Abstract
Background
The impact of activity-related joint loading on cartilage is not clear. Abnormal loading is considered to be a mechanical driver of osteoarthritis (OA), yet moderate amounts of physical activity and rehabilitation exercise can have positive effects on articular cartilage. Our aim was to investigate the immediate effects of joint loading activities on knee and hip cartilage in healthy adults, as assessed using magnetic resonance imaging. We also investigated delayed effects of activities on healthy cartilage and the effects of activities on cartilage in adults with, or at risk of, OA. We explored the association of sex, age and loading duration with cartilage changes.
Methods
A systematic review of six databases identified studies assessing change in adult hip and knee cartilage using MRI within 48 h before and after application of a joint loading intervention/activity. Studies included adults with healthy cartilage or those with, or at risk of, OA. Joint loading activities included walking, hopping, cycling, weightbearing knee bends and simulated standing within the scanner. Risk of bias was assessed using the Newcastle–Ottawa Scale. Random-effects meta-analysis estimated the percentage change in compartment-specific cartilage thickness or volume and composition (T2 relaxation time) outcomes. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) system evaluated certainty of evidence.
Results
Forty studies of 653 participants were included after screening 5159 retrieved studies. Knee cartilage thickness or volume decreased immediately following all loading activities investigating healthy adults; however, GRADE assessment indicated very low certainty evidence. Patellar cartilage thickness and volume reduced 5.0% (95% CI 3.5, 6.4, I2 = 89.3%) after body weight knee bends, and tibial cartilage composition (T2 relaxation time) decreased 5.1% (95% CI 3.7, 6.5, I2 = 0.0%) after simulated standing within the scanner. Hip cartilage data were insufficient for pooling. Secondary outcomes synthesised narratively suggest knee cartilage recovers within 30 min of walking and 90 min of 100 knee bends. We found contrasting effects of simulated standing and walking in adults with, or at risk of, OA. An increase of 10 knee bend repetitions was associated with 2% greater reduction in patellar thickness or volume.
Conclusion
There is very low certainty evidence that minimal knee cartilage thickness and volume and composition (T2 relaxation time) reductions (0–5%) occur after weightbearing knee bends, simulated standing, walking, hopping/jumping and cycling, and the impact of knee bends may be dose dependent. Our findings provide a framework of cartilage responses to loading in healthy adults which may have utility for clinicians when designing and prescribing rehabilitation programs and providing exercise advice.
Similar content being viewed by others
Key Points
-
Weightbearing activities seem to cause minimal change in knee cartilage of healthy adults.
-
Immediate knee cartilage changes after weightbearing activities tend to recover within 15–90 min in healthy adults.
-
Patellar cartilage seems to be particularly affected by loaded knee bends, with the magnitude of cartilage change related to the number of repetitions performed.
Background
Abnormal joint loading is considered a key mechanical driver of osteochondral changes thought to contribute to the initiation and progression of knee and hip osteoarthritis (OA) [1]. It is not clear what intensity or type of loading may increase OA risk as under-/overloading can result in diminution of cartilage thickness and volume and compositional biomarkers [2,3,4,5], but moderate physical activity programs [4, 6] and rehabilitation exercises for OA [7], and knee surgery [8] can have positive effects on cartilage composition. Determining the effect(s) of a known dose of load on knee and/or hip cartilage is difficult to establish over an extended period due to the influence of potential confounding factors (e.g. occupational workloads, injury, body mass index [BMI], levels of compliance/drop out with exercise interventions) [9]. Alternatively, exploring the immediate and delayed effects (within 48 h) of loading on knee and hip cartilage allows for tight control of activity parameters and evaluation of the impact of potential confounders.
We recently synthesised data evaluating the immediate effects of running on cartilage assessed using magnetic resonance imaging (MRI) and found small (likely transient) reductions in knee cartilage thickness and volume (declines of 3–5%) and composition (declines of 4–13%) in healthy adults [10], similar to prior systematic reviews [11,12,13,14]. The immediate and delayed effects of joint loading activities, such as those commonly recommended to meet physical activity guidelines or achieve rehabilitation goals (e.g. walking, cycling, squatting), have not been synthesised using meta-analysis. Quantifying MRI cartilage changes in response to activity in people with healthy knees and those with, or at risk of, OA could inform our understanding of optimal loading for individuals to meet physical activity guidelines and following injury, to reduce OA risk and to design therapeutic exercise programs that facilitate cartilage health.
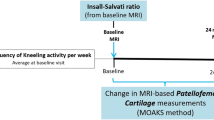
The primary aim of this study was to investigate the immediate effect of joint loading activities other than running on hip and/or knee articular cartilage, as evaluated with MRI, in healthy adults. The secondary aims were to investigate: the delayed (20 min–48 h) effects of joint loading activities, the effects of activities on cartilage in adults with, or at risk of, OA and the explore associations between cartilage changes and sex, age, and loading duration/repetitions.
Methods
Protocol and Registration
The systematic review protocol was prospectively registered (PROSPERO, CRD 42020209368) as part of a larger protocol investigating the immediate effect of various joint loading activities on knee and/or hip cartilage [10]. The study adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [15].
Search Strategy
A systematic search of Medline, Embase, and Cochrane Central Register of Controlled Trials (via Ovid), CINAHL and SPORTDiscus (via EBSCOhost), and Web of Science (via Clarivate) databases, with no restriction of publication year or language, was conducted in July 2020. The original and updated searches (in June 2021 and April 2023) used a search strategy customised for each database that included Medical Subject Heading (MeSH) terms and text words in title, abstract and as keywords related to four key themes: knee/hip and associated injuries, exercise, MRI and cartilage (Additional file 1).
Two authors (SC and TW) identified eligible studies by independently screening the title, abstract and relevant full text. Eligible study reference lists were searched recursively until no additional eligible publications were identified. Disagreement regarding eligibility was resolved by discussion. A third reviewer (AC) was available if consensus could not be reached.
Eligibility Criteria
Peer-reviewed studies were eligible for inclusion if they used any MRI measures of cartilage thickness, volume or composition to investigate changes in knee or hip articular cartilage in individuals with mean age ≥ 18 years (as immature cartilage may respond differently to mechanical load [16, 17]), with at least one scan performed within 48 h prior to and following a joint loading intervention/activity. Due to the large number of studies retrieved, the effects of running were synthesised separately and reported elsewhere [10].
To achieve our primary aim, studies for the current review investigated the effect of any joint loading activity other than running in adults with healthy joints. We also included studies that investigated individuals with, or at risk of developing OA (i.e. high BMI, post-anterior cruciate ligament [ACL] injury or surgery, with femoroacetabular impingement) to achieve our secondary aims. Joint loading activities were defined as any hip or knee joint loading exercise or physical activity that was intentional, land-based and comprised of planned, structured movement or activity (e.g. walking, hopping, weightbearing knee bends and included simulated standing within the scanner) of any type, duration or intensity.
Cartilage changes measured in the same individuals following a second joint loading activity were included if pre-/post-activity MRI was performed at each instance and the activities were separated by > 1 week (to limit potential confounding of cartilage changes that may be detected within 48 h following a strenuous activity [18]), reflecting methodology used in likely eligible studies identified during review development [19]. We excluded non-English language, non-original data studies, case reports, studies of animals or cadavers and studies of other rheumatological diseases. We excluded studies without available full-text or with incomplete data if authors were unable to provide data when contacted.
