Abstract
Background
Sleep is essential for maximal performance in the athletic population. Despite that, the sport context has many factors that can negatively influence athletes’ sleep and subsequent recovery.
Objectives
The purpose of this systematic review was to synthesize the most recent literature regarding sleep interventions aimed at improving sleep and subsequent performance in athletes.
Methods
The present systematic review was conducted based on the PRISMA guidelines and the PICOS approach. The search was conducted in May 2022 using the electronic database PubMed, SPORTDiscus via EBSCOhost, and Web of Science. Once extracted, studies were included if they met the following criteria: (1) participants were athletes of individual or team sports; (2) implemented an intervention aimed at improving sleep; (3) measured at least one objective performance/recovery outcome; and (4) reported the relationship between sleep and performance.
Results
The search returned 1584 records. Following the screening, a total of 25 studies met our inclusion criteria. All the included articles were intervention studies published between 2011 and 2021. The included studies implemented various sleep interventions, such as sleep hygiene, naps, sleep extension, light manipulation, cold water immersion, mindfulness, or a combination of two or more strategies. Sleep extension and naps were the most representative and most effective strategies to improve sleep and performance. Mindfulness and light manipulation demonstrated promising results, but more studies are needed to confirm these findings. Sleep hygiene, removing electronic devices at night, and cold water immersion had no effects on sleep and subsequent performance/recovery, but these results are based on a few studies only.
Conclusion
While acknowledging the limited amount of high-quality evidence reviewed, it appears that increasing sleep duration at night or through napping was the most effective interventions to improve physical and/or cognitive performance.
Protocol Registration This protocol was registered in the International Platform of Registered Systematic Review and Meta-Analysis Protocols (INPLASY) on May 11, 2022, with the registration number INPLASY202250069.
Similar content being viewed by others
Key Points
-
Increasing sleep duration through naps or night-time sleep may positively impact physical and/or cognitive performance.
-
Extending sleep duration by 46–113 min in athletes that habitually sleep ~ 7 h per night may be a general recommendation for future sleep extension programs.
-
Supplementing sleep during the day with a 20–90-min nap can improve performance outcomes after a regular night and restore performance decrements to baseline levels after a night with partial sleep restriction.
Introduction
Sleep is a biological need crucial for human health and well-being [1]. During periods of sleep restriction or deprivation, general health is negatively affected, particularly the immune system, endocrine, physical, or cognitive functions [2,3,4]. While the general sleep recommendations advocate that adults obtain 7–9 h of sleep per night to maintain optimal health and functioning [5], many adults do not comply with these recommendations. For athletes, often exposed to high-intensity training, it is recognized that sleep is the most important method for psychological and physiological recovery [6, 7]. Elite athletes report needing approximately 8 h of sleep per night to feel rested [8]. However, elite athletes often sleep less than 7 h [8, 9] due to several potential sport and non-sport-related factors, which may vary across sports. Several sport-specific factors are associated with sleep inadequacy, including transmeridian travel (disrupting the circadian rhythm and exposing the athletes to an unfamiliar sleeping environment), cognitive arousal on the night before a competition, evening competitions, high training loads, and early morning training [10, 11]. In addition, various non-sport factors, such as social demands, work/study commitments (e.g., sponsorships), lifestyle choices (e.g., diet), individual characteristics (e.g., age), attitudes and beliefs (e.g., societal influence), and family commitments, have been linked with inadequate sleep in athletes [10]. Despite some mixed results, a decline in physical and cognitive performance can occur after a night of sleep restriction [4, 12, 13]. For example, two studies with runners and judo athletes showed that after a night with partial sleep restriction (4 h of sleep), endurance performance, muscle strength, and power were negatively affected [14, 15]. A night with partial sleep restriction can also affect the execution of motor skills that require a high cognitive dimension, such as reported for handball goalkeepers [16], dart players [17], and tennis players [18].
Given the growing concern about athletes' sleep, studies examining sleep interventions have grown exponentially over the recent years [19]. To date, studies examining the sleep/wake behavior of athletes have focused on nutrition [13, 20], sleep hygiene [21], and sleep extension/napping [22, 23]. In a systematic literature review evaluating the effectiveness of sleep interventions for athletes specifically aimed at improving performance outcomes, Bonnar et al. [24] showed that sleep extension was the most beneficial intervention, while napping, sleep hygiene, and post-exercise recovery strategies provided mixed results. However, this review was conducted over 5 years ago. Since then, many studies have been published, and our understanding of the impact of sleep interventions on athletic performance has improved. More recently, in an expert consensus about athletes’ sleep, Walsh et al. [10] narratively reviewed the studies of the general phenomena of athlete’s sleep. Despite being very comprehensive, the study included only a few reports regarding sleep interventions that explored the effect of sleep extension, sleep hygiene and naps on athletic performance. In this regard, a more comprehensive review of the literature on the entire spectrum of sleep interventions is needed.
Therefore, this systematic review aimed to update and expand the findings of Bonnar et al. [24] and synthesize the most recent literature regarding sleep interventions aimed at improving sleep and subsequent performance in athletes.
Methods
Protocol and Registration
This protocol was registered in the International Platform of Registered Systematic Review and Meta-Analysis Protocols (INPLASY) on May 11, 2022, with the registration number INPLASY202250069.
Eligibility Criteria
This systematic review was conducted based on the PRISMA guidelines [25, 26] and the PICO approach [27]. The PICO approach was established as follows: Population: individual or team sports athletes; Intervention: strategies to improve or extend sleep; Comparators: control group or a baseline phase without sleep intervention; Outcomes: subjective and/or objective measurement of sleep and physical and/or cognitive performance. No sex or age restriction was applied. To be considered for the first screening, the studies had to be published or in-press in peer-reviewed journals (i.e., abstracts published in conference proceedings, books, theses, and dissertations were not considered), published in English, and have an abstract available for screening.
