Abstract
Background
People with advanced cancer need to balance their resources and energy in order to experience enjoyment and quality of life in the time they have left. A resource-oriented intervention is developed targeting these aspects. The present protocol presents a feasibility study of this resource-oriented intervention in people with advanced cancer.
Methods
A feasibility study with a repeated-measurement design without a control group will be conducted at the research clinic of REHPA, the Danish Knowledge Center for Rehabilitation and Palliative Care. Data will be gathered at baseline, during and after a 5-day residential stay, after 6 weeks, during a 2-day follow-up stay and after 12 weeks. In total, 20–25 home-living adults (≥ 18 years) with advanced cancer reporting needs in everyday life will be recruited. The intervention consists of workshops and engagement in physical and creative everyday activities provided by a multidisciplinary team.
Outcome measures are quality of life, physical function and fatigue, which will be assessed using the European Organisation for Research and Treatment of Cancer Quality-of-Life Questionnaire Core-30. Balance in everyday activities will be assessed using the Occupational Balance Questionnaire.
Feasibility data will also be collected regarding (1) fidelity, (2) adherence, (3) dose and (4) reach and mechanisms of impact. For exploration of mechanism of impact, participant observations and focus group interviews will be used.
Discussion
This study presents a new approach in rehabilitation and palliative care aimed at supporting people with advanced cancer; instead of identification of problems, the present resource-oriented palliative rehabilitation intervention will target people’s resources, enhancing balance in everyday activities and underpinning enjoyment and quality of life. The results from the feasibility study can inform ways in which to support the everyday life of people with advanced cancer and thus have potential to improve their quality of life. The long-term perspectives are to evaluate the intervention in terms of effect, process and cost-effectiveness. This will provide evidence to adjust the content of rehabilitation and palliative care for this group of people.
Trial registration
Name of the registry: Balance, Activity and Quality of Life (BAL)
Date of registry: February 26, 2021
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Key messages regarding feasibility
-
The content, delivery and outcomes of a newly developed resource-oriented intervention for people with advanced cancer should be feasibility tested.
-
The present study presents a protocol for a feasibility study evaluating a resource-oriented intervention.
-
The present feasibility study may contribute with important knowledge to further develop the contents and delivery of a resource-oriented palliative rehabilitation intervention.
Background
People with advanced cancer wish to manage everyday activities and experience enjoyment in their everyday lives [1, 2]. Furthermore, they want to prioritise spending time with their families (social activities and relations), to remain mobile and to participate in community and recreative activities to the extent possible [3,4,5]. Committing to and participating in these activities are of great importance, enhancing feelings of autonomy, dignity and well-being [6,7,8].
Research shows that people with advanced cancer often suffer from fatigue and find it difficult to prioritise their energy and strength in a manner allowing them to manage activities that are important to them and to achieve a balanced mix of everyday activities [3, 4, 8]. Balancing everyday activities is defined as the subjective experience of having achieved the right mix (amount and variation) of activities in one’s activity pattern [9]. A cross-sectional study by Wæhrens et al. showed that people with advanced cancer spent most of their time on managing activities of daily living, leaving less energy and strength for other joyful everyday activities [4]. Social and physical activities may contribute to enjoyment, i.e. by engaging in craft, listening to music and being and walking in the nature. These activities are important because they can divert attention from illness and problems and contribute to enjoyment and quality of life [10, 11]. A process evaluation from a full-scale randomized controlled trial (RCT) found that people with advanced cancer had a preference for interventions that focus on their resources and contribute to enjoyment than interventions focusing on problems and activities they can no longer conduct [12]. This is in line with findings from a pilot study, which showed that people with advanced cancer wanted more enjoyment and lightness in their everyday lives [1]. Collectively, current literature underscores the need to develop interventions that enhance balance in everyday activities and underpin enjoyment and quality of life despite life-limiting illness.
