Abstract
Background
Severe malnutrition contributes to more than 60 % of deaths in children in developing countries. The minimum international standard set for management of severe acute malnutrition is a cure rate of at least 75 % and death rate of less than 10 %, yet the outcome of severely malnourished children treated in most hospitals in developing countries remain poor.
This study was conducted to determine the treatment outcomes among severely malnourished children admitted at St. Mary's hospital Lacor in Northern Uganda during a one year period in order to inform clinical decisions to maximize management of severely malnourished children.
Methods
This was a retrospective study involving 251 severely malnourished children treated at St. Mary's hospital Lacor within a one year period in 2014. Patients' medical records in the facility therapeutic feeding unit were retrospectively reviewed using a check list to collect basic demographic, clinical, and treatment outcome data of the sampled study patients. The UNICEF treatment outcome categories were used, and further grouped into three summary categories: "successful (cured)", "died" and "potentially unsatisfactory". Data were entered, cleaned and analyzed using statistical package SPSS version 13. For categorical data, proportions with 95 % confidence intervals, odds ratio and Chi-square test to compare different groups were used. Multivariate analysis using logistic regression was used to analyze the association between treatment outcome and potential associated factors. P values less than 0.05 was considered for statistical significance.
Results
The study consisted 251 patients and the treatment outcome was successful (cured) in 168 (66.9 %) and potentially unsatisfactory in 53 (21.2 %), while 30 (11.9 %) died. Hypothermia and HIV infection were the factors significantly associated with mortality among the severely malnourished children in the current study.
Conclusions
The treatment cure rate of severely malnourished children admitted at St. Mary's hospital Lacor of 66.9 % is below the accepted standard of least 75 % cure rate. A high proportion of patients died (11.9 %) or defaulted (8.0 %). Hypothermia and HIV infection were the factors significantly associated with mortality. We recommend that in order to address the high default rate, home based care through the outpatient therapeutic care should be strengthened.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Malnutrition is a contributing factor to nearly 60 % of the over 10 million deaths that occur annually among children under five years old in developing countries [1], where 2 % of children (about 13 million children) suffer from severe acute malnutrition [2]. Uganda has one of the highest child mortality rates in the world [3], 40 % of which is attributed to malnutrition as the underlying cause [4]. Most of these deaths are preventable and easily treatable.
The minimum international standard set for management of severe acute malnutrition is a cure rate of at least 75 % and death rate less than 10 % [5]. However, the case-fatality rates in hospitals treating severe acute malnutrition in developing countries have remained high (average 20–30 %) and has not changed much since the 1950s [6] in spite of the fact that clinical management protocols capable of reducing case-fatality rates to 1–5 % [7] have been in existence for over 30 years.
Despite the success of the current treatment protocols when implemented in specialized units, the adherence to the guidelines is variable, and their publication has not led to widespread decrease in case-fatality rates in most hospitals in the developing countries [8, 9]. The persistence of high case-fatality rates is therefore commonly attributed to inappropriate case management as a result of poor knowledge [6, 10]. Evidence from a review of treatment practices worldwide showed that many health services use discredited practices and that staff are unfamiliar with modern, effective guidelines for the management of severe malnutrition [10]. For instance, although both WHO and Uganda national guidelines for management of severe acute malnutrition recommend withholding transfusion unless a severely malnourished child’s hemoglobin level is <4 g/dl [11], and withholding intravenous infusion unless a child has signs of severe dehydration or is in shock, a recent study in Uganda showed that these guidelines were not followed [12].
This study examined the potential risk factors for mortality among severely malnourished children admitted in St. Mary’s hospital Lacor in Northern Uganda to generate information on a score of individual mortality risks which could be used to identify children at highest risk of death for whom more intensive care may be needed.
