrimethoxysilane
- PF4:
-
Platelets secrete platelet factor 4
- PGA:
-
Poly-glycolic acid
- PHEMA:
-
Poly (hydroxyethyl methacrylate)
- PHSRN:
-
Proline-histidine-serine-arginine-asparagine
- PLA:
-
Poly-lactic acid: PLGA: poly-lactic-co-glycolic acid
- PLL:
-
Poly-l-lysine
- PMAA:
-
Poly (methacrylic acid)
- PMNs:
-
Polymorphonuclear leukocytes
- PMPC:
-
Poly (2-methacryloyloxyethyl phosphorylcholine)
- polyNaSS:
-
Poly (Sodium Styrene Sulfonate)
- PV:
-
Peak and valley
- PVA:
-
Polyvinyl alcohol
- PVP:
-
Polyvinylpyrrolidone
- qPCR:
-
Quantitative polymerase chain reaction
- Ra:
-
Arithmetic mean height
- RAFT:
-
Reversible addition-fragmentation chain transfer
- RGD:
-
Arginine–glycine–asparagine
- SBSi:
-
Sulfobetaine silane
- Sku:
-
Kurtosis value
- SOC:
-
Semi-opened cavities
- Ssk:
-
Surface skewness
- TGF-β:
-
Transforming growth factor beta
- TIMP4:
-
Metalloproteinase inhibitor 4
- TNF-α:
-
Tumour necrosis factor α
- TNSFS11:
-
Tumour necrosis factor ligand superfamily member 11
- WHO:
-
World Health Organization
References
Jalalabadi F, Doval AF, Neese V, Andrews E, Spiegel AJ. Breast Implant Utilization Trends in USA versus Europe and the Impact of BIA-ALCL Publications. Plast Reconstr Surg Glob Open. 2021;9(3):e3449.
Surgery ISoAP. ISAPS international survey on aesthetic/cosmetic procedures performed in 2019. 2020.
Kaoutzanis C, Winocour J, Unger J, Gabriel A, Maxwell GP, editors. The evolution of breast implants. Semin Plast Surg. 2019;33(4):217–23. Thieme Medical Publishers.
Peters W. Current status of breast implant survival properties and the management of the woman with silicone gel breast implants. Can J Plastic Surg. 2000;8(2):54–67.
Choi J, Shin BH, Kim T, Lee JS, Kim S, Choy YB, et al. Micro-textured silicone-based implant fabrication using electrospun fibers as a sacrificial template to suppress fibrous capsule formation. Mater Sci Eng C Mater Biol Appl. 2022;135:112687.
Colaris MJL, de Boer M, van der Hulst RR, Cohen Tervaert JW. Two hundreds cases of ASIA syndrome following silicone implants: a comparative study of 30 years and a review of current literature. Immunol Res. 2017;65(1):120–8.
Bodin F, Jung C, Dieval F, Chakfe N, Wisniewski S, Bruant Rodier C, et al. Aging of retrieved gel breast implants: a comparison between two product generations. J Mech Behav Biomed Mater. 2015;46:11–22.
Stenzelius K, Laszlo L, Madeja M, Pessah-Rasmusson H, Grabe M. Catheter-associated urinary tract infections and other infections in patients hospitalized for acute stroke: A prospective cohort study of two different silicone catheters. Scandinavian journal of urology. 2016;50(6):483–8.
Daniels A. Silicone breast implant materials. Swiss Med Wkly. 2012;142(2930):w13614.
McDonald JC, Whitesides GM. Poly (dimethylsiloxane) as a material for fabricating microfluidic devices. Acc Chem Res. 2002;35(7):491–9.
Randall GC, Doyle PS. Permeation-driven flow in poly (dimethylsiloxane) microfluidic devices. Proc Natl Acad Sci. 2005;102(31):10813–8.
Qin X-H, Senturk B, Valentin J, Malheiro V, Fortunato G, Ren Q, et al. Cell-membrane-inspired silicone interfaces that mitigate proinflammatory macrophage activation and bacterial adhesion. Langmuir. 2018;35(5):1882–94.
Rufin MA, Ngo BKD, Barry ME, Page VM, Hawkins ML, Stafslien SJ, et al. Antifouling silicones based on surface-modifying additive amphiphiles. Green Mater. 2017;5(1):4–13.
James GA, Boegli L, Hancock J, Bowersock L, Parker A, Kinney BM. Bacterial adhesion and biofilm formation on textured breast implant shell materials. Aesthetic Plast Surg. 2019;43(2):490–7.
Doloff JC, Veiseh O, de Mezerville R, Sforza M, Perry TA, Haupt J, et al. The surface topography of silicone breast implants mediates the foreign body response in mice, rabbits and humans. Nat Biomed Eng. 2021;5(10):1115–30.
Bae H-S, Son H-Y, Lee JP, Chang H, Park J-U. The Role of Periostin in Capsule Formation on Silicone Implants. Biomed Res Int. 2018;2018:3167037.
Barr S, Hill E, Bayat A. Functional biocompatibility testing of silicone breast implants and a novel classification system based on surface roughness. J Mech Behav Biomed Mater. 2017;75:75–81.
Kyle DJ, Oikonomou A, Hill E, Bayat A. Development and functional evaluation of biomimetic silicone surfaces with hierarchical micro/nano-topographical features demonstrates favourable in vitro foreign body response of breast-derived fibroblasts. Biomaterials. 2015;52:88–102.
Valencia-Lazcano AA, Alonso-Rasgado T, Bayat A. Characterisation of breast implant surfaces and correlation with fibroblast adhesion. J Mech Behav Biomed Mater. 2013;21:133–48.
Barr S, Hill E, Bayat A. Patterning of novel breast implant surfaces by enhancing silicone biocompatibility, using biomimetic topographies. Eplasty. 2010;10:e31.
Chung L, Maestas DR, Lebid A, Mageau A, Rosson GD, Wu X, et al. Interleukin 17 and senescent cells regulate the foreign body response to synthetic material implants in mice and humans. Science Translational Medicine. 2020;12(539):eaax3799.
Atlan M, Nuti G, Wang H, Decker S, Perry T. Breast implant surface texture impacts host tissue response. J Mech Behav Biomed Mater. 2018;88:377–85.
Cappellano G, Ploner C, Lobenwein S, Sopper S, Hoertnagl P, Mayerl C, et al. Immunophenotypic characterization of human T cells after in vitro exposure to different silicone breast implant surfaces. PLoS ONE. 2018;13(2):e0192108.
Lee SD, Yi M-H, Kim DW, Lee Y, Choi Y, Oh S-H. The effect of botulinum neurotoxin type A on capsule formation around silicone implants: the in vivo and in vitro study. Int Wound J. 2016;13(1):65–71.
Valencia-Lazcano AA, Alonso-Rasgado T, Bayat A. Physico-chemical characteristics of coated silicone textured versus smooth breast implants differentially influence breast-derived fibroblast morphology and behaviour. J Mech Behav Biomed Mater. 2014;40:140–55.
MendonçaMunhoz A, Santanelli di Pompeo F, De Mezerville R. Nanotechnology, nanosurfaces and silicone gel breast implants: current aspects. Case Reports Plast Surg Hand Surg. 2017;4(1):99–113.
Noskovicova N, Hinz B, Pakshir P. Implant Fibrosis and the Underappreciated Role of Myofibroblasts in the Foreign Body Reaction. Cells. 2021;10(7):1794.
Brigaud I, Garabédian C, Bricout N, Pieuchot L, Ponche A, Deltombe R, et al. Surface Texturization of Breast Implants Impacts Extracellular Matrix and Inflammatory Gene Expression in Asymptomatic Capsules. Plast Reconstr Surg. 2020;145(3):542e-e551.
Cronin TD, Gerow FJ. Augmentation mammaplasty: a new “natural feel” prothesis. Transactions of the Third International Congress of Plastic and Reconstructive Surgery, Washington, 1963. Amsterdam: Excerpta Medica; 1963. p. 41–9.
Cronin TD, Greenberg RL. Our experiences with the silastic gel breast prosthesis. Plast Reconstr Surg. 1970;46(1):1–7.
Brandt B, Breiting V, Christensen L, Nielsen M, Thomsen J. Five years experience of breast augmentation using silicone gel prostheses with emphasis on capsule shrinkage. Scand J Plast Reconstr Surg. 1984;18(3):311–6.