Risk of Bias
Risk of bias was assessed independently by two authors (SC, AB), using a modified version of the Newcastle–Ottawa Scale (NOS) [20, 21] (Additional file 2). Relevant items were adapted from the NOS cohort and case–control study scales to assess selection bias (i.e. inclusion criteria, representativeness, sample size), participant comparability (i.e. control of activity prior to baseline MRI, cohort comparability) and observation bias (i.e. MRI assessor blinding, MRI assessor qualifications and reliability, MRI outcome reliability/validity and follow-up adequacy). Risk of bias was rated low, high or not applicable for each of the nine items and considered to be low risk of bias overall if more than half of applicable items (i.e. ≥ 5/8 or ≥ 5/9) were rated low risk. Completed appraisals were discussed in a consensus meeting, and disagreements were decided by an independent arbitrator (JK). Cohen’s Kappa (K) was calculated to assess agreement between raters.
Data Extraction
Data were extracted by one reviewer (SC), recorded in a customised spreadsheet and cross-checked by two reviewers (AC and BM). Participant characteristics (e.g. sex, age, BMI, joint status [e.g. healthy or at risk of/having OA]) together with number of participants/joints and joint loading activity characteristics were extracted. MRI data extracted included MRI sequences utilised and percent change in MRI thickness or volume and/or compositional outcomes. Semiquantitative outcomes included scores of defect size and severity such as the Scoring Hip Osteoarthritis with MRI (SHOMRI) cartilage sub-score for the hip [22] or the Whole-Organ MRI Score (WORMS) cartilage sub-score for the knee [23]. Compositional outcomes included specialised MRI techniques used to provide measures of cartilage composition (considered to be biomarkers of early OA [24, 25]), e.g. T1ρ, T2 and T2* relaxation times, and T1-delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) index. Relaxation time measures are increased when loss of matrix integrity results in decreased concentration of collagen or proteoglycan components and increased or altered distribution of cartilage hydration [26, 27]. Hence, higher relaxation times reflect poorer cartilage health. Longer T1 dGEMRIC relaxation time, measured after injection of a contrast agent, is indicative of higher glycosaminoglycan content and therefore better cartilage quality [28].
Data that documented change in cartilage outcomes from scans conducted closest to the joint loading activity were extracted to achieve our primary aim and explore the immediate effects of joint loading activities. Data from studies that repeated measures > 20 min but within 48 h of activity completion, in the same individuals, were extracted to achieve one of our secondary aims to investigate the delayed effects of activities. For studies that measured the effects of an activity at different intensities (e.g. walking 10 min and walking 60 min on separate occasions), we selected data from the activity that was most similar in intensity to other studies in the analysis. Authors were contacted for data if results were presented graphically or bilaterally. If authors were unable to provide the requested data, a website tool (WebPlotDigitizer, version 4.5, Pacifica, USA) was used to obtain data from graphed results and bilateral data were reported narratively.
Data Synthesis and Analysis
The primary outcome was the percent change in mean MRI cartilage measures from scans performed before and immediately (i.e. within 20 min) after a joint loading activity, because significant effects of loading can occur a short time after activity completion [12]. Delayed measures of cartilage changes (21 min to 48 h after activity) were pooled if data from scans with comparable timing were available, with 48 h chosen as it is the time period where cartilage may be sensitive to a loading event [18, 29]. The equation \(\frac{{\left( {\text{post-load mean}} \right) - \left( {\text{pre-load mean}} \right)}}{{\text{pre-load mean}}} \times 100\) calculated the percent change from pre- and post-joint loading activity means when data were not presented as percent change from baseline. A Taylor expansion equation [30] and a correlation coefficient (correlation = 0.9, derived from an included study with raw and percentage change data) [31], were used to estimate the standard deviation (SD) of the percentage change, as recommended in the Cochrane Handbook [32].
Study results were pooled using random effects meta-analyses and restricted maximum likelihood (REML) models [33] displayed as forest plots (Stata SE 17 metan command), based on the most commonly reported cartilage regions in the knee (i.e. weightbearing femoral, tibial, patellar, femoral trochlear) and hip (i.e. weightbearing femoral, weightbearing acetabular). Data from studies that reported mean percent change in smaller sub-regions (e.g. superficial, deep) were combined according to methods for combining means and SD in the Cochrane Handbook [32]. We synthesised measures of cartilage thickness and volume together with a preference for volume if both measures were reported in the same study as volume has superior reproducibility for the detection of cartilage changes over time [34]. If the same study reported more than one compositional outcome, we selected the single outcome to synthesise using the following hierarchy (according to frequencies found in our previous study [10] and expert opinion [35]): T2, T1ρ, T2* and T1-dGEMRIC. Heterogeneity was calculated for each meta-analysis using the I2 statistic (where 100% is maximal inconsistency) to quantify the impact of inconsistency between studies [36].
Narrative synthesis was used to report results from studies that could not be pooled, such as bilateral and semi-quantitative measures of cartilage change and studies reporting incomparable cartilage regions, loading activities or timing of MRI measures. Meta-regression analysis explored associations between study level characteristics (i.e., sex, age, activity duration/repetitions) and changes in MRI cartilage thickness and volume.
Certainty of the Evidence
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) system appraised the overall certainty in the pooled body of evidence using five criteria: risk of bias, consistency of the reported results, indirectness of evidence, imprecision and publication bias [37]. Funnel plot symmetry and Egger tests for small-study effects were used to analyse publication bias in meta-analyses that contained ≥ 10 studies [38].
Results
Study Characteristics
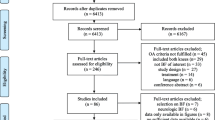
Thirty-eight studies of the knee (n = 647 participants, 40% female) and two studies of the hip (n = 33 participants, 72% female) were included (Fig. 1, Table 1). Participants with healthy knees (n = 511) were predominantly young adults (mean age 31 ± 15 years) with a healthy BMI (mean 23 ± 5 kg m−2). Participants with, or at risk of, knee OA (n = 168) were typically older (mean age 47 ± 12 years) and overweight (mean BMI 27 ± 23 kg m−2). Participants with healthy hips (n = 18) were young adults (mean age 30 years, range 27–33) with a healthy BMI (mean 22 kg m−2, range 21–22), while participants at risk of hip OA (n = 9) were older (mean age 39 years, range 24–50) with a healthy BMI (mean 22 kg m−2, range 19–30).
Knee cartilage thickness and/or volume changes were measured in 28 studies (25 and 6, respectively) [19, 39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64] and compositional changes in 16 studies (T2 = 12, T1ρ = 7, T2* = 1 and dGEMRIC = 1) [31, 46, 47, 50, 55, 58, 62, 65,66,67,68,69,70,71,72,73]. One study used a semi-quantitative measure of knee cartilage defects [74]. Hip cartilage was investigated using MRI thickness and T2 [75] and T2* relaxation time [76] measures. Online software was used to obtain percentage change or pre- and post-activity measures from graphed results, when authors were unable to supply the requested data [39, 41,42,43,44,45,46, 53, 54, 56, 57, 59,60,61, 64, 66,67,68, 76].
