Abstract
Background
Abdominal aortic aneurysm (AAA) is an important cardiovascular health problem. Ultrasound screening is proven to reduce AAA mortality and programmes have been implemented in some healthcare systems. Those who are identified as having a small AAA in screening enter into a surveillance programme to monitor AAA size. Individuals in AAA surveillance are at elevated risk of cardiovascular events, which is not currently addressed sufficiently. We aimed to develop a simple intervention to reduce cardiovascular risk, which could be embedded in AAA surveillance pathways.
Methods
Intervention mapping methods were used to co-develop the intervention with individuals with AAA, families/carers, and healthcare staff. We identified “targets for change” by synthesising research evidence and international guidelines and consulting with patients, caregivers and health service providers. We conducted a series of workshops to identify barriers to and facilitators of change and used taxonomies of behaviour change theories and techniques to match intervention strategies to each target. Further stakeholder involvement work helped refine the intervention.
Results
The developed intervention focusses on assessment and individually tailored discussion of risk factors, exchanging information, building motivation and action planning, followed by review of progress and problem-solving. Workbooks covering physical activity, diet, stress management, alcohol, smoking, blood pressure and mental health are provided to support behaviour change. The intervention is facilitated by trained healthcare professionals during the patient’s AAA screening appointment for the duration that they are in surveillance.
Discussion
The developed intervention will now be tested to assess whether it can be integrated with the current AAA screening programme. The developed intervention is a novel approach to reducing cardiovascular disease in the AAA population, it is also the first intervention which tries to do this in this population.
Trial registration
International Clinical Trial Registration: ISRCTN93993995.
Similar content being viewed by others
Background
All men in the UK are invited for an ultrasound scan to screen for Abdominal Aortic Aneurysm (AAA) in the year of their 65th birthday; similar programmes exist in other countries [1,2,3,4]. The vast majority of those diagnosed with AAA through screening do not require immediate surgery to treat the AAA [1, 2, 4,5,6,7,8,9]. They are entered into a disease-specific surveillance programme to monitor AAA growth with repeat ultrasound measurements [8, 9]. Whilst screening reduces AAA-related mortality by providing an opportunity for timely surgical intervention, it has a very minimal effect on all-cause mortality [2, 4, 6, 10].
Patients with AAA have an elevated cardiovascular risk; in fact, cardiovascular events are one of the principle causes of morbidity and mortality amongst those in AAA surveillance [2, 4, 6, 7]. This elevated risk is mainly driven by modifiable risk factors such as smoking and excess weight [2, 4, 6].
The regular attendance of these individuals with AAA at surveillance clinics represents an excellent opportunity to address their excess cardiovascular risk within an existing, well-defined, and well-attended clinical pathway. AAA surveillance pathways were not specifically developed to deliver cardiovascular risk modification. Further, those with AAA have unique characteristics that make the adoption of cardiovascular interventions developed in different clinical settings challenging. They typically suffer from multiple co-morbidities, avoid contact with primary or secondary healthcare (even though AAA surveillance attendance consistently exceeds 80%), have poor medication adherence, and are often socio-economically deprived [2,3,4, 11]. Consequently, uptake of cardiovascular risk management has been virtually non-existent in AAA surveillance, despite some attempts by screening programmes to offer cardiovascular risk reduction interventions [2,3,4, 11, 12]. No high-quality research has been undertaken to develop and test interventions to reduce cardiovascular risk in this clinical area.
Given the excellent attendance and low dropout of AAA surveillance, this is a major opportunity to offer better cardiovascular prevention to a population at very high risk for cardiovascular events [8, 9]. This research addressed this opportunity by developing a cardiovascular risk reduction intervention specifically designed to be embedded within the existing NHS Abdominal Aortic Aneurysm Screening Programme (NAAASP) clinical care pathway, hoping to reduce the chance of cardiovascular events following the diagnosis of an AAA.