Barker DE, Retsky MI, Schultz S. “ Bleeding” of silicone from bag-gel breast implants, and its clinical relation to fibrous capsule reaction. Plast Reconstr Surg. 1978;61(6):836–41.
Price JE, Barker DE. Initial clinical experience with “low bleed” breast implants. Aesthetic Plast Surg. 1983;7(4):255–6.
Barker DE, Retsky M, Searles SL. New low-bleed implant—Silastic II. Aesthetic Plast Surg. 1985;9(1):39–41.
Hartley JH. Specific applications of the double lumen prosthesis. Clin Plast Surg. 1976;3(2):247–63.
Colon GA. The reverse double-lumen prosthesis–a preliminary report. Ann Plast Surg. 1982;9(4):293–7.
Stevens WG, Calobrace MB, Alizadeh K, Zeidler KR, Harrington JL, d’Incelli RC. Ten-year core study data for Sientra’s food and drug administration-approved round and shaped breast implants with cohesive silicone gel. Plast Reconstr Surg. 2018;141(4S):7S-19S.
Hammond DC, Canady JW, Love TR, Wixtrom RN, Caplin DA. Mentor contour profile gel implants: clinical outcomes at 10 years. Plast Reconstr Surg. 2017;140(6):1142–50.
Spear SL, Murphy DK. Natrelle round silicone breast implants: core study results at 10 years. Plast Reconstr Surg. 2014;133(6):1354.
Spear SL, Murphy DK, Slicton A, Walker PS, Group ISBIUS. Inamed silicone breast implant core study results at 6 years. Plast Reconstr Surg. 2007;120(7):8S-16S.
Chandorkar Y, Basu B. The foreign body response demystified. ACS Biomater Sci Eng. 2018;5(1):19–44.
Anderson JM, Jiang S. Implications of the acute and chronic inflammatory response and the foreign body reaction to the immune response of implanted biomaterials. The Immune Response to Implanted Materials and Devices: Springer; 2017. p. 15–36.
Bazira PJ, Ellis H, Mahadevan V. Anatomy and physiology of the breast. Surg Infect (Larchmt). 2022;40(2):79–83.
McGuire KP. Breast Anatomy and Physiology. In: Aydiner A, İğci A, Soran A, editors. Breast Disease: Diagnosis and Pathology. Cham: Springer International Publishing; 2016. p. 1–14.
Aftab Z, Wladis A. Skandalakis’ Surgical Anatomy: the Embryology and Anatomic Basis of Modern Surgery. Sultan Qaboos Univ Med J. 2008;8(1):97–8.
Pandya S, Moore RG. Breast development and anatomy. Clin Obstet Gynecol. 2011;54(1):91–5.
Macias H, Hinck L. Mammary gland development. Wiley Interdiscip Rev Dev Biol. 2012;1(4):533–57.
Hidalgo DA. Breast augmentation: choosing the optimal incision, implant, and pocket plane. Plast Reconstr Surg. 2000;105(6):2202–16.
Henriksen TF, Fryzek JP, Hölmich LR, McLaughlin JK, Kjøller K, Høyer AP, et al. Surgical intervention and capsular contracture after breast augmentation: a prospective study of risk factors. Ann Plast Surg. 2005;54(4):343–51.
Costa L, Bracco P, Del Prever EB, Luda M, Trossarelli L. Analysis of products diffused into UHMWPE prosthetic components in vivo. Biomaterials. 2001;22(4):307–15.
Romero-Gavilán F, Gomes N, Ródenas J, Sánchez A, Azkargorta M, Iloro I, et al. Proteome analysis of human serum proteins adsorbed onto different titanium surfaces used in dental implants. Biofouling. 2017;33(1):98–111.
Zreiqat H, Howlett C, Zannettino A, Evans P, Schulze-Tanzil G, Knabe C, et al. Mechanisms of magnesium-stimulated adhesion of osteoblastic cells to commonly used orthopaedic implants. J Biomed Mater Res. 2002;62(2):175–84.
Healy KE, Ducheyne P. Hydration and preferential molecular adsorption on titanium in vitro. Biomaterials. 1992;13(8):553–61.
Williams D, Askill I, Smith R. Protein adsorption and desorption phenomena on clean metal surfaces. J Biomed Mater Res. 1985;19(3):313–20.
Vroman L, Adams AL. Findings with the recording ellipsometer suggesting rapid exchange of specific plasma proteins at liquid/solid interfaces. Surf Sci. 1969;16:438–46.
Vroman L, Adams AL. Identification of rapid changes at plasma–solid interfaces. J Biomed Mater Res. 1969;3(1):43–67.
Schmidt DR, Waldeck H, Kao WJ. Protein adsorption to biomaterials. Biological interactions on materials surfaces: Springer; 2009. p. 1–18.
Dee KC, Puleo DA. Bizios R. Protein-Surface Interactions. In: Dee KC, Puleo DA, Bizios R, editors. An Introduction To Tissue-Biomaterial Interactions: Wiley; 2002; p. 37–52. https://doi.org/10.1002/0471270598.ch3.
Hirsh SL, McKenzie DR, Nosworthy NJ, Denman JA, Sezerman OU, Bilek MM. The Vroman effect: competitive protein exchange with dynamic multilayer protein aggregates. Colloids Surf, B. 2013;103:395–404.
Latour RA. Biomaterials: protein-surface interactions. Biomed Mater. 2005;1:270–8.
Barr SP, Hill EW, Bayat A. Novel proteomic assay of breast implants reveals proteins with significant binding differences: implications for surface coating and biocompatibility. Aesthetic Surg J. 2018;38(9):962–9.
Horbett TA. Fibrinogen adsorption to biomaterials. J Biomed Mater Res, Part A. 2018;106(10):2777–88.
Ruoslahti E, Pierschbacher MD. New perspectives in cell adhesion: RGD and integrins. Science. 1987;238(4826):491–7.
Rahmany MB, Van Dyke M. Biomimetic approaches to modulate cellular adhesion in biomaterials: A review. Acta Biomater. 2013;9(3):5431–7.
Ekdahl KN, Hong J, Hamad OA, Larsson R, Nilsson B. Evaluation of the blood compatibility of materials, cells, and tissues: basic concepts, test models, and practical guidelines. Complement Therapeutics: Springer; 2013. p. 257–70.
Tang L, Eaton JW. Fibrin (ogen) mediates acute inflammatory responses to biomaterials. J Exp Med. 1993;178(6):2147–56.
Zdolsek J, Eaton JW, Tang L. Histamine release and fibrinogen adsorption mediate acute inflammatory responses to biomaterial implants in humans. J Transl Med. 2007;5(1):31.
Hsieh JY, Smith TD, Meli VS, Tran TN, Botvinick EL, Liu WF. Differential regulation of macrophage inflammatory activation by fibrin and fibrinogen. Acta Biomater. 2017;47:14–24.
Voskerician G, Anderson J. Sensor Biocompatibility and Biofouling in Real-Time Monitoring. In: Akay M, editor. Wiley Encyclopedia of Biomedical Engineering; 2006. https://doi.org/10.1002/9780471740360.ebs1370.
Clark RAF. Wound Repair. In: Clark RAF, editor. The Molecular and Cellular Biology of Wound Repair. Boston: Springer, US; 1988. p. 3–50.
Kono H, Rock KL. How dying cells alert the immune system to danger. Nat Rev Immunol. 2008;8(4):279–89.
Harvath L. Neutrophil chemotactic factors. Cell Motility Factors: Springer; 1991. p. 35–52.
Deuel TF, Senior RM, Chang D, Griffin GL, Heinrikson RL, Kaiser ET. Platelet factor 4 is chemotactic for neutrophils and monocytes. Proc Natl Acad Sci. 1981;78(7):4584–7.
Ghasemzadeh M, Kaplan ZS, Alwis I, Schoenwaelder SM, Ashworth KJ, Westein E, et al. The CXCR1/2 ligand NAP-2 promotes directed intravascular leukocyte migration through platelet thrombi. Blood. 2013;121(22):4555–66.
Hantash BM, Zhao L, Knowles JA, Lorenz HP. Adult and fetal wound healing. Front Biosci. 2008;13(1):51–61.
Abaricia JO, Shah AH, Olivares-Navarrete R. Substrate stiffness induces neutrophil extracellular trap (NET) formation through focal adhesion kinase activation. Biomaterials. 2021;271:120715.