Joint loading activity included sustained compression loading (50% body weight) applied to the foot of individuals lying within the scanner to simulate upright standing (mean duration 24 ± 13 min) [40, 50, 53, 55, 64, 68,69,70,71,72,73, 75] and a knee flexed protocol was used to simulate squatting [52, 67]. Included studies also investigated walking [39, 41,42,43, 48, 51, 57, 62, 65, 66] (mean duration 21 ± 9.7 min) and cycling [31, 43, 47] (mean duration 22 ± 9 min). Hopping [56, 60], double-leg [54] and single-leg drop-jumps [43] were considered similar (hop/jump) activities and combined in meta-analyses. One study investigated the effects of skiing for 1 h [58]. Nine studies investigated the impact of bilateral, body weight loaded knee flexion (90–120°) activities (described as knee-bends), repeated (mean ± SD) 38 ± 10 times for 1–2 min [19, 43,44,45,46, 49, 59, 63, 76]. Two studies measured the effects of an activity at different intensities (on separate occasions) [45, 57]. To optimise analysis homogeneity, we selected cartilage change data obtained after 30 min walking from a study investigating separate walking bouts of different durations (10, 20, 30, 40, 60 min) with normalised speed [57] and after 50 repeated knee bends (in preference to 100 repetitions) [45].
Risk of Bias and Certainty of Evidence
Nine of 40 studies (23%) were assessed as low risk of bias (Fig. 2, Additional file 3). Most studies (85%) controlled participant activity prior to pre-exercise MRI [19, 39,40,41,42,43,44,45,46,47,48, 51,52,53, 56,57,58,59,60,61,62,63,64,65,66, 68,69,70,71,72,73,74,75,76] and 86% reported reproducibility and/or reliability of their MRI techniques. However, few studies (17%) were assessed as low risk of all (three) participant selection bias items [40, 46, 63, 71, 72, 74], blinded MRI readers (19%) [19, 40, 48, 54, 65, 68, 71] or reported MRI reader qualifications and reliability (15%) [19, 39, 50, 52, 62, 63, 75, 76]. High risk of bias, together with other components of the GRADE criteria, indicated very low certainty of evidence for all findings (Additional file 4).
Immediate Knee Cartilage Thickness and Volume Changes in Healthy Adults
Knee cartilage thickness and volume decreased immediately after most joint loading activities (Fig. 3), but weightbearing femoral cartilage changes were not significant after hopping/jumping and reductions were minimal after walking (2.0%, 95% CI 0.2–3.8%, I2 = 37.5%) (Fig. 4a). Reductions in tibial cartilage thickness and volume were smallest after walking (3.2%, 95% CI 2.3–4.0%, I2 = 73.0%) and greatest after simulated standing (6.3%, 95% CI 1.5–11.0%, I2 = 97.6%) (Fig. 4b). The largest immediate reductions in patellar cartilage thickness and volume occurred following knee bends (5.0%, 95% CI 3.5–6.4%; I2 = 89.3%) (Fig. 5). Single studies indicated that cycling at 80 Hz for 10 min on a stationary bike produced a 4.5% reduction in patellar cartilage (95% CI 3.6–5.4%) (Fig. 5) [43], yet cycling at the same rate for 45 min resulted in no significant change in weightbearing femoral or tibial cartilage thickness and volume. The only study to semi-quantitatively measure knee cartilage lesions found that WORMS cartilage score, signal intensity or lesion shape did not change in healthy participants after simulated standing [74].
Summary of MRI cartilage a thickness and volume and b composition percent change after activity. Summary includes analyses with two or more datasets, *Percent change significant p < 0.05, 1Run pooled meta-analysis sourced from previously published systematic review [10]. MRI icon from Eucalyp, www.flaticon.com
Percent change in tibiofemoral cartilage thickness and volume after different activities. 1Run pooled meta-analysis sourced from previously published systematic review [10], CI Confidence interval, Fr Froude number (calculated from walking velocity [m/s], lower limb length [m, floor to the greater trochanter], and the gravitational constant [9.81, in m/s2] and Fr = 0.25 (1.48 ± 0.05 m/s) represents comfortable walking pace for adults, hr hour, km kilometres, m metres, min minutes, NR not reported, rep repetitions, s seconds, SL single leg
Percent change in patellar cartilage thickness and volume after different activities. 1Run pooled meta-analysis sourced from previously published systematic review [10], CI confidence interval, m metres, min minutes, N newtons, rep repetitions
Immediate Knee Cartilage Composition Changes in Healthy Adults
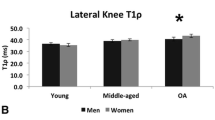
Simulated standing within the scanner resulted in highly variable and not statistically significant reductions in weightbearing femoral cartilage T2 relaxation time (5.2%, 95% CI − 0.9–11.3, I2 = 95.7%) but reduced tibial T2 relaxation times by 5.1% (95% CI 3.7–6.5%, I2 = 0%) (Figs. 3 and 6). Cycling did not appear to impact weightbearing femoral or tibial cartilage relaxation times (Fig. 6). A single study found that a 30 min walk reduced T2 relaxation time 2.7% (95% CI 1.1–4.3%) in tibial cartilage but had no effect on weightbearing femoral cartilage. Only single studies evaluated compositional changes in patellar cartilage after activity, with walking resulting in a 2.9% (95% CI 1.7–4.1%) decrease in T2 relaxation time [65] and no significant changes after simulated squat within the scanner [67] or after knee bends [46] (Fig. 6c). Incomparable cartilage regions and activities precluded pooling of data from studies that evaluated T1ρ outcomes [62, 65,66,67, 71, 72, 77], but individual studies reported reductions in tibial cartilage that ranged from 3.2% (± 2.8%) after walking [65] to 8.2% (± 10.6%) after simulated standing [72]. T1-dGEMRIC relaxation time decreased significantly in weightbearing femoral and tibial cartilage (6.6%, ± 10.5% and 6.1%, ± 9.2%, respectively) after simulated standing [68].
Percent change in cartilage composition after different activities. 1Run pooled meta-analysis sourced from previously published systematic review [10], CI confidence interval, min minutes, NR not reported, rep repetitions, s seconds
Delayed Knee Cartilage Changes in Healthy Adults and Those with OA
Four studies investigated cartilage recovery after different activities with repeated, delayed MRI (20 min–48 h) post-activity [31, 42, 45, 63]. Loss of tibial cartilage thickness and volume had recovered at 25.2 min (root mean square error = 0.24, line fit = 0.46) after a 30 min walk in healthy adults [42]. Significant tibiofemoral cartilage reductions measured immediately after 30 knee bends in healthy individuals and those with mild OA had recovered to baseline within 15 min in both groups [63]. Patellar cartilage has been reported to recover in an approximately linear pattern following 100 knee bends, with approximately 50% recovery of thickness and volume at 45 min and near complete recovery at 90 min in healthy adults [45]. T2 relaxation time recovered in superficial cartilage subregions after simulated standing [70]. However, a small increase in T2 relaxation time measured in the lateral tibial plateau following 10 min cycling in healthy adults had not recovered 20 min later and had also increased in the lateral femoral cartilage [31].
