Abstract
Background
The prevalence of low back pain increases with age and has a profound impact on physical and psychosocial health. With increasing age comes increasing comorbidity, and this also has pronounced health consequences. Whilst exercise is beneficial for a range of health conditions, trials of exercise for low back pain management often exclude older adults. It is currently unknown whether an exercise program for older adults with low back pain, tailored for the presence of comorbidities, is acceptable for participants and primary healthcare providers (PHCPs). Therefore, this mixed-methods study will assess the feasibility of an 8-week comorbidity-adapted exercise program for older people with low back pain and comorbid conditions.
Methods
The 3-phased feasibility study will be performed in a primary healthcare setting. PHCPs will be trained to deliver a comorbidity-adapted exercise program for older people with low back pain and comorbidities. Healthcare-seeking adults > 65 will be screened for eligibility over telephone, with a recruitment target of 24 participants. Eligible participants will attend an initial appointment (diagnostic phase). During this initial appointment, a research assistant will collect patient demographics, self-reported outcome measurement data, and perform a physical and functional examination to determine contraindications and restrictions to an exercise program. During the development phase, PHCPs will adapt the exercise program to the individual and provide patient education. During the intervention phase, there will be two supervised exercise sessions per week, over 8 weeks (total of 16 exercise sessions). Each exercise session will be approximately 60 min in duration. A qualitative evaluation after the last exercise program session will explore the feasibility of the exercise program for participants and PHCPs. Progression criteria will determine the suitability for a fully powered randomised controlled trial.
Discussion
This mixed-methods feasibility study will assess an exercise program for older adults with low back pain and comorbidities. Once assessed for feasibility, the exercise program may be tested for effectiveness in a larger, fully powered randomised controlled trial. This information will add to the sparse evidence base on appropriate options for managing back pain in older adults.
Trial registration
Australian and New Zealand Clinical Trials Registry registration number: ACTRN12621000379819p (06/04/2021; https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12621000379819p).
Trial sponsor
Macquarie University, Department of Chiropractic, Faculty of Medicine, Health and Human Sciences, Macquarie University, NSW 2109, Australia.
Similar content being viewed by others
Background
Low back pain is the leading cause of disability worldwide, and the prevalence of low back pain increases over the lifespan with a peak prevalence observed around the ages of 80 to 89 years [1]. Low back pain has a profound impact on the physical and psychosocial health of an older adult. For example, one-fifth of older adults with low back pain cannot care for themselves at home or participate in family and social activities [2]. Additionally, one in every four people aged > 80 years will report moderate to severe low back pain, and people aged > 80 years are three times more likely to have high intensity low back pain than those aged 50–59 years [3]. Whilst numerous national guidelines suggest exercise as a first-line treatment for low back pain [4, 5], older adults with low back pain who visit a general practitioner are 50% less likely to be advised about exercise than younger patients [6].
Comorbid diseases are defined as “any distinct additional entity that has existed or may occur during the clinical course of a patient who has the index disease under study” [7]. Comorbidity may be the effect of medical diseases existing simultaneously, but independently of each other [8], or of diseases that may be related [9]. Research has shown that women with spinal pain were twice as likely to be overweight or obese, have diabetes, and nearly twice as likely to have pulmonary disease and cardiovascular comorbidity, than older women without spinal pain [10]. Furthermore, musculoskeletal conditions such as low back pain are associated with an increased risk of reporting multiple chronic health conditions [11]. Indeed, it is estimated that two-thirds of people aged over 65 years have two or more chronic health conditions [12]. The consequences of comorbidity in older adults include poorer prognosis and increased healthcare use [13]. For instance, with every additional (non-musculoskeletal) comorbidity, there is a 40% increase in the risk of developing persistent low back pain (OR: 1.4; 95% CI: 1.3 to 1.5) [14]. The widespread exclusion of participants with comorbidities in research is of great concern [15]. There is a need for future trials to evaluate the effectiveness of interventions for older adults who have low back pain and comorbidities.
Exercise has been shown to be beneficial for a wide range of conditions that are associated with ageing such as falls [16], frailty [17], and sarcopaenia [18], as well as comorbidities that co-occur with low back pain [19]. Yet, randomised controlled trials of exercise programs for acute and chronic low back pain often do not include older adults with comorbid conditions [20, 21].