To date, neither rehabilitation nor palliative care efforts have focused on ensuring a balanced mix of everyday activities for this group of people or on how enjoyment can be facilitated [13, 14]. Only a RTC by Nottelman et al. reported a borderline effect on quality of life of a palliative rehabilitation intervention in people with advanced cancer and their relatives [15]. The intervention consisted of two mandatory consultations with a palliative physician and a nurse and a 12-week group-based intervention programme comprising a patient/caregiver school and individual physical training [15]. The patient/caregiver education included sessions, which lasted approximately 1 h where patient and caregiver exchanged personal experiences with different topics like fatigue, body and movement, coping with the patient role and rest and relaxation. The participants reported that the group-based intervention with physical exercise and symptom education made a positive difference in their social and physical well-being [15]. The intervention, however, focused on problems rather than resources and thus failed to pay attention to the elements that contribute to enjoyment in everyday life. A RCT study by Gomersall et al. evaluated an individually tailored, text message-enhanced rehabilitation intervention and found it to be feasible and acceptable in people with cancer and survivors [16]. However, the focus was predominantly on promoting physical activity behaviour than supporting a better balance in everyday activities and providing enjoyment in their everyday life [16]. Two other RCT studies aiming to enhance everyday activities demonstrated that prioritisation of resources and activities was among the most frequently used intervention components among persons with advanced cancer [17, 18]. In order to underpin an expedient balance of everyday activities and resources, it is decisive to change daily activity patterns (habits and routines) [19] so that activities that enhance enjoyment and quality of life may be prioritised. Additionally, extensive evidence shows that physical activity may enhance energy levels, increase physical capacity and enhance quality of life [20, 21]. To our knowledge, no previous studies have reported on interventions that support a better balance in everyday activities in people with advanced cancer.
An intervention for people with advanced cancer that targets balance in everyday activities calls for a complex intervention that integrates rehabilitation and palliative care principles by ensuring that the patient’s functional level is maintained while also providing the required relief and support [22, 23]. The Medical Research Council (MRC) guideline describes a circular and iterative process comprising four phases: (1) development, (2) feasibility, (3) evaluation and (4) implementation [19]. Involvement of stakeholders in all phases is recommended in order to maximise the intervention’s potential impact [24]. We developed version 1.0 of a resource-oriented palliative rehabilitation intervention. This intervention combines rehabilitation and palliative care principles and was developed based on extant research [15, 17, 18, 20, 21, 25], existing clinical experiences [1, 26] and input from a panel of users including people with cancer and advanced cancer and relevant healthcare professionals.
The present paper outlines the protocol for a feasibility study that will test contents and delivery of a resource-oriented palliative rehabilitation intervention in people with advanced cancer [27]. The following questions will be addressed:
Contents and delivery of the intervention
-
1)
Which intervention sessions are particularly relevant in the experience of the participants and the healthcare professionals?
-
2)
How do the participants experience, interact and respond to receiving a resource-oriented palliative rehabilitation intervention?
-
3)
Fidelity, adherence, dose and reach of version 1.0 of the intervention manual
-
a)
Fidelity: Do the healthcare professionals deliver the intervention as planned? And do the healthcare professionals find that they have sufficient knowledge about the intervention?
-
b)
Adherence: Are the participants able to participate in the intervention (the individual sessions)?
-
c)
Dose: Which sessions were offered and what was the overall time expenditure?
-
d)
Reach: What characterises the group that received the intervention?
-
a)
-
4)
Are changes observed in the participant’s quality of life, balance in everyday activities, physical function and fatigue after having received a resource-oriented palliative rehabilitation intervention?
Outcomes and instruments
-
5)
Which outcomes were not completed sufficiently (missing data)?
Methods/design
Trial design and setting
A feasibility study with a repeated-measurement design without a control group will be conducted at the research clinic of REHPA, the Knowledge Center for Rehabilitation and Palliation (in Danish language: REHPA, Videncenter for Rehabilitering og Palliation). REHPA is part of Odense University Hospital, Denmark. The REHPA research clinic offers residential intervention stays for people with life-threatening illness. A residential intervention stay typically consists of a 5-day stay followed by a 2-day follow-up stay approximately 12 weeks later. Since the feasibility study is to be conducted at the REHPA research clinic, a similar structure for the intervention informed the present study. We also know from existing research that 12 weeks of intervention are appropriate for people with advanced cancer since they have a shorter life expectancy [15, 17, 18]. The clinical staff at REHPA is comprised, among others, of occupational therapists and physiotherapists, nurses, physicians, social workers and psychologists. In May 2021 and October 2021, two innovative stays were offered that are different from the standard stays otherwise offered by REHPA [26]. In these innovative stays, the present resource-oriented palliative rehabilitation intervention was tested among people with advanced cancer. Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT statements) were employed in the preparation of this protocol [28].