Methods
Study setting
The study was conducted at St. Mary’s hospital Lacor, a private not-for-profit tertiary health care facility located in Gulu district, northern Uganda and serving a number of rural districts in northern Uganda. The hospital serves a very poor population in a highly challenging social and economic environment. Severe acute malnutrition (SAM), defined as weight-for-height/length < −3 z-score and/or mid upper arm circumference (MUAC) <11.5 cm, or presence of bilateral pitting pedal oedema [13], is the 6th leading cause of admission among children under five years in the hospital. It accounts for up to 13 % of the total mortality among children under-five, with a case fatality rate of 15.4 % [14]. In the hospital, children diagnosed with severe acute malnutrition who have medical complications are hospitalized and treated according to the national guideline using a two phased approach (initial and rehabilitation phases) [11, 15]. The initial treatment phase is focused on stabilizing the child’s condition by careful re-feeding using F75 and identifying and treating life-threatening complications such as dehydration, hypoglycaemia, hypothermia, infections, and very severe anaemia among others [16]. The rehabilitation phase involved increasing the energy and nutrient content of the therapeutic feeds (transition from F75 to F100) to recover lost weight. Most older children (>2 years of age) were also started on nutritious solid food in this phase. At the same time, play therapy to stimulate the child’s emotional, cognitive and physical development were initiated in this phase both individually and in small groups.
Study design
This was a retrospective descriptive study involving 251 severely malnourished children treated in St. Mary’s hospital Lacor within a one year period in 2014. The minimum sample size was calculated using the formula for cross sectional studies by Leslie Kish [17] using a standard normal value corresponding to 95 % confidence interval (1.96); an absolute error between estimated and true value of 5 % (0.05), and an estimated treatment success (cure) rate for hospitalized severely malnourished children of 79.4 % as reported in Niger [18]. The study population comprised severely malnourished children aged 3–59 months hospitalized at the hospital between January to December 2014. The WHO classification of severe acute malnutrition was used: A severely malnourished child was one whose weight-for-height/length was less than −3 z-score (severe wasting) and/or mid upper arm circumference <11.5 cm, or who had bilateral pitting pedal oedema [13]. These were then broadly classified, for the purpose of management, as either oedematous or non-oedematous severe acute malnutrition. Patients with missing age (3 children) and those aged less than 3 months (11 children) and >60 months (37 children) were excluded from the study.
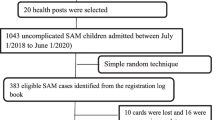
Sampling procedures
Patients’ medical records in the facility therapeutic feeding unit were retrospectively reviewed and a sampling frame for all the eligible patients listed into an excel program which was then used to randomly select the required sample size of 251 from among the eligible patient population. A check list was then used to collect information regarding basic demographic, clinical, and treatment outcome of the sampled study patients.
The treatment outcome was divided into five categories according to guideline-defined criteria. These included: cured (finished treatment and achieved a weight-for-height of ≥85 %); default (left the therapeutic feeding centre/nutrition rehabilitation ward before completing treatment); non-respondents (did not respond to treatment after 40 days on treatment); transfer out (patients whose treatment results are unknown due to transfer to another health facility or outpatient therapeutic program), and died (patients who died from any cause during the course of treatment). These were further grouped into three summary outcome categories: “successful” (cured), “died” and “potentially unsatisfactory” (non-response, default, and transfer out).
Statistical analysis
Data were coded, entered, cleaned, stored and analyzed using Statistical Package for Social Scientists (SPSS) version 13 (the dataset file is available on request to the corresponding author). Categorical variables were summarized as frequencies and proportions, while continuous variables as means, median and standard deviations (SD). In the bi-variate analysis, odds ratios, 95 % confidence interval (CI), and chi-square test were used to measure the strength of association between the factors considered and the dependent variable, while the student’s t-test was used for continuous variables. Multivariate analysis using logistic regression was used to determine the factors that were significantly associated with treatment outcome. Included in the model at multivariate analysis were factors that were significant at bivariate analysis and those with scientific plausibility even though they were not significant at bivariate analysis. P-value <0.05 was considered for statistical significance. Results were summarized in texts, tables and bar graphs.
Ethical considerations
Being a retrospective evaluation of standard treatment guidelines, individual patient consent was deemed impracticable. However, electronic databases created for this analysis were stripped of personal health identifiers and maintained securely and confidentially. This study was approved by the hospital’s research and ethics committee and consent to publish the results of the study was obtained from the hospital administration.