Recently, a comorbidity-adapted exercise intervention was designed and tested for patients with knee osteoarthritis [22], showing that tailored exercise therapy provided significant improvements in pain and physical functioning, and that these improvements were of clinical relevance [23]. It is currently unknown whether an exercise program for older adults with low back pain, tailored for the presence of comorbidities, is acceptable for participants and primary healthcare providers (PHCPs) such as physiotherapists and chiropractors. Therefore, this mixed-methods study will assess the feasibility of a comorbidity-adapted exercise program for older people with back pain and comorbidities. Specific aims directly related to assessing the feasibility are as follows:
-
(1)
Determine the ability to recruit eligible older participants and report the retention rate.
-
(2)
Evaluate adherence to, and fidelity of, the comorbidity-adapted exercise intervention.
-
(3)
Assess the collection and completion of outcome measure data, as well as report adverse events.
-
(4)
Evaluate the acceptability of the exercise program to participants and PHCPs.
Methods
Design and setting
This protocol describes the design of a mixed-methods feasibility study of a COMorbidity-adapted Exercise program for low BACK pain in older adults (COMEBACK). The study will be conducted in a primary healthcare setting. Chiropractors and physiotherapists (PHCPs) with more than 5 years’ experience in back pain management and rehabilitation will deliver the exercise program. Four PHCPs will be trained in how to deliver the exercise program, via structured, in-person training prior to the development phase of the intervention. The study protocol conforms with the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) guidelines [24], with the SPIRIT checklist as Supplementary material 1 Furthermore, as it has been recently shown that exercise interventions for low back pain are poorly reported [25], the intervention has also been reported as per the Template for Intervention Description and Replication (TIDieR) [26] (Supplementary material 2), and the exercise program will comply with the i-CONTENT tool [27]. The study results will be reported according to the CONsolidated Standards Of Reporting Trials (CONSORT) statement extension for pilot and feasibility studies [28]. The trial was registered with the Australian and New Zealand Clinical Trials Registry, reference number: ACTRN12621000379819p (06/04/2021; https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12621000379819p. Ethical approval was granted by the Macquarie University Human Research Ethics Committee, reference number: 52021641028032. The trial resources are being funded by a Macquarie University Research Seeding grant; however, they have no role in study design, data collection, and analysis, interpretation of data, or writing of this manuscript.
Recruitment
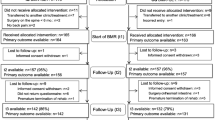
The study population is a convenience sample of adults aged 65 years or older who seek care for their low back pain in a primary healthcare setting. Older adults with low back pain will be invited to participate, via in-clinic posters in general practitioner, university, and PHCP clinics. The involvement of general practitioners in the recruitment process of participants in exercise interventions often needs to be supplemented by other recruitment methods [29], so social media posts will also invite community-dwelling older adults with low back pain to participate. Interested older adults will telephone a research assistant, who will screen for eligibility. If patients meet inclusion and exclusion criteria (Table 1), they will be asked to attend an initial appointment. At the appointment, the patient will be provided with a participant information form, and the study is explained verbally by the research assistant. If the patient is willing to participate, written consent will be obtained.
Participants
In determining the sample size for progression criteria for a pragmatic pilot randomised controlled trial, CTs using a red/amber/green approach, we used the estimation from Lewis et al. [32] with an upper limit red zone (unacceptable) of 45% and a lower limit green zone (acceptable) of 75% for the feasibility outcome protocol adherence (Table 2). The test is a 1-tailed test with suggested alpha (α) of 0.05 and beta (β) of 0.1 [32]. Therefore, our target sample size is 24 participants. Participants must have at least one of the following target comorbidities: coronary heart disease, hypertension, type 2 diabetes, obesity, chronic obstructive pulmonary disorder, and depression (diagnosed by a medical specialist). There will be no cost to participants to undertake the exercise program as part of the study.
Comorbidity-adapted exercise intervention
There will be three phases for the comorbidity-adapted exercise program: diagnostic, development, and intervention phases.
Diagnostic phase
After written informed consent, the research assistant will collect patient demographics (age, gender, marital status, weight, height, living arrangements, work history, education, highest degree, income, retirement status), medical history, and the participant’s pain history such as duration, trajectory, and symptomatology. A PHCP will then perform a physical and functional examination to determine contraindications and restrictions to an exercise program.