Search Strategy
The articles were searched in May 2022, and three electronic databases were used: PubMed, SPORTDiscus via EBSCOhost, and Web of Science. In each database, the following descriptors covering the characteristic of participants, intervention, and outcomes were used: (athlet* OR sport*) AND (sleep AND (education OR hygiene OR Duration OR extension OR therapy OR strateg*) OR nap*) AND (performance OR competiti* OR recovery OR fatigue OR outcome*). Searches were conducted using ‘‘title and abstract’’ (PubMed), ‘‘topic’’ (Web of Science), and “abstract” (SPORTDiscus via EBSCOhost). Discrepancies in the search fields are due to differences in the options available in the databases. Filters for “English” and “articles” were applied. A reference management software (EndNote 20, Clarivate Analytics, USA) was used to import and analyze all references.
Study Selection
Studies were included if they met the following criteria: (1) participants were athletes of individual or team sports, from trained to world-class athletes [28]; (2) implemented an intervention aimed at improving sleep; (3) measured at least one objective performance/recovery outcome; and (4) reported the relationship between sleep and performance.
Studies on referees or military tactical athletes, studies reporting only subjective performance measures, and interventions that included sleep medication were excluded.
Data Collection Process
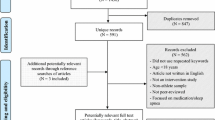
Before starting the article selection process, duplicate citations obtained from the different databases were eliminated. Then, two evaluators (LC and JC) independently examined the article title, abstract, and keywords in the first screening stage according to the established inclusion and exclusion criteria. Subsequently, full-text articles of those citations were read and selected if suitable for inclusion. In cases of disagreement, a third reviewer (PF) was consulted. The detailed data collection process is shown in a flowchart (Fig. 1).
Data Items
For the papers included in the analysis, we considered information about: (1) geographical location where the study was conducted; (2) study design; (3) sport; (4) sample (size, age, and sex); (5) type of intervention (e.g., sleep hygiene, napping, or sleep extension); (6) sleep assessment (e.g., questionnaires, actigraphy, or polysomnography; (7) performance/recovery assessment test and related physiological outcomes (e.g., psychomotor vigilance task, countermovement jump, or Wingate test; creatine kinase, heart rate variability (HRV), or lactate); and (8) main results.
Risk-of-Bias Assessment
We applied the revised Cochrane risk-of-bias tool for randomized trials (RoB2) [29, 30] to assess the potential risk of bias. RoB2 is an outcome-focused, domain-based tool that evaluates the risk of bias in outcomes in individually randomized, parallel-group trials, randomized crossover trials (RCT), and cluster RCTs [29, 30]. RoB2 has five risk-of-bias domains covering the different aspects of the trial design, conduct, and reporting. These include: (1) bias arising from the randomization process; (2) bias due to deviations from intended interventions; (3) bias due to missing outcome data; (4) bias in the measurement of the outcome; and (5) bias in the selection of the reported results. We also applied the RoB2 version for crossover trials, which considers the within-participants design not addressed by the RoB2 for randomized trials and includes an additional domain: bias arising from period and carryover effects and an additional question on domain “bias in the selection of the reported results.” In both RoB2 and RoB2 for crossover trials, responses to signaling questions are mapped using a decision algorithm to determine each risk-of-bias domain judgment [30]. Based on the domain-level assessment, the overall risk-of-bias judgment was made for each assessed outcome in each trial.
The risk-of-bias assessment tool for non-randomized studies (RoBANS) [31] was applied to analyze non-randomized studies included. The RoBANS is a domain-based evaluation tool, compatible with the Cochrane risk-of-bias tool [31], that has six risk-of-bias domains: (1) selection of participants; (2) confounding variables; (3) measurement of exposure; (4) blinding of outcome assessments; (5) incomplete outcome data; and (6) selective outcome reporting. Two researchers (LC and JC) independently applied both tools (RoB2 and RoBANS). After completion, the three tables were compared, and all disagreements were discussed and reanalyzed until consensus was achieved.
Results
Study Selection
The search strategy returned 1584 records. Of the 61 studies retained for full-text screening, we excluded 37 studies that did not meet the inclusion criteria (Fig. 1). An additional article identified through the included studies' reference lists was included. Twenty-five studies were therefore eligible for review.
Characteristics of Included Studies
The characteristics of the included studies are presented in Table 1.
All the included articles were intervention studies published between 2011 and 2021 (60% crossover trials, 8% RCT, and 32% non-RCT). The number of participants in the included studies ranged from 9 to 31 athletes, with an age range from 13 to 33 years. Studies covered 17 different sports (11 studies included team sports, 13 included individual sports, and 1 was unreported). Of the 25 studies analyzed, 17 included only male athletes, 3 had only female athletes, and 5 included both male and female athletes. Finally, the level/category of the athletes was highly heterogeneous and represented mainly by just one or two studies, except for trained athletes that were included in nine studies [32,33,34,35,36,37,38,39,40], highly trained athletes in four studies [41,42,43,44], and elite athletes in three studies [45,46,47].
Risk of Bias
The risk-of-bias analysis is summarized in Fig. 2. Figure 2A describes the analysis of crossover studies. Five studies were judged to be at a high risk of bias, and ten studies were considered with some concerns. Some possible biases were related to the carryover effects and outcome measurement (particularly the use of subjective tools), but the lack of pre-registration of intentions/methodology (which avoids the possibility of selecting the reported result) was particularly relevant for the overall results. Figure 2B describes the analysis of RCT. Two studies were judged to be at a high risk of bias due to the possible bias in all domains, except in domain 3 (missing outcome data). Figure 2C describes the analysis of non-RCT. Some potential biases were the lack of control over confounding variables and the lack of pre-registration of intentions/methodology.
Effects of Sleep Interventions on Cognitive Performance
Twelve studies investigated the effect of sleep interventions on sleep and cognitive performance, of which one study explored sleep hygiene [48], four investigated naps [35, 42, 45, 49], one investigated naps combined with caffeine consumption [47], three investigated sleep extension [37, 41, 50], two investigated the removal of electronic devices [32, 34], and one investigated an artificial light intervention [51]. Only one study [48] examined the impact of sleep hygiene for six weeks and did not find any improvement on vigilance and attention, as measured by the Psychomotor Vigilance Task.