Meszaros AJ, Reichner JS, Albina JE. Macrophage phagocytosis of wound neutrophils. J Leukoc Biol. 1999;65(1):35–42.
Meszaros AJ, Reichner JS, Albina JE. Macrophage-induced neutrophil apoptosis. J Immunol. 2000;165(1):435–41.
Henson PM. The immunologic release of constituents from neutrophil leukocytes: I. The role of antibody and complement on nonphagocytosable surfaces or phagocytosable particles. J Immunol. 1971;107(6):1535–46.
Henson PM. The immunologic release of constituents from neutrophil leukocytes: II. Mechanisms of release during phagocytosis, and adherence to nonphagocytosable surfaces. J Immunol. 1971;107(6):1547–57.
Nour S, Baheiraei N, Imani R, Rabiee N, Khodaei M, Alizadeh A, et al. Bioactive materials: a comprehensive review on interactions with biological microenvironment based on the immune response. J Bionic Eng. 2019;16(4):563–81.
Anderson JM. Biological responses to materials. Annu Rev Mater Res. 2001;31(1):81–110.
McNally AK, Jones JA, MacEwan SR, Colton E, Anderson JM. Vitronectin is a critical protein adhesion substrate for IL-4-induced foreign body giant cell formation. J Biomed Mater Res A. 2008;86(2):535–43.
Xia Z, Triffitt JT. A review on macrophage responses to biomaterials. Biomed Mater. 2006;1(1):R1.
DeFife KM, Jenney CR, Colton E, Anderson JM. Cytoskeletal and adhesive structural polarizations accompany IL-13-induced human macrophage fusion. J Histochem Cytochem. 1999;47(1):65–74.
DeFife KM, Jenney CR, McNally AK, Colton E, Anderson JM. Interleukin-13 induces human monocyte/macrophage fusion and macrophage mannose receptor expression. J Immunol. 1997;158(7):3385–90.
McNally AK, Anderson JM. Interleukin-4 induces foreign body giant cells from human monocytes/macrophages. Differential lymphokine regulation of macrophage fusion leads to morphological variants of multinucleated giant cells. Am J Pathol. 1995;147(5):1487.
Brodbeck WG, MacEwan M, Colton E, Meyerson H, Anderson JM. Lymphocytes and the foreign body response: lymphocyte enhancement of macrophage adhesion and fusion. J Biomed Mater Res A. 2005;74(2):222–9.
Helming L, Gordon S. Molecular mediators of macrophage fusion. Trends Cell Biol. 2009;19(10):514–22.
Dolores W, Christian R, Harald N, Hildegunde P, Georg W. Cellular and molecular composition of fibrous capsules formed around silicone breast implants with special focus on local immune reactions. J Autoimmun. 2004;23(1):81–91.
Major MR, Wong VW, Nelson ER, Longaker MT, Gurtner GC. The foreign body response: at the interface of surgery and bioengineering. Plast Reconstr Surg. 2015;135(5):1489–98.
Anderson JM. In vitro and in vivo monocyte, macrophage, foreign body giant cell, and lymphocyte interactions with biomaterials. Biological interactions on materials surfaces: Springer; 2009. p. 225–44.
Guo X, Hutcheon AE, Melotti SA, Zieske JD, Trinkaus-Randall V, Ruberti JW. Morphologic characterization of organized extracellular matrix deposition by ascorbic acid–stimulated human corneal fibroblasts. Invest Ophthalmol Vis Sci. 2007;48(9):4050–60.
Walboomers X, Croes H, Ginsel L, Jansen J. Contact guidance of rat fibroblasts on various implant materials. J Biomed Mater Res. 1999;47(2):204–12.
Burkhardt MA, Waser J, Milleret V, Gerber I, Emmert MY, Foolen J, et al. Synergistic interactions of blood-borne immune cells, fibroblasts and extracellular matrix drive repair in an in vitro peri-implant wound healing model. Sci Rep. 2016;6(1):1–15.
Feller L, Jadwat Y, Khammissa RA, Meyerov R, Schechter I, Lemmer J. Cellular responses evoked by different surface characteristics of intraosseous titanium implants. BioMed Res Int. 2015;2015:171945.
Liao H, Munoz-Pinto D, Qu X, Hou Y, Grunlan MA, Hahn MS. Influence of hydrogel mechanical properties and mesh size on vocal fold fibroblast extracellular matrix production and phenotype. Acta Biomater. 2008;4(5):1161–71.
Anderson JM, Rodriguez A, Chang DT. Foreign body reaction to biomaterials. Semin Immunol. 2008;20(2):86–100.
Gabbiani G. The myofibroblast in wound healing and fibrocontractive diseases. J Pathol. 2003;200(4):500–3.
Akilbekova D, Bratlie KM. Quantitative characterization of collagen in the fibrotic capsule surrounding implanted polymeric microparticles through second harmonic generation imaging. PLoS ONE. 2015;10(6):e0130386.
Chavrier C, Couble M, Hartmann D. Qualitative study of collagenous and noncollagenous glycoproteins of the human healthy keratinized mucosa surrounding implants. Clin Oral Implant Res. 1994;5(3):117–24.
Vistnes LM, Ksander GA, Kosek J. Study of encapsulation of silicone rubber implants in animals. A foreign-body reaction. Plast Reconstr Surg. 1978;62(4):580–8.
Bui JM, Perry T, Ren CD, Nofrey B, Teitelbaum S, Van Epps DE. Histological characterization of human breast implant capsules. Aesthetic Plast Surg. 2015;39(3):306–15.
Glicksman CA, Danino MA, Efanov JI, El Khatib A, Nelea M. A step forward toward the understanding of the long-term pathogenesis of double capsule formation in Macrotextured implants: a prospective histological analysis. Aesthet Surg J. 2019;39(11):1191–9.
Zhou X, Zhou X, Yan R, Shi X, Du Y, Chen Y, et al. Co-effects of C/Ag dual ion implantation on enhancing antibacterial ability and biocompatibility of silicone rubber. Biomed Mater. 2020;15(6):065003.
Lam M, Migonney V, Falentin-Daudre C. Review of silicone surface modification techniques and coatings for antibacterial/antimicrobial applications to improve breast implant surfaces. Acta Biomater. 2021;121:68–88.
Patel BC, Wong CS, Wright T, Schaffner AD. Breast Implants. 2017.
Nelson JA, McCarthy C, Dabic S, Polanco T, Chilov M, Mehrara BJ, et al. BIA-ALCL and textured breast implants: a systematic review of evidence supporting surgical risk management strategies. Plast Reconstr Surg. 2021;147(5s):7s–13s.
Deva AK, Adams WP Jr, Vickery K. The role of bacterial biofilms in device-associated infection. Plast Reconstr Surg. 2013;132(5):1319–28.
Crowe SA, Simister RL, Spence JS, Kenward PA, Van Slyke AC, Lennox P, et al. Microbial community compositions in breast implant biofilms associated with contracted capsules. PLoS ONE. 2021;16(4):e0249261.
Khavanin N, Clemens MW, Pusic AL, Fine NA, Hamill JB, Kim HM, et al. Shaped versus round implants in breast reconstruction: a multi-institutional comparison of surgical and patient-reported outcomes. Plast Reconstr Surg. 2017;139(5):1063.
Sforza M, Zaccheddu R, Alleruzzo A, Seno A, Mileto D, Paganelli A, et al. Preliminary 3-year evaluation of experience with SilkSurface and VelvetSurface Motiva silicone breast implants: a single-center experience with 5813 consecutive breast augmentation cases. Aesthetic Surg J. 2018;38(suppl_2):S62–73.
Clemens MW, Jacobsen ED, Horwitz SM. 2019 NCCN consensus guidelines on the diagnosis and treatment of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL). Aesthetic Surg J. 2019;39(Supplement_1):S3–13.
McCarthy CM, Loyo-Berríos N, Qureshi AA, Mullen E, Gordillo G, Pusic AL, et al. Patient registry and outcomes for breast implants and anaplastic large cell lymphoma etiology and epidemiology (PROFILE): initial report of findings, 2012–2018. Plast Reconstr Surg. 2019;143(3S):65S-73S.
Burkhardt B, Dempsey P, Schnur P, Tofield J. Capsular contracture: a prospective study of the effect of local antibacterial agents. Plast Reconstr Surg. 1986;77(6):919–32.
Adams WP Jr. Capsular contracture: what is it? What causes it? How can it be prevented and managed? Clin Plast Surg. 2009;36(1):119–26.