Development phase
The first exercise program session, provided by the trained PHCP, will involve a tailored session to adapt the exercise program to the older individual and provide patient education. The exercise program will consist of lower extremity and back extensor muscle-strength training, aerobic training, core stability exercises, balance training, and lower limb and back stretching based on an inventory. The details of the comorbidity-adapted exercise program are presented in Table 3. Adapting the exercise program for individual patients will include tailoring the exercise frequency, intensity, timing, and exercise type based on the presenting comorbid condition(s). Exercise adaptations will be based upon criteria developed from a previously conducted literature search by de Rooji et al. [23] that investigated restrictions, contraindications, and recommended adaptations of the target comorbidities. At this session, the PHCPs will provide patient education, explore the participant’s goals, motivations, and barriers to an exercise program, and provide the participant with paper-based GLA:D Back pain education material [33].
Intervention phase
The exercise program will consist of 16 exercise sessions over an 8-week program. There will be two supervised sessions per week with each session being approximately 60 min in duration. Sessions will be offered onsite at the Macquarie University, in a designated group exercise space. PHCPs will deliver multiple exercise sessions to participants within the program. The Borg Rate of Perceived Exertion scale will be used to monitor training intensity during each supervised exercise program session. Educational and coaching strategies will supplement the comorbidity-adapted exercise program throughout each supervised session [34], with adaptation to the exercise program patient directed.
Data collection
Data will be collected in person by the research assistant at baseline, 4 weeks, and at 8 weeks after the first exercise program session. Patient demographics and outcome measurement data will be collected in the REDCap — Research Electronic Data Capture system and exported to an Excel spreadsheet. De-identified data will then be imported to STATA/IC® (StataCorp, Texas) for analysis. Qualitative interviews will be performed at 8 weeks, and interview data will be stored securely and transcribed verbatim.
Feasibility measures
Predetermined progression criteria are the primary outcomes for this study. A traffic light system of green (go), amber (amend), and red (stop) will be used to determine progression of this feasibility study to a fully powered randomised controlled trial (Table 2) [35]. The study will not be feasible to progress if there are intractable issues that cannot be remedied [35].
Patient recruitment, retention, and intervention adherence
This study will determine how long it takes to recruit 24 participants, report how many older adults are screened, and how many meet eligibility criteria. Attendance will be recorded at each exercise session, by the PHCP. If a participant fails to attend an exercise session, the research assistant will contact the participant to record a reason for not attending the session and discuss additional support to attend future sessions to prevent dropout. Study retention rates will report the percentage of participants who complete the 8-week exercise program and provide complete data through follow-up. Data on adherence will be collected using a smartphone application. On completion of each exercise session, participants will scan a unique RedCap-generated QR code that will open a brief survey that will document the completion of the exercise session, completion of each component of the exercise session, and provide feedback on their exercise session adherence.
Barriers and facilitators for clinicians
One-on-one, semi-structured interviews will be held with PHCPs at the end of the exercise program to discuss the barriers and facilitators of delivering the exercise program.
Clinical measures
Clinical outcome measures and exercise program-specific outcomes will be collected at baseline (diagnostic phase), 4 weeks, and 8 weeks (post treatment) (Table 4). Outcome measures will include a physical and functional assessment performed by the PHCP and a self-reported questionnaire completed by the participants as suggested by the core outcome sets for low back pain [36] and multimorbidity [37].
Physical and functional assessment
The participant will perform the standing forward bending test, back extensor endurance test, and the trunk flexor endurance test. The sit-to-stand test will be performed to assess the functional capacity of participants [38]. Participants will be asked to sit in a chair and stand five times without the use of their arms as quickly as possible. This test will then be repeated, and an average test time will be calculated [39]. The 6-min walk test will be carried out by patients on a 30-m walkway to assess aerobic capacity and endurance. The distance covered over a time of 6 min is used as the outcome by which to compare changes in performance capacity. Patients will be instructed to walk their maximum distance in a 6-min period of time. The total distance covered in metres during 6 min of walking will be scored [6].
