Abstract
Background
The incidence of type 2 diabetes mellitus (T2DM) is rising rapidly in Malaysia. Modifying dietary intake is key to both the prevention and treatment of T2DM. This study aims to investigate the pattern of macronutrient intake among T2DM patients in Malaysia.
Methods
This study was carried out on adults aged between 35 and 70 years, residing in urban and rural Malaysian communities. A series of standardised questionnaires was used to assess the sociodemographic information, dietary intake and physical activity level of 15,353 respondents who provided informed consent to participate in this study. Blood sampling (finger prick test) and physical examination were performed to obtain blood glucose and anthropometric data, respectively. The Chi-square test was used to assess differences in the trends of macronutrient intake among T2DM patients.
Results
The total number of participants diagnosed with T2DM in this study was 2254. Of these, 453 (20.1%) were newly diagnosed, 1156 (51.3%) were diagnosed for ≤5 years and 645 (28.6%) were diagnosed for > 5 years. Male patients show that there were significant differences among the three groups of T2DM according to the following variables: age, BMI, residency, participant comorbidity of hypertension, family history of T2DM and hypertension, and active smoker. Meanwhile, female patients show significant differences among the three groups of T2DM according to the following variables: age, BMI, marital status, education level, residency, participant comorbidity of hypertension and family history of T2DM. Most of the male patients consumed appropriate proportions of carbohydrate (458, 60.7%) and protein (618, 81.9%). However, female patients did not show any significant differences of the macronutrients intake among the three groups of T2DM patients.
Conclusions
The pattern of dietary intake among T2DM patients in this study showed consumption of carbohydrate and protein within the range of Malaysian RNI, coupled with high fat intake. Compliance with the Recommended Nutrient Intake (RNI) was satisfactory for both carbohydrate and protein but not for fat. The pattern indicated a preference for fat rather than protein when carbohydrate intake was restricted.
Similar content being viewed by others
Introduction
The global prevalence of diabetes mellitus is estimated to rise from 9.3% (463 million cases) in 2019 to 10.2% (578 million) by 2030 and 10.9% (700 million) by 2045 [1, 2]. The prevalence of T2DM has been escalating rapidly in developing countries such as Malaysia [3]. The National Health and Morbidity Surveys (NMHS) in Malaysia reported an increase in T2DM prevalence from 15.2% in 2011 to 18.3% in 2019 [4, 5]. Meanwhile, the NHMS also reported that the prevalence of newly diagnosed T2DM cases (amongst those not known to have T2DM) in Malaysia increased from 8.0% in 2011 to 8.9% in 2019 [4, 5]. This group has the same risk of developing complications of diabetes as already-diagnosed T2DM patients. Newly diagnosed T2DM patients are more prone to developing T2DM complications at a later stage due to uncontrolled glucose levels [6]. T2DM is associated with both unmodifiable factors (age and genetics) and modifiable risk factors (obesity and dietary intake) [1].
Modification of dietary intake is key to both the prevention and treatment of T2DM [7]. The Nutrition Division of the Ministry of Health, Malaysia, has been promoting healthy eating practices among the Malaysian population to facilitate a higher quality of life. The healthy eating campaign included advocacy for the food pyramid guideline and the recent healthy meal intake guide of ‘quarter quarter half’ plate portions [8]. These campaigns were derivatives of the macronutrient guideline provided by the Malaysian Recommended Nutrient Intake (RNI). The RNI suggested that the general macronutrient requirements for an adult were 50–65% of total energy intake (TEI) from carbohydrate, 10–20% of TEI from protein and the remaining 25–35% of TEI from fat [9]. The Malaysian Adult Nutrition Survey (MANS) has shown that total carbohydrate intake decreased from 59% of TEI in 2003 to 55% in 2014, while the total protein and fat intake increased from 14 to 16% and 27 to 29%, respectively, for the same years [10, 11].