Klopfleisch R, Jung F. The pathology of the foreign body reaction against biomaterials. J Biomed Mater Res Part A. 2017;105(3):927–40.
Anderson JM, Jiang S. Implications of the Acute and Chronic Inflammatory Response and the Foreign Body Reaction to the Immune Response of Implanted Biomaterials. In: Corradetti B, editor. The Immune Response to Implanted Materials and Devices: The Impact of the Immune System on the Success of an Implant. Cham: Springer International Publishing; 2017. p. 15–36.
Castner DG, Ratner BD. Biomedical surface science: Foundations to frontiers. Surf Sci. 2002;500(1):28–60.
Cook PD, Osborne BM, Connor RL, Strauss JF. Follicular lymphoma adjacent to foreign body granulomatous inflammation and fibrosis surrounding silicone breast prosthesis. Am J Surg Pathol. 1995;19(6):712–7.
Foster TJ, Geoghegan JA, Ganesh VK, Höök M. Adhesion, invasion and evasion: the many functions of the surface proteins of Staphylococcus aureus. Nat Rev Microbiol. 2014;12(1):49–62.
Burkhardt BR. Capsular contracture: hard breasts, soft data. Clin Plast Surg. 1988;15(4):521–32.
Becker H, Springer R. Prevention of capsular contracture. Plast Reconstr Surg. 1999;103(6):1766–8.
Rohrich RJ, Kenkel JM, Adams WP. Preventing capsular contracture in breast augmentation: in search of the Holy Grail. Plast Reconstr Surg. 1999;103(6):1759–60.
Poeppl N, Schreml S, Lichtenegger F, Lenich A, Eisenmann-Klein M, Prantl L. Does the surface structure of implants have an impact on the formation of a capsular contracture? Aesthetic Plast Surg. 2007;31(2):133–9.
Hakelius L, Ohlsén L. A clinical comparison of the tendency to capsular contracture between smooth and textured gel-filled silicone mammary implants. Plast Reconstr Surg. 1992;90(2):247–54.
Spear SL, Baker JL Jr. Classification of capsular contracture after prosthetic breast reconstruction. Plast Reconstr Surg. 1995;96(5):1119–23 discussion 24.
Zahavi A, Sklair ML, Ad-El DD. Capsular contracture of the breast: working towards a better classification using clinical and radiologic assessment. Ann Plast Surg. 2006;57(3):248–51.
Malata CM, Varma S, Scott M, Liston JC, Sharpe DT. Silicone breast implant rupture: common/serious complication? Med Prog Technol. 1994;20(3–4):251–60.
Maxwell GP, Gabriel A. The evolution of breast implants. Clin Plast Surg. 2009;36(1):1–13, v.
O’Shaughnessy K. Evolution and update on current devices for prosthetic breast reconstruction. Gland Surg. 2015;4(2):97–110.
Malata CM, Feldberg L, Coleman DJ, Foo IT, Sharpe DT. Textured or smooth implants for breast augmentation? Three year follow-up of a prospective randomised controlled trial. Br J Plast Surg. 1997;50(2):99–105.
Namnoum JD, Largent J, Kaplan HM, Oefelein MG, Brown MH. Primary breast augmentation clinical trial outcomes stratified by surgical incision, anatomical placement and implant device type. J Plast Reconstr Aesthet Surg. 2013;66(9):1165–72.
Brorson F, Thorarinsson A, Kölby L, Elander A, Hansson E. Early complications in delayed breast reconstruction: a prospective, randomized study comparing different reconstructive methods in radiated and non-radiated patients. Eur J Surg Oncol. 2020;46(12):2208–17.
Sgarzani R, Pasquali S, Buggi F, Tognali D, Marongiu F, Mingozzi M, et al. Sub-muscular reconstruction after NAC sparing mastectomy: direct to implant breast reconstruction with human ADM versus tissue expander. Aesthetic Plast Surg. 2021;45(2):413–20.
Barnsley GP, Sigurdson LJ, Barnsley SE. Textured surface breast implants in the prevention of capsular contracture among breast augmentation patients: a meta-analysis of randomized controlled trials. Plast Reconstr Surg. 2006;117(7):2182–90.
Wong C-H, Samuel M, Tan B-K, Song C. Capsular contracture in subglandular breast augmentation with textured versus smooth breast implants: a systematic review. Plast Reconstr Surg. 2006;118(5):1224–36.
Ono MT, Karner BM. Four-step augmentation mastopexy: Lift and Augmentation at Single Time (LAST). Plast Reconstr Surg Glob Open. 2019;7(11):e2523.
Coleman DJ, Foo IT, Sharpe DT. Textured or smooth implants for breast augmentation? A prospective controlled trial. Br J Plast Surg. 1991;44(6):444–8.
Asplund O, Gylbert L, Jurell G, Ward C. Textured or smooth implants for submuscular breast augmentation: a controlled study. Plast Reconstr Surg. 1996;97(6):1200–6.
Hakelius L, Ohlsén L. Tendency to capsular contracture around smooth and textured gel-filled silicone mammary implants: a five-year follow-up. Plast Reconstr Surg. 1997;100(6):1566–9.
Food U, Administration D. Anaplastic large cell lymphoma (ALCL) in women with breast implants: Preliminary FDA findings and analyses. MD: Center for Devices and Radiological Health Silver Spring; 2011.
Stein H, Foss HD, Dürkop H, Marafioti T, Delsol G, Pulford K, et al. CD30(+) anaplastic large cell lymphoma: a review of its histopathologic, genetic, and clinical features. Blood. 2000;96(12):3681–95.
Groth AK, Graf R. Breast implant-associated anaplastic large cell lymphoma (BIA-ALCL) and the textured breast implant crisis. Aesthetic Plast Surg. 2020;44(1):1–12.
Loch-Wilkinson A, Beath KJ, Knight RJW, Wessels WLF, Magnusson M, Papadopoulos T, et al. Breast implant–associated anaplastic large cell lymphoma in Australia and New Zealand: high-surface-area textured implants are associated with increased risk. Plast Reconstr Surg. 2017;140(4):645–54.
Dixon JM, Clemens M. Breast implants and anaplastic large cell lymphoma. Bmj. 2018;363:k5054.
Doren EL, Miranda RN, Selber JC, Garvey PB, Liu J, Medeiros LJ, et al. U.S. epidemiology of breast implant-associated anaplastic large cell lymphoma. Plast Reconstr Surg. 2017;139(5):1042–50.
Bishara MR, Ross C, Sur M. Primary anaplastic large cell lymphoma of the breast arising in reconstruction mammoplasty capsule of saline filled breast implant after radical mastectomy for breast cancer: an unusual case presentation. Diagn Pathol. 2009;4:11.
Clemens MW, Brody GS, Mahabir RC, Miranda RN. How to diagnose and treat breast implant-associated anaplastic large cell lymphoma. Plast Reconstr Surg. 2018;141(4):586e-e599.
Deva AK, Turner SD, Kadin ME, Magnusson MR, Prince HM, Miranda RN, et al. Etiology of Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL): Current Directions in Research. Cancers (Basel). 2020;12(12):3861.
Hu H, Johani K, Almatroudi A, Vickery K, Van Natta B, Kadin ME, et al. Bacterial biofilm infection detected in breast implant–associated anaplastic large-cell lymphoma. Plast Reconstr Surg. 2016;137(6):1659–69.
Walker JN, Hanson BM, Pinkner CL, Simar SR, Pinkner JS, Parikh R, et al. Insights into the microbiome of breast implants and periprosthetic tissue in breast implant-associated anaplastic large cell lymphoma. Sci Rep. 2019;9(1):1–12.
Hu H, Jacombs A, Vickery K, Merten SL, Pennington DG, Deva AK. Chronic biofilm infection in breast implants is associated with an increased T-cell lymphocytic infiltrate: implications for breast implant–associated lymphoma. Plast Reconstr Surg. 2015;135(2):319–29.
Lajevardi SS, Rastogi P, Isacson D, Deva AK. What are the likely causes of breast implant associated anaplastic large cell lymphoma (BIA-ALCL)? JPRAS open. 2022;32:34–42.
Collett DJ, Rakhorst H, Lennox P, Magnusson M, Cooter R, Deva AK. Current risk estimate of breast implant–associated anaplastic large cell lymphoma in textured breast implants. Plast Reconstr Surg. 2019;143(3S):30S-40S.