Self-reported outcome measures
Low back pain severity will be assessed using an 11-point numerical rating scale (NRS) ranging from 0 (no pain) to 10 (worst pain imaginable). Two severity questions will be asked at baseline, including current pain and average pain over the last week. Low back pain-related disability will be assessed using the Oswestry Disability Index (ODI). The ODI consists of 10 items representing different health constructs. The total score of the ODI is calculated by adding all scores of applicable items, dividing the obtained score by the maximal total score, and by multiplying the result by 100 to obtain a percentage score [40].
Health-related quality of life
The health-related quality of life will be measured using the EQ-5D-5L instrument. EQ-5D-5L is a generic instrument comprised of five questions about mobility, self-care, usual activities, pain and discomfort, and anxiety and depression, each measured on a 5-point scale from no problems to extreme problems. Australian EQ-5D-5L instrument scores are consistent with EQ-5D-5L utility and visual analog scores reported for other countries [41].
Illness burden
The Bayliss measure of illness burden is used to indicate how much illness affects the participant’s daily life and is measured using a 5-point scale for each individual condition and summed to a total score across conditions [42].
Mental health
The Hospital Anxiety and Depression score (HADS) will be used to measure anxiety and depression and has been validated across the lifespan [43]. It consists of 14 items, with scores that range between 0 and 21: scores from 0 to 7 are ‘normal’, from 8 to 10 ‘mild’, from 11 to 15 considered ‘moderate’, and from 16 to 21 ‘severe’ [44, 45].
Frailty
The Clinical Frailty Scale will be used to summarise the overall level of fitness or frailty of an older adult [46]. The scale is a way to summarise information from a clinical encounter with an older person, which is useful to screen for and quantify an individual’s overall health status [46].
Exercise program-specific outcomes
At 4 weeks and 8 weeks, global perceived effect and patient satisfaction data will be collected. Patients will be asked to rate perceived effectiveness on a scale of 1–9, with a score of 1 meaning much better, 5 meaning no change, and 9 meaning much worse [47]. Participant satisfaction with treatment will be measured using the numerical rating scale (0–10), with higher scores indicating greater satisfaction [48].
Comorbid conditions and adverse events
PHCPs and the research assistant will not monitor comorbid conditions regularly at exercise program sessions. The patient will continue their normal contact with their general practitioner and other healthcare professionals.
Adverse events
Adverse events are defined as any undesirable experience occurring during the study (regardless of whether this was related to the treatment) by the participant [49] and will be reported by both the participant and PHCP. Classification of adverse event severity is shown in Table 5. The PHCP will have a current first aid certificate and will record any adverse events that happen during the feasibility study period (8 weeks). Adverse events or discomfort experienced by participants during this study may relate to possible side effects from performing the exercise program. Participation in the exercise program may exacerbate individual comorbid condition(s), and some participants may also be at risk of falling. During the administration of the exercise program, should a severe exacerbation of a comorbid condition arise, an ambulance will be called, and the event will be documented in the patient’s file. There is also the possibility of uncovering an unexpected medical condition during the diagnostic phase of the exercise program. Should this arise, the participant will be referred to their general practitioner by the PHCP with a letter stating the relevant findings. In both cases, continuation in the study will be at the discretion of the participant and/or the participant’s general practitioner.
Changes in low back pain will be reported by participants via a daily SMS asking for a numerical ratings scale score (0–10) on the severity of their low back pain throughout the 8-week exercise program. If SMS data identifies an increase in low back pain, participants will be contacted to be asked whether they felt the exercise program may have caused an increase in low back pain. Additionally, the daily SMS will ask about any undesirable experiences related to the exercise program. If the SMS identifies an exacerbation of a comorbidity, the participant will be contacted to be asked about the nature of the adverse event.
Qualitative evaluation
After their last session, participants and PHCPs will be interviewed by a researcher with relevant qualitative expertise to explore the feasibility of the exercise program and barriers and facilitators to their participation.
Participant interviews
At the end of the study period, participants will be invited to take part in a one-on-one semi-structured interview to discuss the acceptability of the exercise program, fidelity of delivery, and the barriers and facilitators to adherence with the exercise program. Arrangements for the interview will be made at the time of the last exercise program session (8 weeks), with interviews carried out by a researcher who did not work with the delivery of the exercise program.
PHCP interviews
At the end of the exercise program, PHCPs responsible for administering the exercise program will be invited to take part in a one-on-one semi-structured interview to determine the degree to which the exercise program was delivered as intended (fidelity). They will also be asked to discuss the barriers and facilitators of delivering the exercise program to older adults with low back pain and comorbidities. The interviews will be carried out by a researcher who did not work with the delivery of the exercise program.