Regarding napping, despite differences in study design, a positive effect was found for short (20–40 min) and long naps (90–120 min) on attention, simple reaction time, multiple choice reaction time, juggling performance, mental rotation test, and lower reaction test [35, 42, 45, 49]. After a night of partial sleep deprivation and a typical night, Romdhani et al. [47] examined the effect of napping and caffeine or placebo and found that two-choice reaction time was improved, regardless of caffeine ingestion or sleep deprivation. For simple reaction time, performance was only enhanced after caffeine ingestion, regardless of sleep deprivation or napping.
Regarding sleep extension interventions, the results showed that increasing sleep duration positively impacts psychomotor vigilance task and reaction time [37, 41, 50].
Following the removal of electronics, Dunican et al. [32] and Jones et al. [34] did not observe any effects on sleep or cognitive performance (the Cogstate research tool and 5-min psychomotor vigilance task). Rosa et al. [51] examined the effect of artificial bright light on the sleep/wake cycle and psychomotor vigilance task performance. They observed an improvement in mean reaction time and a delay in the sleep/wake cycle, although sleep duration was significantly reduced.
In summary, naps, sleep extension, and light therapy demonstrated positive results on cognitive performance [35, 37, 41, 42, 45, 47, 49,50,51]. In contrast, removing electronic devices and sleep hygiene revealed no effects [32, 34, 48]. Data from these studies are summarized in Table 1.
Effects of Sleep Interventions on Physical Performance
Sixteen studies investigated the effect of sleep interventions on sleep and physical performance, of which eight investigated the effect of napping [35, 36, 39, 40, 44, 45, 49, 52], one investigated naps combined with caffeine [46], three examined the impact of sleep extension [37, 41, 43], one investigated the effect of removing electronic devices [32], one investigated the effect of light intervention [38], one investigated the effect of mindfulness [33], and one investigated the effect of combining sleep hygiene and mindfulness [53].
Boukhris et al. [35], Romdhani et al. [45], and Nishida et al. [44] investigated the effects of short (20–40 min) and long naps (60–90 min) on maximal strength (knee extensors maximal voluntary isometric contraction), anaerobic capacity (running-based anaerobic sprint test and 5-min shuttle run test), and handball performance. The results showed a positive effect of naps, although Boukhris et al. [35] observed greater effects with a longer nap, and Nishida et al. [44] found positive effects following a 60-min nap in individuals with poor sleep quality. Boukhris et al. [39] and Hsouna et al. [40] examined the effect of a 40-min nap compared with no nap on the 5-min shuttle run test. They found a positive impact in total and best distance, despite no differences in fatigue index.
Despite the different contexts, Petit el al. [36] and Daaloul et al. [49] found no effects of napping when examining the impact of a short nap (20–30 min) on the Wingate test, squat jump, countermovement jump (CMJ), and karate-specific test. In a study divided into two experiments, Suppiah et al. [52] showed that napping negatively impacted sprint performance in track and field athletes. However, no effect was observed on shooting performance in shooters. Romdhani et al. [46] showed that a 20-min nap combined with caffeine improved running-based anaerobic sprint test (RAST) performance. In addition, caffeine without nap and a 20-min nap with a placebo improved maximum power.
Regarding sleep extension, increasing sleep duration improved basketball and tennis performance (timed 282 feet sprint, free throw, three-point shooting accuracy, and serving accuracy) and endurance capacity [37, 41, 43]. With respect to removing electronic devices and light intervention studies, Dunican et al. [32] did not show any effect of removing the electronic devices on the single leg three hop test, while Zhao et al. [38] found that 14 days of red-light treatment at night increased sleep quality and endurance performance (Cooper 12-minute run test). Jones et al. [33] showed that an 8-week mindfulness-based stress reduction program improved rowing performance (6000-m ergometer test). In contrast, Lever et al. [53] showed no improvement in tennis match performance (games won or lost) after combining mindfulness and sleep hygiene education.
In summary, napping interventions had conflicting results since five studies showed a positive effect [35, 39, 40, 44, 45], one showed positive results but was combined with caffeine [46], three showed no effect [36, 49, 52], and one a negative effect [52]. All sleep extension studies demonstrated improvements in physical performance [37, 41, 43], as did light [38] and mindfulness interventions [33]. Lastly, removing electronic devices [32] or combining mindfulness with sleep hygiene [53] did not affect physical performance measures. The main effects are summarized in Table 1.
Effects of Sleep Interventions on Recovery
Five studies investigated the effect of sleep interventions on sleep quality, sleep duration, and recovery, of which one study investigated the effect of an acute sleep hygiene intervention [54], two investigated the effect of naps [39, 44], one investigated the effect of cold water immersion [55], and one investigated the impact of combining three strategies [56].
Concerning naps, Boukhris et al. [39] studied the effect of a 40-min nap on levels of muscle damage and inflammatory responses and found positive effects. On the other hand, Nishida et al. [44] compared the effect of short (20 min) and long naps (60 min) compared with no naps on HRV and did not find any difference between experiments. Chauvineau et al. [55] compared the effect of whole-body and partial-body cold water immersion with the control condition (i.e., sitting 10 min in a controlled environment) on HRV, wellness (Hooper index), creatine kinase, CMJ, and maximal isometric strength 24 h and 48 h post-intervention and found no differences between conditions. In regard to sleep hygiene, Fullagar et al. [54] demonstrated that a sleep hygiene intervention following a late-night soccer match had no effect on physical recovery (Yo–Yo intermittent recovery test—level 2 and CMJ 12 h and 36 h post-match, submaximal interval-based running test 18 h and 42 h post-match) or in blood markers of muscle damage and inflammation (C-reactive protein, creatine kinase, and urea 10 h, 20 h, 34 h, and 44 h post-match). Duffield et al. [56] combined sleep hygiene, full-body compression, and cold water immersion after and between two sessions of on-court tennis on the same day. They found a reduction in muscle and joint soreness the next morning, and large effect sizes, despite no significant differences, in reducing fatigue and increasing total sleep time, but no differences in vigor or sleep efficiency.