Lineaweaver WC. Breast implant–associated anaplastic large cell lymphoma and textured breast implants. Ann Plast Surg. 2019;82(6):595–6.
Rondón-Lagos M, Rangel N, Camargo-Villalba G, Forero-Castro M. Biological and genetic landscape of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL). Eur J Surg Oncol. 2021;47(5):942–51.
Deva AK, Turner SD, Kadin ME, Magnusson MR, Prince HM, Miranda RN, et al. Etiology of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL): current directions in research. Cancers. 2020;12(12):3861.
Turton P, El-Sharkawi D, Lyburn I, Sharma B, Mahalingam P, Turner SD, et al. UK Guidelines on the Diagnosis and Treatment of Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL) on behalf of the Medicines and Healthcare products Regulatory Agency (MHRA) Plastic, Reconstructive and Aesthetic Surgery Expert Advisory Group (PRASEAG). J Plast Reconstr Aesthet Surg. 2021;74(1):13–29.
Collins MS, Miranda RN, Medeiros LJ, Silva de Meneses MP, Iyer SP, Butler CE, et al. Characteristics and Treatment of Advanced Breast Implant-Associated Anaplastic Large Cell Lymphoma. Plast Reconstr Surg. 2019;143(3S A Review of Breast Implant-Associated Anaplastic Large Cell Lymphoma):41s–50s.
Hwang MJ, Brown H, Murrin R, Momtahan N, Sterne GD. Breast implant-associated anaplastic large cell lymphoma: a case report and literature review. Aesthetic Plast Surg. 2015;39(3):391–5.
Lechner MG, Lade S, Liebertz DJ, Prince HM, Brody GS, Webster HR, et al. Breast implant-associated, ALK-negative, T-cell, anaplastic, large-cell lymphoma: establishment and characterization of a model cell line (TLBR-1) for this newly emerging clinical entity. Cancer. 2011;117(7):1478–89.
Kadin ME, Deva A, Xu H, Morgan J, Khare P, MacLeod RA, et al. Biomarkers provide clues to early events in the pathogenesis of breast implant-associated anaplastic large cell Lymphoma. Aesthet Surg J. 2016;36(7):773–81.
Lechner MG, Megiel C, Church CH, Angell TE, Russell SM, Sevell RB, et al. Survival signals and targets for therapy in breast implant-associated ALK–anaplastic large cell lymphoma. Clin Cancer Res. 2012;18(17):4549–59.
Grivennikov S, Karin M. Autocrine IL-6 signaling: a key event in tumorigenesis? Cancer Cell. 2008;13(1):7–9.
DeCoster RC, Clemens MW, Di Napoli A, Lynch EB, Bonaroti AR, Rinker BD, et al. Cellular and molecular mechanisms of breast implant-associated anaplastic large cell lymphoma. Plast Reconstr Surg. 2021;147(1):30e–41e.
Ratner BD, Bryant SJ. Biomaterials: where we have been and where we are going. Annu Rev Biomed Eng. 2004;6:41–75.
Wang MY, Chen C, Gao XZ, Li J, Yue J, Ling F, et al. Distribution of Helicobacter pylori virulence markers in patients with gastroduodenal diseases in a region at high risk of gastric cancer. Microb Pathog. 2013;59–60:13–8.
Narayana P, Srihari P. Biofilm resistant surfaces and coatings on implants: A review. Materials Today: Proceedings. 2019;18:4847–53.
Ferreri AJ, Govi S, Pasini E, Mappa S, Bertoni F, Zaja F, et al. Chlamydophila psittaci eradication with doxycycline as first-line targeted therapy for ocular adnexae lymphoma: final results of an international phase II trial. J Clin Oncol. 2012;30(24):2988–94.
Munhoz AM, Clemens MW, Nahabedian MY. Breast Implant Surfaces and Their Impact on Current Practices: Where We Are Now and Where Are We Going? Plast Reconstr Surg Glob Open. 2019;7(10): e2466.
Turner SD. The Cellular Origins of Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL): Implications for Immunogenesis. Aesthet Surg J. 2019;39(Suppl_1):S21-s7.
Kearns V, McMurray R, Dalby M. Biomaterial surface topography to control cellular response: technologies, cell behaviour and biomedical applications. Surface modification of biomaterials: Elsevier; 2011. p. 169–201.
Danino A, Rocher F, Blanchet-Bardon C, Revol M, Servant JM. A scanning electron microscopy study of the surface of porous-textured breast implants and their capsules. Description of the “velcro” effect of porous-textured breast prostheses. Ann Chir Plast Esthet. 2001;46(1):23–30.
Pangman WJ. Compound prosthesis. Google Patents; Filed 1968, Ser. No. 768,315 Int, C. A41c3/00 A61f1/001968. 3,559,214. Patented Feb. 2, 1971.
Herman S. The Même implant. Plast Reconstr Surg. 1984;73(3):411–4.
Castel N, Soon-Sutton T, Deptula P, Flaherty A, Parsa FD. Polyurethane-coated breast implants revisited: a 30-year follow-up. Arch Plast Surg. 2015;42(2):186–93.
Benoit FM. Degradation of polyurethane foams used in the Même breast implant. J Biomed Mater Res. 1993;27(10):1341–8.
Barr S, Hill E, Bayat A. Current implant surface technology: an examination of their nanostructure and their influence on fibroblast alignment and biocompatibility. Eplasty. 2009;9:e22.
Ersek R. Molecular impact surface textured implants (MISTI) alter beneficially breast capsule formation at 36 months. J Long Term Eff Med Implants. 1991;1(2):155–69.
Brohim RM, Foresman PA, Hildebrandt PK, Rodeheaver GT. Early tissue reaction to textured breast implant surfaces. Ann Plast Surg. 1992;28(4):354–62.
Carpaneda CA. Inflammatory reaction and capsular contracture around smooth silicone implants. Aesthetic Plast Surg. 1997;21(2):110–4.
Wyatt LE, Sinow JD, Wollman JS, Sami DA, Miller TA. The influence of time on human breast capsule histology: smooth and textured silicone-surfaced implants. Plast Reconstr Surg. 1998;102(6):1922–31.
Bern S, Burd A, May JW Jr. The biophysical and histologic properties of capsules formed by smooth and textured silicone implants in the rabbit. Plast Reconstr Surg. 1992;89(6):1037–42 discussion 43.
Stevens WG, Pacella SJ, Gear AJ, Freeman ME, McWhorter C, Tenenbaum MJ, et al. Clinical experience with a fourth-generation textured silicone gel breast implant: a review of 1012 Mentor MemoryGel breast implants. Aesthetic Surg J. 2008;28(6):642–7.
Stevens WG, Hirsch EM, Tenenbaum MJ, Acevedo M. A prospective study of 708 form-stable silicone gel breast implants. Aesthetic Surg J. 2010;30(5):693–701.
Fischer S, Hirche C, Reichenberger MA, Kiefer J, Diehm Y, Mukundan S Jr, et al. Silicone implants with smooth surfaces induce thinner but denser fibrotic capsules compared to those with textured surfaces in a rodent model. PLoS ONE. 2015;10(7):e0132131.
Bergmann PA, Tamouridis G, Lohmeyer JA, Mauss KL, Becker B, Knobloch J, et al. The effect of a bacterial contamination on the formation of capsular contracture with polyurethane breast implants in comparison with textured silicone implants: an animal study. J Plast Reconstr Aesthet Surg. 2014;67(10):1364–70.
Tolksdorf J, Horch RE, Grüner JS, Schmid R, Kengelbach-Weigand A, Schubert DW, et al. Size matters—in vitro behaviour of human fibroblasts on textured silicone surfaces with different pore sizes. J Mater Sci - Mater Med. 2020;31(2):1–10.
Den Braber E, De Ruijter J, Ginsel L, Von Recum A, Jansen J. Orientation of ECM protein deposition, fibroblast cytoskeleton, and attachment complex components on silicone microgrooved surfaces. J Biomed Mater Res. 1998;40(2):291–300.
Crouch AS, Miller D, Luebke KJ, Hu W. Correlation of anisotropic cell behaviors with topographic aspect ratio. Biomaterials. 2009;30(8):1560–7.
Jones P, Mempin M, Hu H, Chowdhury D, Foley M, Cooter R, et al. The functional influence of breast implant outer shell morphology on bacterial attachment and growth. Plast Reconstr Surg. 2018;142(4):837–49.