Methods and results
This research was approved by the NHS Wales Research Ethics Committee 7 (NHS Wales REC 7) and the NHS Health Research Authority (HRA) in January 2020 (reference: 19/EM/0366). The research was funded by the National Institute for Health and Care Research (NIHR) Academy (reference: NIHR300059) and sponsored by the University of Leicester (reference: 0479); the funder and sponsor had no input in data collection, analysis or interpretation. Participants provided written informed consent upon recruitment.
The main aim was to develop a complex clinical intervention, the Cardiovascular risk reduction in patients with aneurysms (CRISP) intervention, in order to reduce cardiovascular risk in those taking part in the NHS AAA surveillance programmes across the UK and who have a small or medium-sized aneurysm. Based on current definitions, a small or medium AAA measures between 3.0 and 5.5 cm in maximal anteroposterior diameter (ultrasound measurement), using NAAASP standard operating procedures (SOPs) [2, 5]. Patients with an AAA exceeding 5.5 cm in size are referred to secondary care for consideration of surgical repair [1, 8, 9, 13, 14]. All patients are advised to take antiplatelet and lipid-control medications (statin); however, the mechanism to ensure this happens varies considerably across screening programmes [1, 2, 6, 8].
The CRISP intervention was designed based on the Medical Research Council (MRC) guidelines for the development of complex interventions for clinical settings [15], using the intervention mapping approach and principles. The intervention mapping framework, widely used in the development of health behaviour change interventions, is described in detail elsewhere [16]. It comprises a six-step ecological approach to assessing and intervening in health problems via the development or modification of an intervention.
-
Step 1: Logic model of the problem
-
Step 2: Programme outcomes and objectives – Logic model of change
-
Step 3: Programme design
-
Step 4: Programme production
-
Step 5: Programme implementation plan
-
Step 6: Evaluation plan
As this is an iterative process, methods and results will be presented together for each step.
Participants and stakeholders
To develop the intervention, three stakeholder groups were formed:
-
Group A: Patient (lay) advisory group, consisting of 63 men with a small or medium-sized AAA who were taking part in AAA surveillance within NAAASP, 26 men who had undergone AAA repair surgery following attendance to AAA screening in the NHS (AAA picked up via AAA screening), 8 men who had been considered for AAA repair once they had been diagnosed with an AAA via screening and had attended at least one surveillance appointment but were eventually deemed not fit for surgery once they had been seen in secondary care, one man who had surgery due to an AAA rupture and had survived (had previously not attended screening despite having received an invitation), and one man diagnosed with an AAA after having suffered a myocardial infarction (incidental finding) and awaiting to be seen in AAA surveillance via NAAASP. Seven partners (wives in all cases) also took part. Participants were from across all aneurysm screening and surveillance programmes in the UK.
-
Group B: A service provider advisory group, consisting of 43 healthcare staff involved in delivery and management of NHS AAA screening/surveillance.
-
Group C: A cardiovascular expert advisory group, consisting of 21 clinicians involved in cardiovascular care of individuals with AAA (cardiologists, vascular surgeons, general practitioners, pharmacists, vascular nurses) alongside 4 experts on the prescription of exercise to reduce cardiovascular risk.
Further to the 3 research-specific advisory groups, advice was sought, when necessary from the NAAAP Research Committee, NAAASP clinical lead, a senior Public Health (Professor Holland, University of Leicester) and Behaviour Change (Professor Colin Greaves) researcher, as well as members of the councils of the Vascular Society of Great Britain and Ireland (VSGBI) and Society of Vascular Nursing. An independent AAA-specific patient advisory group provided advice on patient-facing materials, barrier, and facilitators. Participants were recruited to the stakeholder advisory groups by advertising the opportunity on social media, word of mouth and the authors asking their professional networks to circulate an advert (direct recruitment). Due to the coronavirus disease 2019 (COVID-19) pandemic, all advisory groups were held online using videoconferencing software. The chief investigator (AS) liaised with participants who did not have access to videoconferencing to provide appropriate software and hardware (free) and facilitate participation. No lay participants or expert stakeholders invited to take part declined taking part due to inability to join the online advisory groups. Potential participants who could not understand written and spoken English were not able to take part as there was no translation facility during the advisory groups and discussion in English was necessary in order to obtain relevant data of sufficient quality. When necessary, lay individuals or experts were interviewed by AS and/or TW over the telephone to address queries.