In summary, cold water immersion [55] and sleep hygiene [54] had no impact on performance recovery, muscle damage, or inflammation. Naps positively impacted muscle damage and inflammation [39], despite no effect on HRV [44]. Combining sleep hygiene, cold water immersion, and full-body compression positively affected muscle and joint soreness [56].
Discussion
Sleep is widely recognized as one of the foundations for optimal health, well-being, and performance for athletes [10, 13, 57]. This systematic review synthesized the evidence regarding sleep interventions aimed at improving sleep, and whether this improvement would influence performance and/or recovery. Twenty-five studies with different sports and sleep interventions were analyzed. The findings reinforced that napping and sleep extension were the most promising sleep interventions for improved sleep and subsequent physical and/or cognitive performance.
All the included studies that implemented sleep extension showed a positive impact on performance outcomes (e.g., reaction time or sport-specific performance). The results showed that extending sleep duration by 46–113 min (e.g., increase of 11–27%) over 3–49 nights in athletes that habitually slept ~ 7 h per night may be a logical recommendation for future sleep extension programs [37, 41, 43, 50]. To achieve such sleep duration, studies have reported that athletes needed to extend their usual time in bed to 9–10 h [37, 41, 43, 50]. In addition, the individual characteristics of the athlete's sleep habits should be considered before implementing any sleep intervention, as it is important to adapt to individual needs [24]. Lastella et al. [9] demonstrated, in a sample of 124 participants, that elite athletes obtained well below 8 h of sleep per night (6.8 ± 1.1 h), which may not be enough to maximize performance. For example, Sargent et al. [8] revealed that elite athletes reported needing approximately 8.3 h of sleep to feel rested. Despite this self-reported sleep need, only 3% of athletes obtained their required sleep amount. It is plausible that athletes who fall short of their sleep requirements are likely to benefit from a sleep extension intervention.
Napping was the most representative sleep intervention of the included studies [35, 36, 39, 40, 42, 44, 45, 49, 52]. Napping is a strategy that provides an opportunity to supplement the night-time sleep period, offering an alternative for athletes to increase sleep duration. In most of the studies analyzed, the results revealed a positive impact of napping on cognitive performance [35, 42, 45, 49]. However, some mixed results were reported for physical performance [35, 36, 45, 49, 52] and recovery [39, 44] outcomes. During nights of partial sleep restriction (e.g., 4 h of sleep), decreases in general performance outcomes such as muscle power or psychomotor vigilance were observed [4]. The included studies showed that napping could restore performance to baseline levels [45, 49]. With regard to nap duration, the improvements in physical and cognitive performance were greater in naps of longer duration (e.g., 90 min) compared with shorter durations (e.g., 40 min) after a normal night [35]. However, following a night of partial sleep restriction, a short nap (20 min) was as effective as a long nap (90 min) in restoring performance to baseline levels (normal sleep night) [45]. There are still questions about the effects of daytime naps on night-time sleep variables (e.g., latency), especially naps of longer durations [36, 58]. Further, the notion of sleep inertia (e.g., feeling of grogginess upon wakening) needs to be considered when napping is implemented. For example, the longer the nap the higher the chance of experiencing sleep inertia [59]. A period of at least 30 min should be allowed after a nap to avoid the detrimental effects of sleep inertia on physical or cognitive performance [60], particularly for naps longer than 90 min. Based on the results of the included studies, it is unlikely that naps negatively affect performance outcomes in athletes. For all included studies, only one showed that napping decreased sprint performance in track-and-field athletes. However, the study did not reveal any effects on other sprint variables or shooting performance in pistol and rifle shooters [52].
The results of sleep hygiene interventions showed no effect on performance recovery, blood markers of damage (creatine kinase) and inflammation (C-reactive protein), or cognitive performance [48, 54]. Sleep hygiene currently refers to a list of behaviors, environmental conditions, and other sleep-related factors believed to promote improvements in sleep duration and quality [61]. Van Ryswyk et al. [48], contrasting with other studies that applied sleep hygiene with success [62, 63], concluded that a sleep hygiene protocol did not improve sleep quality and/or duration. Fullagar et al. [54] found that a sleep hygiene protocol resulted in a significant improvement in sleep duration after a late night soccer match compared to no sleep hygiene (6:09 ± 0:43 h vs 4:30 ± 0:27 h; P < 0.05), but no differences in recovery were observed between conditions. A possible explanation could be that even with an improvement in sleep duration, this improvement may not be enough, as it was still far from the 7 h of the minimum recommended sleep duration [5].
In studies that investigated the removal of electronic devices, the results showed no impact on sleep and/or athletic/cognitive performance [32, 34]. The main objective of this strategy is to reduce the exposure to the artificial light emitted by screens, especially before bedtime, reducing the decline in sleep quality and disturbance in the biorhythms [64]. Biorhythms are explained by the oscillation levels of endogenous hormones, like melatonin or cortisol, that regulate the sleep–wake cycle [65]. Despite this rationale, the results showed that the removal of electronic devices did not result in any change in sleep [32, 34]. Based on these results, it is unlikely that the removal of electronic devices should be on the “first line” of sleep interventions, because the difficulty of adherence by the athletes should also be considered. In addition, using electronic devices up to one hour before bedtime with the “night shift” mode (short-wavelength light limitation) significantly reduced melatonin suppression when compared with blue-light exposure (10 ± 2.7% vs 41 ± 4.1%) [66]. Furthermore, if devices were used with low light levels, the suppression of 10% may have been even smaller. It appears that using electronic devices in these circumstances, within reasonable limits, may not be problematic for athletes’ sleep. Moreover, it is still unclear whether ~ 10% of melatonin suppression induces circadian disruption and whether the type of activities (e.g., social media or gaming) can promote cognitive arousal.