Eligibility criteria
Participants need to meet the following inclusion criteria:
-
Adult (≥ 18 years) and residing in his or her own home
-
Has chronic or advanced cancer
-
Experiences a need for support to manage everyday activities and to enhance the balance between various activities and tasks of daily living, e.g. enhance the balance between necessary activities and activities that produce enjoyment and meaningfulness
-
Is able to participate in the course and willing to complete questionnaires and participate in interviews
-
Must be independent with respect to personal activities of daily living (personal care, dressing and eating)
-
Speaks and understands Danish language
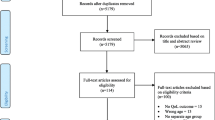
Recruitment
REHPA will prepare participant information, which will be sent to all palliative teams at hospitals, relevant municipalities, patient associations and cancer counselling services. In addition, the participant information will also be made available on REHPA’s web site and social media like LinkedIn and Facebook. The general practitioner or oncologist at the hospitals will assess potential participants based on the above-listed inclusion and exclusion criteria and will refer them to a REHPA stay if they fulfil these criteria. A responsible clinical healthcare worker will then in collaboration with the group of researchers decide who is eligible for a stay. Potential participants will receive detailed verbal and written information about the study. Prior to inclusion, the study participants are to provide written informed consent.
Interventions
The “template for intervention description and replication” (TIDieR) checklist will be used to describe the intervention [29]. The intervention will be implemented as two residential REHPA stays consisting of a 5-day stay with subsequent half-way contact and a 2-day follow-up stay after 6 weeks.
The intervention will target peoples’ resources, enhance balance in everyday activities and underpin enjoyment and quality of life. The intervention is structured much like standard REHPA stays with a combination of group presentations and activities [26]. In order to underpin the focus on balance, activity, enjoyment and quality of life, the intervention comprises the following sessions:
-
1)
Introduction to activity, balance and everyday life
-
2)
Introduction to “Walk to get happy”— activities in nature
-
3)
My everyday routine and activities: introduction to diaries
-
4)
Balancing resources, fatigue and energy — how to?
-
5)
My everyday life — balance, challenges and enjoyment
-
6)
“Walk to get happy” — activities in nature
-
7)
Life in movement
-
8)
Yoga
-
9)
Meaningful activities: what makes you happy?
-
10)
Creative expression
-
11)
Relaxing massage: “be good to yourself”
-
12)
Values and action plan
-
13)
“Developments since the previous session”
-
14)
Life in movement — family, friends and network
-
15)
Body and movement
Thus, a total of 15 sessions are planned during the 5-day stay and 2-day follow-up stay combined. Each session has a duration of 45–150 min. Additionally, two individual conversations are offered at both stays and one optional session during the 2-day stay, the contents of which is determined by the participants. An optional half-way follow-up telephone contact is also offered to the participants. The sessions are imparted by a multidisciplinary team consisting of a nurse, an occupational therapist, a physiotherapist, a medical trained artist, a mindfulness coach and a social worker. The intervention is primarily group-based, and all 15 sessions are mandatory (See Table 1). If participants are absent from the mandatory sessions, this will be recorded as not being adherent to the protocol and will be registered in an intervention logbook (more information is provided under data collection). See Table 2 for more details about the sessions. At the 2-day follow-up stay, an optional session is offered to the participants of which they determine the content. On the last day at the 5-day stay, a healthcare professional asks the participants about their wishes to the content of the optional session.
Furthermore, the participants will also be offered to participate in the following evening activities:
-
Music and singing
-
Everyday life and existence
The evening activities are not sessions part of the present resource-oriented palliative rehabilitation intervention but are optional activities that are offered to the participants two times during the 5-day stay. The evening activities are led by a professional singer and a priest. These activities have a duration of 1 and half hour.
In the beginning of the course, the focus is on getting to know each other and learning about each other’s everyday life. Subsequently, the participants become engaged in various activities. Towards the end of the course, an action plan is prepared in dialogue between the professionals and the participants describing how they can implement the elements that produced enjoyment in their everyday lives when they return home. The preparation of the action plan will, among others, be based on the participants’ diaries and their own priorities of what they want to do and how they prefer to structure their everyday lives to ensure sufficient energy and time for the activities that provide enjoyment and improve their quality of life. For that purpose, the time-geography method is used [30]. This involves working with a structured diary where everyday activity patterns are recorded along with perceptions of enjoyment and values, productivity and rest and the balance between these elements [30]. The diary needs to be completed before the 5-day stay and is used in session 3.