Step 1: logic model of the problem
To identify target behaviours for reduction of cardiovascular risk the existing evidence-base on lifestyle intervention components and behaviour change strategies associated with effectiveness for reducing cardiovascular risk was reviewed (AS, TW, CG). This included updating a prior review on this topic [17] as part of a commissioned “state-of-the-art” review [18]. We also reviewed cardiovascular interventions developed for other high-risk populations with similar characteristics, such as male long-distance truck drivers and patients with psoriasis [19,20,21] and undertook a systematic review on the long-term effectiveness of physical activity interventions, searched other relevant systematic reviews [17] and relevant clinical guidelines [22,23,24,25,26,27]. Almost all lay participants were against the exclusive use of digital technologies to deliver the intervention, although they were supportive of having links to sources of online support for those who were capable and willing to use them.
Scaffolding questionnaire
Based on the initial work, described above, we developed a ‘scaffolding questionnaire.’ This was used to inform the initial design of the intervention. There were two versions: a patient and healthcare professional version. The questions explored optimal contents as well as barriers and enablers in creating and delivering the intervention. They were modified appropriately in each group to ensure that they were relevant for the target audience. The questions focused on understanding the respondent’s knowledge of AAA, to ensure that the intervention is informative and not repeating what is already known, and their views on what cardiovascular risk factors are the most important to focus on and which one are more likely to be successful, an example scaffolding questionnaire is provided in Additional file 1: Appendix 1. The scaffolding questionnaire was distributed via social media, through screening programmes and the authors’ professional networks. All responses to the questionnaire were anonymised therefore it is not possible to assess if there was any overlap between those who answered the scaffolding questionnaire and took part in the advisory group(s) described above. Responses to numerical questions were collated descriptively, and free text responses were analysed thematically.
A total of 14 responses were received for the patient questionnaire, made up of 10 respondents who are currently undergoing AAA screening, 3 who had and AAA repaired surgically and one who did not specify. We received 59 responses for the healthcare professional questionnaire (GPs n = 13, consultant vascular surgeon n = 13, trainee vascular surgeon n = 7, surgeon n = 4, AAA screening nurse n = 3, AAA screening technician n = 3, vascular specialist nurse n = 3, other healthcare professional n = 12, did not state profession n = 1). Both groups, patient and healthcare professionals, broadly agreed on including medication review, increasing physical activity and heart healthy eating/weight management (Table 1). The other potential components received a more mixed response.
The scaffolding questionnaire also explored the optimum delivery method (Table 2); this information was used in step 2, described later.
Following this process we identified the below components would make up the intervention and that patients would be able to choose which components they wished to focus on:
-
Stop smoking support
-
Increasing physical activity
-
Improving diet/weight management
-
Medication review
-
Managing stress/anxiety
-
Managing low mood/depression
-
Alcohol support, this was added retrospectively during step 2. As during the advisory groups, it became apparent that a number of participants felt that this was important.
Step 2: programme outcomes and objectives
We then convened three online advisory group discussions with our lay membership, one joint between our cardiovascular and delivery experts, one joint between the delivery and lay group and one for the lay group, an example topic guide is presented in Additional file 2: Appendix 2. Following that, we involved primary care doctors through a national online survey (194 responses by general practitioners and practice nurses across the UK) and interviewed four GPs. We explored the following topics:
-
Which are the main barriers or facilitators in engaging with cardiovascular risk modification during AAA surveillance? Both from the perspective of healthcare professionals and patients.
-
Which of the identified barriers are modifiable and have the greatest scope for change?
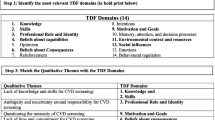
Based on the specification of the behavioural, environmental and psychological targets for change which emerged from the needs assessment (step 1), performance objectives were specified. Performance objectives are the description of the specific behaviours that the at-risk group or other agents (HCPs in this case) have to perform to achieve the desired change [16]. For each performance objective, modifiable determinants of change (barriers and enablers) were identified via our stakeholder workshops as well as (in some cases) previously published research and were labelled using existing taxonomies of theory-informed behaviour change processes [28].
