Abstract
Objectives
To investigate the potential protective role of exercise on the odds of COVID-19 infection in unvaccinated contact persons (CPs) who were at higher risk of infection due to confirmed contact with infected persons.
Methods
Before the onset of the vaccination campaign, the first wave of the CoCo-Fakt online survey was conducted with SARS-CoV-2-positive persons and their confirmed contacts who were isolated/quarantined between 1 March 2020 and 9 December 2020. Within this analysis, 5338 CPs were included and divided into those who subsequently tested positive (CP-P) and those who remained negative (CP-N). We assessed demographics as well as pre-pandemic lifestyle characteristics including physical activity (PA; type, frequency, time, intensity; duration clustered as ‘below PA guidelines’, ‘meeting PA guidelines’, and ‘above PA guidelines’; intensity clustered as ‘low intensity’ and ‘moderate-to-vigorous intensity’) and sedentary behaviour.
Results
A greater percentage of CP-Ns reported being active before the pandemic compared to CP-Ps (69% vs. 63%; p = .004). Moreover, CP-Ns reported higher PA duration (164.1 min/week vs. 143.2 min/week; p = .038) and higher PA intensities than CP-Ps (67% vs. 60% moderate-to-vigorous intensity, 33% vs. 40% low intensity; p = .003). Adjusting for age, sex, socioeconomic status, migration background, and pre-existing chronic diseases, the odds of infection were negatively associated with exercise (yes/no) (Nagelkerke R2 = 1.9%), PA levels above PA guidelines (Nagelkerke R2 = 2.0%), and PA intensity (Nagelkerke R2 = 1.8%).
Conclusion
Due to the beneficial effects of PA on the odds of infection, an active lifestyle should be promoted especially during possible subsequent pandemics (while taking into account necessary hygiene measures). Moreover, inactive and chronically ill persons should be especially encouraged to adopt a healthier lifestyle.
Similar content being viewed by others
Key Points
-
In unvaccinated persons who had confirmed contact with a COVID 19-infected person, pre-pandemic physical activity was associated with lower odds of infection.
-
Engaging in physical activity at all, but also higher intensities and durations resulted in reduced odds of infection.
Introduction
Although, 3 years on, the coronavirus disease 2019 (COVID-19) pandemic is gradually turning into an endemic-wave occurrence [1], it remains an incisive episode that leaves unanswered questions, also with regard to possible future pandemics. Before the onset of the vaccination campaign, elderly patients and patients with chronic diseases were at especially high risk of severe courses and death [2, 3], which led to strict measures such as social distancing, lockdowns, and mask-wearing [4]. Though these measures also entailed negative consequences such as psychological perturbations [5], poorer sleep patterns [6], and changes in lifestyle [6,7,8], they were, along with vaccination, the most important factors in avoiding the overloading of the health care system and fatal courses [4]. However, considering the substantial psychological stress caused by such rigorous measures, further possibilities for the prevention of COVID-19 should be investigated. In the few studies available to date (March 2023), physical activity (PA) before a COVID-19 infection has been shown to have a beneficial effect on infectivity and outcomes, such as hospitalisation, intensive care unit admission, mortality, and severity and number of post-COVID-19 symptoms [9,10,11,12,13]. These findings are assumed to be due to the immunomodulatory and anti-inflammatory effects of exercise leading to protection from chronic diseases, reduced risk of severe disease progression, and lower hospitalisation rates in COVID-19 patients [9, 12].
However, most studies have evaluated the infection risk in the general population and not among specifically exposed persons who therefore are at an increased risk of SARS-CoV-2 infection [14, 15]. A contact person (CP) is defined as any person who has had close exposure (< 1.5 m) to a confirmed COVID-19 case for longer than 10 min without adequate protection (FFP2 or medicine mask) and/or any person who has had face-to-face contact (< 1.5 m) without adequate protection, regardless of duration of conversation or direct contact (with respiratory secretions), and/or any person who was present in the same room with a case and probably high concentration of infectious aerosols regardless of distance for longer than 10 min, even if a FFP2 mask was worn continuously and correctly [16]. Therefore, the aim of this analysis was to determine, based on data from the first wave of the CoCo-Fakt cohort study, to what extent PA can protect confirmed contacts without vaccination against infection. Additionally, we investigated whether increased sedentary behaviour increases the odds of getting infected with COVID-19 in CPs.