Theoretical framework for the intervention
The overall theoretical framework for the intervention is the WHO’s definition of palliative care [31] and the white book on the concept of rehabilitation (in Danish language) [32]. While palliative care focuses on relief of suffering, rehabilitation focuses on functional ability. Both concepts share the aim of enhancing quality of life [31, 32]. More specifically, the preparation of the intervention is inspired by the American philosopher, psychologist and learning theorist John Dewey [33]. Dewey describes learning as a social process of interaction that involves continuous transaction between action, activity and experience, where learning is furthered by the interplay between presentation/introduction of knowledge and experience-based perception [33]. Following Dewey, the acquisition of new knowledge/learning embraces the following five aspects: (1) experiences with activities that are relevant and of interest for the person, (2) challenges that are perceived as real/relevant, (3) introduction to necessary and relevant knowledge, (4) possible action strategies must be acknowledged or developed by the person, and (5) it must be possible to test ideas through action/activity and to bring them to practical use. On this basis, the intervention is established through interaction between sessions consisting of presentation of knowledge and workshops allowing the participants to test and engage in different activities. Additionally, each individual session is informed by theory about the topic in question [19, 26, 34, 35] and by knowledge from several of the previously mentioned studies that have combined/coordinated rehabilitation and palliative care [15, 18]. See Table 2 for more detailed description of the intervention.
Context/location
The intervention is implemented through stays at the REHPA research clinic, located on the 3rd floor of Nyborg Hospital, Denmark. The clinic was designed in accordance with principles of ‘architecture and relief”, including individual rooms with a shower and rest room for the participants. Furthermore, a dining room and two living rooms are available. The ground floor includes a gym, a classroom, a reception (the welcome area), a café area and several group rooms. REHPA is located in a recreational area characterised by natural beauty and easy access to walking or running, etc. by the ramparts of Nyborg Castle [26].
Data collection
Data will be collected at baseline (T1), during the 5-day residential stay (T2), after the 5-day stay has concluded (T3), before the follow-up stay at 6 weeks (T4), during the follow-up stay (T5) and after 12 weeks of follow-up (T6). Data at T2 and T5 is collected after each session for all participants. The following data collection methods will be used: (1) questionnaires, (2) focus group interviews and (3) participant observations.
Outcomes
Since the intervention aims to enhance the participants’ quality of life and balance in everyday activities through prioritisation of energy and strength, engagement in physical and meaningful and joyful activities, the following outcomes will be chosen: (1) quality of life, (2) balance in everyday activity, (3) physical function and (4) fatigue, collected at T1, T3, T4 and T6. The outcome questionnaires will be sent and filled out electronically by the participants using the Civil Registration System in Denmark and the Research Electronic Data Capture (REDCaP). Two written reminders will be sent 3 and 6 days after deadline. Then, a reminder will be conducted by phone.
Quality of life, physical function and fatigue
Quality of life, physical function and fatigue are measured using the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire Core-30 (EORTC QLQ-C-30). The EORTC QLQ-C-30 is a cancer-specific questionnaire containing 30 questions that address function as well as symptoms and quality of life. Answers are scored on an ordinal scale ranging from 1 to 4 (1 = not at all, 2 = a little, 3 = quite a bit, 4 = very much). Additionally, the questionnaire measures quality of life using an ordinal scale ranging from 1 to 7. Subsequently, the ordinal data are transformed into a score ranging from 0 to 100, where a higher score equals better function and higher quality of life or poorer experienced symptoms. The EORTC QLQ-C-30 was found to be valid, reliable and associated with high response rates among persons with advanced cancer [36].
Balance in everyday activities
The Occupational Balance Questionnaire (OBQ) is a generic questionnaire comprising a total of 11 items that provide an overall assessment of balance in everyday activities. The items assess in different ways the satisfaction with the amount of and variation in various everyday activities in which people become engaged. Each question is scored on a 4-step ordinal scale ranging from 1 = completely disagree to 4 = completely agree. Based on the 11 questions, a sum score ranging from 11 to 44 is calculated. A higher score indicates a better balance in everyday activities. The QBQ has be found to be valid and reliable [37, 38].
Quantitative feasibility data
An intervention logbook will be prepared that collects data about: (1) dose (duration and number of intervention sessions given) (T2 and T5), (2) if the contents were delivered as planned (fidelity) (T2 and T5), (3) if the participants were able to participate in the intervention sessions (adherence) (T2 and T5) and (4) the relevance of the intervention sessions (T2 and T5). The intervention logbook will be developed based on the guidance by O’Cathain et al. about feasibility studies [27]. We also record how many participated in the half-way follow-up. The healthcare professionals from the REHPA collect data from participants and among themselves and also state which intervention sessions were particularly relevant. All of these data are collected in the course of T1-T6 (see Table 3).
Data on reach will be collected based on the REHPA’s “How are you?” questionnaire [26] in which both demographics and patient-reported outcome (PRO) data will be employed to describe the group that received the intervention. See Table 3 for overview of the time line.