Immediate Knee Cartilage Changes in Adults with, or at Risk of, OA
Eleven studies evaluated immediate cartilage thickness and volume changes [39,40,41, 46, 48, 53, 56, 60, 62, 63, 73] and six studies evaluated composition changes [46, 62, 71, 72, 78, 79] in individuals with, or at risk of, knee OA. Comparability of cartilage regions and activities was limited; two pooled analyses identified reductions in weightbearing femoral and tibial cartilage thickness and volume following simulated standing (2.7% and 2.5%, respectively) and walking (4.4% and 4.8%), respectively (Additional files 5 and 6). A single study of individuals with patellofemoral pain found smaller patellar cartilage thickness and volume changes (4.4%, ± 3.3%) after 50 knee bends, compared to healthy participants (10.0%, ± 4.2%), but no composition differences [46]. Similarly, smaller reductions in patellar cartilage thickness (2.5%, ± 1.4) have been reported in ACL deficient knees compared to the intact contralateral knees (5.4%, ± 1.1) after 60 hops [56]. In contrast, tibiofemoral cartilage volume reductions after 30 knee bends were found to be similar in individuals with mild OA (Kellgren–Lawrence [KL] = 1–2) and healthy participants [63]. Subregion analysis of the medial femoral condylar cartilage, immediately adjacent to the intercondylar notch, decreased more in ACL deficient knees than healthy contralateral knees after hopping [60]. The only study to semi-quantitatively measure changes in knee cartilage lesions found that 16.6% of participants with radiographic OA (KL = 2–3) had increased WORMS cartilage score, signal intensity or lesion shape after simulated standing [74]. Greater reductions in tibiofemoral [39] and patellofemoral [62] cartilage thickness after (20 min) walking were found in individuals with high BMI compared to participants with normal BMI.
Immediate Hip Cartilage Changes in Healthy Adults and Those at Risk of OA
From the two studies that evaluated immediate changes in hip cartilage after activity, thickness and volume did not change after simulated standing but individuals with hip dysplasia had significant post-activity reductions in peripheral acetabular cartilage thickness (7.9%, ± 11.5%) and T2 relaxation time (7.6%, ± 10.6%) [75]. The second study investigated hip cartilage composition (using T2* relaxation time) following 50 knee bends in healthy adults and found no changes compared to pre-activity [76].
The Effects of Sex, Age, and Activity Duration/Repetitions
There were generally no other associations between knee cartilage thickness and volume changes and sex, age or joint loading activity duration (Additional file 7). However, for repeated weightbearing knee bends, for every increase of 10 repetitions, patellar cartilage thickness and volume reduced by 2% (95% CI 0.6–3.3%) (Fig. 7).
Discussion
Our systematic review is the first to investigate immediate and delayed changes to knee and hip cartilage after joint loading activities other than running. The results build on our recent systematic review (immediate effects of running) from the same overarching protocol [10]. Broadly, knee cartilage thickness, volume and composition reduced immediately following various activities, but changes were small (0–6%) with the largest immediate reductions in thickness and volume and composition after simulated standing. MRI-assessed cartilage changes after joint loading activities could be explained by the current multiphasic models of normal cartilage viscoelastic response to loading, which describe the redistribution and exudation of small amounts of water [80, 81]. The current data, and our previous findings, support MRI research protocols that utilise a period of 30 min of non-weightbearing prior to quantifying cartilage [18] and avoiding strenuous activity (i.e. repeated squatting, running) for at least 90 min to 48 h prior to the scan. Our findings were graded very low certainty due to limitations associated with high risk of bias and heterogeneity of included studies. Only two of the forty eligible studies investigated hip cartilage changes after activity, which may reflect the challenges associated with obtaining reproducible and sensitive MRI measures of hip cartilage [82].
We found the magnitude of change depended on the cartilage region and activity assessed. For example, 1–2 min of repeated knee bends (e.g. 30–50 repetitions, knee flexion 90–110°) appeared to have a greater impact on weightbearing femoral (− 4.8%) and a similar impact on patellar (− 5.0%) cartilage thickness and volume as running (− 3.6% and 5.2%, respectively) for (mean) 33 min [10]. This result is perhaps surprising given the shorter overall activity duration of repeated knee bends and high magnitude forces estimated to be five times body weight when running [83]. The cartilage effects of repeated knee bends could be due to activity parameters such as longer instances of load (1–2 s repetitions) which were up to tenfold longer than the 0.2–0.3 s load time estimated to occur during each stance phase of running [84]. Weightbearing femoral cartilage contact with the patella can occur during the maximum compressive force of a knee bend at 90° flexion [85] which has been estimated to be high (up to 18 times body weight) and associated with activities requiring greater knee flexion [43, 83]. We also identified a dose–response to loading in patellar cartilage where every increase of 10 knee bend repetitions resulted in decreases in cartilage thickness and volume by 2%. This finding aligns with larger reductions in patellar and tibial cartilage thickness and volume following increased run [86] and walk [57] durations, with controlled gait speed. Delayed (21 min–48 h) cartilage changes could not be pooled due to insufficient data, but individual studies indicated that cartilage reductions in tibial and femoral thickness and volume recovered within 15 min after knee bends [63]. Partial recovery of patellar cartilage volume occurred between repeated bouts of (50) knee bends spaced 15 min apart [45], but 90 min was required to completely recover after one bout of 100 knee bends [45]. As weightbearing knee bends, or “squats”, are a common component of rehabilitation and fitness programs, our findings could guide program design by incorporating bouts of fewer, faster knee bend repetitions to minimise patellofemoral cartilage effects.
Static unilateral application of 50% body weight loading within the scanner (to simulate upright standing) resulted in 20% greater tibial composition reduction than we found in tibial cartilage after running [10]. Reduced cartilage compositional measures (e.g. T2 relaxation times) have been associated with reduced free water [87], a more consolidated cartilage collagen matrix [88] and are related to normal viscoelastic behaviour of loaded cartilage. The cartilage effects of simulated standing could also illustrate the time-dependent behaviour of healthy cartilage, as sustained body weight loading appears to have a similar impact on composition as cyclic instances of brief but higher magnitude loads of running. It is also possible that scans taken during simulated standing better reflect the immediate effects of loading, as some recovery of cartilage composition may have already occurred in the running studies, in which scans were commenced (minutes) after activity completion [10]. Static unilateral application of 50% body weight loading within the scanner may not actually simulate standing in vivo as the contribution of weight-shifts and minor load perturbations that likely maintain cartilage thickness and volume during upright standing [89] have been eliminated by more passive supine positioning combined with foot and trunk fixation to minimise movement within the scanner. We found smaller composition reductions in OA populations, which may reflect heterogeneity in the severity of OA disease, as early stages of disease are more responsive to therapeutic exercise load [8].