In general, there is none equivocal guidelines regarding macronutrients intake among T2DM patients. Malaysian Ministry of Health (MOH) provides suggestion of macronutrients intake among T2DM patients as follows; 45–60% carbohydrate, 15–20% protein, and 25–35% fat of TEI [12]. This guideline was similar to Canadian Diabetes Association (CDA) that suggest distribution macronutrients intake byT2DM patients were 45–60% carbohydrate, 15–20% protein, and 20–35% fat of TEI [13]. However, both guidelines emphasise individualisation of the macronutrients’ distribution based on weight, glycaemic and other metabolic goals, cultural preferences and individual lifestyle [12, 13]. Instead of inconclusive evidence for the best macronutrient proportion for all patients with T2DM, Hamdy & Barakatun-Nisak concluded that lower carbohydrate consumption (< 40% from TEI), intake of low glycemic index food, and balancing macronutrients improve postprandial blood glucose levels [14]. Besides, dietary patterns such as the Mediterranean diet or Dietary Approaches to Stop Hypertension (DASH) diet, are beneficial in managing diabetes [14].
Although there was evidence showing dietary factors in the development and management of T2DM, studies regarding dietary pattern for diabetes prevention and management in Malaysia is still lacking. Studies have previously been conducted in different settings to assess the dietary intake of T2DM patients in Malaysia [15,16,17]. However, these studies did not address dietary intake among newly diagnosed T2DM patients. Therefore, this study aimed to investigate the pattern of macronutrient (carbohydrate, protein and fat) intake among Malaysian adults with newly diagnosed and already-diagnosed T2DM.
Methodology
Design of the prospective urban and rural epidemiological (PURE) study
The PURE study has been described in previous literature [18,19,20]. It is a large-scale, international study of the incidence, mortality and risk factors associated with non-communicable diseases, which includes individuals from urban and rural communities in 21 countries, including Malaysia. The PURE study is coordinated by the Population Health Research Institute (PHRI), Hamilton, Ontario, Canada. The Malaysian arm of the study is coordinated by two public universities, namely Universiti Kebangsaan Malaysia (UKM) and Universiti Teknologi MARA (UiTM). This study has enrolled 15,353 Malaysian individuals since 2007, and follow-up data collection is ongoing until 2030. Participants were recruited from selected urban and rural areas of Malaysia that represent the heterogeneity of the national population in terms of social and economic factors.
Participants were recruited based on purposive sampling. Sampling was executed by reaching out to the community leaders of the purposively selected study locations, which included all 14 states of Malaysia. Once agreement from the community leaders was obtained, a health screening program was implemented. Prior to recruitment, individuals from the community health screening program were asked about their interest in participating in the study. Interested individuals were followed up through home visits. Individuals aged between 35 and 70 years and living in the same household were also invited as study participants. Participants aged 35–70 were selected due to the prevalence of diabetes mellitus were high starting at the age of 35 years old compared to younger Malaysian population [4, 5, 21]. Meanwhile, elders aged above 70 years old were excluded due to various underlying health issues that could be confounding factor to this study. Only the household members intend to continue living in their current home for a further 4 years were selected to join this study to ensure the feasibility of long-term follow-up. Written informed consent was obtained after participants understood the provided study information and their rights as study participants.
To ensure standardised methods of data collection, research assistants were trained with comprehensive operation manuals, videos and workshops. Data were transferred electronically to the project office and coordinating centre at PHRI for quality control.
Measurements
Participants were defined as having T2DM if they reported having been diagnosed with T2DM or had a glucose level of ≥7 mmol/L (fasting blood glucose) or ≥ 11.1 mmol/L (non-fasting blood glucose) [12]. The measurement of blood glucose was recorded as fasting blood sugar when the participants fasted for at least 8 hours prior to the test. The non-fasting blood sugar test was carried out for participants who did not fast prior to blood collection. The GlucoSure Plus blood glucose monitor was used to measure participants’ blood glucose levels. Participants were defined as newly diagnosed if they had never been diagnosed with T2DM but had an elevated blood glucose level at the baseline study. Those who were already diagnosed were stratified into either the diagnosed for ≤5 years or diagnosed for > 5 years group. The grouping was based on the number of years from diagnosis to the time of baseline data collection.
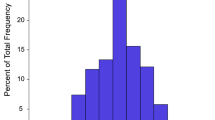
Participants’ habitual food intake was recorded using a validated food frequency questionnaire (FFQ) [22]. Participants reported the usual portion size of each food item in the FFQ and the average frequency of consumption. Then, macronutrients in terms of total energy, carbohydrate, protein and fat intake were calculated based on the Malaysian food composition and US Department of Agriculture food composition databases, with reference to nutrient databases containing the recipes of mixed dishes [23]. Participant dietary intake was stratified into three groups according to the RNI for Malaysians [9]. The recommended proportions of carbohydrate, protein and fat in the TEI were 50–65%, 10–20% and 25–30%, respectively [9].