Qualitative feasibility data
Data on the participants’ experiences, interaction and responses to the intervention will be collected through participant observation and focus group interviews. Participant observation is conducted during the two stays to gain insight into the participants’ immediate reactions to and experience with the intervention and their interaction with the REHPA healthcare professionals. Furthermore, a structured observation table will be used to register expressions of flow and enjoyment while the participants are engaged in session 10. Focus group interviews will be conducted on the 5th day of the 5-day stay and again at the second stay in smaller 5–7 participant groups [39].
A focus group interview will be conducted with the healthcare professionals who imparted the intervention in order to collect their experiences and perceptions from this type of intervention [39].
Sample size
There are no requirements as to the number of participants needed in feasibility studies [40]. We deem that 20–30 persons will be sufficient to ensure that enough information about the contents of the intervention is collected and to explore potential changes over time in the chosen outcomes [40].
Analysis
Continuous, normally distributed data are analysed by mean and standard deviation (SD). Otherwise, medians and percentiles will be used. Ordinal data are analysed by medians and percentiles, whereas categorical data and dichotomous data are analysed using numbers and percentages. The number of missing answers in the outcome instruments is calculated and presented descriptively as numbers and percentages. Wilcoxon signed-rank test will be used to analyse changes from T1-T3, T1-T4, and again from T1-T6 with respect to quality of life, balance in everyday activities, physical function and fatigue. Furthermore, a responder analysis will be conducted to determine how many of the participants have achieved a clinically relevant change (5–10 points) [36]. This analysis will focus on quality of life, physical function and fatigue, where it is possible to establish a clinically relevant difference [36]. The significance level will be ≤ 0.05, and 95% confidence intervals will be presented. Analyses will be performed using STATA 16.
Qualitative data will be transcribed verbatim from interviews and field notes and analysed using thematic analysis [41]. First, all texts from participant observations and focus groups will be analysed separately through an iterative process of reading, identifying themes, rereading and collapsing themes into distilled themes of the core findings. The preliminary findings from the first round of analysis of both participant observations and focus groups will be discussed to identify themes across the data material, and final themes will be identified. For the purpose of process analysis, the identified themes will be further qualified by relevant theory.
Ethics
The study follows the principles of the Helsinki Declaration [42]. The scientific-ethical committee decided that no approval was required for this study (S-20210013). The study was approved by the Region of Southern Denmark Data Agency (R. no. 21/13073) and registered at ClinicalTrials.gov (NCT04772690). Data from the research database — rehabilitation and palliative care for cancer patients and others with life-threatening illness — have been approved and recorded with the Region of Southern Denmark: R. no. 18/27843. Oral and written consent will be obtained from all participants. Data will be collected electronically and stored in the REDCaP, a safe database administered by the Region of Southern Denmark. Any forms not collected electronically will be scanned and placed on a safe Sharepoint site. This also applies to audio files from the focus group interviews and written transcripts.
Discussion
This protocol for a feasibility study presents a new approach in rehabilitation and palliative care for supporting people with advanced cancer. Instead of a predominant focus on functional problems and suffering, the present resource-oriented palliative rehabilitation intervention will target the participants’ resources, enhance balance in everyday activities and underpin experiences of enjoyment. In particular, leisure activities seem to be bring enjoyment for people with advanced cancer while at the same time they can support functioning [43]. It is therefore important to assist people with advanced cancer in prioritising their energy on leisure activities rather using all their resources on self-care activities [3, 4], although these kind of activities also serve an important purpose [8]. The focus on a balanced mix of everyday activities is pivotal and may improve quality of life [2, 44]. From a theoretical perspective, balance in everyday activities is important as all human beings need a variety of everyday activities that offer desirable levels of pleasure, productivity and restoration [35]. Still, a crucial point seems to be the balance itself between activity on the one hand and restituation and relief on the other. While attention towards the positive aspects of life through a focus on resources and enjoyment may be highly needed for people with advanced cancer [1, 12, 43], it is equally important not to ignore the potential risk of overlooking the difficult and painful challenges of these peoples’ circumstances, requiring relief and supportive care.