Walking is an important mode of physical activity for older adults, with the accumulation of at least 10,000 steps per day thought to lower risk of mortality [90]. We found reductions in weightbearing femoral and tibial cartilage thickness and volume after walking for a (mean) duration of 21 min were smaller (1–3%) than with all other activities. Patellar cartilage thickness and volume reductions after walking (3%) (measured in only one study) were approximately half the magnitude measured after running [10], which aligns with smaller patellofemoral joint reaction forces measured during walking [83]. Greater tibiofemoral cartilage thickness and volume changes may occur at higher walking speeds [57]; however, there were insufficient data to pool the cartilage effects of different walking load intensities. Our analyses found that individuals with, or at risk of, OA, appear to have a larger reduction in tibial and weightbearing femoral cartilage thickness and volume compared to healthy individuals. Due to limited data, we were unable to compare responses of individuals with OA and those at risk of OA who may be at different stages on the degeneration continuum. Current evidence, limited to only one study, indicates a gradual, nonlinear recovery of healthy tibial cartilage thickness and volume after walking 30 min, with complete recovery occurring after 25 min [42]. The transient nature of these immediate cartilage thickness and volume changes is consistent with those observed after running where tibiofemoral cartilage returns to baseline levels within 60–90 min post-run [10], suggesting that (at least a single bout of) walking (and running) is not detrimental to knee joint health.
From limited data, narrative synthesis indicates that hip cartilage thickness and volume reductions are smaller than those observed in the knee for the same activities (i.e. simulated standing, knee bends). However, for individuals at risk of hip OA (i.e. those with hip dysplasia), simulated standing appears to result in significant loss of acetabular cartilage thickness and quality. Hip cartilage may be less responsive to load compared to knee cartilage and contribute to occupational loads being less of a factor in the development of OA in the hip compared to the knee [91]. However, further research evaluating the impact on different activities on hip cartilage and OA is needed.
Limitations
Building on recent systematic reviews of the immediate effects of running on lower-limb cartilage, we included data from all other joint loading activities in the current review. However, there were limited data evaluating tasks such as hopping, jumping, step down and cycling, with generally small changes in thickness and volume and composition observed. A single study did find a large reduction in patellar cartilage morphology after cycling, similar to running and repeated knee bends, potentially due to the increases in patellofemoral joint forces with cycling intensity [92, 93]. As a relatively new tool, MRI evaluation of articular cartilage is expensive and time intensive, and so the number of participants in included studies was small (mean n = 17). The number of studies in each meta-analysis was small due to the variety of activities investigated, cartilage regions reported, and MRI measures used and limited studies measuring individuals with, or at risk of, OA. Averaging sub-region MRI outcome measures may have diluted smaller and larger changes in cartilage after activity, although small sub-region analyses are thought to be less reliable due to high heterogeneity [94]. Caution should be adopted when making comparisons across studies in this review due to the variability in MRI sequences and equipment used that may have confounded the pooling of results [95]. This supports the need to address standardisation of MRI methodology [96] to improve certainty in the body of evidence, which was very low in our GRADE evaluation. Nevertheless, a key strength of most of the included studies was the standardisation of a period of non-weightbearing prior to the first MRI scan acquisition. This is a recommendation for MRI reproducibility [18, 29], particularly for all compositional sequences, which can be confounded by pre-scan joint loading, as confirmed in our review.
Conclusion
We found very low certainty evidence for small percent changes in knee cartilage thickness and volume and composition (0–5%) following all activities investigated. This is the first review to synthesise the evidence regarding the effects of everyday joint loading activities and rehabilitation-type exercises on knee and hip cartilage, using MRI measures. There are minimal data about the effect of joint loading activities on hip cartilage. From limited data available, it appears that most of these immediate changes were transient in healthy adults, suggesting that bouts of walking, cycling, squatting and jumping do not adversely impact cartilage health in the short term. While we know less about those with OA, our findings could be useful for clinicians when designing and prescribing rehabilitation programs and providing exercise advice. Based on current evidence, patients with knee OA should be educated that the benefits of these activities (i.e. physical, mental health and well-being) are likely to outweigh the risks for cartilage health.
Availability of Data and Materials
The datasets generated and/or analysed during the current study are available from the corresponding author on request.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- dGEMRIC:
-
Delayed Gadolinium-enhanced MRI of cartilage
- GRADE:
-
Grading of Recommendations Assessment, Development and Evaluation
- I 2 :
-
Variation across studies due to heterogeneity
- K :
-
Kappa
- KL:
-
Kellgren–Lawrence OA severity classification
- MRI:
-
Magnetic resonance imaging
- NOS:
-
Newcastle–Ottawa Scale
- OA:
-
Osteoarthritis
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- REML:
-
Restricted maximum likelihood
- SHOMRI:
-
Scoring Hip Osteoarthritis with MRI
- SD:
-
Standard deviation
- WORMS:
-
Whole-Organ MRI Score
References
Hodgkinson T, Kelly DC, Curtin CM, O’Brien FJ. Mechanosignalling in cartilage: an emerging target for the treatment of osteoarthritis. Nat Rev Rheumatol. 2022;18(2):67–84.
Hinterwimmer S, Krammer M, Krötz M, Glaser C, Baumgart R, Reiser M, et al. Cartilage atrophy in the knees of patients after seven weeks of partial load bearing. Arthritis Rheum. 2004;50(8):2516–20.
Souza RB, Baum T, Wu S, Feeley BT, Kadel N, Li X, et al. Effects of unloading on knee articular cartilage T1rho and T2 magnetic resonance imaging relaxation times: a case series. J Orthop Sports Phys Ther. 2012;42(6):511–20.
Munukka M, Waller B, Häkkinen A, Nieminen MT, Lammentausta E, Kujala U, et al. Physical activity is related with cartilage quality in women with knee osteoarthritis. Med Sci Sports Exerc. 2017;49(7):1323–30.
Lin W, Alizai H, Joseph G, Srikhum W, Nevitt M, Lynch J, et al. Physical activity in relation to knee cartilage T2 progression measured with 3 T MRI over a period of 4 years: data from the Osteoarthritis Initiative. Osteoarthr Cartil. 2013;21(10):1558–66.
Bricca A, Wirth W, Juhl CB, Kemnitz J, Hunter DJ, Kwoh CK, et al. Moderate physical activity and prevention of cartilage loss in people with knee osteoarthritis: data from the osteoarthritis initiative. Arthritis Care Res (Hoboken). 2019;71(2):218–26.
Munukka M, Waller B, Rantalainen T, Häkkinen A, Nieminen MT, Lammentausta E, et al. Efficacy of progressive aquatic resistance training for tibiofemoral cartilage in postmenopausal women with mild knee osteoarthritis: a randomised controlled trial. Osteoarthr Cartil. 2016;24(10):1708–17.
Roos EM, Dahlberg L. Positive effects of moderate exercise on glycosaminoglycan content in knee cartilage: a four-month, randomized, controlled trial in patients at risk of osteoarthritis. Arthritis Rheum. 2005;52(11):3507–14.
Alentorn-Geli E, Samuelsson K, Musahl V, Green CL, Bhandari M, Karlsson J. The association of recreational and competitive running with hip and knee osteoarthritis: a systematic review and meta-analysis. J Orthop Sports Phys Ther. 2017;47(6):373–90.
Coburn SL, Crossley KM, Kemp JL, Warden SJ, West TJ, Bruder AM, et al. Is running good or bad for your knees? A systematic review and meta-analysis of cartilage morphology and composition changes in the tibiofemoral and patellofemoral joints. Osteoarthr Cartil. 2023;31(2):144–57.
Dong X, Li C, Liu J, Huang P, Jiang G, Zhang M, et al. The effect of running on knee joint cartilage: a systematic review and meta-analysis. Phys Ther Sport. 2021;47:147–55.