Analysis
The analysis will include a descriptive analysis and qualitative evaluation. Outcome measures change scores will be calculated by subtracting the postexercise program scores (8 weeks) from baseline scores and means with standard deviation (SD) and 95% confidence intervals (CI) reported. All one-on-one semi-structured interviews will be electronically recorded, transcribed, and imported into the NVivo data management program (NVivo qualitative data analysis software; QSR International Pty Ltd.). Transcripts will be coded to the domains of the Theoretical Domains Framework to extract the acceptability, barriers, and facilitators of the exercise program [50]. Transcripts will be coded systematically and iteratively until saturation is achieved. PHCP diaries will be reviewed to identify barriers to inform future trials.
Participant withdrawal
Participation is voluntary, and withdrawal from the study at any stage is at the discretion of the participant, and relationships with the study’s researchers, PHCPs, or Macquarie University will not be affected. The research assistant will notify the chief investigator if a participant wishes to withdraw from the trial, and the participant will be asked to complete and sign a withdrawal form. Providing reasoning for withdrawal is voluntary and will be documented. Participants will still be provided with their usual care from their general practitioner if they wish to withdraw from the study.
Data protection, storage, and dissemination
Participants will be provided with a unique identification code upon providing written informed consent. Quantitative data will be collected in REDCap, exported to an Excel spreadsheet, and then de-identified data will be imported to STATA/IC® (StataCorp, Texas) for analysis. The master dataset in Excel will be stored in a secure server, and access to the final dataset will be granted for the research team as required. Participant confidentiality will be maintained, and data will be non-identifiable in conference presentations and publications disseminating the study results. The full protocol will be made available via peer-review publication, and participant-level dataset will be made available via contacting the corresponding author.
Discussion
This protocol describes the rationale, design, and assessment for a comorbidity-adapted exercise program for older adults with low back pain. Although exercise is a recommended first-line treatment for low back pain, older adults are 50% less likely to be advised about exercise than younger patients [6]. Qualitative studies have revealed that a lack of professional guidance, inadequate distribution of information, and limited participation in physical activity programs are barriers to the uptake of exercise programs in older adults [51]. Similar to younger adults, motivation to engage in an exercise program is often a problem in older adults, which may be overcome by appropriate access to affordable, convenient, and stimulating exercise programs. Our study will use a qualitative evaluation to better understand barriers and facilitators to the uptake of exercise programs in older adults with low back pain. Importantly, in this study, the exercise program is developed to overcome physical limitations due to ageing and comorbidity. Older adults are twice as likely to have comorbidity if they have spinal pain [10] and often have pronounced health consequences due to comorbidity [52]; thus, the exercise program has been designed to be physiologically appropriate for older adults with low back pain and comorbidities. That is, that the exercise program is designed to be safe, acceptable, and will address the main impairments and functional limitations of older people. Other studies implementing standard exercise programs designed for younger adults with low back pain for older adults do not account for comorbidity that is present.
Results from this feasibility study will inform the design of an intervention for a large community-based randomised controlled trial. The fully powered trial will aim to investigate the long-term effects of an individualised, physiologically appropriate, exercise program on older people’s capacity to self-manage their low back pain, on low back-related disability, and the effect on specific comorbid conditions. If an exercise program appropriate for older adults with low back pain and comorbidities is found to be effective, further research would be needed to implement the exercise program in both primary care and community settings. This may result in improved health service delivery for older adults with low back pain and decreased healthcare expenditure in this population. With low back pain being the greatest cause of disability globally, and the prevalence of comorbid conditions increasing due to an ageing population whereby older adults have a higher number of comorbid conditions, research focused on older people with spinal pain and comorbidities is urgently needed.
Availability of data and materials
Not applicable.
Abbreviations
- AE:
-
Adverse events
- CI:
-
Confidence Interval
- CONSORT:
-
Consolidated Standards of Reporting Trials
- HADS:
-
Hospital Anxiety and Depression score
- NRS:
-
Numerical ratings scale
- OR:
-
Odds ratio
- ODI:
-
Oswestry Disability Index
- PHCPs:
-
Primary healthcare providers
- REDCap:
-
Research Electronic Data Capture
- RCTs:
-
Randomized controlled trials
- SPIRIT:
-
Standard Protocol Items: Recommendations for Interventional Trials
- TIDieR:
-
Template for Intervention Description and Replication
References
Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med. 2020;8(6):299.