Methods
Study Design
Since the beginning of the SARS-CoV-2 outbreak at the end of February 2020, persons with residence in Cologne who tested positive for SARS-CoV-2 by PCR testing (infected persons, or IPs) were reported to the Cologne Health Authority as required by the German Infection Protection Act. Those persons were contacted, registered using the software “Digitales Kontakt Management” [digital contact management] (DiKoMa) [17], quarantined based on the German Infection Protection Act, and interviewed in a standardised manner about possible transmission routes, medical history, symptoms, and relevant CPs. To detect possible infection early and prevent further spread, the CPs were also contacted and quarantined. During the survey phase, isolation or quarantine usually lasted 10 days from symptom onset (for IPs) or 14 days from the last contact (for CPs).
Based on this procedure, the Cologne-Corona-Beratung und Unterstützung Für Index- und KontAkt-Personen während der Quarantäne-ZeiT (CoCo-Fakt) survey was conducted. This analysis is part of the CoCo-Fakt cohort study that assessed demographic data, transmission routes, living situation, adherence, psychosocial consequences, coping strategies, and lifestyle during quarantine in three waves. This analysis includes data of the first wave, which was conducted before the vaccination campaign with IPs and their CPs who were isolated/quarantined between 1 March 2020 and 9 December 2020 and utilised the online survey tool Unipark [18]. The questionnaire (Additional file 1) was developed and modified according to the COVID-19 Snapshot Monitoring (COSMO) study [19]. Answering the questionnaire took approximately 30 min, with all questions answered on a voluntary basis. The study protocol was published previously [20].
Sample
A total of 36,498 persons registered in DiKoMa between February and 9 December 2020 were extracted from the dataset. Exclusion criteria were: under 16 years of age, missing informed consent, noncompliance, deceased patients, and patients in medical or nursing facilities.
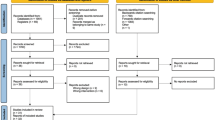
An email with information about the background of the study, the summarized content, and an invitation to follow the link to the online survey was sent to 33,699 people, of whom 13,057 gave their informed consent and answered the questionnaire. After cleaning the sample, the CoCo-Fakt cohort comprised 10,547 data records. Of these, the 5338 CPs who provided any information on pre-pandemic PA behaviour were included in this analysis and clustered into groups: CPs who did not test positive for coronavirus (uninfected CP, or CP-N; ‘I was a contact person’, ‘I was a contact person several times’; n = 4884) and CPs who subsequently tested positive for coronavirus (infected contact person, or CP-P; ‘I was a contact person and tested positive for the coronavirus afterwards’; n = 454) (Fig. 1).
Survey
The following parameters were assessed:
Demographic Data
We assessed age (years), sex (male/female), socioeconomic status (SES), migration background, and smoking status [21]. SES was calculated using the participants’ answers on education and vocational training and categorised as high, middle, or low based on the German Health Interview and Examination Survey for Adults (DEGS) [22]. Migration background was based on the language primarily spoken at home (German = no; any other language = yes). Additionally, we assessed current smoking status (yes/no).
We also recorded whether the subjects had one or more of the following chronic diseases:
-
Asthma
-
Chronic bronchitis/chronic obstructive pulmonary disease/pulmonary emphysema
-
Heart attack/coronary heart disease
-
Congestive heart failure
-
Stroke
-
Diseases of the musculoskeletal system
-
Diabetes type 1/type 2
-
Hypertension/high blood pressure
-
Hypercholesterolemia
-
Allergies
-
Chronic liver diseases
-
Chronic kidney problems/kidney failure
-
Depression
-
Cancer
-
Inflammatory bowel disease
-
Other
Lifestyle
PA, relaxation, and sedentary behaviour before the pandemic and during the quarantine period were recorded (modified according to [23]). Our analysis only included lifestyle parameters before the pandemic. Daily life activities, such as walking the dog, gardening, and occupational or home activities were excluded.