Hoessly ML, Wildi LM. Magnetic resonance imaging findings in the knee before and after long-distance running—documentation of irreversible structural damage? A systematic review. Am J Sports Med. 2017;45(5):1206–17.
Khan M, O’Donovan J, Charlton JM, Roy J-S, Hunt MA, Esculier J-F. The influence of running on lower limb cartilage: a systematic review and meta-analysis. Sports Med. 2022;52(1):55–74.
Shu D, Chen F, Guo W, Ding J, Dai S. Acute changes in knee cartilage and meniscus following long-distance running in habituate runners: a systematic review on studies using quantitative magnetic resonance imaging. Skelet Radiol. 2021.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372.
Boeth H, MacMahon A, Poole AR, Buttgereit F, Önnerfjord P, Lorenzo P, et al. Differences in biomarkers of cartilage matrix turnover and their changes over 2 years in adolescent and adult volleyball athletes. J Exp Orthop. 2017;4(1):7.
Walsh SK, Schneider SE, Amundson LA, Neu CP, Henak CR. Maturity-dependent cartilage cell plasticity and sensitivity to external perturbation. J Mech Behav Biomed Mater. 2020;106: 103732.
Chalian M, Li X, Guermazi A, Obuchowski NA, Carrino JA, Oei EH, et al. The QIBA profile for MRI-based compositional imaging of knee cartilage. Radiology. 2021;301(2):423–32.
Horng A, Raya J, Stockinger M, Notohamiprodjo M, Pietschmann M, Hoehne-Hueckstaedt U, et al. Topographic deformation patterns of knee cartilage after exercises with high knee flexion: an in vivo 3D MRI study using voxel-based analysis at 3T. Eur Radiol. 2015;25(6):1731–41.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle–Ottawa scale (NOS) for assessing the quality of non randomised studies in meta-analyses. Ottawa ON Ottawa Hosp Res Inst. 2011;2(1):1–2.
Bruder AM, Culvenor AG, King MG, Haberfield M, Roughead EA, Mastwyk J, et al. Let’s talk about sex (and gender) after ACL injury: a systematic review and meta-analysis of self-reported activity and knee-related outcomes. Br J Sports Med. 2023;57(10):602–10.
Lee S, Nardo L, Kumar D, Wyatt CR, Souza RB, Lynch J, et al. Scoring hip osteoarthritis with MRI (SHOMRI): a whole joint osteoarthritis evaluation system. J Magn Reson Imaging. 2015;41(6):1549–57.
Peterfy C, Guermazi A, Zaim S, Tirman P, Miaux Y, White D, et al. Whole-organ magnetic resonance imaging score (WORMS) of the knee in osteoarthritis. Osteoarthr Cartil. 2004;12(3):177–90.
Liebl H, Joseph G, Nevitt MC, Singh N, Heilmeier U, Subburaj K, et al. Early T2 changes predict onset of radiographic knee osteoarthritis: data from the osteoarthritis initiative. Ann Rheum Dis. 2015;74(7):1353–9.
Martín Noguerol T, Raya JG, Wessell DE, Vilanova JC, Rossi I, Luna A. Functional MRI for evaluation of hyaline cartilage extracelullar matrix, a physiopathological-based approach. Br J Radiol. 2019;92(1103):20190443.
Koff M, Amrami K, Kaufman KR. Clinical evaluation of T2 values of patellar cartilage in patients with osteoarthritis. Osteoarthr Cartil. 2007;15(2):198–204.
Choi J-A, Gold GE. MR imaging of articular cartilage physiology. Magn Reson Imaging Clin N Am. 2011;19(2):249–82.
Burstein D, Velyvis J, Scott KT, Stock KW, Kim YJ, Jaramillo D, et al. Protocol issues for delayed Gd (DTPA) 2–-enhanced MRI (dGEMRIC) for clinical evaluation of articular cartilage. Magn Reson Med. 2001;45(1):36–41.
Alliance QIB. QIBA Profile: MR-based cartilage compositional biomarkers (T1ρ,T2) for risk prediction, early diagnosis and monitoring of treatment of degenerative joint disease.: RSNA; 2019 [updated 2020. Available from: https://qibawiki.rsna.org/images/1/1c/QIBA_Profile_MSK-Cartilage-Stage2_Profile.pdf.
Kendall MG. Kendall's advanced theory of statistics: distribution theory. In: Stuart A, Ord JK, editors. 6th ed. New York: Oxford University Press; 1998.
Verschueren J, van Tiel J, Reijman M, Bron E, Klein S, Verhaar J, et al. Influence of delayed gadolinium enhanced MRI of cartilage (dGEMRIC) protocol on T2-mapping: Is it possible to comprehensively assess knee cartilage composition in one post-contrast MR examination at 3 Tesla? Osteoarthr Cartil. 2017;25(9):1484–7.
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions: John Wiley & Sons; 2021 [version 6.2:[Available from: www.training.cochrane.org/handbook.
Hedges LV, Vevea JL. Fixed-and random-effects models in meta-analysis. Psychol Methods. 1998;3(4):486.
Wang Y, Wluka AE, Jones G, Ding C, Cicuttini FM. Use magnetic resonance imaging to assess articular cartilage. Ther Adv Musculoskelet Dis. 2012;4(2):77–97.
Roemer F, Kijowski R, Guermazi A. from theory to practice–the challenges of compositional MRI in osteoarthritis research. Osteoarthr Cartil. 2017;25(12):1923–5.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–6.
Bruder AM, Shields N, Dodd KJ, Taylor NF. Prescribed exercise programs may not be effective in reducing impairments and improving activity during upper limb fracture rehabilitation: a systematic review. J Physiother. 2017;63(4):205–20.
Collins AT, Kulvaranon ML, Cutcliffe HC, Utturkar GM, Smith WA, Spritzer CE, et al. Obesity alters the in vivo mechanical response and biochemical properties of cartilage as measured by MRI. Arthritis Res Ther. 2018;20(1):1–9.
Cotofana S, Ring-Dimitriou S, Hudelmaier M, Himmer M, Wirth W, Sänger AM, et al. Effects of exercise intervention on knee morphology in middle-aged women: a longitudinal analysis using magnetic resonance imaging. Cells Tissues Organs. 2010;192(1):64–72.
Crook BS, Collins AT, Lad NK, Spritzer CE, Wittstein JR, DeFrate LE. Effect of walking on in vivo tibiofemoral cartilage strain in ACL-deficient versus intact knees. J Biomech. 2021;116: 110210.
Cutcliffe HC, DeFrate LE. Comparison of cartilage mechanical properties measured during creep and recovery. Sci Rep. 2020;10(1):1–8.
Eckstein F, Lemberger B, Gratzke C, Hudelmaier M, Glaser C, Englmeier K, et al. In vivo cartilage deformation after different types of activity and its dependence on physical training status. Ann Rheum Dis. 2005;64(2):291–5.
Eckstein F, Lemberger B, Stammberger T, Englmeier K, Reiser M. Patellar cartilage deformation in vivo after static versus dynamic loading. J Biomech. 2000;33(7):819–25.
