Abstract
Background
We aimed to investigate the aetiology and outcomes of illnesses in patients presenting to an emergency department after travelling to a malaria-endemic country, in order to raise awareness of both tropical and cosmopolitan diseases.
Methods
A retrospective chart review was performed for all patients who underwent blood smear testing for malaria at the Emergency Department of the University Hospitals Leuven from 2017 to 2020. Patient characteristics, results of laboratory and radiological examinations, diagnoses, disease course and outcome were collected and analysed.
Results
A total of 253 patients were included in the study. The majority of ill travellers returned from Sub-Saharan Africa (68.4%) and Southeast Asia (19.4%). Their diagnoses fell into three major syndrome categories: systemic febrile illness (30.8%), inflammatory syndrome of unknown origin (23.3%) and acute diarrhoea (18.2%). Malaria (15.8%) was the most common specific diagnosis in patients with systemic febrile illness, followed by influenza (5.1%), rickettsiosis (3.2%), dengue (1.6%), enteric fever (0.8%), chikungunya (0.8%) and leptospirosis (0.8%). The presence of hyperbilirubinemia and thrombocytopenia increased the probability of malaria, with a likelihood ratio of 4.01 and 6.03, respectively. Seven patients (2.8%) were treated in the intensive care unit, and none died.
Conclusion
Systemic febrile illness, inflammatory syndrome of unknown origin and acute diarrhoea were the three major syndromic categories in returning travellers presenting to our emergency department after a stay in a malaria-endemic country. Malaria was the most common specific diagnosis in patients with systemic febrile illness. None of the patients died.
Similar content being viewed by others
Background
Until early 2020, international travel was increasing steadily. In 2018, more than 1.4 billion international trips were undertaken [1]. Illness during and after travelling to developing countries occurs frequently and results in 8% of all travellers seeking medical care [2]. The most frequent diagnoses are febrile illnesses, gastrointestinal disorders, dermatological disorders and respiratory tract infections [3, 4]. Malaria has been reported as the leading tropical cause of fever and the primary cause of death [5].
The emergency physician faces several challenges: most importantly, life-threatening diseases, such as malaria, must be recognised and treated adequately in a timely manner. Yet there is a knowledge gap in the diagnosis and management of patients with tropical diseases, leading to increased mortality and morbidity [6]. Moreover, the differential diagnoses of patients returning from the tropics are very broad, since not only tropical infections, but also cosmopolitan infectious and non-infectious diseases must be considered.
The aim of this study was to investigate the aetiology and outcomes of illnesses in patients presenting to the emergency department (ED) after a stay in a malaria-endemic country, in order to raise awareness of both tropical and cosmopolitan diseases.
Methods
Study design and patient population
This retrospective observational study was conducted at the University Hospitals Leuven, Belgium, a tertiary care referral hospital. A computer-assisted search for this chart review was performed to identify all patients who underwent diagnostic blood smear testing for malaria during a three-year period, from 28/02/2017 to 07/03/2020. We chose blood smear testing as a surrogate for illness after a stay in a malaria-endemic, as this test was part of the diagnostic workup for ill travellers returning from these countries [7, 8]. The files of all the selected patients were checked manually. Patients were excluded when they were younger than 16 years, when there was no evidence of a trip to a malaria-endemic country within the past year, when they were asymptomatic and when blood smears had been taken outside the ED in which was the study was conducted. Patients with repeated blood smears within the same illness episode were included in the analysis only once. The study protocol was approved by the Ethics Research Committee of University Hospitals Leuven (S64951).