Concerning light interventions, two studies investigated the effect of phototherapy but with different objectives. Zhao et al. [38] studied the effect of whole-body red-light phototherapy on sleep quality and endurance performance. At the same time, Rosa et al. [51] investigated the effect of bright-light therapy on sleep/wake cycle and reaction time. It is known that light is the most powerful circadian synchronizer for humans, which begins with its reception in the eyes and finishes in the pineal gland, which produces melatonin, a neurohormone essential for the functioning of the body-clock [67]. Zhao et al. [38] applied red-light therapy, which, unlike bright light, appears to have no impact on melatonin suppression [68] and may improve recovery [69, 70]. Despite increased sleep quality and melatonin levels after red-light therapy, it is important to interpret these results cautiously. The study used an inappropriate tool (the Pittsburgh Sleep Quality Index) to examine sleep quality over a short period and only analyzed melatonin levels upon waking. The authors also found a higher increase in running distance (Cooper 12-min run test) in the red-light treatment group (12.8%) compared to the control group (5.5%; P < 0.05). As the method used to examine sleep over a short period was unreliable and did not measure any exercise recovery outcome, these conclusions must be interpreted cautiously. In contrast, Rosa et al. [51] showed that bright-light therapy in the evening delayed the sleep/wake cycle and improved reaction time, promoting higher levels of alertness in a period when the athletes would usually be preparing for sleep. Further studies are needed to confirm these findings, considering that bright-light therapy can manipulate the body-clock to compete at night when alertness is usually already starting to drop.
The rationale for the possible positive effects of cold water immersion on sleep is that cold water immersion could accelerate the declining core body temperature and the reactivation of parasympathetic activity after exercise [71, 72]. Despite this, Chavineau et al. [55] did not find any impact on sleep architecture, muscle damage, core temperature, or fatigue, while Duffield et al. [56], combining cold water immersion with sleep hygiene and full-body compression, showed a positive effect on muscle/joint soreness and sleep duration (large effect sizes though non-significant results). However, Duffield et al.’s study [56] applied sleep hygiene and compression garments in addition to cold water immersion, and this could explain the differences between the results of the studies.
Finally, the studies that investigated the effect of mindfulness combined with sleep hygiene or mindfulness alone showed promising results. For example, Lever et al. [53] showed that combining sleep hygiene with mindfulness during a tennis tournament improved sleep duration, compared with a control group without any intervention (7.1 h vs 7.7 h). Despite an increase in sleep duration, no performance or sleep quality improvements were observed. Since this study only examined general performance that may be influenced by several factors (games won or lost), the impact of this type of intervention needs to be examined in detail in future studies. Jones et al. [33] tested a mindfulness intervention and showed no effect on sleep duration but did find improvements in sleep quality, mindfulness tendency (Five Facet Mindfulness Questionnaire) and rowing performance (6000-m ergometer test). It is plausible that mindfulness can improve sleep quality and/or duration; it could also positively impact physical/cognitive performance, as seen in sleep extension studies. However, it remains to be clarified whether the increase in mindfulness directly benefits athletic performance via attentional strategy, because mindfulness training appears to improve performance in precision sports such as shooting and dart throwing. Still, few controlled experimental studies have investigated the effects in non-precision sports [73].
In summary, this systematic review updated the knowledge about several sleep interventions' effects on improving sleep and subsequent performance in athletes. In 2017, Bonnar et al. [24] conducted a systematic review with a similar aim to the present review. Since then, many studies have been published and our understanding about the phenomena has improved. In the present review, we were able to include 15 more studies that brought new interventions, supporting some of the conclusions and showing different directions in other topics, compared to those of Bonnar et al. [24]. The effectiveness of sleep extension programs was reinforced with two new studies that showed, once again, the positive effects on sleep and subsequent performance. Napping was the most studied intervention since Bonnar et al.'s [24] study. The present review includes eight new studies that gave a different perspective, identifying positive effects on cognitive performance, despite mixed results on physical performance and recovery, while Bonnar et al. [24] only had two studies included with very different protocols, which did not allow for an in-depth discussion. The amount of studies examining sleep hygiene remained the same, considering that Duffield et al.’s study [56] also included compression and cold water immersion and Lever et al. [53] included mindfulness, suggesting that more research is warranted. New interventions, such as mindfulness, removing electronic devices at night or sleep/wake cycle manipulation through bright-light exposure are included in this review. Bonnar et al.’s review pointed out the lack of studies that evaluated cognitive techniques to improve sleep and subsequent performance. The negative impact of increasing arousal on the pre-competition night due to stress and anxiety, a common situation in the sports field, is known [74]. Although we are far from a definitive conclusion about the effect of cognitive interventions, such as mindfulness, researchers are beginning to be aware of the importance of studying this topic. Our review reinforces the importance of this line of research that could attenuate the detrimental effects of cognitive arousal on pre-competition night and improve sleep.
Before implementing any strategy to improve sleep in athletes, there is some information that should be considered (Fig. 3). The first step should to provide a sleep education session, conducted by a specialist. The goal will be to raise awareness among athletes and coaches about the importance of sleep for optimal performance/recovery and explain the different strategies that could be used [10, 24]. After that, the habitual sleep/wake patterns should be identified [10]. This should be done with reliable and validated tools (e.g., actigraphy) for 7 to 14 days and apply validated questionnaires in athletes (e.g., Athlete Sleep Behaviour Questionnaire) [74]. This will facilitate an individualized approach to meet individual needs and identify the athletes with clinical sleep issues (e.g., insomnia) who should be referred to a sleep physician. Some caution should be taken with sleep monitors, as some athletes may be concerned about sleep monitor data, which may increase anxiety and result in worse sleep [10, 74].
To implement a sleep extension program, it is necessary to consider whether the athlete is obtaining adequate sleep for their needs [22]. If the athlete feels the need to sleep more, the recommendations based on included articles could be applied, although with some caution, as none of the included studies showed a low risk of bias. Furthermore, it is important to consider that to increase sleep duration based on the recommendations of this review, athletes may need to extend their usual time in bed to 9–10 h [37, 41, 43, 50]. In cases of athletes who are satisfied with the amount of sleep that they usually get, the possibility of increasing wakefulness in bed should be considered before trying to extend sleep duration. Napping is an alternative strategy to supplement insufficient night-time sleep, but can also be beneficial for those who only want a boost in alertness during the day [10, 60].