Rudy TE, Weiner DK, Lieber SJ, Slaboda J, Boston JR. The impact of chronic low back pain on older adults: a comparative study of patients and controls. Pain. 2007;131(3):293–301.
Stewart Williams J, Ng N, Peltzer K, Yawson A, Biritwum R, Maximova T, et al. Risk factors and disability associated with low back pain in older adults in low- and middle-income countries. results from the WHO Study on global AGEing and adult health (SAGE). PLoS One. 2015;10(6):e0127880.
Stochkendahl MJ, Kjaer P, Hartvigsen J, Kongsted A, Aaboe J, Andersen M, et al. National Clinical Guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. Eur Spine J. 2018;27(1):60–75.
Qaseem A, Wilt TJ, McLean RM, Forciea MA, Denberg TD, Barry MJ, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–30.
Macfarlane GJ, Beasley M, Jones EA, Prescott GJ, Docking R, Keeley P, et al. The prevalence and management of low back pain across adulthood: results from a population-based cross-sectional study (the MUSICIAN study). Pain. 2012;153(1):27–32.
Feinstein AR. The pre-therapeutic classification of comorbidity in chronic disease. J Chronic Dis. 1970;23(7):455–68.
Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M. Defining comorbidity: implications for understanding health and health services. Ann Fam Med. 2009;7(4):357–63.
Jakovljević M, Ostojić L. Comorbidity and multimorbidity in medicine today: challenges and opportunities for bringing separated branches of medicine closer to each other. Psychiatr Danub. 2013;25:18–28.
de Luca KE, Parkinson L, Haldeman S, Byles JE, Blyth F. The relationship between spinal pain and comorbidity: a cross-sectional analysis of 579 community-dwelling, older Australian women. J Manipulative Physiol Ther. 2017;40(7):459–66.
Duffield SJ, Ellis BM, Goodson N, Walker-Bone K, Conaghan PG, Margham T, et al. The contribution of musculoskeletal disorders in multimorbidity: implications for practice and policy. Best Pract Res Clin Rheumatol. 2017;31(2):129–44.
National Guideline Centre (UK). Multimorbidity: assessment, prioritisation and management of care for people with commonly occurring multimorbidity. London: National Institute for Health and Care Excellence (UK); 2016.
Hartvigsen J, Natvig B, Ferreira M. Is it all about a pain in the back? Best Pract Res Clin Rheumatol. 2013;27(5):613–23.
Von Korff M, Crane P, Lane M, al. e. Chronic spinal pain and physical-mental comorbidity in the United States: results from the national comorbidity survey replication. Pain. 2005;113(3):331–9.
Van Spall HG, Toren A, Kiss A, Fowler RA. Eligibility criteria of randomized controlled trials published in high-impact general medical journals: a systematic sampling review. Jama. 2007;297(11):1233–40.
Sherrington C, Michaleff ZA, Fairhall N, Paul SS, Tiedemann A, Whitney J, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med. 2017;51(24):1750–8.
de Labra C, Guimaraes-Pinheiro C, Maseda A, Lorenzo T, Millán-Calenti JC. Effects of physical exercise interventions in frail older adults: a systematic review of randomized controlled trials. BMC Geriatr. 2015;15:154.
Vlietstra L, Hendrickx W, Waters DL. Exercise interventions in healthy older adults with sarcopenia: a systematic review and meta-analysis. Australas J Ageing. 2018;37(3):169–83.
Bricca A, Harris LK, Jäger M, Smith SM, Juhl CB, Skou ST. Benefits and harms of exercise therapy in people with multimorbidity: a systematic review and meta-analysis of randomised controlled trials. Ageing Res Rev. 2020;63:101166.
Cherkin DC, Deyo RA, Battié M, Street J, Barlow W. A comparison of physical therapy, chiropractic manipulation, and provision of an educational booklet for the treatment of patients with low back pain. N Engl J Med. 1998;339(15):1021–9.