Medical records review
The following information was retrieved from the medical records: demographic data (age, gender, nationality and country of birth); travel history (travel destination, travel times and length of stay); reason for travel (tourism, work, visiting friends and relatives, volunteering, internship and recently arrived immigrant/expatriate); prophylaxis and adherence to malaria treatment (non-adherence was defined as not following the prescribed medication regimen); referral source (self-referred, general practitioner or another hospital or department within our hospital). Duration and onset of symptoms, intake of antimicrobial therapy before presentation, symptoms at presentation (fever (reported or measured in the ED), isolated fever (without focal signs or symptoms), respiratory symptoms, ear, nose and throat abnormalities, anorexia, diarrhoea, dysuria or urinary frequency, myalgia and arthralgia) were recorded. Relevant physical findings (e.g. lymphadenopathy, hepatosplenomegaly, skin lesions, abnormal lung auscultation,..) were collected from patient files. All available laboratory results (e.g. total blood cell count with differential, liver and kidney function test, blood smear, urinalysis, blood and stool cultures, serologic tests,…) were reviewed. Results of all performed radiological examinations were registered. Also records of follow-up care (during hospitalisation and until the final follow-up visit at the outpatient clinic) were reviewed for information on diagnosis, disease evolution and outcome.
Travel destinations were grouped in eight global regions corresponding to those defined for the GeoSentinel Surveillance Network: Sub-Saharan Africa, the Middle East and North Africa, Southeast Asia, South-Central Asia, Northeast Asia, Latin America and the Caribbean, North America and Australia, New Zealand and Oceania [9]. When different regions were visited, only the last visited destination was recorded.
Outcome measures
Diagnoses were made in accordance with internationally recognised case definitions [10]. All diagnoses were confirmed by an infectious disease specialist (LH) and assigned to one of three categories: ‘confirmed diagnosis’ (demonstration of a pathogenic microorganism in a relevant specimen, or confirmed seroconversion to an infectious agent), ‘highly probable diagnosis’ (combination of clinical findings and a single serologic test result) or ‘clinical diagnosis’ (e.g. fever undisputedly due to a specific syndrome, such as erysipelas). Febrile episodes not meeting any precise etiologic or clinical diagnosis were classified as an ‘inflammatory syndrome of unknown origin’. In cases of more than one diagnosis, the principal diagnosis was retained. Hospitalisation (including length of stay) and mortality were recorded.
Data analysis
Categorical variables are reported as totals and frequencies, and continuous variables are expressed as medians with interquartile ranges (IQR). We used 2 × 2 tables to calculate sensitivity, specificity, positive and negative likelihood ratios of signs, symptoms and laboratory findings. The confidence intervals (CI) for sensitivity, specificity and accuracy were 'exact' Clopper-Pearson confidence intervals.
The CI of the likelihood ratios were calculated using the log method [11]. Data were analysed using Medcalc Statistical Software version 20.011 (MedCalc Software, Ostend, Belgium).
Results
Patient characteristics
A total of 362 blood smears from the returning travellers in our ED were performed in the predefined period, and 109 blood smears were excluded from further analysis because of failure to meet the age criterion (n = 39), repeated blood smears from the same patient (n = 38), absence of travel to malaria-endemic country within the past year (n = 26), incomplete patient records (n = 4), blood smear taken outside the ED (n = 1) or being asymptomatic (n = 1).
The characteristics of the 253 patients who met the inclusion criteria are shown in Table 1. The median duration of travel was 18 days (IQR 10–28). Most patients presented at the clinic within the first month after their return (87%). The majority of ill travellers returned from Sub-Saharan Africa (68.4%) and Southeast Asia (19.4%), followed by Latin America and the Caribbean (6.3%), South-Central Asia (5.5%) and Northeast Asia (0.4%). Tourism (45.8%), work (22,1%) and visiting friends and relatives (20.9%) were the most frequent reasons for travel.
Clinical findings
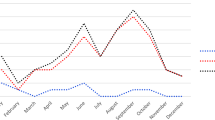
Frequencies of clinical signs and symptoms at presentation are shown in Fig. 1. Fever was present in 93.7% of the patients. Other frequently presenting symptoms included headache (58.9%), anorexia (53.8%), myalgia (43.1%), respiratory symptoms (32.8%) and diarrhoea (30.8%).