Step 3: programme design
We then ‘mapped’ the performance objectives and modifiable determinants of change onto strategies to change behaviour to produce intervention maps, also known as intervention matrices. Change techniques were identified using a combination of the experience of the research team, advisory group participant suggestions and the use of the behaviour change technique taxonomy [29] and the associated Theory and Techniques Tool [30]. The latter tool provides a method for identifying a range of behaviour change techniques that have supportive evidence for influencing the proposed intervention processes. Initially, all possible/candidate behaviour change techniques were identified using the Theory and \techniques Tool and then reviewed by both our intervention development team (CG, TW) and by discussion with our stakeholder advisory groups. The ones which were inappropriate or not practical in the context of this study were removed. For example, ‘Instruction of how to perform behaviour’ was initially identified as a potential technique to improve ‘knowledge’ for the alcohol intervention map. However, it was subsequently removed as instructions on how to drink less alcohol would have been simplistic and perceived as patronising by patients.
An extract of the reducing alcohol consumption intervention map is presented in Table 3 with the performance objectives and modifiable determinants filling the first two columns. In addition to this, the proposed mechanism of action was also identified to aid in the identification of potential behaviour change techniques from the Theory and Techniques Tool, developed by Johnston and colleagues [30] and a taxonomy of behaviour change techniques [31]. A total of eight intervention maps were developed:
-
1.
Reducing alcohol consumption
-
2.
Improving diet and losing weight
-
3.
Engaging with the CRISP intervention
-
4.
Increasing physical activity
-
5.
Managing blood pressure
-
6.
Smoking cessation
-
7.
Managing stress, anxiety and low mood
Engaging with the CRISP intervention map focused on how to ensure engagement with the intervention for both patients and healthcare professionals. Its creation was necessitated as it was identified through the healthcare professional and patient focus groups that motivation to engage with a cardiovascular risk reduction intervention is highly variable. The other intervention maps focused on specific health behaviours.
In addition to the intervention maps a logic model was developed, below, which shows how the intervention should work in theory (Fig. 1).
Step 4: Programme production
The aim of this step is to finalise what the intervention is going to ‘look like’ and how the component change techniques will be organised and delivered in practice. This was initially done by recording ideas in the final column of the intervention (Table 3) about strategies that could be used to carry out the behaviour change technique. For example, the strategy used for the behaviour change technique ‘feedback on behaviour’ was to give patients feedback on their drinking habits via the validated AUDIT-C alcohol-intake questionnaire [32]. Following this process, a draft intervention was presented to a joint meeting of all the advisory groups (lay and expert participants) to elicit their feedback and finalise the intervention format/contents.
For the final feedback session of the joint advisory group, the session focused on feedback on an example work booklet, which was for physical activity. The feedback was broadly positive however a few improvements were suggested:
-
Need to explain why lifting heavy weights is inappropriate but yoga and tai chi are fine.
-
Offering the ability to monitor blood pressure would be beneficial as a motivational tool.
-
Need to highlight what heavy household items are/are not acceptable to lift.
Following this the intervention was finalised. Along with the finalisation of the patient workbooks which were developed using both current best practice and patient’s views on what is important to highlight. It was not possible, due to time constraints, to receive patient feedback on all patient workbooks. The finalised intervention, summarised in Fig. 2, is delivered in two stages. In the first stage, the patient fills out a risk factor questionnaire and sends it back to their local screening service. When the screening service receives the filled-out questionnaire they enter the data into a bespoke computer program which calculates the personalised risk factor profile of the patient this is presented as a letter (example in Additional file 3: Appendix 3). With permission, the validated SMART risk score [33] was used to predict cardiovascular risk score.
The beginning of the second stage starts at the nurse assessment. The nurse assessment is part of standard care following the diagnosis of a small or medium aneurysm. The purpose of the nurse assessment is to assess the overall health of the patient and suggest things a patient could do to improve their health for example; lose weight, quit smoking and or increase physical activity. The aim of the intervention is not to modify what is currently being done during the nurse assessment, which varies across the country, but to add to it.