Eckstein F, Tieschky M, Faber S, Englmeier K-H, Reiser M. Functional analysis of articular cartilage deformation, recovery, and fluid flow following dynamic exercise in vivo. Anat Embryol (Berl). 1999;200(4):419–24.
Farrokhi S, Colletti PM, Powers CM. Differences in patellar cartilage thickness, transverse relaxation time, and deformational behavior: a comparison of young women with and without patellofemoral pain. Am J Sports Med. 2011;39(2):384–91.
Gatti AA, Noseworthy MD, Stratford PW, Brenneman EC, Totterman S, Tamez-Peña J, et al. Acute changes in knee cartilage transverse relaxation time after running and bicycling. J Biomech. 2017;53:171–7.
Ho K-Y, McClaren J, Sudweeks S. Acute effects of walking on the deformation of femoral articular cartilage in older adults. J Geriatr Phys Ther. 2019;42(3):E35–41.
Hudelmaier M, Glaser C, Hohe J, Englmeier KH, Reiser M, Putz R, et al. Age-related changes in the morphology and deformational behavior of knee joint cartilage. Arthritis Rheum. 2001;44(11):2556–61.
Jogi SP, Thaha R, Rajan S, Mahajan V, Venugopal VK, Mehndiratta A, et al. Device for assessing knee joint dynamics during magnetic resonance imaging. J Magn Reson Imaging. 2022;55(3):895–907.
Lad NK, Liu B, Ganapathy PK, Utturkar GM, Sutter EG, Moorman CT III, et al. Effect of normal gait on in vivo tibiofemoral cartilage strains. J Biomech. 2016;49(13):2870–6.
Lange T, Taghizadeh E, Knowles BR, Südkamp NP, Zaitsev M, Meine H, et al. Quantification of patellofemoral cartilage deformation and contact area changes in response to static loading via high-resolution MRI with prospective motion correction. J Magn Reson Imaging. 2019;50(5):1561–70.
Marsh M, Souza R, Wyman B, Le Graverand M-PH, Subburaj K, Link T, et al. Differences between X-ray and MRI-determined knee cartilage thickness in weightbearing and non-weightbearing conditions. Osteoarthr Cartil. 2013;21(12):1876–85.
Niehoff A, Müller M, Brüggemann L, Savage T, Zaucke F, Eckstein F, et al. Deformational behaviour of knee cartilage and changes in serum cartilage oligomeric matrix protein (COMP) after running and drop landing. Osteoarthr Cartil. 2011;19(8):1003–10.
Nishii T, Kuroda K, Matsuoka Y, Sahara T, Yoshikawa H. Change in knee cartilage T2 in response to mechanical loading. J Magn Reson Imaging. 2008;28(1):175–80.
Owusu-Akyaw KA, Heckelman LN, Cutcliffe HC, Sutter EG, Englander ZA, Spritzer CE, et al. A comparison of patellofemoral cartilage morphology and deformation in anterior cruciate ligament deficient versus uninjured knees. J Biomech. 2018;67:78–83.
Paranjape CS, Cutcliffe HC, Grambow SC, Utturkar GM, Collins AT, Garrett WE, et al. A new stress test for knee joint cartilage. Sci Rep. 2019;9(1):1–8.
Schütz U, Martensen T, Kleiner S, Dreyhaupt J, Wegener M, Wilke H-J, et al. T2*-mapping of knee cartilage in response to mechanical loading in alpine skiing: a feasibility study. Diagnostics. 2022;12(6):1391.
Sitoci K, Hudelmaier M, Eckstein F. Nocturnal changes in knee cartilage thickness in young healthy adults. Cells Tissues Organs. 2012;196(2):189–94.
Sutter EG, Liu B, Utturkar GM, Widmyer MR, Spritzer CE, Cutcliffe HC, et al. Effects of anterior cruciate ligament deficiency on tibiofemoral cartilage thickness and strains in response to hopping. Am J Sports Med. 2019;47(1):96–103.
Sutter EG, Widmyer MR, Utturkar GM, Spritzer CE, Garrett WE Jr, DeFrate LE. In vivo measurement of localized tibiofemoral cartilage strains in response to dynamic activity. Am J Sports Med. 2015;43(2):370–6.
Tamayo K, Heckelman L, Spritzer C, DeFrate L, Collins A. Obesity impacts the mechanical response and biochemical composition of patellofemoral cartilage: an in vivo, MRI-based investigation. J Biomech. 2022;134: 110991.
Van Ginckel A, Witvrouw E. Acute cartilage loading responses after an in vivo squatting exercise in people with doubtful to mild knee osteoarthritis: a case-control study. Phys Ther. 2013;93(8):1049–60.
Wang H, Koff MF, Potter HG, Warren RF, Rodeo SA, Maher SA. An MRI-compatible loading device to assess knee joint cartilage deformation: effect of preloading and inter-test repeatability. J Biomech. 2015;48(12):2934–40.
Chen M, Qiu L, Shen S, Wang F, Zhang J, Zhang C, et al. The influences of walking, running and stair activity on knee articular cartilage: quantitative MRI using T1 rho and T2 mapping. PLoS ONE. 2017;12(11): e0187008.
Hatcher CC, Collins AT, Kim SY, Michel LC, Mostertz WC III, Ziemian SN, et al. Relationship between T1rho magnetic resonance imaging, synovial fluid biomarkers, and the biochemical and biomechanical properties of cartilage. J Biomech. 2017;55:18–26.
Lange T, Knowles BR, Herbst M, Izadpanah K, Zaitsev M. Comparative T2 and T1ρ mapping of patellofemoral cartilage under in situ mechanical loading with prospective motion correction. J Magn Reson Imaging. 2017;46(2):452–60.
Mayerhoefer ME, Welsch GH, Mamisch TC, Kainberger F, Weber M, Nemec S, et al. The in vivo effects of unloading and compression on T1-Gd (dGEMRIC) relaxation times in healthy articular knee cartilage at 3.0 Tesla. Eur Radiol. 2010;20(2):443–9.
Nag D, Liney GP, Gillespie P, Sherman KP. Quantification of T2 relaxation changes in articular cartilage with in situ mechanical loading of the knee. J Magn Reson Imaging. 2004;19(3):317–22.
Schoenbauer E, Szomolanyi P, Shiomi T, Juras V, Zbýň Š, Zak L, et al. Cartilage evaluation with biochemical MR imaging using in vivo knee compression at 3 T-comparison of patients after cartilage repair with healthy volunteers. J Biomech. 2015;48(12):3349–55.
Souza R, Stehling C, Wyman B, Le Graverand M-PH, Li X, Link T, et al. The effects of acute loading on T1rho and T2 relaxation times of tibiofemoral articular cartilage. Osteoarthr Cartil. 2010;18(12):1557–63.
Souza RB, Kumar D, Calixto N, Singh J, Schooler J, Subburaj K, et al. Response of knee cartilage T1rho and T2 relaxation times to in vivo mechanical loading in individuals with and without knee osteoarthritis. Osteoarthr Cartil. 2014;22(10):1367–76.
Subburaj K, Souza R, Stehling C, Wyman B, Le Graverand-Gastineau MP, Link T, et al. Association of MR relaxation and cartilage deformation in knee osteoarthritis. J Orthop Res. 2012;30(6):919–26.