The MRC guide recommends drawing on both clinical expertise and evidence when developing a new intervention [22]. The evidence base of the resource-oriented palliative rehabilitation intervention draws mainly on knowledge from the Cancer Home-Life Intervention [12, 18, 45,46,47] together with evidence about creative [11, 48] and physical activities [20, 21]. The Cancer Home-Life Intervention is an occupational therapy-based intervention aiming at enabling people with advanced cancer to perform and participate in the everyday activities at home that they prioritise but have difficulties performing [47]. The newly updated MRC framework has added some core elements to the existing model of how to develop and evaluate complex interventions. These elements are as follows: context, programme theory, identify key uncertainties, refine intervention, economic considerations and involvement of stakeholders. These elements should be considered throughout all the phases [24]. In particular, it may be highly important to involve stakeholders early in the development phase [24]. However, involvement of stakeholders requires careful consideration of how to identify and engage them in the process [24]. We identified stakeholders among REHPA’s user panel of people with life-threatening illness including advanced cancer. We presented the initial ideas to these stakeholders and obtained their opinions about the suggested ideas. Co-production is a recommended approach to intervention development, which means that relevant stakeholders are involved in the decision-making process together with the researchers [49]. Professionals who were involved in the intervention delivery were also consulted about the ideas, and they had the same level of decision-making powers as the researchers [49]. In co-production with the researchers, the professionals developed the manual for the present resource-oriented palliative rehabilitation intervention. Co-production may have pros and cons; it may reduce the gap between research and clinical practice and thus later encounter fewer implementation barriers [49]. The downside may be that it can affect the evidence base if the professionals’ points of view are getting to much influence on the contents, as some experiences might be based on old and ineffective ways to intervene [50]. Nevertheless, the value of the practitioners experience and knowledge is equally important as that of scientific evidence which accords the principle of evidence-based practice (scientific evidence, patient preferences and clinical knowledge) [51]. Overall, this illustrates the complexity and lengthy process when drawing on the MRC framework to develop and evaluate a complex intervention. However, the approach provides a robust and meticulous process from intervention development to implementation, which, in turn, can prevent important flaws and save resources.
Since the intervention is newly developed, several uncertainties remain. These uncertainties need to be tested and explored in a feasibility study before proceeding to a pilot and RCT study [24]. The present feasibility study will therefore contribute with important knowledge to further develop the contents of the resource-oriented palliative rehabilitation intervention. Following the present feasibility study, the next step will be to adjust the intervention and then perform a pilot study in Danish municipalities. The pilot study will test the final version of the intervention in the context in which it will be implemented. The main focus of the pilot study will be on methodological issues like recruitment and drop-out rate, randomisation and test procedures regarding data collection. Future perspectives are to evaluate the intervention for effect, process and cost-effectiveness.
Availability of data and materials
Data will be stored in REDCaP and on a safe Sharepoint site.
Abbreviations
- RCT:
-
Randomised controlled trial
- MRC:
-
Medical Research Council
- REHPA:
-
Danish Knowledge Centre for Rehabilitation and Palliative Care
- SPIRIT:
-
Standard Protocol Items: Recommendations for Interventional Trials
- TIDieR:
-
Template for intervention description and replication
- T1:
-
Baseline
- T2:
-
Collection of data during the 5-day residential stay
- T3:
-
Collection of data after end of the 5-day stay
- T4:
-
Collection of data before the follow-up stay at 7 weeks
- T5:
-
Collection of data during the follow-up stay
- T6:
-
Collection of data after 12 weeks of follow-up
- PRO:
-
Patient-reported outcome data
- OBQ:
-
Occupational Balance Questionnaire
- SD:
-
Standard deviation
- REDCaP:
-
Research Electronic Data Capture
- EORTC:
-
European Organisation for Research and Treatment of Cancer
References
Raunkiær M, Gärtner HS. Sammentænkning og koordinering af rehabilitering og palliation for mennesker med kronisk kræft [Linking and coordinating rehabilitation and palliative care for people with advanced cancer]. REHPA Notat. 2020, in press.
Peoples H, Nissen N, Brandt Å, et al. Belonging and quality of life as perceived by people with advanced cancer who live at home. J Occup Sci. 2018;25(2):200–13.
la Cour K, Nordell K, Josephsson S. Everyday lives of people with advanced cancer: activity, time, location, and experience. OTJR (Thorofare N J). 2009;29(4):154–62.
Wæhrens EE, Brandt Å, Peoples H, la Cour K. Everyday activities when living at home with advanced cancer: a cross-sectional study. Eur J Cancer Care. 2020;29(5):e13258.
Peoples H, Brandt Å, Waehrens EE, et al. Managing occupations in everyday life for people with advanced cancer living at home. Scand J Occup Ther. 2017;24(1):57–64.
Morgan DD, Currow DC, Denehy L, Aranda SA. Living actively in the face of impending death: constantly adjusting to bodily decline at the end-of-life. BMJ Support Palliat Care. 2017;7(2):179–88.
Sviden GA, Tham K, Borell L. Involvement in everyday life for people with a life threatening illness. Palliat Support Care. 2010;8(3):345–52.
von Post H, Wagman P. What is important to patients in palliative care? A scoping review of the patient’s perspective. Scand J Occup Ther. 2019;26(1):1–8.