Whilst the patient is in the waiting room waiting for the start of their nurse assessment they will be given their personalised risk factor letter to read. A small number of patients request that their nurse assessment happen via email, phone or online. In this case, the letter will be sent to them beforehand. The patient will then be called in, and initially, their feelings and thoughts about the risk factor letter will be discussed along with anything that they may not have understood. The patient will then be asked to pick one or two (maximum three) risk factors to focus on. Patients were limited to a maximum of three risk factors to ensure that they had sufficient time to develop their strategy to change their behaviour for the chosen risk factor(s). The nurse may assist the patient in deciding which risk factors to focus on but it must ultimately be the patient’s decision. The nurse will then introduce the appropriate workbook(s) for the risk factors the patient has decided to focus on. A workbook has been developed for each risk factor for patients to help patients. The workbooks contain both information on why reducing the risk factor is beneficial and activities designed to help patients reduce the risk factor. If appropriate patients will also be offered the opportunity for home blood pressure monitoring. In subsequent appointments, which alternate between phone and in-person contacts initially patient progress will be reviewed. This will be followed by problem-solving collaboratively with the patient any challenges they may have come across. This may include but is not limited to modifying goals, working through solutions to identified barriers and changing risk factors to focus on. Finally, the session will review and set goals until the next appointment. All patient contacts should last no longer than 30 min on average. The length of time between face-to-face appointments is dictated by the AAA screening programme, with the phone appointments happening approximately halfway between the face-to-face appointments. Those delivering the intervention attended a one-day training course where they were trained in the delivery of the intervention. This will include training in both intervention content and using the guiding style of communication. Before attendance at the training day participants completed a self-directed online learning module which was accessed through NHS learn. The online training introduced the aim and contentment of the CRISP intervention. It also contained examples of best practice videos and explained the theory behind them.
Steps 5 and 6: programme implementation and evaluation plan
Implementation planning is built into our approach via the involvement of service providers and service managers as stakeholders in the co-development of the intervention. The intervention has been specifically designed to be feasible for implementation within the NHS AAA Screening Programme. Feedback from the planned feasibility study and trial (below) will help to iteratively refine and optimise implementation.
Evaluation of the CRISP intervention will involve a feasibility trial including a mixed-methods process evaluation focused on refining the intervention process model (as well as establishing acceptability and fidelity of the intervention and trial procedures). The aim of the process evaluation is twofold: to test the logic model and assess intervention fidelity This is currently ongoing. Following this, the intervention will be modified based on the feedback received and a version 2 developed. Following this a multi-site randomised controlled trial to establish effectiveness and cost-effectiveness will follow and, if successful, the intervention will be rolled out across the AAA surveillance programme.
The final step of intervention mapping is to develop an in-service evaluation plan when the intervention has been adopted to ensure constant improvement. This step will be completed if/when the intervention is rolled out across NAAASP.
Discussion
In work package 1 of this research, we developed a complex clinical intervention which is purpose-built for use in AAA screening and surveillance pathways, aiming to reduce the cardiovascular risk of the participants. The intervention is based not only on best available evidence/guidance and on behaviour change theory, but most importantly it is grounded on the views and opinions of patients and healthcare professionals. The final intervention, currently being feasibility-tested in the NHS, consists of a number of workbooks and interactions between NAAASP staff and patients.
The intervention mapping framework used to develop the intervention was time and resource-intensive, requiring one research fellow to work on it full time for 1.5 years, but produced an intervention for use in clinical care that takes into consideration the requirements of the patient, healthcare professionals and service providers. The core research team required to develop this intervention consisted of two vascular surgeons (AS, MJB), two experienced psychologists with expertise in intervention mapping (CG, TW), and a national support network of experts in a variety of clinical areas. Further, hundreds of lay individuals (with or without aneurysms) supported our advisory groups, interviews, and online surveys. The resources required to develop this intervention were considerable, with an overall cost of £244,000 for the development activities (funded by the NIHR). At the same time [34], there are 348 preventable cardiovascular deaths and 720 non-fatal major cardiovascular events every year in England amongst men in AAA surveillance [35]. A 20% decrease would lead to an annual saving of £14.8 million in treatment costs alone across the NHS [3, 8, 9, 36, 37]. Achieving a systolic blood pressure < 140 mmHg, stopping smoking and achieving normal LDL levels in men with a small AAA would lead to a 29% overall absolute risk reduction in 10-year predicted cardiovascular events with seven cardiovascular-disease-free years of survival gained [6, 37].