Stehling C, Souza RB, Le Graverand M-PH, Wyman BT, Li X, Majumdar S, et al. Loading of the knee during 3.0 T MRI is associated with significantly increased medial meniscus extrusion in mild and moderate osteoarthritis. Eur J Radiol. 2012;81(8):1839–45.
Nishii T, Shiomi T, Tanaka H, Yamazaki Y, Murase K, Sugano N. Loaded cartilage T2 mapping in patients with hip dysplasia. Radiology. 2010;256(3):955–65.
Hesper T, Hosalkar HS, Schleich C, Antoch G, Welsch GH, Krauspe R, et al. T2* mapping for hip joint cartilage assessment: pre-MRI exercise and time of imaging do not bias the T2* measurement in asymptomatic volunteers. Cartilage. 2017;8(4):400–5.
Kessler DA, MacKay JW, McDonald S, McDonnell S, Grainger AJ, Roberts AR, et al. Effectively measuring exercise-related variations in T1ρ and T2 relaxation times of healthy articular cartilage. J Magn Reson Imaging. 2020;52(6):1753–64.
Esculier J-F, Jarrett M, Krowchuk NM, Rauscher A, Wiggermann V, Taunton JE, et al. Cartilage recovery in runners with and without knee osteoarthritis: a pilot study. Knee. 2019;26(5):1049–57.
Lindner D, Chechik Y, Beer Y, Tal S, Lysyy O, Blumenfeld-Katzir T, et al. T2 mapping values in postmeniscectomy knee articular cartilage after running: Early signs of osteoarthritis? J Knee Surg. 2022;35(7):739–49.
Lai WM, Hou J, Mow VC. A triphasic theory for the swelling and deformation behaviors of articular cartilage. J Biomech Eng. 1991;113(8):245–58.
Mow VC, Kuei S, Lai WM, Armstrong CG. Biphasic creep and stress relaxation of articular cartilage in compression: theory and experiments. J Biomech Eng. 1980;102(1):73–84.
Gold GE, Cicuttini F, Crema MD, Eckstein F, Guermazi A, Kijowski R, et al. OARSI clinical trials recommendations: hip imaging in clinical trials in osteoarthritis. Osteoarthr Cartil. 2015;23(5):716–31.
Hart HF, Patterson BE, Crossley KM, Culvenor AG, Khan MC, King MG, et al. May the force be with you: understanding how patellofemoral joint reaction force compares across different activities and physical interventions—a systematic review and meta-analysis. Br J Sports Med. 2022;56(9):521–30.
Morin JB, Samozino P, Zameziati K, Belli A. Effects of altered stride frequency and contact time on leg-spring behavior in human running. J Biomech. 2007;40(15):3341–8.
Hartmann H, Wirth K, Klusemann M. Analysis of the load on the knee joint and vertebral column with changes in squatting depth and weight load. Sports Med. 2013;43(10):993–1008.
Heckelman LN, Riofrio AD, Vinson EN, Collins AT, Gwynn OR, Utturkar GM, et al. Dose and recovery response of patellofemoral cartilage deformations to running. Orthop J Sports Med. 2020;8(12):2325967120967512.
Lüsse S, Claassen H, Gehrke T, Hassenpflug J, Schünke M, Heller M, et al. Evaluation of water content by spatially resolved transverse relaxation times of human articular cartilage. Magn Reson Imaging. 2000;18(4):423–30.
Nieminen MT, Rieppo J, Töyräs J, Hakumäki JM, Silvennoinen J, Hyttinen MM, et al. T2 relaxation reveals spatial collagen architecture in articular cartilage: a comparative quantitative MRI and polarized light microscopic study. Magn Reson Med. 2001;46(3):487–93.
Benson J, Kook C, Moore A, Voinier S, Price C, Burris D. Range-of-motion affects cartilage fluid load support: functional implications for prolonged inactivity. Osteoarthr Cartil. 2021;29(1):134–42.
del Pozo Cruz B, Ahmadi MN, Lee I-M, Stamatakis E. Prospective associations of daily step counts and intensity with cancer and cardiovascular disease incidence and mortality and all-cause mortality. JAMA Internal Med. 2022;182(11):1139-48.
Vignon E, Valat J-P, Rossignol M, Avouac B, Rozenberg S, Thoumie P, et al. Osteoarthritis of the knee and hip and activity: a systematic international review and synthesis (OASIS). Jt Bone Spine. 2006;73(4):442–55.
Bini RR, Hume PA. Effects of workload and pedalling cadence on knee forces in competitive cyclists. Sports Biomech. 2013;12(2):93–107.
Ericson MO, Nisell R. Patellofemoral joint forces during ergometric cycling. Phys Ther. 1987;67(9):1365–9.
MacKay JW, Low SBL, Smith TO, Toms AP, McCaskie AW, Gilbert FJ. Systematic review and meta-analysis of the reliability and discriminative validity of cartilage compositional MRI in knee osteoarthritis. Osteoarthr Cartil. 2018;26(9):1140–52.
Atkinson HF, Birmingham TB, Moyer RF, Yacoub D, Kanko LE, Bryant DM, et al. MRI T2 and T1ρ relaxation in patients at risk for knee osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019;20(1):1–18.
Kijowski R. Standardization of compositional MRI of knee cartilage: why and how. Radiology. 2021;301(2):433–4.
Acknowledgements
Not applicable.
Funding
Sally Coburn was supported by National Health & Medical Research Council (NHMRC) of Australia Dora Lush Biomedical Postgraduate Research Scholarship GNT1169635. Adam Culvenor is a recipient of a NHMRC of Australia Investigator Grant (Emerging Leadership Fellow, GNT2008523) and Stuart Warden is supported by NIH/NIAMS P30 AR072581. The sponsors were not involved in the study design, data analysis and interpretation, writing or submission of the manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualisation was performed by SC, KC, JK, SW and AC; methodology by SC, JK, TW, AB, BM and AC; data analyses by SC, KC, JK, SW and AC; writing—original draft preparation—by SC, KC, JK, SW and AC; writing—review and editing—by SC, KC, JK, SW, TW, AB, BM and AC. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing interests
Sally Coburn, Kay Crossley, Joanne Kemp, Stuart Warden, Tom West, Andrea Bruder, Benjamin Mentiplay and Adam Culvenor declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Search strategy.
Additional file 2:
The modified Newcastle-Ottawa Quality Assessment Scale (NOS) for risk of bias assessment.
Additional file 3:
Risk of bias assessment using the NOS.
Additional file 4:
GRADE Certainty of the evidence assessment.
Additional file 5:
Percent change in tibiofemoral cartilage thickness and volume in participants with, or at risk of, OA.
Additional file 6:
Percent change in tibiofemoral cartilage composition in participants with, or at risk of, OA.
Additional file 7:
Summary of meta-regression analyses exploring associations between sex, age, and activity duration/repetitions and cartilage thickness and volume changes.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Coburn, S.L., Crossley, K.M., Kemp, J.L. et al. Immediate and Delayed Effects of Joint Loading Activities on Knee and Hip Cartilage: A Systematic Review and Meta-analysis. Sports Med - Open 9, 56 (2023). https://doi.org/10.1186/s40798-023-00602-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40798-023-00602-7