Wagman P, Håkansson C, Björklund A. Occupational balance as used in occupational therapy: a concept analysis. Scand J Occup Ther. 2011;19(4):322–7.
la Cour K, Josephsson S, Tishelman C, Nygård L. Experiences of engagement in creative activity at a palliative care facility. Palliat Support Care. 2007;5(3):241–50.
Reynolds F, Prior S. The role of art-making in identity maintenance: case studies of people living with cancer. Eur J Cancer Care. 2006;15(4):333–41.
la Cour K, Oestergaard LG, Brandt, et al. Process evaluation of the Cancer Home-Life Intervention: what can we learn from it for future intervention studies? Palliat Med. 2020;34(10):1425–35.
Feldstein A, Lebel S, Chasen MR. An interdisciplinary palliative rehabilitation intervention bolstering general self-efficacy to attenuate symptoms of depression in patients living with advanced cancer. Support Care Cancer. 2016;24(1):109–17.
Payne C, Mcllfatrick S, Larkin P, et al. A qualitative exploration of patient and healthcare professionals’ views and experiences of palliative rehabilitation during advanced lung cancer treatment. Palliat Med. 2018;32(10):1624–32.
Nottelman L, Jensen LH, Vejlgaard TB, Groenvold M. A new model of early, integrated palliative care: palliative rehabilitation for newly diagnosed patients with non-resectable cancer. Support Care Cancer. 2018;27(9):3291–300.
Gomersall SR, Skinner TL, Winkler E, et al. Feasibility, acceptability and efficacy of a text message-enhanced clinical exercise rehabilitation intervention for increasing ‘whole-of-day’activity in people living with and beyond cancer. BMC Public Health. 2019;19(Suppl 2):542.
Lindahl-Jacobsen L. Occupational therapy for cancer patients - a randomised, controlled study. PhD [thesis]. Odense: University of Southern Denmark; 2014.
Pilegaard MS, la Cour K, Oestergaard LG, et al. The ‘Cancer Home-Life Intervention’: a randomisered controlled trial evaluating an occupational therapy-based intervention in people with advanced cancer. Palliat Med. 2018;32:744–56.
Taylor RR, editor. Kielhofner’s model of human occupation: theory and application, vol. xii. 5th ed. Philadelphia: Wolters Kluwer; 2017. p. 499.
Dittus KL, Gramling RE, Ades PA. Exercise interventions for individuals with advanced cancer: a systematic review. Prev Med. 2017;104:124–32.
Salakari MRJ, Surakka T, Nurminen R. Effects of rehabilitation among patients with advanced cancer: a systematic review. Acta Oncol. 2015;54(5):618–28.
Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655.
Padgett LS, Asher A, Cheville A. The intersection of rehabilitation and palliative care: patients with advanced cancer in the inpatient rehabilitation setting. Rehabil Nurs. 2018;43(4):219–28.
Skivington K, Matthews L, Simpson SA, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 2021;374:n2061.
Assing Hvidt E, Hvidt NC, Graven V, la Cour K, Rottmann N, Thomsen KF, et al. An existential support program for people with cancer: development and qualitative evaluation. Eur J Oncol Nurs. 2020;2020(46):101768.
Praksisbeskrivelser – Forskningsklinik REHPA. Standardforløb for mennesker med eller efter kræft [Description of practice - REHPAs’ Research Clinic. Standard courses for people with or after cancer]. 2020.
O’Cathain A, Hoddinott P, Lewin S, et al. Maximising the impact of qualitative research in feasibility studies for randomized controlled trials: guidance for researchers. Pilot Feasibility Stud. 2015;1(32):1–13.
Chan AW, Tetzaff JM, Altman DG, et al. SPIRIT 2013 Statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158:200–7.
Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687.
Ellegård K, Nordell K. Att byta vanmakt mot egenmakt. Stockholm: Johansson & Skyttmo Forlag AB; 1997.
World Health Organisation. WHO definition of palliative care; 2019. Available from: https://www.who.int/cancer/palliative/definition/en/.
Hvidbog om rehabiliteringsbegrebet – rehabilitering I Danmark [White book about the concept of rehabilitation – rehabilitation in Denmark]. Aarhus: MarselisborgCentret; 2004.
Dewey Society. Education and culture. Iowa City: University of Iowa; 1994.
Csikszentmihalyi M. Flow: the psychology of optimal experience. J Leis Res. 1990;24(1):93–4.
Christiansen C. Three perspectives on balance in occupation. In: Zemke R, Clark F, editors. Occupational science: the evolving discipline. Philadelphia: F.A. Davis Company; 1996.