It is not clear if using a different intervention development framework, such as the Behaviour Change Wheel [38] would result in a different outcome [38]. However, both approaches require an initial identification of what behaviour(s) require changing, followed by identification of mechanisms/processes of behaviour change (including contextual /implementation factors) and appropriate behaviour change techniques that could be used to modify the identified change processes. Socio-demographic data was not collected so it is not clear how represented the patients who engaged with intervention development were and if this had any influence on the design of the intervention.
This is the first study to set out the theoretical framework and development process behind a cardiovascular risk reduction intervention in individuals with AAA or similar life-threatening vascular pathology. However, despite the significant detail presented, it is unlikely that a different team would exactly replicate this intervention, due to the interpretative nature of intervention development. The approach taken is robust and documentable, however. The following feasibility study will access the feasibility of using the developed intervention in routine clinical care. We will be able to fine-tune elements/components of the intervention or proceed to direct adoption into care, in discussion with relevant national stakeholders. All behavioural /psychological components of the intervention (our ‘targets for change’) are based on high-quality evidence (mostly of randomised nature), which has evaluated the clinical effectiveness of each parameter (e.g. weight loss, optimal blood pressure control, prescription of antithrombotic therapy and statins) for reducing cardiovascular risk.
Conclusions
In this work, we present a detailed description of the design of an intervention to reduce cardiovascular risk in those with a AAA using intervention mapping [16]. This intervention has been developed in collaboration with both stakeholders and patients, addressing the particular characteristics of both patients in AAA screening/surveillance across the NHS, as well as the actual clinical pathways in place. This intervention has the potential to save and improve thousands of lives in the future. Following a period of feasibility testing, the intervention will then be assessed in a trial, before wider adoption in the NHS.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AAA:
-
Abdominal aortic aneurysm
- CRISP:
-
Cardiovascular risk reduction in patients with aneurysms (CRISP) intervention
- NAAASP:
-
National Abdominal Aortic Aneurysm Screening Programme
References
Campbell A, Waggett H, Armer M, Jacomelli J, Earnshaw JJ. Quality assurance for the NHS abdominal aortic aneurysm screening programme in England. BJS Open. 2022;6(1):zrab148. https://doi.org/10.1093/bjsopen/zrab148.
Sidloff DA, Saratzis A, Thompson J, Katsogridakis E, Bown MJ. Editor’s Choice - Infra-Renal Aortic Diameter and Cardiovascular Risk: Making Better Use of Abdominal Aortic Aneurysm Screening Outcomes. Eur J Vasc Endovasc Surg. 2021;62(1):38–45.
Bath MF, Sidloff D, Saratzis A, Bown MJ, investigators UKAGS. Impact of abdominal aortic aneurysm screening on quality of life. Br J Surg. 2018;105(3):203–8.
Bath MF, Saratzis A, Saedon M, Sidloff D, Sayers R, Bown MJ, et al. Patients with Small Abdominal Aortic Aneurysm are at Significant Risk of Cardiovascular Events and this Risk is not Addressed Sufficiently. Eur J Vasc Endovasc Surg. 2017;53(2):255–60.
Earnshaw JJ, Lees T. Update on Screening for Abdominal Aortic Aneurysm. Eur J Vasc Endovasc Surg. 2017;54(1):1–2.
Saratzis A, Dattani N, Brown A, Shalhoub J, Bosanquet D, Sidloff D, et al. Multi-Centre Study on Cardiovascular Risk Management on Patients Undergoing AAA Surveillance. Eur J Vasc Endovasc Surg. 2017;54(1):116–22.