Physical Activity
We assessed whether the subjects were active (yes/no) as well as the type, intensity (very light, light, moderate, vigorous, or very vigorous), frequency (number of sessions per week), and duration (minutes per session) of activity before the pandemic. Based on the type of activity and its intensity, an average baseline metabolic equivalent (MET) value was derived using the Compendium of Physical Activities by Ainsworth et al. [24]. If subjects reported not being active, the baseline MET value was set to 1.0. PA intensity was categorized based on baseline MET value as ‘sedentary behaviour’ (1.0–1.5 METs), ‘light intensity’ (1.6–2.9 METs), ‘moderate intensity’ (3–5.9 METs) or ‘vigorous intensity’ (≥ 6 METs). For the present analysis, the categories ‘sedentary behaviour’ and ‘light intensity’ were combined into ‘low intensity’, while ‘moderate intensity’ and ‘vigorous intensity’ were combined into ‘moderate-to-vigorous intensity’.
PA duration per week was calculated taking into account all activities with self-reported moderate, vigorous, or very vigorous intensities using the following formula:
PA duration per week = PA minutes per week * PA frequency per week.
If the subject reported being inactive, the PA duration per week was set to 0 min.
Based on the World Health Organization (WHO) Guidelines on Physical Activity and Sedentary Behaviour [25] and Bull et al. [26], PA duration was categorised into three PA levels: ‘below PA guidelines’ (< 150 min/week), ‘meeting PA guidelines’ (150 to < 300 min/week), and ‘above PA guidelines’ (≥ 300 min/week).
Sedentary Behaviour
Sedentary behaviour was assessed in minutes per week in occupational (office work with and without screen work, driving a car, other) and private settings (using a phone, watching TV, driving a car, reading/writing, hobbies, other). From this data, total time spent sitting, screen time (office work with screen work, using a phone, watching TV), and transportation time (driving a car in occupational and private settings) were summed.
Data Cleaning and Analysis
Implausible and duplicate data was deleted. Types of PA were converted from answers to open-ended questions into clustered labelled numerical variables. Missing variables were set to the value “9999” and defined as such. Where applicable, missing data was reproduced using the answers to open-ended questions.
We evaluated frequency (percentage), central tendency (mean values) and variation (standard deviation) to describe the sample. Associations between participant characteristics (age, sex, migration background, SES, chronic diseases, smoking status) and lifestyle factors were examined using Pearson’s χ2 tests and Mann–Whitney U-tests. Effect sizes were calculated for significant differences between CP-Ns and CP-Ps using Cohen’s d (Mann–Whitney U t-test; trivial: < 0.2; small: 0.2–0.5; moderate: 0.5–0.8; large. ≥ 0.8) or Cramer’s V (Pearson’s χ2 test; small: 0.06–0.15; moderate: 0.16–0.26; large: ≥ 0.26).
Logistic regression analyses were conducted to determine the effects of PA on susceptibility to COVID-19 infection; therefore, odds ratios (OR) and 95% confidence intervals (CI) were calculated. The covariates were age, sex, migration background, SES, chronic diseases, and smoking status. All analyses met the assumptions for the use of logistic regression analyses.
The level of statistical significance was set to p < 0.05. All analyses were performed using SPSS software version 29.0.