Garabédian C, Delille R, Deltombe R, Anselme K, Atlan M, Bigerelle M. A multi-topographical-instrument analysis: The breast implant texture measurement. Surf Topogr Metrol Prop. 2017;5(2):025004.
Chi T, Ballinger T, Olds R, Zecchino M. Surface texture analysis using dektak stylus profilers: Veeco Instruments Inc; 2004. p. 1–4. https://fliphtml5.com/ibwv/hpas/basic.
Lampin M, Warocquier-Clérout R, Legris C, Degrange M, Sigot-Luizard M. Correlation between substratum roughness and wettability, cell adhesion, and cell migration. J Biomed Mater Res. 1997;36(1):99–108.
Atlan M, Bigerelle M, Larreta-Garde V, Hindié M, Hedén P. Characterization of breast implant surfaces, shapes, and biomechanics: a comparison of high cohesive anatomically shaped textured silicone, breast implants from three different manufacturers. Aesthetic Plast Surg. 2016;40(1):89–97.
Prasad BR, Brook MA, Smith T, Zhao S, Chen Y, Sheardown H, et al. Controlling cellular activity by manipulating silicone surface roughness. Colloids Surf, B. 2010;78(2):237–42.
Barth KA, Waterfield JD, Brunette DM. The effect of surface roughness on RAW 264.7 macrophage phenotype. J Biomed Mater Res A. 2013;101(9):2679–88.
Iso I. 14607 Non-Active Surgical Implants—Mammary Implants—Particular Requirements. Geneva, Switzerland: ISO; 2018.
Garabedian C, Vayron R, Bricout N, Deltombe R, Anselme K, Bigerelle M. In vivo damage study of different textured breast implants. Biotribology. 2020;23:100133.
Brody GS, Deapen D, Taylor CR, Pinter-Brown L, House-Lightner SR, Andersen JS, et al. Anaplastic large cell lymphoma occurring in women with breast implants: analysis of 173 cases. Plast Reconstr Surg. 2015;135(3):695–705.
Mazzocchi M, Dessy LA, Corrias F, Scuderi N. A clinical study of late seroma in breast implantation surgery. Aesthetic Plast Surg. 2012;36(1):97–104.
Giot J-P, Paek LS, Nizard N, El-Diwany M, Gaboury LA, Nelea M, et al. The double capsules in macro-textured breast implants. Biomaterials. 2015;67:65–72.
Quirós MC, Bolaños MC, Fassero JJ. Six-year prospective outcomes of primary breast augmentation with nano surface implants. Aesthetic Surg J. 2019;39(5):495–508.
Noskovicova N, Schuster R, van Putten S, Ezzo M, Koehler A, Boo S, et al. Suppression of the fibrotic encapsulation of silicone implants by inhibiting the mechanical activation of pro-fibrotic TGF-β. Nature Biomedical Engineering. 2021;5(12):1437–56.
Magill LJ, Tanska A, Keshtgar M, Mosahebi A, Jell G. Mechanical and surface chemical analysis of retrieved breast implants from a single centre. J Mech Behav Biomed Mater. 2019;91:24–31.
Grinnell F, Ho C-H. The effect of growth factor environment on fibroblast morphological response to substrate stiffness. Biomaterials. 2013;34(4):965–74.
Oakes PW, Patel DC, Morin NA, Zitterbart DP, Fabry B, Reichner JS, et al. Neutrophil morphology and migration are affected by substrate elasticity. Blood. 2009;114(7):1387–95.
Blakney AK, Swartzlander MD, Bryant SJ. The effects of substrate stiffness on the in vitro activation of macrophages and in vivo host response to poly (ethylene glycol)-based hydrogels. J Biomed Mater Res, Part A. 2012;100(6):1375.
Cai L, Liu W, Cui Y, Liu Y, Du W, Zheng L, et al. Biomaterial stiffness guides cross-talk between chondrocytes: implications for a novel cellular response in cartilage tissue engineering. ACS Biomater Sci Eng. 2020;6(8):4476–89.
Agrawal G, Negi YS, Pradhan S, Dash M, Samal S. Wettability and contact angle of polymeric biomaterials. Characterization of Polymeric Biomaterials: Elsevier; 2017. p. 57–81.
Sethuraman A, Han M, Kane RS, Belfort G. Effect of surface wettability on the adhesion of proteins. Langmuir. 2004;20(18):7779–88.
Xu L-C, Siedlecki CA. Effects of surface wettability and contact time on protein adhesion to biomaterial surfaces. Biomaterials. 2007;28(22):3273–83.
Lee JH, Lee HB. Platelet adhesion onto wettability gradient surfaces in the absence and presence of plasma proteins. J Biomed Mater Res. 1998;41(2):304–11.
Choee JH, Lee SJ, Lee YM, Rhee JM, Lee HB, Khang G. Proliferation rate of fibroblast cells on polyethylene surfaces with wettability gradient. J Appl Polym Sci. 2004;92(1):599–606.
Wassmann T, Kreis S, Behr M, Buergers R. The influence of surface texture and wettability on initial bacterial adhesion on titanium and zirconium oxide dental implants. Int J Implant Dent. 2017;3(1):1–11.
Harvey AG, Hill EW, Bayat A. Designing implant surface topography for improved biocompatibility. Expert Rev Med Devices. 2013;10(2):257–67.
Tamada Y, Ikada Y. Fibroblast growth on polymer surfaces and biosynthesis of collagen. J Biomed Mater Res. 1994;28(7):783–9.
Archer M, Dasari P, Walsh D, Britt KL, Evdokiou A, Ingman WV. Immune regulation of mammary fibroblasts and the impact of mammographic density. J Clin Med. 2022;11(3):799.
Montoya-Villegas KA, Ramírez-Jiménez A, Zizumbo-López A, Pérez-Sicairos S, Leal-Acevedo B, Bucio E, et al. Controlled surface modification of silicone rubber by gamma-irradiation followed by RAFT grafting polymerization. Eur Polym J. 2020;134:109817.
Wang B, Chen L, Abdulali-Kanji Z, Horton JH, Oleschuk RD. Aging effects on oxidized and amine-modified poly (dimethylsiloxane) surfaces studied with chemical force titrations: effects on electroosmotic flow rate in microfluidic channels. Langmuir. 2003;19(23):9792–8.
Minko S. Grafting on solid surfaces:“Grafting to” and “grafting from” methods. Polymer surfaces and interfaces: Springer; 2008. p. 215–34.
Chen H, Brook MA, Sheardown HD, Chen Y, Klenkler B. Generic bioaffinity silicone surfaces. Bioconjug Chem. 2006;17(1):21–8.
Maheshwari N, Kottantharayil A, Kumar M, Mukherji S. Long term hydrophilic coating on poly (dimethylsiloxane) substrates for microfluidic applications. Appl Surf Sci. 2010;257(2):451–7.
Mikhail AS, Ranger JJ, Liu L, Longenecker R, Thompson DB, Sheardown HD, et al. Rapid and efficient assembly of functional silicone surfaces protected by PEG: cell adhesion to peptide-modified PDMS. J Biomater Sci Polym Ed. 2010;21(6–7):821–42.
Plegue TJ, Kovach KM, Thompson AJ, Potkay JA. Stability of polyethylene glycol and zwitterionic surface modifications in PDMS microfluidic flow chambers. Langmuir. 2018;34(1):492–502.
Wang L, Sun B, Ziemer KS, Barabino GA, Carrier RL. Chemical and physical modifications to poly (dimethylsiloxane) surfaces affect adhesion of Caco-2 cells. J Biomed Mater Res A. 2010;93(4):1260–71.
Li M, Neoh KG, Xu LQ, Wang R, Kang E-T, Lau T, et al. Surface modification of silicone for biomedical applications requiring long-term antibacterial, antifouling, and hemocompatible properties. Langmuir. 2012;28(47):16408–22.
Nasef MM, Güven O. Radiation-grafted copolymers for separation and purification purposes: Status, challenges and future directions. Prog Polym Sci. 2012;37(12):1597–656.
Mata A, Fleischman AJ, Roy S. Characterization of polydimethylsiloxane (PDMS) properties for biomedical micro/nanosystems. Biomed Microdevice. 2005;7(4):281–93.
Zhao LH, Lee J, Sen PN. Long-term retention of hydrophilic behavior of plasma treated polydimethylsiloxane (PDMS) surfaces stored under water and Luria-Bertani broth. Sens Actuators A. 2012;181:33–42.