Results
During the one year study period 402 severely malnourished children were admitted to the hospital’s nutrition unit (Fig. 1). Of these, we enrolled and evaluated the treatment outcome of 251 severely malnourished children aged 3–59 months (mean age 24.2 [SD 16.0] and median of 21.0). Majority, 154 (61.4 %) of the children were between 3 and 24 months of age (Fig. 2), about two-third (61.0 %) of whom were males. Whereas up to 70 (27.9 %) of the malnourished children were HIV positive, only 24 (32.9 %) were on antiretroviral therapy (ART). Over half of the children (58.2 %) had oedematous severe acute malnutrition, and only 61.8 % of the children were immunized up to date. The other characteristics of the children are summarized in Table 1. Of the 251 severely malnourished hospitalized children, 168 (66.9 %) were successfully discharged as cured, 30 (11.9 %) died, and the rest had potentially unsatisfactory outcome comprising defaulting treatment (8.0 %), transfer out (9.6 %), and non-response (3.6 %).
At bivariate analysis, HIV negative children were significantly more likely to have a successful treatment outcome (76.9 %) compared to their HIV positive counterparts, who were more likely to die (18.6 % vs 9.6 %), P < 0.001, χ 2 = 19.981. The mean age of the children who died (18.87 months) was lower than that of the children who achieved a cure (25.13 months) and those with potentially unsatisfactory outcome (24.26 months), but this was not statistically significant (F = 1.966, P = 0.142). Children with non-oedematous severe acute malnutrition were more likely to die during the course of their management compared to those with oedematous acute malnutrition (16 [15.2 %] vs 14 [9.6 %]), but this was not statistically significant, P = 0.077, χ 2 = 5.115 (Table 2).
Very low body temperature (hypothermia) also had a significantly increased association with mortality (χ 2 = 7.788, P = 0.020). Similarly, children who received IV fluid infusion were significantly more likely to die compared to those who did not receive IV fluids (31.7 % vs 5.0 %), P < 0.001. In the same breath, significantly higher proportion of children that received blood transfusion died (27.6 %) compared to those who were not transfused (5.0 %), P < 0.001, χ 2 = 17.797 (Table 3). Majority of these deaths occurred in the first few days following IV infusion or blood transfusion (42.9 % within 24 h; 57.1 % within 48 h, and 71.4 % within 72 h after IV fluid infusion/blood transfusion).
At multivariate analysis, hypothermia and HIV infection were the only factors significantly associated with poor treatment outcome (mortality) among the severely malnourished children in the present study. Children with hypothermia were about five times more likely to die (OR 4.940, p = 0.017), while HIV infected children were three times more likely to die (OR 3.087, p = 0.010). The other factors that remained in the model even though they were not statistically significant were persistent diarrhoea and presence of visible severe wasting (Table 4).
Discussion
The adherence to current available treatment guidelines is expected to contribute to improved survival by achieving a high cure rate and reducing death rate among severely malnourished children. The present study assessed the treatment outcome in 251 severely malnourished children aged 3–59 months admitted at St. Mary’s hospital Lacor in Uganda within a one year period. Our main findings show that hypothermia and HIV infection seems to contribute significantly to poor outcome.
The high mortality rate as found in the present study accords with previous findings of high case fatality rate in hospitalized severely malnourished children in other African countries [6, 12, 19, 20]. However, our findings show a much higher mortality rate than that reported in studies in Ethiopia [5] and Niger [18], but much lower than that reported in another Ugandan and other studies [12, 21, 22]. This difference could be attributed to the fact that most children in our study setting are brought to the hospital at critical stages of their illnesses as a result both of late referrals as well as late health care seeking. In addition, differences in the level of health care could also be the other possible factors for the contrasting variation in outcomes.