Results
Demographic Data
The sample had a mean age of 41.1 years (SD 14.2; range: 16 to 93 years) and included 64.3% females (Table 1). Overall, 214 subjects (4.1%) had a migration background, 4314 (81.3%) had a high SES, 956 (18.0%) had a middle SES and 38 (0.7%) had a low SES. Both migration background and SES were significantly different between CP-Ns and CP-Ps (migration background: p = 0.045; SES: p = 0.037). Furthermore, 4160 persons (78.7%) had no comorbidities, 547 (10.3%) had one comorbidity and 581 (11.0%) had two or more comorbidities. The CP-Ps were significantly more likely to have at least one chronic disease than the CP-Ns (p = 0.003). In addition, 1010 persons (21.4%) reported smoking prior to the pandemic. More CP-Ns were smokers than CP-Ps (p < 0.001).
Lifestyle
Physical Activity
In total, 3658 persons (68.5%) reported being active before the pandemic (Table 2a). The average PA duration was 162.4 min/week (SD 194.1 min/week). The PA levels of most subjects were below guidelines (n = 2705, 56.7%). Significantly more CP-Ns were active before the pandemic than CP-Ps (69.1% vs. 62.6%; p = 0.004). Furthermore, CP-Ns reported more PA per week than CP-Ps (164.1 min/week vs. 143.2 min/week; p = 0.038), resulting in higher PA levels (above PA guidelines: 20.6% vs. 13.9%; meeting PA guidelines: 23.1% vs. 25.6%; below PA guidelines: 56.3% vs. 60.5%; p = 0.006). CP-Ns also performed higher intensity PA than CP-Ps (low intensity: 33.1% vs. 40.2%; moderate-to-vigorous intensity: 66.9% vs. 59.8%; p = 0.003). Controlling for demographics, chronic conditions, and smoking, the odds of becoming infected were significantly higher in inactive people (OR 1.293; 95% CI: 1.036–1.613; exercise (yes) as reference group; Table 3a, Fig. 2a). People who were below PA guidelines had 1.45-fold increased odds of infection compared with people above PA guidelines (95% CI: 1.059–1.998; Table 3b, Fig. 2b). People meeting PA guidelines had 1.53-fold increased odds of infection compared with people above PA guidelines (95% CI: 1.077–2.162, Table 3b, Fig. 2b). Also, people who reported low intensity had 1.28-fold increased odds of infection compared with those who reported moderate-to-vigorous intensity (95% CI: 1.022–1.593, Table 3c, Fig. 2c).
Risk factors for COVID-19 infection; binary logistic regression analyses, adjusted for age, sex, migration background, and socioeconomic status. A Exercise (no compared to yes); B PA guidelines (below and meeting PA guidelines compared to above PA guidelines); C PA intensity (low intensity vs. moderate-to-vigorous intensity). PA, physical activity
Sedentary Behaviour
The average total sedentary behaviour was 4.1 h/day (SD 3.5 h/day), of which screen time was 3.0 h/day (SD 2.8 h/day; Table 2c). Neither average total sedentary behaviour nor screen time was significantly different between the two groups.
Discussion
To our knowledge, this is the first study analysing the association between exercise and COVID-19 infection in unvaccinated persons who had a confirmed relevant contact with an infected individual. We found that CPs who reported being consistently physically active prior to the pandemic had 29% lower odds of being infected with COVID-19 than inactive CPs. In addition, our data indicated reduced odds of infection with increased PA levels. Specifically, the odds of COVID-19 infection decreased by 53% and 45%, respectively, in CPs whose PA levels were below 150 min and between 150 and 300 min, respectively, compared with CPs whose PA levels were greater than 300 min/week. Furthermore, the odds of infection increased by 28% among CPs who reported performing low intensity pre-pandemic compared with those who reported moderate-to-vigorous intensity.
These findings are consistent with those of other studies examining PA and risk of infection. For example, PA lowered the risk of COVID-19 infection by 11% in a systematic review and meta-analysis [12]. Furthermore, Cunningham found, at county level, that PA was negatively associated with the number of COVID-19 cases per 100,000 inhabitants [27].