Laboratory and radiology results
Blood cultures were obtained from 231 out of 253 patients and were positive in 5.2% (n = 12). Detected bacteria included Salmonella Paratyphi A (n = 1), Salmonella Paratyphi B (n = 1), Salmonella group B (n = 1), Salmonella group D (n = 1), Escherichia coli (n = 3), Streptococcus agalactiae (n = 1) and Streptococcus pneumoniae (n = 1). The other three positive cultures were contaminated with coagulase negative staphylococci (n = 1), Acinetobacter Iwoffii (n = 1) and Corynebacterium spp. (n = 1). Urine cultures turned positive in 5.2% (10/192). Stool cultures were positive in 13 out of 38 tests: isolated pathogens consisted of Salmonella spp. (6/13), Shigella spp. (5/13) and Campylobacter spp. (2/13). All 54 patients that were tested for HIV were negative. Only 12 (6.9%) of the 175 chest X-rays performed were abnormal, showing an infiltrate (n = 10), pleural effusion (n = 1) or pulmonary nodule (n = 1). Abdominal ultrasound was performed in 138 patients (54.5%) and showed abnormalities in 23.9% of the examinations, including splenomegaly (n = 10), hepatosplenomegaly (n = 6), hepatomegaly (n = 3), lymphadenopathy (n = 3), colitis (n = 7), signs of enteritis (n = 3), acute appendicitis (n = 1) and sedimentation at the bladder base (n = 1). In 1 patient, 2 abnormalities were detected (hepatosplenomegaly and lymphadenopathy).
Diagnoses
Table 2 represents the syndromic groups and specified diagnoses by geographic region. Diagnoses were classified in 11 syndromic categories. Malaria and viral and bacterial infections were grouped under syndromic category of ‘systemic febrile illness’. The diagnoses of 72.3% of the 253 returning travellers fell into three major syndrome categories: systemic febrile illness (30.8%), acute diarrhoea (18.2%) and inflammatory syndrome of unknown origin (23.3%). The diagnosis of non-infectious origin was found in 9.9% of patients. Life-threatening diseases of non-infectious origin included pulmonary embolism (n = 2), subarachnoid haemorrhage (n = 1) and lymphoproliferative disorder (n = 1).
Malaria was detected in 40 patients (15.8%), all of them not taking malaria prophylaxis (n = 33) or non-adherent (n = 7) with the prophylaxis (early discontinuation). In our study 5/40 (12,5%) had a negative blood smear. In four of these patients the rapid antigen detection test (BinaxNOW™ Malaria test, Abbott, Chicago, USA) turned positive (presence of histidine-rich protein II detected). One patient needed a PCR test (performed in the reference lab at the Institute of Tropical Medicine (ITM)) for diagnosis. Plasmodium falciparum was found in 75% of the malaria cases. Four patients (4/30, 13%) with falciparum malaria met the WHO criteria for severe malaria (impaired consciousness n = 3, jaundice n = 1). The majority of patients diagnosed with malaria returned from Sub-Saharan Africa (95.0%) and their most frequently reported symptoms were fever (97.5%), headache (75.0%), myalgia (55.0%), anorexia (37.5%), arthralgia (25.0%), abdominal pain (20.0%) and diarrhoea (17.5%). In three patients with a malaria diagnosis (3/40, 7.5%), a co-infection was detected (1 rickettsiosis (positive IgG antibodies to Rickettsia conorii), 1 acute hepatitis E and 1 influenza B).
The presence of hyperbilirubinemia and thrombocytopenia increased the likelihood of malaria, with likelihood ratios of 4.01 (95% CI, 2.17—7.38) and 6.03 (95% CI: 4.08 – 8.90), respectively (Table 3). Splenomegaly was observed in five of the 19 patients with malaria who underwent abdominal ultrasound.
Outcomes
The majority of the 253 patients (55.7%) were treated in ambulatory care setting; 44.3% required admission to the hospital, and 2.8% were admitted to the intensive care unit. The median length of hospital stay was 4 days (IQR 3–6). None of the patients died.
Discussion
This study focusses on characteristics and outcomes of ill returning travellers presenting to the emergency department after a stay in a malaria-endemic country.