Information on demographics, personal and family medical history, and active or passive smoking status was extracted from the validated PURE questionnaire and physical activity levels were assessed using the International Physical Activity Questionnaire (IPAQ) [19, 23, 24]. Demographic characteristics included age (rounded to the nearest year of birth), gender, race (Malay or non-Malay), marital status (single, married or divorced), education level (none, primary, secondary or tertiary) and employment status (yes or no). The residency area (urban or rural) was based on local government-gazetted areas. Rural areas were defined as areas occupied by less than 150 residents per square kilometre. Height and weight were measured using a portable stature meter and the TANITA (BC-558 Ironman®) segmental body composition analyser, respectively. Body mass index (BMI) was derived by dividing weight by height squared. BMI was categorised into underweight (< 18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25–29 kg/m2) and obese (≥ 30 kg/m2).
The participants were asked whether they had been diagnosed with hypertension as comorbidity. Family medical history of T2DM and hypertension was defined as the occurrence of these comorbidities in at least one family member (father, mother or siblings) as reported by the participant. Active smoking status was categorised into current smokers and former tobacco smokers who had quit within the previous year, while inactive smoker was those who had never smoked. Passive smokers included those who had been exposed to environmental tobacco smoke at least once a week for the previous year. Physical activity level was considered low if it was < 600 Metabolic Equivalent (MET) min/week and high if it was ≥600 MET min/week [25, 26].
Statistical analysis
The data were analysed using SPSS version 26. Chi-square test was used to assess differences in the T2DM groups stratified by gender according to the following variables: carbohydrate intake, protein intake, fat intake, age, BMI, race, marital status, education level, employment status, residency, participant comorbidities, family history of comorbidities, smoking status and physical activity level. The results were reported as frequencies and percentages, and a p-value of < 0.05 was considered significant.
Results
A total of 15,352 participants completed the personal medical history assessment of T2DM. Of these, 2254 participants were diagnosed with T2DM without missing data on years of being diagnosed, age, gender and obesity. Finally, a total of 1719 participants completed the FFQs.
The total number of participants diagnosed with T2DM in this study was 2254. Of these, 453 (20.1%) were newly diagnosed, 1156 (51.3%) were diagnosed for ≤5 years and 645 (28.6%) were diagnosed for > 5 years. Table 1 shows the general characteristics of this study population stratified by gender. Among male, there were significant differences among the three groups of T2DM patients according to the following variables: age, BMI, residency, participant comorbidity of hypertension, family history of T2DM and hypertension, and active smoker. Majority of male participants that has been diagnosed with T2DM ≤5 years were aged 51–60 years old (207, 52.9%), overweight (314, 56.1%), resided in urban area (272, 53.6%), have comorbidity of hypertension (302, 57.4%), have family history of T2DM (228, 58.6%) and hypertension (201, 58.1%), and being active smokers (262, 55.3%). Meanwhile, female shows significant differences among the three groups of T2DM patients according to the following variables: age, BMI, marital status, education level, residency, participant comorbidity of hypertension and family history of T2DM. Most of the female participants that has been diagnosed with T2DM ≤5 years were aged 51–60 years old (253, 50.9%), overweight (350, 53.5%), married (513, 49.8%), have primary education level (275, 50.6%), resided in rural area (356, 52.1%), have comorbidity of hypertension (410, 56.6%) and have family history of T2DM (281, 55.8%).
The Chi-square analysis showed that there were significant differences in carbohydrate and protein intake by male among the three groups of T2DM patients (Table 2). Most of the male patients consumed appropriate proportions of carbohydrate (458, 60.7%) and protein (618, 81.9%). However, female patients did not show any significant differences of the macronutrients intake among the three groups of T2DM patients.
Discussion
Basic characteristics of T2DM patients
A majority of the newly diagnosed T2DM patients were between 51 and 60 years old (72, 15.4%) among male patients and 41–50 years old (99, 30.6%) among female patients. The findings for male patients were comparable with those of the NHMS, which reported that the prevalence of newly diagnosed T2DM was highest among 50–59 years old Malaysian male (143, 47.4%) [5]. While for female, the NHMS has reported that the highest prevalence of newly diagnosed T2DM were also 50–59 years old (160, 52.6%) which is older compared to this study that show the highest prevalence among 41–50 years old [5].