The underlying mechanisms behind these findings can only be speculated. Data on the risk of upper respiratory tract infection suggest that PA increases the circulation of immunoglobulins, neutrophils, and natural killer cells, thereby enhancing immune response [28]. Although levels decrease a few hours after the end of a PA session, PA induces overall increased immunosurveillance of pathogens and thereby lowers susceptibility to infection. Along these lines, a systematic review and meta-analysis showed that regular moderate-to-vigorous PA resulted in a 31% lower prospective risk of upper respiratory tract infection [29].
In addition to improved immunosurveillance, PA has beneficial effects on systemic inflammation and thus on preventing the development of chronic diseases [30]; in our model, it influenced the odds of infection with COVID-19 alongside lifestyle factors. To date, most studies have focused on the association between comorbidities and patients’ COVID-19 outcomes. For example, a systematic review and meta-analysis included 16 studies investigating various comorbidities as potential risk factors for an infection [31]. The results indicated only obesity as a risk factor; schizophrenia, dementia, and coronary heart disease resulted in lower odds of infection. Other comorbidities, such as hypertension, high cholesterol, and diabetes, had no significant influence on infection. Nevertheless, data in the field remain ambiguous, and further studies are needed to clarify the association between individual diseases and the risk of infection.
Surprisingly, our data showed that individuals who smoked before the pandemic had a lower risk of infection than non-smokers. Similarly, another review and meta-analysis showed that, although smokers were more likely to present for testing, they were less likely to test positive for SARS-CoV-2 [32]. Its authors discussed the methods that led to this result critically. Among other factors, an inaccurate recording of smoking status was possible, whereby ex-smokers were potentially counted as non-smokers. A change in the sensitivity of COVID-19 testing methods and/or impaired access to or lower prioritisation within the healthcare system were other possible contributing factors. Still, the extent to which these factors may explain the findings is unclear.
Strengths and Limitations
The major strength of this study is the large sample size, which was acquired using systematic data collection by the largest public health department in Germany. As no authorised vaccine was available at the time of the survey, the data are free of any bias that may have resulted from vaccination. Moreover, the sample consisted entirely of clearly defined CPs who had confirmed exposure to the virus.
Regardless, the study has several limitations. First, the data are based on self-reporting which could have led to answering based on social desirability, misreporting or overestimating PA levels. With about 43% of the sample achieving the WHO recommendations on PA, the data resemble that of the German Health Update by the Robert Koch Institute. According to this data, about 45% of females and 51% of males achieved the WHO PA recommendations in force at the time of at least 150 min/week [33]. Secondly, the data are limited by being confined to a regional cohort, as well as the questionnaires being mainly completed by individuals with high SES. We are aware that the assessment of SES is at risk of being biased, as people with lower SES might have poorer access to the internet or fewer skills with which to answer the survey. Thirdly, answering the questionnaire took about 30 min. Therefore, answering fatigue cannot be ruled out. Nevertheless, the amount of completely answered questionnaires is almost 60%. Fourthly, due to the adjustments of lockdowns and reopening of sports facilities during the course of the pandemic, we referred to the pre-pandemic data. This temporal distance might have led to misreporting or changes in behaviour as a result of the pandemic [34]. It remains unclear whether current lifestyle has a more sensitive effect on the risk of infection than pre-pandemic status.
Furthermore, adherence to quarantine measures, which was not investigated here, might have had an important impact on infection risk. However, analyses of this dataset concerning adherence have been published previously [35]. Finally, it must be emphasized that at this stage of the pandemic, nearly 70% of the world population has received at least one dose of a COVID-19 vaccine [36], and that vaccination was one of the most important pandemic control measures.
Nevertheless, our data show that PA had an impact on the odds of infection independently of vaccination. Still, the models were explained only to a small extent by PA or fitness; further studies are required to examine the risk factors.
Conclusion
Having considered the limitations, we conclude that the data indicate that pre-pandemic, self-reported PA (especially for at least 300 min/week and at moderate-to-vigorous intensity) was associated with lower odds of COVID-19 infection in unvaccinated CPs. Other than smoking status and comorbidities, PA was the strongest modifiable risk factor for infection. Although the long-term effects of PA can only be speculated, inactive persons and persons with chronic conditions should be encouraged in the context of medical examinations and check-ups to adopt a more active lifestyle.