Bath MF, Gokani VJ, Sidloff DA, Jones LR, Choke E, Sayers RD, et al. Systematic review of cardiovascular disease and cardiovascular death in patients with a small abdominal aortic aneurysm. Br J Surg. 2015;102(8):866–72.
Davis M, Harris M, Earnshaw JJ. Implementation of the National Health Service Abdominal Aortic Aneurysm Screening Program in England. J Vasc Surg. 2013;57(5):1440–5.
Earnshaw JJ. Triumphs and tribulations in a new national screening programme for abdominal aortic aneurysm. Acta Chir Belg. 2012;112(2):108–10.
Glover MJ, Kim LG, Sweeting MJ, Thompson SG, Buxton MJ. Cost-effectiveness of the National Health Service Abdominal Aortic Aneurysm Screening Programme in England. Br J Surg. 2014;101(8):976–82.
Saratzis A, Dattani N, Brown A, Shalhoub J, Bosanquet D, Sidloff D, et al. Multi-Centre Study on Cardiovascular Risk Management on Patients Undergoing AAA Surveillance. Eur J Vasc Endovasc Surg. 2017;54(1):116–22.
Saratzis A, Jaspers NEM, Gwilym B, Thomas O, Tsui A, Lefroy R, et al. Observational study of the medical management of patients with peripheral artery disease. Br J Surg. 2019;106(9):1168–77. https://doi.org/10.1002/bjs.11214.
Wanhainen A, Verzini F, Van Herzeele I, Allaire E, Bown M, Cohnert T, et al. Editor’s Choice - European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur J Vasc Endovasc Surg. 2019;57(1):8–93.
Chaikof EL, Dalman RL, Eskandari MK, Jackson BM, Lee WA, Mansour MA, et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018;67(1):2-77 e2.
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ (Clinical research ed). 2021;374:n2061.
Bartholomew Eldredge LK, Markham CM, Ruiter RA, Fernández ME, Kok G, Parcel GS. Planning health promotion programs: an intervention mapping approach. Hoboken, New Jersey: John Wiley & Sons; 2016.
Greaves CJ, Sheppard KE, Abraham C, Hardeman W, Roden M, Evans PH, et al. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health. 2011;11:119.
Schwarz PEH, Timpel P, Harst L, Greaves CJ, Ali MK, Lambert J, et al. Blood Sugar Regulation for Cardiovascular Health Promotion and Disease Prevention: JACC Health Promotion Series. J Am Coll Cardiol. 2018;72(15):1829–44.
Keyworth C, Nelson PA, Chew-Graham CA, Kane K, Pearce CJ, Griffiths CE, et al. Communicating Cardiovascular Disease Risk to People with Psoriasis: What Techniques do Practitioners Use? Int J Behav Med. 2016;23(2):168–78.
Nelson PA, Kane K, Chisholm A, Pearce CJ, Keyworth C, Rutter MK, et al. “I should have taken that further” - missed opportunities during cardiovascular risk assessment in patients with psoriasis in UK primary care settings: a mixed-methods study. Health Expect. 2016;19(5):1121–37.
Varela-Mato V, Caddick N, King JA, Yates T, Stensel DJ, Nimmo MA, et al. A Structured Health Intervention for Truckers (SHIFT): A Process Evaluation of a Pilot Health Intervention in a Transport Company. J Occup Environ Med. 2018;60(4):377–85.
National Institute for Health and Care Excellence. Cardiovascular disease prevention. 2010.
National Institute for Health and Care Excellence. Behaviour change: general approaches. 2007.
NICE. Behaviour change: the principles for effective interventions. In: Excellance NIfHaC, editor. 2014.
NICE NIfHaSCE. Non-surgical interventions for slowing aneurysm growth and reducing the risk of rupture: Abdominal aortic aneurysm: diagnosis and management: Evidence review. 2020.
NICE NIfHaSCE. Cardiovascular disease: risk assessment and reduction, including lipid modification. 2016.