Sleep hygiene is a set of behaviors that should be implemented, although its effectiveness may be limited when used alone [48, 53, 56]. Implementing mindfulness is a long-term strategy because it needs to be learned. Preliminary evidence showed the long-term effect of mindfulness (5 to 12 months) on sleep [75], although Jones et al. [33] showed positive results on sleep quality within a 9-week period (one session per week). More research is needed to allow more solid recommendations. Motivation is also an important variable when a behavioral change is necessary, as in the case of sleep hygiene and mindfulness, and should be considered. Future research should investigate the impact of this variable on the effectiveness of behavioral interventions.
Long-term sleep monitoring should be conducted (sleep logs or validated devices) to assess whether interventions resulted in better sleep [10].
Limitations
The current systematic review has limitations which should be acknowledged. First, the strengths of our conclusions are limited, since none of the included studies presented a low risk of bias. This is in line with a recent expert consensus statement about athletes' sleep studies, warning about the poor quality of the evidence, and the need to use more consistent, reliable, and valid research methods in athletes’ sleep studies [10]. To reduce the risk of bias, future studies should: design randomized controlled or crossover trials; identify the chronotype, due to possible bias in performance measures; explain in detail the randomization process; monitor a baseline sleep period (1–2 weeks) without any intervention; consider the carry over effect of the interventions, in the case of crossover trials; use objective and/or subjective validated tools for monitoring sleep; use objective performance measures; report missing data; and register the protocol before conducting the study. Second, there was high heterogeneity between the type of sleep interventions, type of sport, performance tests used, and level of the athletes. Lastly, there is a risk of language bias because we only considered studies written in English.
Conclusion
Based on the results of this systematic review, increasing sleep duration through naps or night-time sleep may positively impact physical and/or cognitive performance. If athletes habitually obtain ~ 7 h of sleep per night, a general recommendation may be to increase sleep duration up to 2 h over 3–49 nights. Also, supplementing sleep during the day with a nap (20–90 min) can be implemented when necessary. In addition to improving the sleep duration, naps can improve performance outcomes after a regular night and restore performance decrements to baseline levels after a night with partial sleep restriction. For strategies such as sleep hygiene, mindfulness, or limiting the use of electronic devices before bedtime, it is plausible that such interventions can positively impact performance outcomes if they can improve sleep quality and/or duration. Strategies with light exposure may be an option to manipulate the biological clock and increase the alertness of the athletes in the moments when this starts to fall (e.g., at night). However, more studies are needed to confirm these findings. Future research on this topic should use more reliable and valid research methods to increase the quality of evidence so that more solid conclusions can be drawn. In addition, studies that explore the effect of 1–3 h of sleep restriction on physical and cognitive performance may be interesting, as this is the most common situation detected in the athletes’ context.
Availability of Data and Materials
Not applicable.
Code Availability
Not applicable.
References
Troynikov O, Watson CG, Nawaz N. Sleep environments and sleep physiology: a review. J Therm Biol. 2018;78:192–203.
Van Dongen HPA, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–26.
Haack M, Sanchez E, Mullington JM. Elevated inflammatory markers in response to prolonged sleep restriction are associated with increased pain experience in healthy volunteers. Sleep. 2007;30:1145–52.
Fullagar HHK, Skorski S, Duffield R, Hammes D, Coutts AJ, Meyer T. Sleep and athletic performance: the effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sport Med. 2015;45:161–86.
Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National sleep foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health Natl Sleep Found. 2015;1:40–3.
Venter RE. Perceptions of team athletes on the importance of recovery modalities. Eur J Sport Sci. 2014;14:37–41.
Querido SM, Brito J, Figueiredo P, Carnide F, Vaz JR, Freitas SR. Postmatch recovery practices carried out in professional football: a survey of 56 Portuguese professional football teams. Int J Sports Physiol Perform. 2022;17:748–54.
Sargent C, Lastella M, Halson SL, Roach GD. How much sleep does an elite athlete need? Int J Sports Physiol Perform. 2021;1–12.
Lastella M, Roach GD, Halson SL, Sargent C. Sleep/wake behaviours of elite athletes from individual and team sports. Eur J Sport Sci. 2015;15:94–100.
Walsh NP, Halson SL, Sargent C, Roach GD, Nédélec M, Gupta L, et al. Sleep and the athlete: narrative review and 2021 expert consensus recommendations. Br J Sports Med. 2020. https://doi.org/10.1136/bjsports-2020-102025.
Gupta L, Morgan K, Gilchrist S. Does elite sport degrade sleep quality? A systematic review. Sport Med. 2017;47:1317–33.
Charest J, Grandner MA. Sleep and athletic performance: impacts on physical performance, mental performance injury risk and recovery, and mental health. Sleep Med Clin. 2020;15:41–57. https://doi.org/10.1016/j.jsmc.2019.11.005.
Halson SL. Sleep in elite athletes and nutritional interventions to enhance sleep. Sport Med. 2014;44:13–23.
Souissi N, Chtourou H, Aloui A, Hammouda O, Dogui M, Chaouachi A, et al. Effects of time-of-day and partial sleep deprivation on short-term maximal performances of judo competitors. J Strength Cond Res. 2013;27:2473–80.
Souissi W, Hammouda O, Ayachi M, Ammar A, Khcharem A, de Marco G, et al. Partial sleep deprivation affects endurance performance and psychophysiological responses during 12-minute self-paced running exercise. Physiol Behav. 2020;227:113165.
Jarraya S, Jarraya M, Chtourou H, Souissi N. Effect of time of day and partial sleep deprivation on the reaction time and the attentional capacities of the handball goalkeeper. Biol Rhythm Res. 2014;45:183–91.
Edwards BJ, Waterhouse J. Effects of one night of partial sleep deprivation upon diurnal rhythms of accuracy and consistency in throwing darts. Chronobiol Int. 2009;26:756–68.
Reyner LA, Horne JA. Sleep restriction and serving accuracy in performance tennis players, and effects of caffeine. Physiol Behav. 2013;120:93–6. https://doi.org/10.1016/j.physbeh.2013.07.002.
Lastella M, Memon AR, Vincent GE. Global research output on sleep research in athletes from 1966 to 2019: a bibliometric analysis. Clocks Sleep. 2020;2:99–119.