Availability of Data and Materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CoCo-Fakt:
-
Cologne-Corona-Beratung und Unterstützung Für Index- und KontAKt-Personen während der Quarantäne-ZeiT (Cologne-Corona counselling and support for index and contacts during the quarantine period—author’s translation)
- COVID-19:
-
Coronavirus disease
- CP:
-
Contact person
- CP-P:
-
Contact person who tested positive
- CP-N:
-
Contact person who stayed negative
- DiKoMa:
-
Digitales Kontaktmanagement (digital contact management)
- DEGS:
-
German Health Interview and Examination Survey for Adults
- IP:
-
Infected person
- MET:
-
Metabolic equivalent
- NCD:
-
Non-communicable disease
- PA:
-
Physical activity
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus type 2
- SES:
-
Socioeconomic status
References
Robert Koch Institute. RKI—Infektionskrankheiten A-Z—Antworten auf häufig gestellte Fragen zum Coronavirus SARS-CoV-2/Krankheit COVID-19, 2023. https://www.rki.de/SharedDocs/FAQ/NCOV2019/gesamt.html?nn=2386228. Accessed 21 Feb 2023
World Health Oraganization. WHO Coronavirus (COVID-19) Dashboard|WHO Coronavirus (COVID-19) Dashboard with vaccination data, 2022. https://covid19.who.int/. Accessed 18 Feb 2023.
World Health Organization. COVID-19 high risk groups, 2021. https://www.who.int/westernpacific/emergencies/covid-19/information/high-risk-groups. Accessed 27 Nov 2022.
Woods JA, Hutchinson NT, Powers SK, et al. The COVID-19 pandemic and physical activity. Sports Med Health Sci. 2020;2:55–64. https://doi.org/10.1016/j.smhs.2020.05.006.
Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–20. https://doi.org/10.1016/s0140-6736(20)30460-8.
Trabelsi K, Ammar A, Masmoudi L, et al. Globally altered sleep patterns and physical activity levels by confinement in 5056 individuals: ECLB COVID-19 international online survey. Biol Sport. 2021;38:495–506. https://doi.org/10.5114/biolsport.2021.101605.
Washif JA, Farooq A, Krug I, et al. Training during the COVID-19 lockdown: knowledge, beliefs, and practices of 12,526 athletes from 142 countries and six continents. Sports Med. 2022;52:933–48. https://doi.org/10.1007/s40279-021-01573-z.
Wessely S, Tappiser M, Eisenburger N, Feddern S, Gehlhar A, Kilimann A, et al. Changes in alcohol consumption, eating behaviors, and body weight during quarantine measures: analysis of the CoCo-Fakt study. Obes Facts. 2022;15(4):570–80. https://doi.org/10.1159/000524352.
Sallis R, Young DR, Tartof SY, et al. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients. Br J Sports Med. 2021;55:1099–105. https://doi.org/10.1136/bjsports-2021-104080.
Steenkamp L, Saggers RT, Bandini R, et al. Small steps, strong shield: directly measured, moderate physical activity in 65 361 adults is associated with significant protective effects from severe COVID-19 outcomes. Br J Sports Med. 2022;56:568–76. https://doi.org/10.1136/bjsports-2021-105159.
Lee SW, Lee J, Moon SY, et al. Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study. Br J Sports Med. 2022;56:901–12. https://doi.org/10.1136/bjsports-2021-104203.
Ezzatvar Y, Ramírez-Vélez R, Izquierdo M, et al. Physical activity and risk of infection, severity and mortality of COVID-19: a systematic review and non-linear dose-response meta-analysis of data from 1 853 610 adults. Br J Sports Med. 2022;56:1188–93. https://doi.org/10.1136/bjsports-2022-105733.