In the present study, patients with overweight BMI were most common among those who were diagnosed for ≤5 years for male (314, 56.1%) and female (350, 53.5%). Similar trend were observed for obese patients with percentage of 56.3 and 53.3% among male and female patients respectively. A study done by Mafauzy et al. reported that 72% of T2DM patients were obese, which reflects the imbalance between energy intake and expenditure [27,28,29]. According to a Malaysian report, obese persons were recommended to reduce their initial weight by 5–10% over a period of 6 months [29]. To achieve this goal, medical nutrition therapy (MNT) was provided via individualised nutritional recommendations for T2DM patients with obesity [29]. Although overweight and obesity are well-known risk factors for type 2 diabetes, the disease also noticeable among newly diagnosed T2DM patients with normal BMI in this study (male: 77, 32.6%; female: 79, 30.7%). According to Gujral et al., diabetes development among patients with BMI < 25 kg/m2 might be due to impairments in insulin secretion, in utero undernutrition, and epigenetic alterations to the genome [30].
Our results showed that patients already diagnosed with T2DM for ≤5 years had a notably high prevalence of hypertension comorbidities (male: 302, 57.4%; female: 410, 56.6%), compared to newly diagnosed patients (male: 43, 8.2%; female: 59, 8.1%). Increased comorbidities would increase the risk of complications such as cardiovascular disease and impact the management of comorbidities, long-term survival and the health care system [6]. Other than that, family history of diabetes also shows similar trends. This is because comorbidities are heritable [31]. The results of the present study also showed that active smoking status among male participants was significantly related to T2DM. Smoking behaviours have been reported as risk factors contributing to T2DM [32].
Pattern of macronutrient intake among T2DM patients
The Chi-square analysis showed significant differences among the three groups of T2DM patients in terms of carbohydrate and protein intake by male patients. Compliance with the recommended carbohydrate intake (50–65% of TEI) among the newly diagnosed, ≤ 5 years and > 5 years groups was 83 (18.1%), 239 (52.2%) and 136 (29.7%), respectively. Similarly, carbohydrate consumption less than recommended intake (< 50% of TEI) among the newly diagnosed, ≤ 5 years and > 5 years groups was 49 (19.4%), 131 (51.8%) and 73 (28.9%), respectively. Meanwhile, T2DM patients who consumed carbohydrate at proportions > 65% of TEI was highest among the group newly diagnosed (20, 45.5%), compared to ≤5 years (16, 36.4%) and > 5 years groups (8, 18.2%).
Compliance with the recommended protein intake (10–20% of TEI) among the newly diagnosed, ≤ 5 years and > 5 years groups was 123 (19.9%), 320 (51.8%) and 175 (28.3%), respectively. Similar patterns were observed for a protein intake of > 20% of TEI among the newly diagnosed, ≤ 5 years and > 5 years groups (18.5, 49.2 and 32.3%, respectively). In addition, very few T2DM patients consumed protein in amounts less than the recommended proportions. Although the differences were not significant, the majority of the T2DM patients consumed amounts of fat higher than the recommended proportion (> 30% of TEI).
A previous study conducted at the outpatient clinic of the University of Malaya Medical Centre reported that the mean proportions of carbohydrate, protein and fat consumed by T2DM patients were 56.9, 14.7 and 28.4% of TEI, respectively [15]. Another study by Chin et al. found that the mean proportions of carbohydrate, protein and fat consumed by T2DM patients were 60.0, 16.0 and 24.0% of TEI, respectively [17]. Meanwhile, this study shows that the mean proportions of carbohydrate, protein and fat intake among T2DM patients were 51.9, 17.7 and 30.4% of TEI, respectively (results were not shown). The present study found that the mean carbohydrate intake among T2DM patients was lower than in previous studies (51.9% vs 56.9 and 60.0% of TEI) [15, 17]. Conversely, the mean intake of protein (17.7% of TEI) and fat (30.4% of TEI) among T2DM patients in this study was higher compared to the previous studies [15, 17]. The mean proportions of macronutrients consumed by participants in this study were found to be within the range recommended in the clinical practice guidelines for the nutritional management of T2DM patients [12].