Piepoli MF, Corrà U, Adamopoulos S, Benzer W, Bjarnason-Wehrens B, Cupples M, et al. Secondary prevention in the clinical management of patients with cardiovascular diseases. Core components, standards and outcome measures for referral and delivery: a policy statement from the cardiac rehabilitation section of the European Association for Cardiovascular Prevention & Rehabilitation. Endorsed by the Committee for Practice Guidelines of the European Society of Cardiology. Eur J Prev Cardiol. 2014;21(6):664–81. https://doi.org/10.1177/2047487312449597.
Carey RN, Connell LE, Johnston M, Rothman AJ, de Bruin M, Kelly MP, et al. Behavior Change Techniques and Their Mechanisms of Action: A Synthesis of Links Described in Published Intervention Literature. Ann Behav Med. 2019;53(8):693–707.
Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008;27(3):379.
Johnston M, Carey RN, Connell Bohlen LE, Johnston DW, Rothman AJ, de Bruin M, et al. Development of an online tool for linking behavior change techniques and mechanisms of action based on triangulation of findings from literature synthesis and expert consensus. Translat Behav Med. 2020;11(5):1049–65.
Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95.
Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789–95.
Dorresteijn JA, Visseren FL, Wassink AM, Gondrie MJ, Steyerberg EW, Ridker PM, et al. Development and validation of a prediction rule for recurrent vascular events based on a cohort study of patients with arterial disease: the SMART risk score. Heart. 2013;99(12):866–72.
Oliver-Williams C, Sweeting MJ, Jacomelli J, Summers L, Stevenson A, Lees T, et al. Safety of Men With Small and Medium Abdominal Aortic Aneurysms Under Surveillance in the NAAASP. Circulation. 2019;139(11):1371–80.
Tomee SM, Bulder RMA, Meijer CA, van Berkum I, Hinnen JW, Schoones JW, et al. Excess Mortality for Abdominal Aortic Aneurysms and the Potential of Strict Implementation of Cardiovascular Risk Management: A Multifaceted Study Integrating Meta-Analysis, National Registry, and PHAST and TEDY Trial Data. Eur J Vasc Endovasc Surg. 2023;65(3):348–57.
Bath MF, Saratzis A, Saedon M, Sidloff D, Sayers R, Bown MJ. Patients with Small Abdominal Aortic Aneurysm are at Significant Risk of Cardiovascular Events and this Risk is not Addressed Sufficiently. Eur J Vasc Endovasc Surg. 2017;53(2):255–60.
Saratzis A, Jaspers NEM, Gwilym B, Thomas O, Tsui A, Lefroy R, et al. Observational study of the medical management of patients with peripheral artery disease. Br J Surg. 2019;106(9):1168–77.
Michie S, Atkins L, West R. The behaviour change wheel: A guide to designing interventions. 2014.
Acknowledgements
The research was funded in whole by the National Institute for Health and Care Research (NIHR) Academy (reference: NIHR300059) and sponsored independently by the University of Leicester (reference: 0479); the funder and sponsor had no input in data collection, analysis or interpretation.
Funding
The research was funded by the National Institute for Health and Care Research (NIHR) Academy (reference: NIHR300059) and sponsored by the University of Leicester (reference: 0479); the funder and sponsor had no input in data collection, analysis or interpretation.
Author information
Authors and Affiliations
Contributions
TW, CG, MB and AS run the focus groups. TW analysed the focus group data with the support of CG. TW and CG drafted the first version of the developed intervention with the support of AS. All authors reviewed and further developed the intervention. TW with the support of AS drafted the initial manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was approved by the NHS Wales Research Ethics Committee 7 (NHS Wales REC 7) and the NHS Health Research Authority (HRA) in January 2020 (reference: 19/EM/0366). Informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix 1.
Scaffolding Questionaire.
Additional file 2: Appendix 2.
Topic Guide.
Additional file 3: Appendix 3.
Risk Factor letter.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Withers, T.M., Greaves, C.J., Bown, M.J. et al. Improving cardiovascular health in patients with an abdominal aortic aneurysm: development of the cardiovascular risk reduction in patients with aneurysms (CRISP) behaviour change intervention. Pilot Feasibility Stud 10, 17 (2024). https://doi.org/10.1186/s40814-024-01445-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40814-024-01445-z