Jimeno-Almazán A, Martínez-Cava A, Buendía-Romero Á, et al. Relationship between the severity of persistent symptoms, physical fitness, and cardiopulmonary function in post-COVID-19 condition. A population-based analysis. Intern Emerg Med. 2022;17:2199–208. https://doi.org/10.1007/s11739-022-03039-0.
Tian T, Huo X. Secondary attack rates of COVID-19 in diverse contact settings, a meta-analysis. J Infect Dev Ctries. 2020;14:1361–7. https://doi.org/10.3855/jidc.13256.
Ng OT, Marimuthu K, Koh V, Pang J, Linn KZ, Sun J, et al. SARS-CoV-2 seroprevalence and transmission risk factors among high-risk close contacts: a retrospective cohort study. Lancet Infect Dis. 2021;21:333–43. https://doi.org/10.1016/s1473-3099(20)30833-1.
Robert-Koch-Institut. RKI - Coronavirus SARS-CoV-2 - Kontaktpersonen-Nachverfolgung (KP-N) bei SARS-CoV-2-Infektionen, 2022. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Kontaktperson/Management.html;jsessionid=7FEF8435A72EBF7C6DF2495040FA3F6B.internet051?nn=13490888#doc13516162bodyText10. Accessed 23 Sep 2022.
Neuhann F, Buess M, Wolff A, et al. Entwicklung einer Software zur Unterstützung der Prozesse im Gesundheitsamt der Stadt Köln in der SARS-CoV-2-Pandemie, Digitales Kontaktmanagement (DiKoMa). Epidemiol Bull. 2020;23:3–11. https://doi.org/10.25646/6923.
Tivian. Startseite|Unipark, 2023. https://www.unipark.com/en/. Accessed 18 Feb 2023.
WHO Regional Office for Europe. COVID-19 Snapshot MOnitoring (COSMO Standard): Monitoring knowledge, risk perceptions, preventive behaviours, and public trust in the current coronavirus outbreak—WHO standard protocol; PsychArchives 2020. https://doi.org/10.23668/PSYCHARCHIVES.2782
Joisten C, Kossow A, Book J, Broichhaus L, Daum M, Eisenburger N, et al. How to manage quarantine-adherence, psychosocial consequences, coping strategies and lifestyle of patients with COVID-19 and their confirmed contacts: study protocol of the CoCo-Fakt surveillance study, Cologne, Germany. BMJ Open. 2021;11:e048001. https://doi.org/10.1136/bmjopen-2020-048001.
Saß A-C, Lange C, Finger JD, Allen J, Born S, Hoebel J, et al. “Gesundheit in Deutschland aktuell”—Neue Daten für Deutschland und Europa Hintergrund und Studienmethodik von GEDA 2014/2015-EHIS. J Health Monit. 2017;2:83–90. https://doi.org/10.17886/RKI-GBE-2017-012.
Lampert T, Kroll L, Müters S, et al. Messung des sozioökonomischen Status in der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1). Bundesgesundheitsbl. 2013;56:631–6. https://doi.org/10.1007/s00103-012-1663-4.
Graf C, Schlepper S, Bauer C, Ferrari N, Frank S, Gartner L, et al. Feasibility and acceptance of exercise recommendations (10,000 steps a day) within routine German health check (check-up 35/GOÄ29)-study protocol. Pilot Feasibility Stud. 2016;2:52. https://doi.org/10.1186/s40814-016-0092-9.
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Tudor-Locke C, et al. 2011 compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–81. https://doi.org/10.1249/mss.0b013e31821ece12.
World Health Organization. WHO guidelines on physical activity and sedentary behaviour, 2020. https://apps.who.int/iris/bitstream/handle/10665/336657/9789240015111-eng.pdf. Accessed 15 Aug 2022.
Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451–62. https://doi.org/10.1136/bjsports-2020-102955.
Cunningham GB. Physical activity and its relationship with COVID-19 cases and deaths: analysis of U.S. counties. J Sport Health Sci. 2021;10:570–6. https://doi.org/10.1016/j.jshs.2021.03.008.