Machado LA, Maher CG, Herbert RD, Clare H, McAuley JH. The effectiveness of the McKenzie method in addition to first-line care for acute low back pain: a randomized controlled trial. BMC Med. 2010;8:10.
de Rooij M, van der Leeden M, Avezaat E, Häkkinen A, Klaver R, Maas T, et al. Development of comorbidity-adapted exercise protocols for patients with knee osteoarthritis. Clin Interv Aging. 2014;9:829–42.
de Rooij M, van der Leeden M, Cheung J, van der Esch M, Häkkinen A, Haverkamp D, et al. Efficacy of tailored exercise therapy on physical functioning in patients with knee osteoarthritis and comorbidity: a randomized controlled trial. Arthritis Care Res (Hoboken). 2017;69(6):807–16.
Thabane L, Lancaster G. A guide to the reporting of protocols of pilot and feasibility trials. Pilot and Feasibility. Studies. 2019;5(37). https://doi.org/10.1186/s40814-019-0423-8.
Davidson SRE, Kamper SJ, Haskins R, Robson E, Gleadhill C, da Silva PV, et al. Exercise interventions for low back pain are poorly reported: a systematic review. J Clin Epidemiol. 2021;139:279-286.
Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. Bmj. 2014;348:g1687.
Hoogeboom TJ, Kousemaker MC, van Meeteren NL, Howe T, Bo K, Tugwell P, et al. i-CONTENT tool for assessing therapeutic quality of exercise programs employed in randomised clinical trials. Br J Sports Med. 2021;55(20):1153–60.
Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. Bmj. 2016;355:i5239.
Brach M, Moschny A, Bücker B, Klaaßen-Mielke R, Trampisch M, Wilm S, et al. Recruiting hard-to-reach subjects for exercise interventions: a multi-centre and multi-stage approach targeting general practitioners and their community-dwelling and mobility-limited patients. Int J Environ Res Public Health. 2013;10(12):6611–29.
Ren K. Grand challenges in musculoskeletal pain research: chronicity, comorbidity, immune regulation, sex differences, diagnosis, and treatment opportunities. Front Pain Res (Lausanne). 2020;1:575479. https://doi.org/10.3389/fpain.2020.575479.
WHO. ICD-11: International Statistical Classification of Diseases and Related Health Problems. 11th ed. World Health Organization; 2019.
Lewis M, Bromley K, Sutton CJ, McCray G, Myers HL, Lancaster GA. Determining sample size for progression criteria for pragmatic pilot RCTs: the hypothesis test strikes back! Pilot Feasibility Stud. 2021;7(1):40.
Kjaer P, Kongsted A, Ris I, Abbott A, Rasmussen CDN, Roos EM, et al. GLA:D(®) back group-based patient education integrated with exercises to support self-management of back pain- development, theories and scientific evidence. BMC Musculoskelet Disord. 2018;19(1):418.
de Rooij M, Steultjens MPM, Avezaat E, Häkkinen A, Klaver R, van der Leeden M, et al. Restrictions and contraindications for exercise therapy in patients with hip and knee osteoarthritis and comorbidity. Phys Ther Rev. 2013;18(2):101–11.
Avery KN, Williamson PR, Gamble C, O'Connell Francischetto E, Metcalfe C, Davidson P, et al. Informing efficient randomised controlled trials: exploration of challenges in developing progression criteria for internal pilot studies. BMJ Open. 2017;7(2):e013537.
Chiarotto A, Boers M, Deyo RA, Buchbinder R, Corbin TP, Costa LOP, et al. Core outcome measurement instruments for clinical trials in nonspecific low back pain. Pain. 2018;159(3):481–95.
Smith SM, Wallace E, Salisbury C, Sasseville M, Bayliss E, Fortin M. A Core Outcome Set for Multimorbidity Research (COSmm). Ann Fam Med. 2018;16(2):132–8.
Andersson EI, Lin CC, Smeets RJ. Performance tests in people with chronic low back pain: responsiveness and minimal clinically important change. Spine. 2010;35(26):E1559–E63.
Simmonds MJ, Olson SL, Jones S, Hussein T, Lee CE, Novy D, et al. Psychometric characteristics and clinical usefulness of physical performance tests in patients with low back pain. Spine. 1998;23(22):2412–21.
Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25(22):2940–53.