Malaria (n = 40) was the most common specific diagnosis in the patients with systemic febrile illness, followed by influenza (n = 13) and rickettsiosis (n = 8). Plasmodium falciparum, the cause of severe (potentially lethal) malaria, was identified in 75.0% of the patients with malaria. Compared to the study of Siikamaki et al., who performed a similar retrospective study in the ED looking at febrile adults after travel to malaria-endemic areas, our data show a higher percentage of Plasmodium falciparum malaria (11.9% vs 3.5%) [8]. As the great majority of falciparum malaria occurs in the region Sub-Saharan Africa, this difference can be explained by the higher proportion of patients returning from this region in our study (68.4% vs only 41.8%). Our data are in concordance with data from Bottieau et al. (ITM), who included mainly ambulatory patients with fever after a stay in the tropics: sub-Saharan Africa was the most frequent region of exposure (68%) and falciparum malaria was recorded in 22.1% of patients [5]. Our study confirms that most cases of falciparum malaria in returning travelers occur when the prescribed regimen for chemoprophylaxis is not followed. Nevertheless, as no prophylactic regimen gives complete protection, malaria should always be excluded in patients with a relevant travel history up until months after their return, and both medical professionals and patients should be educated about this [12]. Although thrombocytopenia increases the likelihood for malaria, it should be used with caution when trying to determine if fever is due to malaria or to another acquired infection. Thrombocytopenia was also found in patients with viral (hantavirus, dengue, chikungunya, influenza A and varicella zoster virus) as well as bacterial (rickettsiosis and enteric fever) infections. Thirteen % of the patients in our study had severe falciparum malaria, compared to 7.7% of cases in a London registry and 25% in the Finnish ED study [8, 13].
Early diagnosis and treatment of malaria is of utmost importance, since delay in diagnosis is associated with fatal outcome [14]. When analyzing the history of the patients eventually having malaria, 5 patients mentioned previous clinical visits before malaria was considered in the differential diagnosis. For example, one patient presented after five days of illness (shivering and general weakness) at the general practitioner. No blood smear was performed and paracetamol was prescribed. On day nine of symptoms he presented with fever and change of consciousness at our emergency department with diagnoses of severe falciparum malaria. Admission at the intensive care was necessary.
It is important to stress that malaria may be acquired together with other pathogens that are endemic in the visited areas (e.g. bacteria, viruses, other parasites), and that symptoms can overlap. Therefore, additional diagnoses should always be considered, even when a diagnosis of malaria has already been made: a tropical co-infection may be present, may require specific therapy and may cause significant morbidity when left untreated [15]. In our study blood cultures were not taken in all patients, whereas this would have been more prudent. A recent retrospective study from Sweden on travellers diagnosed with malaria showed a low frequency of bacterial coinfection (positive blood cultures in 0.3% of patients (Salmonella Enteritidis and E. coli)) [16].
Although recognition and early treatment of life-threatening tropical diseases by the emergency physician is crucial, in our study only 22.5% of the patients had a ‘tropical’ diagnosis (additional file 1). This is higher to the study of Siikamäki et al. in which 10% of the patients suffered from a tropical infection, but lower than in the ITM study (39%) [5, 8]; the higher ITM percentage reflecting the selection of patients sent to ITM. The most frequent cosmopolitan infections we found were acute diarrhoea (18.2%), respiratory tract infections (5.1%) and ear, nose and throat infections (4.7%). Previous studies show that physicians should always remain vigilant to the possibility of a serious cosmopolitan bacterial infection (that can resemble tropical viral infection on clinical grounds) when facing a returning traveller, so that antimicrobial therapy can be started in time, awaiting results from additional testing [17].