Overall, the results of this study showed that T2DM patients mainly consumed carbohydrate and protein within the range of recommended nutrient intakes (RNI) for Malaysia but had a high fat intake (Table 2). This pattern contradicted a review by Hussein et al., which concluded that Malaysian diabetics were more prone to consuming high amounts of carbohydrate and fat [29]. The differences may be because the former study included only already known T2DM patients, while this study included both newly diagnosed and already-diagnosed T2DM categories. Several studies have highlighted that the general dietary intake recommendations based on macronutrients were not easily followed by both the general population and T2DM patients [7, 14, 33, 34]. Furthermore, previous reviews have stated that the effectiveness of the existing guidelines, which set goals based on macronutrient quantity, was still equivocal in efforts to reduce the risk of T2DM [33, 34]. Thus, the Malaysian Ministry of Health (MOH) has been implementing MNT to provide individualised nutritional recommendations based on personal preferences to manage the dietary intake of T2DM patients [31]. However, this approach only showed a 16.4% rate of compliance among Malaysian T2DM patients despite its effectiveness in glycaemic control [31]. Despite the efforts of the MOH to manage T2DM, lack of patient compliance with dietary counselling remains a huge challenge for both health practitioners and T2DM patients themselves.
The main limitation of this study was the cross-sectional study design that only included baseline data. The causal and temporal effects of macronutrient intake on T2DM patients were not considered. Future research should include controlled trials or prospective data analyses so that the causal effects of specific components of carbohydrate, protein and fat can be studied.
Conclusion
The T2DM patients in this study mainly consumed amounts of carbohydrate and protein within the range of RNI for Malaysia but had a high fat intake. Compliance with RNI recommendations for macronutrient proportions was satisfactory for carbohydrate and protein but not for fat. This trend shows that T2DM patients preferred fat over protein to replace lower proportions of carbohydrate. Further research regarding specific components of carbohydrate, protein and fat is necessary to understand the effects of macronutrients on T2DM in Malaysia. This study has also revealed a high proportion of newly diagnosed T2DM patients (20.1%), indicating a lack of awareness among the general population regarding this disease.
Availability of data and materials
The data that support the findings of this study are available from PHRI but restrictions apply to the availability of the data, which were used under license for the current study, and are not publicly available. Data are however available from the authors upon reasonable request and with permission from PHRI.
Change history
07 February 2023
A Correction to this paper has been published: https://doi.org/10.1186/s40795-023-00687-z
Abbreviations
- T2DM:
-
Type-2 Diabetes Mellitus
- TEI:
-
Total energy intake
- NHMS:
-
National Health and Morbidity Survey
- PURE:
-
Prospective Urban and Rural Epidemiological Study
- RESTU:
-
Risk Epidemiological Study
- FFQs:
-
Food frequency questionnaires
- TMC:
-
The Malaysian Cohort
- MOH:
-
Malaysian Ministry of Health
- MNT:
-
Medical nutrition therapy
References
International Diabetes Federation. IDF Diabetes Atlas. 9th ed. Brussels: Atlas de la Diabetes de la FID; 2019.
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843.
World Health Organization (WHO). Fact sheet diabetes. 2020. Available from: https://www.who.int/news-room/fact-sheets/detail/diabetes. Cited 2 Dec 2022.
IPH. National health and morbidity survey 2011 volume ii non-communicable diseases. 2011. Available from: https://iku.moh.gov.my/images/IKU/Document/REPORT/NHMS2011-VolumeII.pdf. Cited 19 May 2022.
IPH. National Health and Morbidity Survey (NHMS) 2019: NCDs - non-communicable diseases: risk factors and other health problems. Vol. 1, Institute for Public Health, National Institutes of Health (NIH), Ministry of Health Malaysia; 2020.
Rahim FF, Abdulrahman SA, Maideen SFK, Rashid A. Prevalence and factors associated with prediabetes and diabetes in fishing communities in Penang, Malaysia: a cross-sectional study. PLoS One. 2020;15(2):e0228570.
PD MA, Mellor D, Rilstone S, Taplin J. The role of carbohydrate in diabetes management. Vol. 33, practical diabetes; 2016. p. 237–42.
Nutrition Department M of HM. Piramid Makanan Malaysia 2020 – Mendidik Rakyat Mengambil Makanan Dengan Betul. Available from: https://www2.moh.gov.my/index.php/pages/view/2725. Cited 5 Dec 2022.
NCCFN. Recommended nutrient intakes for Malaysia (RNI). In a report of the technical working group on nutritional guidelines. 2017.