Doherty R, Madigan S, Warrington G, Ellis J. Sleep and nutrition interactions: implications for athletes. Nutrients. 2019;11:822.
Vitale KC, Owens R, Hopkins SR, Malhotra A. Sleep hygiene for optimizing recovery in athletes: review and recommendations. Int J Sports Med. 2019;40:535–43.
Silva AC, Silva A, Edwards BJ, Tod D, Souza Amaral A, de Alcântara BD, et al. Sleep extension in athletes: what we know so far—a systematic review. Sleep Med. 2020;77:128–35.
Lastella M, Halson S, Vitale J, Memon A, Vincent G. To Nap or Not to Nap? A systematic review evaluating napping behavior in athletes and the impact on various measures of athletic performance. Nat Sci Sleep. 2021.
Bonnar D, Bartel K, Kakoschke N, Lang C. Sleep interventions designed to improve athletic performance and recovery: a systematic review of current approaches. Sport Med. 2018;48:683–703. https://doi.org/10.1007/s40279-017-0832-x.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:W-65.
Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:264–9.
Schardt C, Adams MB, Owens T, Keitz S, Fontelo P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak. 2007;7:1–6.
McKay AKA, Stellingwerff T, Smith ES, Martin DT, Mujika I, Goosey-Tolfrey VL, et al. Defining training and performance caliber: a participant classification framework. Int J Sports Physiol Perform. 2022;17:317–31.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:1–9.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:1–8.
Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013;66:408–14. https://doi.org/10.1016/j.jclinepi.2012.09.016.
Dunican IC, Martin DT, Halson SL, Reale RJ, Dawson BT, Caldwell JA, et al. The effects of the removal of electronic devices for 48 hours on sleep in elite judo athletes. J Strength Cond Res. 2017;31:2832–9.
Jones BJ, Kaur S, Miller M, Spencer RMC. Mindfulness-based stress reduction benefits psychological well-being, sleep quality, and athletic performance in female collegiate rowers. Front Psychol. 2020;11:572980.
Jones MJ, Dawson B, Eastwood PR, Halson SL, Miller J, Murray K, et al. Influence of electronic devices on sleep and cognitive performance during athlete training camps. J Strength Cond Res. 2019.
Boukhris O, Trabelsi K, Ammar A, Abdessalem R, Hsouna H, Glenn JM, et al. A 90 min daytime nap opportunity is better than 40 min for cognitive and physical performance. Int J Environ Res Public Health. 2020;17:4650.
Petit E, Mougin F, Bourdin H, Tio G, Haffen E. A 20-min nap in athletes changes subsequent sleep architecture but does not alter physical performances after normal sleep or 5-h phase-advance conditions. Eur J Appl Physiol. 2014;114:305–15.
Roberts SSH, Teo WP, Aisbett B, Warmington SA. Extended sleep maintains endurance performance better than normal or restricted sleep. Med Sci Sports Exerc. 2019;51:2516–23.
Zhao J, Tian Y, Nie J, Xu J, Liu D. Red light and the sleep quality and endurance performance of Chinese female basketball players. J Athl Train. 2012;47:673–8.
Boukhris O, Trabelsi K, Ammar A, Hsouna H, Abdessalem R, Altmann S, et al. Performance, muscle damage, and inflammatory responses to repeated high-intensity exercise following a 40-min nap. Res Sport Med. 2021. https://doi.org/10.1080/15438627.2021.1988951.
Hsouna H, Boukhris O, Hill DW, Abdessalem R, Trabelsi K, Ammar A, et al. A daytime 40-min nap opportunity after a simulated late evening soccer match reduces the perception of fatigue and improves 5-m shuttle run performance. Res Sport Med. 2021. https://doi.org/10.1080/15438627.2021.1917400.
Mah CD, Mah KE, Kezirian EJ, Dement WC. The effects of sleep extension on the athletic performance of collegiate basketball players. Sleep. 2011;34:943–50.
Morita Y, Ogawa K, Uchida S. The effect of a daytime 2-hour nap on complex motor skill learning. Sleep Biol Rhythms. 2012;10:302–9.
Schwartz J, Simon RDJ. Sleep extension improves serving accuracy: a study with college varsity tennis players. Physiol Behav. 2015;151:541–4.
Nishida M, Yamamoto K, Murata Y, Ichinose A, Shioda K. Exploring the effect of long naps on handball performance and heart rate variability. Sport Med Int Open. 2021;5:E73-80.
Romdhani M, Souissi N, Chaabouni Y, Mahdouani K, Driss T, Chamari K, et al. Improved physical performance and decreased muscular and oxidative damage with postlunch napping after partial sleep deprivation in athletes. Int J Sports Physiol Perform. 2020;15:874–83.
Romdhani M, Souissi N, Moussa-Chamari I, Chaabouni Y, Mahdouani K, Sahnoun Z, et al. Caffeine use or napping to enhance repeated sprint performance after partial sleep deprivation: Why not both? Int J Sports Physiol Perform. 2021;16:711–8.
Romdhani M, Souissi N, Dergaa I, Moussa-Chamari I, Abene O, Chtourou H, et al. The effect of experimental recuperative and appetitive post-lunch nap opportunities, with or without caffeine, on mood and reaction time in highly trained athletes. Front Psychol. 2021;12:1–11.
Van Ryswyk E, Weeks R, Bandick L, O’Keefe M, Vakulin A, Catcheside P, et al. A novel sleep optimisation programme to improve athletes’ well-being and performance. Eur J Sport Sci. 2017;17:144–51.
Daaloul H, Souissi N, Davenne D. Effects of napping on alertness, cognitive, and physical outcomes of karate athletes. Med Sci Sports Exerc United States. 2019;51:338–45.
Swinbourne R, Miller J, Smart D, Dulson DK, Gill N. The effects of sleep extension on sleep, performance, immunity and physical stress in rugby players. Sport. 2018;6:42.