McCaffrey N, Kaambwa B, Currow DC, Ratcliffe J. Health-related quality of life measured using the EQ-5D-5L: South Australian population norms. Health Qual Life Outcomes. 2016;14(1):133.
Bayliss EA, Ellis JL, Steiner JF. Seniors’ self-reported multimorbidity captured biopsychosocial factors not incorporated into two other data-based morbidity measures. J Clin Epidemiol. 2009;62:550–7.
Spinhoven P, Ormel J, Sloekers PP, Kempen GI, Speckens AE, Van Hemert AM. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27(2):363–70.
Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–70.
Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. Cmaj. 2005;173(5):489–95.
Kamper SJ, Ostelo RW, Knol DL, Maher CG, de Vet HC, Hancock MJ. Global perceived effect scales provided reliable assessments of health transition in people with musculoskeletal disorders, but ratings are strongly influenced by current status. J Clin Epidemiol. 2010;63(7):760–6. e1.
Hartrick CT, Kovan JP, Shapiro S. The numeric rating scale for clinical pain measurement: a ratio measure? Pain Pract. 2003;3(4):310–6.
Atkinson TM, Li Y, Coffey CW, Sit L, Shaw M, Lavene D, et al. Reliability of adverse symptom event reporting by clinicians. Qual Life Res. 2012;21(7):1159–64.
Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care. 2005;14(1):26–33.
Bethancourt HJ, Rosenberg DE, Beatty T, Arterburn DE. Barriers to and facilitators of physical activity program use among older adults. Clin Med Res. 2014;12(1-2):10–20.
Divo MJ, Martinez CH, Mannino DM. Ageing and the epidemiology of multimorbidity. Eur Respir J. 2014;44(4):1055–68.
Acknowledgements
STS is currently funded by a program grant from the Region Zealand (Exercise First) and two grants from the European Union’s Horizon 2020 research and innovation program, one from the European Research Council (MOBILIZE, grant agreement no. 801790) and the other under grant agreement no. 945377 (ESCAPE). MLF is funded by the National Health and Medical Research Council of Australia.
Funding
The authors would like to acknowledge the receipt of the competitively awarded Macquarie University Seeding grant (AUD $24,964). The funders were not involved in the design of the study or writing of this manuscript. They will not be involved with data collection and analysis, or interpretation of data from the study.
Author information
Authors and Affiliations
Contributions
KD, MF, and SBZ were involved in the concept of the study. All authors were involved in the design of the study, with KD and MY actively developing the exercise program content. KD and AD supervise the Master of Research student MY. All authors provided substantial intellectual revision of the content of this manuscript and gave their final approval of the version of the manuscript to be submitted. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was granted by the Macquarie University Human Research Ethics Committee, Reference No: 52021641028032.
Consent for publication
Not applicable.
Competing interests
STS is associate editor of the Journal of Orthopaedic & Sports Physical Therapy and has received grants from the Lundbeck Foundation, personal fees from Munksgaard, all of which are outside the submitted work. He is co-founder of the Good Life with Osteoarthritis in Denmark (GLA:D®), a not-for profit initiative hosted at the University of Southern Denmark aimed at implementing clinical guidelines for osteoarthritis in clinical practice. JH is chief investigator or coinvestigator on multiple previous and current research grants from government research agencies and charities in Denmark and internationally. His travel expenses have been covered when he has been invited speaker at conferences, and he has received honoraria for talks, reviewing of grants, and theses. He is codeveloper of the GLA:D Back program, a not-for profit initiative hosted at the University of Southern Denmark aimed at implementing clinical guidelines for persistent back pain in clinical practice. SBZ is associate editor of the Osteoarthritis and Cartilage; received grants from the Netherlands Organisation for Health Research and Development, CZ, European Union, Foreum, and Dutch Arthritis Association; and received consultancy fee from Pfizer and from Infirst Healthcare. The other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary material 1
. SPIRIT 2013 Checklist: Recommended items to address in a clinical trial protocol and related documents.
Additional file 1: Supplementary material 2.
Template for Intervention Description and Replication (TIDieR).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
de Luca, K., Yanz, M., Downie, A. et al. A mixed-methods feasibility study of a comorbidity-adapted exercise program for low back pain in older adults (COMEBACK): a protocol. Pilot Feasibility Stud 8, 133 (2022). https://doi.org/10.1186/s40814-022-01097-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40814-022-01097-x