IPH. Malaysian adult nutrition survey 2003. Vol 5: dietary intake of adults aged 18 to 59 years. Nutrition section, family health development division, ministry of health Malaysia; 2008.
IPH. National health and morbidity survey 2014: Malaysian adult nutrition survey (MANS): Vol. III: food consumption statistics of Malaysia. Institute for public health, ministry of health, Malaysia; 2014.
Pheng CS, Bebakar WMW, Hussein Z, Aun AH, Mustapha FI, Mohamad M. Clinical practice guidelines Management of Type 2 diabetes mellitus (6th Edition). Vol. 6, Angewandte Chemie International Edition. 2020.
Sievenpiper JL, Chan CB, Dworatzek PD, Freeze C, Williams SL. Nutrition therapy. Can J Diabetes. 2018;42:S64–79.
Hamdy O, Barakatun-Nisak MY. Nutrition in diabetes. Endocrinol Metab Clin. 2016;45(4):799–817 Available from: http://www.endo.theclinics.com/article/S0889852916300688/fulltext. Cited 30 Nov 2022.
Ming MF, Rahman SA. Anthropometry and dietary intake of type 2 diabetes patients attending an outpatient clinic. Malays J Nutr. 2002;8(1):63–73.
Tan SL, Juliana S, Sakinah H. Dietary compliance and its association with glycemic control among poorly controlled type 2 diabetic outpatients in Hospital Universiti Sains Malaysia. Malays J Nutr. 2011;17(3):287–99.
Chin KH, Sathyasurya DR, Abu Saad H, Jan Mohamed HJB. Effect of ethnicity, dietary intake and physical activity on plasma adiponectin concentrations among Malaysian patients with type 2 diabetes mellitus. Int J Endocrinol Metab. 2013;11(3) Available from: https://brief.land/ijem/articles/17629.html.
Corsi DJ, Subramanian SV, Chow CK, McKee M, Chifamba J, Dagenais G, et al. Prospective urban rural epidemiology (PURE) study: baseline characteristics of the household sample and comparative analyses with national data in 17 countries. Am Heart J. 2013;166(4):636–646.e4.
Yusuf S, Islam S, Chow CK, Rangarajan S, Dagenais G, Diaz R, et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE study): a prospective epidemiological survey. Lancet. 2011;378(9798):1231–43.
Teo K, Chow CK, Vaz M, Rangarajan S, Yusuf S, Islam S, et al. The prospective urban rural epidemiology (PURE) study: examining the impact of societal influences on chronic noncommunicable diseases in low-, middle-, and high-income countries. Am Heart J. 2009;158(1):7.e1.
IPH. National Health & Morbidity Survey (NHMS) 2015. Fact Sheet; 2015;
Norimah AK, Safiah M, Jamal K, Siti H, Zuhaida H, Rohida S, et al. Food consumption patterns: findings from the Malaysian adult nutrition survey (MANS). Malays J Nutr. 2008;14(1):25–39 Available from: https://europepmc.org/article/med/22691762. Cited 2 Dec 2022.
Teo K, Lear S, Islam S, Mony P, Dehghan M, Li W, et al. Prevalence of a healthy lifestyle among individuals with cardiovascular disease in high-, middle- and low-income countries: the prospective urban rural epidemiology (PURE) study. JAMA. 2013;309(15):1613–21.
Dehghan M, Mente A, Zhang X, Swaminathan S, Li W, Mohan V, et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet. 2017;390(10107):2050–62.
Thanamee S, Pinyopornpanish K, Wattanapisit A, Suerungruang S, Thaikla K, Jiraporncharoen W, et al. A population-based survey on physical inactivity and leisure time physical activity among adults in Chiang Mai, Thailand, 2014. Arch Public Heal. 2017;75(1):1–9 Available from: https://archpublichealth.biomedcentral.com/articles/10.1186/s13690-017-0210-z. Cited 2 Dec 2022.
Alzahrani H, Alshehri F, Alsufiany M, Allam HH, Almeheyawi R, Eid MM, et al. Impact of the 2019 coronavirus disease pandemic on health-related quality of life and psychological status: the role of physical activity. Int J Environ Res Public Health. 2021;18(8):3992 Available from: https://www.mdpi.com/1660-4601/18/8/3992/htm. Cited 2 Dec 2022.
Mafauzy M, Hussein Z, Chan SP. The status of diabetes control in Malaysia: results of Diabcare 2008. Med J Malaysia. 2011;66(3):175–81.