Duffy DC, McDonald JC, Schueller OJ, Whitesides GM. Rapid prototyping of microfluidic systems in poly (dimethylsiloxane). Anal Chem. 1998;70(23):4974–84.
Sellin N, Campos JSdC. Surface composition analysis of PP films treated by corona discharge. Mater Res. 2003;6:163–6.
Haji K, Zhu Y, Otsubo M, Honda C. Surface modification of silicone rubber after corona exposure. Plasma Processes Polym. 2007;4(S1):S1075–80.
Meincken M, Berhane T, Mallon P. Tracking the hydrophobicity recovery of PDMS compounds using the adhesive force determined by AFM force distance measurements. Polymer. 2005;46(1):203–8.
Bilgin S, Isik M, Yilgor E, Yilgor I. Hydrophilization of silicone–urea copolymer surfaces by UV/ozone: Influence of PDMS molecular weight on surface oxidation and hydrophobic recovery. Polymer. 2013;54(25):6665–75.
Efimenko K, Wallace WE, Genzer J. Surface modification of Sylgard-184 poly (dimethyl siloxane) networks by ultraviolet and ultraviolet/ozone treatment. J Colloid Interface Sci. 2002;254(2):306–15.
Lam M, Moris V, Humblot V, Migonney V, Falentin-Daudre C. A simple way to graft a bioactive polymer–Polystyrene sodium sulfonate on silicone surfaces. Eur Polymer J. 2020;128:109608.
Wong I, Ho C-M. Surface molecular property modifications for poly (dimethylsiloxane)(PDMS) based microfluidic devices. Microfluid Nanofluid. 2009;7(3):291–306.
Serafetinides A, Makropoulou M, Skordoulis C, Kar A. Ultra-short pulsed laser ablation of polymers. Appl Surf Sci. 2001;180(1–2):42–56.
Armyanov S, Stankova N, Atanasov P, Valova E, Kolev K, Georgieva J, et al. XPS and μ-Raman study of nanosecond-laser processing of poly (dimethylsiloxane)(PDMS). Nucl Instrum Methods Phys Res Sect B. 2015;360:30–5.
Yang L, Li L, Tu Q, Ren L, Zhang Y, Wang X, et al. Photocatalyzed surface modification of poly (dimethylsiloxane) with polysaccharides and assay of their protein adsorption and cytocompatibility. Anal Chem. 2010;82(15):6430–9.
Silverio V, Canane PA, Cardoso S. Surface wettability and stability of chemically modified silicon, glass and polymeric surfaces via room temperature chemical vapor deposition. Colloids Surf A. 2019;570:210–7.
Lee D, Yang S. Surface modification of PDMS by atmospheric-pressure plasma-enhanced chemical vapor deposition and analysis of long-lasting surface hydrophilicity. Sens Actuators B Chem. 2012;162(1):425–34.
Kohjiya S, Ikeda Y. Reinforcement of general-purpose grade rubbers by silica generated in situ. Rubber Chem Technol. 2000;73(3):534–50.
Roman GT, Culbertson CT. Surface engineering of poly (dimethylsiloxane) microfluidic devices using transition metal sol− gel chemistry. Langmuir. 2006;22(9):4445–51.
Roman GT, Hlaus T, Bass KJ, Seelhammer TG, Culbertson CT. Sol− gel modified poly (dimethylsiloxane) microfluidic devices with high electroosmotic mobilities and hydrophilic channel wall characteristics. Anal Chem. 2005;77(5):1414–22.
van Kooten TG, Whitesides JF, von Recum AF. Influence of silicone (PDMS) surface texture on human skin fibroblast proliferation as determined by cell cycle analysis. J Biomed Mater Res. 1998;43(1):1–14.
Xia Y, Whitesides GM. Soft lithography. Annu Rev Mater Sci. 1998;28(1):153–84.
Kim EJ, Boehm CA, Mata A, Fleischman AJ, Muschler GF, Roy S. Post microtextures accelerate cell proliferation and osteogenesis. Acta Biomater. 2010;6(1):160–9.
Mata A, Boehm C, Fleischman AJ, Muschler G, Roy S. Analysis of connective tissue progenitor cell behavior on polydimethylsiloxane smooth and channel micro-textures. Biomed Microdevice. 2002;4(4):267–75.
Green AM, Jansen JA, Van der Waerden J, Von Recum AF. Fibroblast response to microtextured silicone surfaces: texture orientation into or out of the surface. J Biomed Mater Res. 1994;28(5):647–53.
Ai H, Mills DK, Jonathan AS, Jones SA. Gelatin-glutaraldehyde cross-linking on silicone rubber to increase endothelial cell adhesion and growth. In vitro Cell Dev Biol Anim. 2002;38(9):487–92.
Yoo BY, Kim BH, Lee JS, Shin BH, Kwon H, Koh W-G, et al. Dual surface modification of PDMS-based silicone implants to suppress capsular contracture. Acta Biomater. 2018;76:56–70.
Zeplin PH, Larena-Avellaneda A, Jordan M, Laske M, Schmidt K. Phosphorylcholine-coated silicone implants: effect on inflammatory response and fibrous capsule formation. Ann Plast Surg. 2010;65(6):560–4.
Maharjan AS, Pilling D, Gomer RH. High and low molecular weight hyaluronic acid differentially regulate human fibrocyte differentiation. PLoS ONE. 2011;6(10):e26078.
Bračič M, Fras-Zemljič L, Pérez L, Kogej K, Stana-Kleinschek K, Kargl R, et al. Protein-repellent and antimicrobial nanoparticle coatings from hyaluronic acid and a lysine-derived biocompatible surfactant. Journal of Materials Chemistry B. 2017;5(21):3888–97.
Ferreira P, Carvalho Á, Correia TR, Antunes BP, Correia IJ, Alves P. Functionalization of polydimethylsiloxane membranes to be used in the production of voice prostheses. Sci Technol Adv Mater. 2013;14(5):055006.
DeFife KM, Shive MS, Hagen KM, Clapper DL, Anderson JM. Effects of photochemically immobilized polymer coatings on protein adsorption, cell adhesion, and the foreign body reaction to silicone rubber. J Biomed Mater Res. 1999;44(3):298–307.
Zhang M, Desai T, Ferrari M. Proteins and cells on PEG immobilized silicon surfaces. Biomaterials. 1998;19(10):953–60.
Kovach KM, Capadona JR, Gupta AS, Potkay JA. The effects of PEG-based surface modification of PDMS microchannels on long-term hemocompatibility. J Biomed Mater Res Part A. 2014;102(12):4195–205.
Trantidou T, Elani Y, Parsons E, Ces O. Hydrophilic surface modification of PDMS for droplet microfluidics using a simple, quick, and robust method via PVA deposition. Microsyst Nanoeng. 2017;3(1):16091.
Li J, Wang M, Shen Y. Chemical modification on top of nanotopography to enhance surface properties of PDMS. Surf Coat Technol. 2012;206(8):2161–7.
Lu Y, Wang D, Li T, Zhao X, Cao Y, Yang H, et al. Poly (vinyl alcohol)/poly (acrylic acid) hydrogel coatings for improving electrode–neural tissue interface. Biomaterials. 2009;30(25):4143–51.
Ham J, Kim Y, An T, Kang S, Ha C, Wufue M, et al. Covalently grafted 2-methacryloyloxyethyl phosphorylcholine networks inhibit fibrous capsule formation around silicone breast implants in a porcine model. ACS Appl Mater Interfaces. 2020;12(27):30198–212.
Chien H-W, Tsai C-C, Tsai W-B, Wang M-J, Kuo W-H, Wei T-C, et al. Surface conjugation of zwitterionic polymers to inhibit cell adhesion and protein adsorption. Colloids Surf B. 2013;107:152–9.
Keefe AJ, Brault ND, Jiang S. Suppressing surface reconstruction of superhydrophobic PDMS using a superhydrophilic zwitterionic polymer. Biomacromol. 2012;13(5):1683–7.
Sharma D, Jia W, Long F, Pati S, Chen Q, Qyang Y, et al. Polydopamine and collagen coated micro-grated polydimethylsiloxane for human mesenchymal stem cell culture. Bioactive Materials. 2019;4:142–50.
Chuah YJ, Koh YT, Lim K, Menon NV, Wu Y, Kang Y. Simple surface engineering of polydimethylsiloxane with polydopamine for stabilized mesenchymal stem cell adhesion and multipotency. Sci Rep. 2015;5(1):18162.