Rosa JPP, Silva A, Rodrigues DF, Simim MA, Narciso FV, Tufik S, et al. Effect of bright light therapy on delayed sleep/wake cycle and reaction time of athletes participating in the Rio 2016 Olympic Games. Chronobiol Int. 2018;35:1095–103. https://doi.org/10.1080/07420528.2018.1459660.
Suppiah HT, Low CY, Choong G, Chia M. Effects of a short daytime nap on shooting and sprint performance in high-level adolescent athletes. Int J Sports Physiol Perform. 2018;14:76–82.
Lever JR, Murphy AP, Duffield R, Fullagar HHK. A combined sleep hygiene and mindfulness intervention to improve sleep and well-being during high-performance youth tennis tournaments. Int J Sports Physiol Perform. 2020;16:250–8.
Fullagar H, Skorski S, Duffield R, Meyer T. The effect of an acute sleep hygiene strategy following a late-night soccer match on recovery of players. Chronobiol Int England. 2016;33:490–505.
Chauvineau M, Pasquier F, Guyot V, Aloulou A, Nedelec M. Effect of the depth of cold water immersion on sleep architecture and recovery among well-trained male endurance runners. Front Sport Act Living. 2021;3:1–12.
Duffield R, Murphy A, Kellett A, Reid M. Recovery from repeated on-court tennis sessions: combining cold-water immersion, compression, and sleep recovery interventions. Int J Sports Physiol Perform. 2014;9:273–82.
Nedelec M, Halson S, Abaidia A-E, Ahmaidi S, Dupont G. Stress, sleep and recovery in elite soccer: a critical review of the literature. Sport Med. 2015;45:1387–400.
Thornton HR, Duthie GM, Pitchford NW, Delaney JA, Benton DT, Dascombe BJ. Effects of a 2-week high-intensity training camp on sleep activity of professional rugby league athletes. Int J Sports Physiol Perform. 2017;12:928–33.
Tassi P, Muzet A. Sleep inertia. Sleep Med Rev. 2000;4:341–53.
Lastella M, Halson SL, Vitale JA, Memon AR, Vincent GE. To nap or not to nap? A systematic review evaluating napping behavior in athletes and the impact on various measures of athletic performance. Nat Sci Sleep. 2021;13:841–62.
Stepanski EJ, Wyatt JK. Use of sleep hygiene in the treatment of insomnia. Sleep Med Rev. 2003;7:215–25.
Caia J, Scott TJ, Halson SL, Kelly VG. The influence of sleep hygiene education on sleep in professional rugby league athletes. Sleep Health. 2018;4:364–8. https://doi.org/10.1016/j.sleh.2018.05.002.
O’Donnell S, Driller MW. Sleep-hygiene education improves sleep indices in elite female athletes. Int J Exerc Sci. 2017;10:522–30.
Cho YM, Ryu SH, Lee BR, Kim KH, Lee E, Choi J. Effects of artificial light at night on human health: a literature review of observational and experimental studies applied to exposure assessment. Chronobiol Int. 2015;32:1294–310.
Okamoto-Mizuno K, Mizuno K. Effects of thermal environment on sleep and circadian rhythm. J Physiol Anthropol. 2012;31:14. https://doi.org/10.1186/1880-6805-31-14.
Nagare R, Plitnick B, Figueiro MG. Does the iPad Night Shift mode reduce melatonin suppression? Light Res Technol. 2019;51:373–83.
Touitou Y, Reinberg A, Touitou D. Association between light at night, melatonin secretion, sleep deprivation, and the internal clock: health impacts and mechanisms of circadian disruption. Life Sci. 2017;173:94–106. https://doi.org/10.1016/j.lfs.2017.02.008.
Yeager RL, Oleske DA, Sanders RA, Watkins JB, Eells JT, Henshel DS. Melatonin as a principal component of red light therapy. Med Hypotheses. 2007;69:372–6.
Borsa PA, Larkin KA, True JM. Does phototherapy enhance skeletal muscle contractile function and postexercise recovery? A systematic review. J Athl Train. 2013;48:57–67.
Leal-Junior ECP, Vanin AA, Miranda EF, de Carvalho PDTC, Dal Corso S, Bjordal JM. Effect of phototherapy (low-level laser therapy and light-emitting diode therapy) on exercise performance and markers of exercise recovery: a systematic review with meta-analysis. Lasers Med Sci. 2015;30:925–39.
Szymusiak R. Body temperature and sleep. Handb Clin Neurol. 2018. https://doi.org/10.1016/B978-0-444-63912-7.00020-5.
Machado AF, Ferreira PH, Micheletti JK, de Almeida AC, Lemes ÍR, Vanderlei FM, et al. Can water temperature and immersion time influence the effect of cold water immersion on muscle soreness? A systematic review and meta-analysis. Sports Med. 2016;46:503–14.
Bühlmayer L, Birrer D, Röthlin P, Faude O, Donath L. Effects of mindfulness practice on performance-relevant parameters and performance outcomes in sports: a meta-analytical review. Sport Med. 2017;47:2309–21.
Halson SL. Sleep monitoring in athletes: motivation, methods, miscalculations and why it matters. Sport Med. 2019;49:1487–97. https://doi.org/10.1007/s40279-019-01119-4.
Rusch HL, Rosario M, Levison LM, Olivera A, Livingston WS, Wu T, et al. The effect of mindfulness meditation on sleep quality: a systematic review and meta-analysis of randomized controlled trials. Ann N Y Acad Sci. 2019;1445:5–16.
Funding
Lúcio Cunha was supported by the Portuguese Foundation for Science and Technology [UI/BD/151482/2021]. No other sources of funding were used to assist in the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
LC and PF devised the study. LC, EM, and PF developed the methodology and interpreted the data. LC performed database searches and wrote the initial draft of the manuscript. LC and JC executed the screening process, data extraction, and risk-of-bias assessment. The manuscript was critically revised by JC, EM, JB, ML, and PF. PF supervised the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cunha, L.A., Costa, J.A., Marques, E.A. et al. The Impact of Sleep Interventions on Athletic Performance: A Systematic Review. Sports Med - Open 9, 58 (2023). https://doi.org/10.1186/s40798-023-00599-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40798-023-00599-z