Fayers PM, Aaronson NK, Bjordal K, et al. The EORTC QLQ-C30 Scoring Manual. 3th ed. Brussels: European Organisation for Research and Treatment of Cancer; 2001.
Wagman P, Håkansson C. Introducing the Occupational Balance Questionnaire (OBQ). Scand J Occup Ther. 2014;21(3):227–31.
Håkansson C, Wagman P, Hagell P. Construct validity of a revised version of the Occupational Balance Questionnaire. Scand J Occup Ther. 2020;27(6):441–9.
Kvale S, Brinkmann S. Introduktion til et håndværk [Introduction to a craft]. København: Hans Reitzels Forlag; 2009.
Billingham SA, Whitehead AL, Julious SA. An audit of sample sizes for pilot and feasibility trials being undertaken in the United Kingdom registered in the United Kingdom Clinical Research Network database. BMC Med Res Methodol. 2013;13:104.
Brinkmann S, Tanggard L. Kvalitative metoder – En grundbog [Qualitative methods – a textbook]. 3rd ed. København: Hans Reitzels Forlag; 2020.
Williams JR. The Declaration of Helsinki and public health. Bull World Health Organ. 2008;86(8):650–2.
Bentz H, Madsen SH, Pilegaard MS, Brandt Å, Offersen SMH, Oestergaard LG, et al. Occupations contributing to joy for people living with advanced cancer: a qualitative descriptive study. Br J Occup Ther. 2021; Epub ahead of print.
Wilcock AA, Chelin M, Hall M, Hamley N, Morrison B, Scrivener L, et al. The relationship between occupational balance and health: a pilot study. Occup Ther Inter. 1997;4(1):17–30.
Brandt A, Pilegaard MS, Oestergaard LG, et al. Effectiveness of the ‘Cancer Home-Life Intervention’ on everyday activities and quality of life in people with advanced cancer living at home: a randomised controlled trial and an economic evaluation. BMC Palliat Care. 2016;15:10.
Pilegaard MS, Oestergaard LG, la Cour K, et al. Subgroup effects of an occupational therapy-based intervention for people with advanced cancer. Scand J Occup Ther. 2020;27(7):517–23.
Lindahl-Jacobsen L, la Cour K, Oestergaard LG, et al. The Development of the ‘Cancer Home-Life Intervention’: an occupational therapy-based intervention programme for people with advanced cancer living at home. Scand J Occup Ther. 2021;28(7):542–52.
Kim KS, Loring S, Kwekkeboom K. Use of art-making intervention for pain and quality of life among cancer patients: a systematic review. J Holist Nurs. 2018;36(4):341–53.
O’Cathain A, Croot L, Duncan E, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open. 2019;9(8):1–9.
Eriksson C, Erikson A, Tham K, et al. Occupational therapists’ experiences of implementing a new complex intervention in collaboration with researchers: a qualitative longitudinal study. Scand J Occup Ther. 2017;24(2):116–25.
Sackett DL, Rosenberg WMC, Gray JAM, et al. Evidence based medicine: what it is and what it isn’t. BMJ. 1997;312:71.
Acknowledgements
The authors thank the participating patients for their interest in the project and for time used to fill out questionnaires and participate in interviews. Also, a special thanks to REHPA’s research clinic for the valuable input to the intervention and for providing the intervention during the intervention stay at REHPA. Finally, thanks to Birthe Kargaard Jensen and Tina Broby Mikkelsen for helping with the recruitment of participants and data collection.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: the Danish Cancer Society (R53-A2783) and REHPA and the Danish Knowledge Centre for Rehabilitation and Palliative Care funded the study.
Author information
Authors and Affiliations
Contributions
HT, KlC and MSP conceived the original idea of the project, sought and obtained funding. HT is the grant recipient. HT, KlC and MSP contributed to the design of the feasibility study. MSP, KlC, SBD, DSJ and HKB developed the intervention in co-production with other professionals. MSP is the daily project leader. A future PhD student will undertake all quantitative and qualitative data analyses. MSP wrote the manuscript with input from the other authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The scientific-ethical committee decided that no approval was required for this study (S-20210013), and the Region of Southern Denmark Data Agency approved the study (R. no. 21/13073). Consent will be provided by all included participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pilegaard, M.S., Timm, H., Birkemose, H.K. et al. A resource-oriented intervention addressing balance in everyday activities and quality of life in people with advanced cancer: protocol for a feasibility study. Pilot Feasibility Stud 8, 86 (2022). https://doi.org/10.1186/s40814-022-01038-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40814-022-01038-8