Valencia-Lazcano A, Román-Doval R, De La Cruz-Burelo E, Millán-Casarrubias E, Rodríguez-Ortega A. Enhancing surface properties of breast implants by using electrospun silk fibroin. J Biomed Mater Res B Appl Biomater. 2018;106(5):1655–61.
Xue P, Li Q, Li Y, Sun L, Zhang L, Xu Z, et al. Surface modification of poly (dimethylsiloxane) with polydopamine and hyaluronic acid to enhance hemocompatibility for potential applications in medical implants or devices. ACS Appl Mater Interfaces. 2017;9(39):33632–44.
Hung H-S, Yu AY-H, Hsieh S-C, Kung M-L, Huang H-Y, Fu R-H, et al. Enhanced biocompatibility and differentiation capacity of mesenchymal stem cells on poly (dimethylsiloxane) by topographically patterned dopamine. ACS Appl Mater Interfaces. 2020;12(40):44393–406.
Mohan T, Čas A, Bračič M, Plohl O, Vesel A, Rupnik M, et al. Highly Protein Repellent and Antiadhesive Polysaccharide Biomaterial Coating for Urinary Catheter Applications. ACS Biomater Sci Eng. 2019;5(11):5825–32.
Hauser J, Zietlow J, Köller M, Esenwein SA, Halfmann H, Awakowicz P, et al. Enhanced cell adhesion to silicone implant material through plasma surface modification. J Mater Sci Mater Med. 2009;20(12):2541–8.
Barthes J, Lagarrigue P, Riabov V, Lutzweiler G, Kirsch J, Muller C, et al. Biofunctionalization of 3D-printed silicone implants with immunomodulatory hydrogels for controlling the innate immune response: An in vivo model of tracheal defect repair. Biomaterials. 2021;268:120549.
Kim BH, Park M, Park HJ, Lee SH, Choi SY, Park CG, et al. Prolonged, acute suppression of cysteinyl leukotriene to reduce capsular contracture around silicone implants. Acta Biomater. 2017;51:209–19.
Razavi M, Primavera R, Vykunta A, Thakor AS. Silicone-based bioscaffolds for cellular therapies. Mater Sci Eng C Mater Biol Appl. 2021;119:111615.
Jarvelainen H, Sainio A, Koulu M, Wight TN, Penttinen R. Extracellular matrix molecules: potential targets in pharmacotherapy. Pharmacol Rev. 2009;61(2):198–223.
Ricard-Blum S. The collagen family. Cold Spring Harb Perspect Biol. 2011;3(1):a004978.
Zhang Y, Reif G, Wallace DP. Extracellular matrix, integrins, and focal adhesion signaling in polycystic kidney disease. Cell Signal. 2020;72:109646.
Yilgor C, YilgorHuri P, Huri G. Tissue engineering strategies in ligament regeneration. Stem Cells Int. 2012;2012:374676.
Leonga LM, Sahalana AZ, Tana LH, Mustafaa NH. Clarias batrachus collagen extract increases fibroblast cell adhesion, migration and proliferation. J Appl Pharm Sci. 1930;5(3):019–23.
Gaudet C, Marganski WA, Kim S, Brown CT, Gunderia V, Dembo M, et al. Influence of type I collagen surface density on fibroblast spreading, motility, and contractility. Biophys J. 2003;85(5):3329–35.
Li Q, Sun L, Zhang L, Xu Z, Kang Y, Xue P. Polydopamine-collagen complex to enhance the biocompatibility of polydimethylsiloxane substrates for sustaining long-term culture of L929 fibroblasts and tendon stem cells. J Biomed Mater Res Part A. 2018;106(2):408–18.
Gao C-Y, Guo Y-Y, He J, Wu M, Liu Y, Chen Z-L, et al. L-3, 4-dihydroxyphenylalanine-collagen modified PDMS surface for controlled cell culture. J Mater Chem. 2012;22(21):10763–70.
Price RD, Berry M, Navsaria HA. Hyaluronic acid: the scientific and clinical evidence. J Plast Reconstr Aesthet Surg. 2007;60(10):1110–9.
Dong Y, Cui M, Qu J, Wang X, Kwon SH, Barrera J, et al. Conformable hyaluronic acid hydrogel delivers adipose-derived stem cells and promotes regeneration of burn injury. Acta Biomater. 2020;108:56–66.
Cañibano-Hernández A, Del Burgo LS, Espona-Noguera A, Orive G, Hernández RM, Ciriza J, et al. Hyaluronic acid enhances cell survival of encapsulated insulin-producing cells in alginate-based microcapsules. Int J Pharm. 2019;557:192–8.
Yue Z, Liu X, Molino PJ, Wallace GG. Bio-functionalisation of polydimethylsiloxane with hyaluronic acid and hyaluronic acid – Collagen conjugate for neural interfacing. Biomaterials. 2011;32(21):4714–24.
Matou-Nasri S, Gaffney J, Kumar S, Slevin M. Oligosaccharides of hyaluronan induce angiogenesis through distinct CD44 and RHAMM-mediated signalling pathways involving Cdc2 and γ-adducin. Int J Oncol. 2009;35(4):761–73.
Sahoo N, Sahoo RK, Biswas N, Guha A, Kuotsu K. Recent advancement of gelatin nanoparticles in drug and vaccine delivery. Int J Biol Macromol. 2015;81:317–31.
Li P, Dou X, Feng C, Schönherr H. Enhanced cell adhesion on a bio-inspired hierarchically structured polyester modified with gelatin-methacrylate. Biomater Sci. 2018;6(4):785–92.
Liu B-S. Fabrication and evaluation of a biodegradable proanthocyanidin-crosslinked gelatin conduit in peripheral nerve repair. J Biomed Mater Res Part A. 2008;87A(4):1092–102.
Hatton PV, Walsh J, Brook IM. The response of cultured bone cells to resorbable polyglycolic acid and silicone membranes for use in orbital floor fracture repair. Clin Mater. 1994;17(2):71–80.
Miller DC, Thapa A, Haberstroh KM, Webster TJ. Endothelial and vascular smooth muscle cell function on poly(lactic-co-glycolic acid) with nano-structured surface features. Biomaterials. 2004;25(1):53–61.
Pedraza E, Brady A-C, Fraker CA, Stabler CL. Synthesis of macroporous poly (dimethylsiloxane) scaffolds for tissue engineering applications. J Biomater Sci Polym Ed. 2013;24(9):1041–56.
Huang C-Y, Hu K-H, Wei Z-H. Comparison of cell behavior on pva/pva-gelatin electrospun nanofibers with random and aligned configuration. Sci Rep. 2016;6(1):37960.
Hower JC, Bernards MT, Chen S, Tsao H-K, Sheng Y-J, Jiang S. Hydration of “nonfouling” functional groups. J Phys Chem B. 2009;113(1):197–201.
Sin M-C, Chen S-H, Chang Y. Hemocompatibility of zwitterionic interfaces and membranes. Polym J. 2014;46(8):436–43.
Kathmann EE, White LA, McCormick CL. Water soluble polymers: 70. Effects of methylene versus propylene spacers in the pH and electrolyte responsiveness of zwitterionic copolymers incorporating carboxybetaine monomers. Polymer. 1997;38(4):879–86.
Kheirandish S, Jabbari E. Effect of surface polarity on wettability and friction coefficient of silicone rubber/poly (acrylic acid) hydrogel composite. Colloid Polym Sci. 2006;284(12):1411–7.
Acknowledgements
Authors would like to thank Yessica Elizondo Hidalgo (Establishment Labs Holdings, Alajuela, Costa Rica) for critical reading and helpful comments on the manuscript.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conceptualization: F.T.F., K.D., N.K., and A.B.; Methodology: F.T.F., K.D., N.K., and A.B.; Writing—original draft preparation: F.T.F., K.D., and A.B.; Writing—review and editing: F.T.F., K.D., N.K., V.Z.M., R.M., and A.B.; Supervision: K.D., N.K., and A.B.; All authors have read and agreed to the version of manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests” in this section.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Foroushani, F.T., Dzobo, K., Khumalo, N.P. et al. Advances in surface modifications of the silicone breast implant and impact on its biocompatibility and biointegration. Biomater Res 26, 80 (2022). https://doi.org/10.1186/s40824-022-00314-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40824-022-00314-1