Hypothermia was significantly associated with an increased risk of mortality among severely malnourished children in the present study. The negative consequence of hypothermia in relation to mortality among severely malnourished children has been documented in previous studies [12, 21], and may be explained by the fact that hypothermia in these children is an indicator of serious infections as well as hypoglycaemia – two common causes of death among severely malnourished children. Similarly, children who were HIV infected were significantly more likely to die during treatment compared to their HIV negative counterparts who were more likely to have a successful outcome. HIV infection as a risk factor for poor outcome among severely malnourished children as found in the present study agrees with findings previously reported by other authors [12, 23], but contrasts with results from another Ugandan study which found no adequate association between HIV positive status and death – attributed to the effect of HIV being overshadowed by the prominent effect of fluid overload [12]. However, the findings in the present study may not be surprising since both HIV and malnutrition tend to accelerate the progression of each other, a phenomenon that could have been compounded in this case by the increased risk of concurrent opportunistic infections given that majority of the HIV infected children in the current study were ART naïve.
Though IV infusions, either in the form of an I.V fluid infusion or blood transfusion were associated with an increased risk of mortality, these were not statistically significant at multivariate analysis. This finding, however, compares well with that from previous studies [10, 12, 21], and could be due to the fact that the use of IV fluids/blood transfusion serve as markers of severity of malnutrition. In addition, the fact that most of these deaths occurred soon after transfusion or infusion means that fluid overload could also be a plausible consequence of IV infusion/blood transfusion contributing to mortality, and corroborates the general recommendation to restrict transfusions or infusions of severely malnourished children [24, 25].
Whereas children with non-oedematous malnutrition (severe wasting) were more likely to die than those with oedematous malnutrition, this was not statistically significant. These findings, however, mirror that reported by Moges et al. (2009) in Ethiopia [22], but contrasts with that reported by Bachou et al. [12], and could be explained by the fact that malnourished children with severe wasting in the current study were more likely to be HIV positive (39.1 %) compared to those with oedematous malnutrition (25.4 %), thus increasing their vulnerability to death. There was no significant difference in treatment outcome with regard to the patients’ age, though younger infants aged 3–12 months were more likely to die compared to children above one year of age. This finding agrees with that by Teferi et al. in Ethiopia [5], and could reflect the fact that majority of the severely malnourished children in the current study were in the younger age group 3–24 months, coupled with the fact that complications and mortality due to infectious diseases are generally higher in young infants, exacerbated in this case by severe acute malnutrition.
Limitations of the study
Being a retrospective study, other factors that could have important bearing on treatment outcome, including biochemical laboratory parameters and health system factors (diagnostic capacity, knowledge and skills, referral system, and patient monitoring) among others could not be analyzed because they were either not done or not documented.
Conclusions
The treatment cure rate of severely malnourished children admitted at St. Mary’s hospital Lacor of 66.9 % is below the accepted standard of least 75 % cure rate. A high proportion of patients died (11.9 %) or defaulted (8.0 %), a situation which is of public health concern that needs consideration. Factors significantly associated with poor treatment outcome (mortality) in the study setting are hypothermia and HIV infection. We recommend that in order to address the high default rate, home based care through the outpatient therapeutic care should be strengthened through training of lower level healthcare workers in outpatient therapeutic care, as well as decentralizing services to lower health facilities to make home-based treatment of severely malnourished children without medical complications possible.
Abbreviations
- HIV:
-
human immunodeficiency virus
- ART:
-
antiretroviral therapy
- WHO:
-
World Health Organization
References
World Health Organization. Global forum for health reserach. Child health research: a foundation for improving child health. Geneva: WHO; 2002.
Steeve C, Kate S, Nicky D, et al. Key issues in the success of community based management of severe malnutrition. Food Nutr Bull. 2006;27(3):S49-82.
Uganda Demographic Health Survey. Ministry of Health. Kampala: Uganda Bureau of Statistics; 2011.
Uganda Demographic health survey. Ministry of Health. Kampala: Uganda Bureau of Statistics; 2000/2001.
Teferi E, Meskele L, Sahle S, et al. Treatment outcome of children with severe acute malnutrition admitted to therapeutic feeding centers in Southern Region of Ethiopia. Ethiop J Health Dev. 2010;24(3):234–8.