Nieman DC, Wentz LM. The compelling link between physical activity and the body’s defense system. J Sport Health Sci. 2019;8:201–17. https://doi.org/10.1016/j.jshs.2018.09.009.
Nieman DC, Henson DA, Austin MD, Sha W. Upper respiratory tract infection is reduced in physically fit and active adults. Br J Sports Med. 2011;45:987–92. https://doi.org/10.1136/bjsm.2010.077875.
Nieman DC. exercise is medicine for immune function: implication for COVID-19. Curr Sports Med Rep. 2021;20:395–401. https://doi.org/10.1249/jsr.0000000000000867.
Mishra P, Parveen R, Bajpai R, Agarwal N. Vitamin D deficiency and comorbidities as risk factors of COVID-19 infection: a systematic review and meta-analysis. J Prev Med Public Health. 2022;55:321–33. https://doi.org/10.3961/jpmph.21.640.
Simons D, Shahab L, Brown J, Perski O. The association of smoking status with SARS-CoV-2 infection, hospitalization and mortality from COVID-19: a living rapid evidence review with Bayesian meta-analyses (version 7). Addiction. 2021;116:1319–68. https://doi.org/10.1111/add.15276.
Richter A, Schienkiwitz A, Starker A, Krug S, Domanska O, Kuhnert R, et al. Gesundheitsfördernde Verhaltensweisen bei Erwachsenen in Deutschland—Ergebnisse der Studie GEDA 2019/2020-EHIS. J Health Monit. 2021. https://doi.org/10.25646/8460.
Tison GH, Avram R, Kuhar P, Abreau S, Marcus GM, Pletcher MJ, et al. Worldwide effect of COVID-19 on physical activity: a descriptive study. Ann Intern Med. 2020;173:767–70. https://doi.org/10.7326/m20-2665.
Book J, Broichhaus L, Grüne B, Nießen J, Wiesmüller GA, Joisten C, et al. Adherence to stay-at-home orders: awareness, implementation and difficulties of officially ordered quarantine measures in the context of the COVID-19 pandemic in Cologne—a retrospective cohort study. BMJ Open. 2022;12:e063358. https://doi.org/10.1136/bmjopen-2022-063358.
Mathieu E, Ritchie H, Rodés-Guirao L, Appel C, Giattino C, Hasell J et al. Coronavirus Pandemic (COVID-19). Our World in Data 2020. https://ourworldindata.org/covid-vaccinations. Accessed 3 Mar 2023
Acknowledgements
We would like to thank all members of the contact tracing team at the Cologne Health Authority and Hidayet Oruc for his support with the Turkish translation. Additionally, we would also like to thank all persons who participated in this questionnaire.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
NS wrote the manuscript. CJ, BG, AK and JN conceived and conducted the study. NS, SW and CJ ran all data analyses. AG conducted the questions regarding physical activity and sedentary lifestyle. TK contributed to the application at the Ethics Committee of the Medical Faculty of RWTH Aachen University as well as the evaluation and interpretation of this analysis. All authors read the manuscript and agreed to publication.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Participants were asked to actively consent to their participation in the online survey. Human Ethics Research Committee ethics approval was obtained from the Rheinisch-Westfälische Technische Hochschule Aachen Human Ethics Research Committee (351/20) and the research was conducted in accordance with the approved protocol.
Consent for Publication
Not applicable.
Competing Interests
Nikola Schmidt, Andreas Gehlhar, Barbara Grüne, Annelene Kossow, Thomas Kraus, Johannes Nießen, Stefanie Wessely and Christine Joisten declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Online survey of the first wave of the CoCo-Fakt cohort study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schmidt, N., Gehlhar, A., Grüne, B. et al. Self-Reported Pre-Pandemic Physical Activity and Likelihood of COVID-19 Infection: Data from the First Wave of the CoCo-Fakt Survey. Sports Med - Open 9, 48 (2023). https://doi.org/10.1186/s40798-023-00592-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40798-023-00592-6