When we looked at the prevalence of tropical disease according to geographical region of exposure, rickettsiosis (typical eschar (7 of 8 patients) and/or positive IgG antibody titer to Rickettsia conorii (3 of 8 patients) was almost exclusively seen after return from Sub-Saharan Africa (7 of 8 patients), especially South-Africa (6/8), based on epidemiological data presumably 6 cases of African tick-bite fever. Enteric fever was only found in Asia in our study (Southeast Asia [n = 1] and South-Central Asia [n = 1]). Dengue was diagnosed in 4 patients (1.6%), all after travels to Asia or Latin America. These data are in accordance with the GeoSentinel surveillance data, and emphasize the importance of the region of return when determining the prior probability for a specific disease [9].
For a large proportion of the travellers presenting at the ED (23.3%), the aetiology of illness remained unclear, which is consistent with other reports in and outside the ED (no specific diagnosis in respectively 25.1 and 24.4% of patients) [5, 8].
Mortality in returning travellers has been reported to range from 0.2 to 0.5% in other studies [4, 5, 7], and was mainly caused by falciparum malaria (case fatality ranging from 0.2 to 3% [14]), and occasionally by dengue, melioidosis, leptospirosis, enteric fever and Strongyloides hyperinfection syndromes [5, 18,19,20,21]. In our study none of the patients died.
Study limitations
Since this is a single-centred study performed in a tertiary care hospital, there are restrictions on generalisability to other non-tertiary centres. We used the blood smear test as a surrogate for illness in the returning travellers after a stay in a malaria-endemic country. Theoretically we may have missed some patients that erroneously did not have a blood smear, but we believe this is unlikely since training on imported diseases is organised on a yearly basis in our centre and the threshold to request a blood smear is low. We were not able to collect reliable data on pre-travel vaccination status and so we did not include it on our study. Furthermore inpatients presenting with diarrhoea; parasitic testing was not routinely performed. The indication was evaluated case by case. In our study, there were no diagnoses of parasitic diarrhoea (e.g. giardiasis or amebiasis) and this could be an underestimation. Finally, this study discusses the patient population before the onset of the Covid-19 pandemic. For now, it remains unclear if the pandemic will have a permanent influence on international travel and cause a shift in the epidemiology of diseases in returning travellers.
Conclusion
Our study confirms the broad differential diagnoses of illnesses in returning travellers presenting at the ED after a stay in a malaria-endemic country, and thus the need for continued vigilance in the ED physician. Both tropical and non-tropical, infectious and non-infectious causes should be taken into account. Whether they are tropical or non-tropical, potentially life-threatening diseases should be excluded or confirmed first. A thorough clinical examination, directed laboratory tests and knowledge about the prevalence of tropical disease according to the geographical region of exposure can help narrow down the possibilities.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ED:
-
Emergency department
- CI:
-
Confidence intervals
- ITM:
-
Institute of Tropical Medicine Antwerp
References
International Tourism Highlights, 2019 Edition. World Tourism Organization (UNWTO); 2019. https://www.e-unwto.org/doi/pdf/10.18111/9789284421152.
Hill DR. Health problems in a large cohort of Americans traveling to developing countries. J Travel Med. 2000;7:259–66.
Freedman DO, Weld LH, Kozarsky PE, Fisk T, Robins R, von Sonnenburg F, et al. Spectrum of disease and relation to place of exposure among Ill returned travelers. N Engl J Med. 2006;354:119–30.
Wilson ME, Weld LH, Boggild A, Keystone JS, Kain KC, von Sonnenburg F, et al. Fever in returned travelers: results from the Geosentinel surveillance network. Clin Infect Dis. 2007;44:1560–8.
Bottieau E, Clerinx J, Schrooten W, Van den Enden E, Wouters R, Van Esbroeck M, et al. Etiology and outcome of fever after a stay in the tropics. Arch Intern Med. 2006;166:1642.
Meshkat N, Misra S, Hunchak C, Cleiman P, Khan Y, Ritchie LMP. Knowledge gaps in the diagnosis and management of patients with tropical diseases presenting to Canadian emergency departments: are the gaps being met? Can Assoc Emerg Physicians. 2014;16:458–66.
Thwaites GE, Day NPJ. Approach to fever in the returning traveler. Longo DL, editor. N Engl J Med. 2017;376:548–60.