Schofield C, Ashworth A. Why have mortality rates for severe malnutrition remained high? Bull World Health Organ. 1996;74:223–29.
Ahmed T, Ali M, Ullah MM, et al. Mortality in severely malnourished children with diarrhoea and use of standardised management protocol. Lancet. 1999;353:1919–22.
Briend A. Management of severe malnutrition: efficacious or effective? J Pediatr Gastroenterol Nutr. 2001;32:521–22.
Waterlow JC. Intensive nursing care of kwashiorkor in Malawi. Acta Paediatr. 2000;89:138–40.
Schofield C, Ashworth A. Severe malnutrition in children: high case-fatality rates can be reduced. Africa Health. 1997;19(September issue):17–8.
WHO. Management of severe malnutrition: a manual for physicians and other senior health workers. Geneva: WHO; 1999.
Bachou H, Tumwine JK, Mwadime R, et al. Risk factors in hospital deaths in severely malnourished children in Kampala, Uganda. BMC Pediatrics. 2006;16(6):7.
WHO/Unicef. WHO growth standards and the identification of severe acute malnutrition in infants and children. A joint statement by the World Health Organization and the United Nations Children’s Fund, 2009. http://www.who.int/nutrition/publications/severemalnutrition/9789241598163/en/. (Accessed April 22, 2015).
St. Mary's hospital Lacor. Annual Report. Gulu Uganda: Hospital Management; 2010/2011.
Ashworth A, Jackson A, Khanum S, Schofield C. Ten steps to recovery. Child Health Dialogue. 1996;(3-4):10-12.
Picot J, Hartwell D, Harris P, et al. The effectiveness of interventions to treat severe acute malnutrition in young children: a systematic review. Health Technol Assess. 2012;16(19):1366–5278.
Leslie K. Survey Sampling. New York: John Wiley and Sonsa; 1965. p. 59–60.
Nael L, Andrea M, Ali D, et al. Mortality risk among children admitted in a large-scale nutritional program in Niger. PLoS One. 2009;4(1):e4313.
Gernaat HB, Dechering WH, Voorhoeve HW. Mortality in severe protein-energy malnutrition at Nchelenge, Zambia. J Trop Pediatr. 1998;44:211–7.
Erinoso HO, Akinbami FO, Akinyinka OD. Prognostic factors in severely malnourished hospitalised Nigerian children: Anthropometric and Biochemical factors. Trop Geogr Med. 1993;45:290–3.
Thandi P, David S, Mickey C, et al. Evaluating the clinical management of severely malnourished children-a study of two rural district hospitals. S Afr Med J. 2001;91:137–41.
Moges T, Haidar J. Management and outcome of severely malnourished children admitted to Zewditu Memorial Hospital, Ethiopia. East Afr J Public Health. 2009;6(2):162–7.
Fergusson P, Tomkins A. HIV prevalence and mortality among children undergoing treatment in sub-Saharan Africa: a systematic review and meta-analysis. Trans R Soc Trop Med Hyg. 2009;103:541–8.
World Health Organization. Management of severe malnutrition, in a manual for physicians and other senior health workers. Geneva: WHO; 1999.
Bauer AW, Kirby WMM, Sherries JC, Turck M. Antibiotic susceptibility testing by a standardised single disk method. Amer J Clin Pathol. 1966;45:493–6.
Acknowledgements
We acknowledge all the staff of the nutrition unit and the department of Paediatrics, St. Mary’s hospital Lacor for their support and inputs towards this study. A special tribute goes to the children whose information contributed to this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
RN was the initiator of the study and contributed to the study design, data collection, analysis and interpretation of results. VC contributed to getting relevant literature, design of the study and interpretation of results, BOS contributed to data collection, analysis and interpretation and GFA contributed to data collection. All authors contributed to drafting the manuscript, including reading and approving the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Nyeko, R., Calbi, V., Ssegujja, B.O. et al. Treatment outcome among children under-five years hospitalized with severe acute malnutrition in St. Mary’s hospital Lacor, Northern Uganda. BMC Nutr 2, 19 (2016). https://doi.org/10.1186/s40795-016-0058-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40795-016-0058-6