Bauer F, Beulens JWJ, Van Der ADL, Wijmenga C, Grobbee DE, Spijkerman AMW, et al. Dietary patterns and the risk of type 2 diabetes in overweight and obese individuals. Eur J Nutr. 2013;52(3):1127–34.
Hussein Z, Taher SW, Gilcharan Singh HK, Swee CS, W. Diabetes Care in Malaysia: problems, new models, and solutions. Vol. 81, Annals of Global Health: Elsevier Inc; 2015. p. 851–62. https://doi.org/10.1016/j.aogh.2015.12.016.
Gujral UP, Weber MB, Staimez LR, KMV N. Diabetes among non-overweight individuals: an emerging public health challenge. Curr Diabetes Rep. 2018;18(8):1–10 Available from: https://link.springer.com/article/10.1007/s11892-018-1017-1. Cited 24 Nov 2022.
Abdullah N, Murad NAA, Attia J, Oldmeadow C, Kamaruddin MA, Jalal NA, et al. Differing contributions of classical risk factors to type 2 diabetes in multi-ethnic Malaysian populations. Int J Environ Res Public Health. 2018;15(12):2813.
Pan A, Wang Y, Talaei M, Hu FB, Wu T. Relation of active, passive, and quitting smoking with incident type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015;3(12):958–67.
Forouhi NG, Misra A, Mohan V, Taylor R, Yancy W. Dietary and nutritional approaches for prevention and management of type 2 diabetes. BMJ. 2018;361:k2234.
Feinman RD, Pogozelski WK, Astrup A, Bernstein RK, Fine EJ, Westman EC, et al. Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition. 2015;31(1):1–13.
Acknowledgements
The authors would like to thank all PURE staff members at PHRI for continuous staff training and data management support. The authors are also grateful for the dedication and commitment of RESTU research assistants from UKM and UiTM who were involved in the data collection process. The voluntary participation of all respondents is greatly appreciated.
Funding
RESTU was supported by the Ministry of Science, Technology and Innovation of Malaysia (grant numbers 100-IRDC/BIOTEK 16/6/21(13/2007) and 07–05-IFN-BPH 010), Ministry of Higher Education of Malaysia (grant number 600-RMI/LRGS/5/3(2/2011)), UiTM and UKM (PHUM-2012-01).
The PURE study is an investigator-initiated study that is funded by the Population Health Research Institute (grant number 101414), the Canadian Institutes of Health Research (CIHR), and the Heart and Stroke Foundation of Ontario, with support from CIHR’s Strategy for Patient Oriented Research (through the Ontario SPOR Support Unit), as well as the Ontario Ministry of Health and Long-Term Care. This study also received unrestricted grants from several pharmaceutical companies (with major contributions from AstraZeneca [Canada], Sanofi-Aventis [France and Canada], Boehringer Ingelheim [Germany and Canada], Servier, and GlaxoSmithKline) and additional contributions from Novartis and King Pharma.
Author information
Authors and Affiliations
Contributions
Conceptualization, Z.M.I, N.H.I, R. I, A.M.T and M.H.J; data collection, K.H.Y; data analysis, N.H.A.R, N.Z.A and K.H.Y; funding acquisition, N.H.I, R. I, and M.H.J; methodology, Z.M.I, N.H.I, R. I, A.M.T, M.H.J and K.H.Y; writing—original draft preparation, N.H.A.R and Z.M.I; writing—review and editing; N.H.A.R, Z.M.I, N.H.I, R. I, A.M.T, M.H.J, N.A.M.N.K, N.M.N.; supervision, N.H.I. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from Hamilton Health Sciences Research Ethics Board (PHRI), Hamilton Health Sciences and McMaster University, Hamilton, Ontario, Canada; Research and Ethics Committee (UKM Medical Centre); and Research and Ethics Committee (UiTM). The research is under the project code PHUM-2012-01. A written consent was obtained from each participant before conducting the survey. All methods were carried out in accordance to relevant guideline.
Consent for publication
Not applicable.
Competing interests
The authors declare that there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: The author group display order has been corrected.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Md Isa, Z., Ismail, N.H., Mohd Tamil, A. et al. Pattern of macronutrients intake among type-2 diabetes mellitus (T2DM) patients in Malaysia. BMC Nutr 9, 21 (2023). https://doi.org/10.1186/s40795-022-00648-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40795-022-00648-y