Siikamäki HM, Kivelä PS, Sipilä PN, Kettunen A, Kainulainen MK, Ollgren JP, et al. Fever in travelers returning from malaria-endemic areas: Don’t look for malaria only. J Travel Med. 2011;18:239–44.
Leder K, Torresi J, Libman MD, Cramer JP, Castelli F, Schlagenhauf P, et al. GeoSentinel surveillance of illness in returned travelers, 2007–2011. Ann Intern Med. 2013;158:456–68.
Centers for disease controle and prevention. Surveillance case definitions for current and historical conditions. Available from: https://ndc.services.cdc.gov/. [Cited 20 Feb 2021].
Altman D. Statistics with confidence: Confidence intervals and statistical guidelines. 2nd edn. BMJ Books; 2000.
Boggild AK, Parise ME, Lewis LS, Kain KC. Atovaquone-proguanil: report from the CDC expert meeting on malaria chemoprophylaxis (II). Am J Trop Med Hyg. 2007;76:208.
Marks ME, Armstrong M, Suvari MM, Batson S, Whitty CJM, Chiodini PL, et al. Severe imported falciparum malaria among adults requiring intensive care: a retrospective study at the hospital for tropical diseases. London BMC Infect Dis. 2013;13:118.
Lüthi B, Schlagenhauf P. Risk factors associated with malaria deaths in travellers: a literature review. Travel Med Infect Dis. 2015;13:48–60.
Deen J. Coinfections and Malaria. In: Hommel, M., Kremsner, P. (eds) Encyclopedia of Malaria. New York: Springer; 2014. https://doi.org/10.1007/978-1-4614-8757-9_113-1.
Sandlund J, Naucler P, Dashti S, Shokri A, Eriksson S, Hjertqvist M, et al. Bacterial coinfections in travelers with malaria: rationale for antibiotic therapy. J Clin Microbiol. 2013;51:15–21.
Note S, Soentjens P, Van Laer M, Meert P, Vanbrabant P. Streptococcal toxic shock syndrome in a returning traveller. Acta Clin Belg. 2019;74:430–4.
Huits R, Schwartz E. Fatal outcomes of imported dengue fever in adult travelers from non-endemic areas are associated with primary infections. J Travel Med. 2021;28:taab020.
Jensenius M, Han PV, Schlagenhauf P, Schwartz E, Parola P, Castelli F, et al. Acute and potentially life-threatening tropical diseases in western travelers - a GeoSentinel multicenter study, 1996–2011. Am J Trop Med Hyg. 2013;88:397–404.
De Vries SG, Visser BJ, Stoney RJ, Wagenaar JFP, Bottieau E, Chen LH, et al. Leptospirosis among returned travelers: a geosentinel site survey and multicenter analysis-1997-2016. Am J Trop Med Hyg. 2018;99:127–35.
Patel TA, Armstrong M, Morris-Jones SD, Wright SG, Doherty T. Imported enteric fever: case series from the hospital for tropical diseases, London, United Kingdom. Am J Trop Med Hyg. 2010;82:1121–6.
Acknowledgements
Writing support, in the form of language editing, was performed by Oxford Science Editing.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
PV, LH, SD conceived and designed the study. PV, LH, SD, SO performed data collection and analysis. All authors interpreted the data. PV and SD drafted the manuscript and all authors contributed substantially to its revision. BD provided statistical advice on study design and analysed the data. PVB takes responsibility for the paper as a whole. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved and registered by the Ethics Research Committee of University Hospitals Leuven (number S64951). The need to obtain informed consent was waived by the competent Ethics Research Committee of University Hospitals Leuven.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Final diagnoses.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Desmet, S., Henckaerts, L., Ombelet, S. et al. Imported diseases in travellers presenting to the emergency department after a stay in a malaria-endemic country: a retrospective observational study. Trop Dis Travel Med Vaccines 9, 3 (2023). https://doi.org/10.1186/s40794-023-00190-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40794-023-00190-0