Abstract
Background
Gastric conduit necrosis (GCN) after esophagectomy is a serious complication that can prove fatal. Herein, we report a rare case of GCN with a severe course that improved with conservative treatment.
Case presentation
We present the case of a 78-year-old male patient who underwent an Ivor Lewis esophagectomy and developed a massive GCN. The patient was critically ill in the initial phase but recovered quickly; he also had a ruptured gallbladder and a bleeding jejunal ulcer. On the 22nd postoperative day, massive GCN was revealed on endoscopy. Considering the recovery course, careful observation with a decompressing nasal gastric tube was the treatment of choice. The GCN was managed successfully, having been completely replaced by fine mucosa within 9 months postoperatively. The patient completed his follow-up visit 5 years after surgery without any evident disease recurrence. Five and a half years after the surgery, the patient presented with progressive weakness and deterioration of renal function. Gastrointestinal endoscopy revealed a large ulcer at the anastomotic site. Three months later, computed tomography revealed a markedly thin esophageal wall, accompanied by adjacent lung consolidation. An esophagopulmonary fistula was diagnosed; surgery was not considered, owing to the patient’s age and markedly deteriorating performance status. He died 2013 days after the diagnosis.
Conclusions
Massive GCN after esophagectomy often requires emergency surgery to remove the necrotic conduit. However, this report suggests that a conservative approach can save lives and preserve the gastric conduit in these cases, thereby augmenting the quality of life.
Similar content being viewed by others
Background
Gastric conduit necrosis (GCN) after esophagectomy is a serious complication with fatal consequences if not detected and treated in time. Herein, we present the case of a 78-year-old male patient who underwent an Ivor Lewis esophagectomy and developed a massive GCN. In general, massive GCN after esophagectomy requires emergency surgery to remove the necrotic conduit. However, the case presented in this report suggests that a conservative approach may save lives as well as preserve the gastric conduit in such cases, thereby augmenting the quality of life.
Case presentation
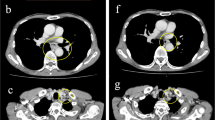
A 78-year-old male patient presented with dysphagia caused by advanced esophageal squamous cell carcinoma (ESCC) of the lower thoracic esophagus. The disease was diagnosed as cT3N0, according to the Japanese Classification of Esophageal Cancer (11th Edition) [1]. The patient had no relevant medical history except for hypertension and moderate chronic kidney disease (Table 1). An Ivor Lewis esophagectomy was performed as a curative surgery. The postoperative course was uneventful before the acute onset of right hypochondrial pain on the 4th postoperative day (POD 4). Computed tomography (CT) revealed a moderate amount of fluid collection around the gallbladder (Fig. 1a); however, no remarkable abnormalities were observed around the anastomotic site (Fig. 1b). As he developed a high-grade fever on POD 6, his respiratory condition deteriorated steeply (PaO2: 68.8 mmHg at FiO2: 0.5). His mean blood pressure fell to 75 mmHg, and re-evaluation using CT revealed an anastomotic breakdown (Fig. 2). He was intubated and moved to the intensive care unit, where his general condition quickly improved after decompression of the gastric conduit using a nasogastric tube. While the patient was stable without notable pyrexia, thoracocentesis of the left chest revealed bile-containing pleural fluid on POD 8. The leaked bile also drained from the abdominal wound, and percutaneous transhepatic gallbladder drainage was performed on POD 9. The bile leakage subsided soon afterward. This episode was retrospectively diagnosed as a gallbladder rupture based on the histopathological findings of the resected gallbladder, which were obtained through open surgery performed on POD 128. The patient experienced another episode of gastrointestinal bleeding on POD 16 due to a jejunal ulcer forming near the site of the percutaneous feeding jejunostomy placed during the initial surgery. Bleeding was managed by an emergency operation to resect the bleeding area of the jejunum, revealing no other pathological conditions in the abdominal viscera, including the gallbladder.
The anastomotic leakage was considerably well-managed, and a contrast swallow was performed 16 days after the relook laparotomy, which revealed no contrast leakage. Before oral intake was restarted, an upper gastrointestinal endoscopy was performed on POD 22, which revealed circular necrosis of the gastric conduit wall extending 3 cm in length (Fig. 3). Careful observation with decompression via the nasogastric tube was regarded as a safer strategy than surgery, considering the patient’s recovery course. The intermittent suction pressure on the nasogastric tube was set at 50 cmH2O, and suction was continued until POD 36. The patient’s condition did not deteriorate, and enteral nutrition was initiated with a nasal nutritional tube placed proximal to the jejunum. Repeated evaluation by endoscopy on POD 36 showed partial replacement of the necrotic tissue by an ulcer, and the subsequent endoscopic findings revealed gradual improvements over 3 months (Fig. 4). Elective cholecystectomy and percutaneous feeding jejunostomy were performed on POD 128. He had been fed with 1400 kcal of polymeric formula by a nasal jejunal tube so far and by the percutaneous tube afterward. His serum nutritional marker recovered: albumin 3.2 g/dL on POD 164. Oral intake was permitted on POD 98, and repeated sessions of endoscopic dilatation for anastomotic strictures were required. After rehabilitation by a speech therapist, the patient was discharged on POD 183. The esophageal cancer was diagnosed as pT3N1 (11th Edition of Japanese Classification) [1]. Although several endoscopic interventions for balloon dilation were required, the anastomotic site was fully covered with regenerative mucosa (Fig. 4). The patient’s oral intake gradually improved, and the jejunostomy tube was removed 26 months postoperatively. His routine activities of daily living were well-restored, and he showed no evidence of cancer recurrence during 5 years of follow-up with regular CT surveillance.
Upper gastrointestinal endoscopy. The necrotic black part of the conduit was gradually replaced by an ulcerous lesion and finally by regenerated mucosa on the 280th POD. a POD 36, b POD 90, c POD 280. White arrowhead: circular necrosis of the gastric conduit wall. Black arrowhead: normal esophageal mucosa. White arrow: gastric mucosa
Meanwhile, the patient’s renal function slowly deteriorated, and a nephrologist followed him up. Hemodialysis was scheduled, and an arteriovenous shunt was created for vascular access. As his weakness worsened, an endoscopy was performed to evaluate the reasons for the patient’s worsening anorexia. A severe esophageal ulcer was observed, and reflux esophagitis was diagnosed; however, anastomotic dehiscence was retrospectively diagnosed (Fig. 5). CT revealed no anastomotic failure. Two months later, his weakness progressed with worsening loss of appetite. The patient was re-evaluated using CT, which revealed a markedly thin esophageal wall accompanied by an adjacent lung consolidation (Fig. 6). He was hospitalized with a diagnosis of an esophagopulmonary fistula; radical surgery was not recommended, considering his age, end-stage kidney disease, and performance status at that time. He was about to undergo hemodialysis, but the conduit necrosis developed before the start of hemodialysis.
Upper gastrointestinal endoscopy 5 years and 4 months after surgery. A severe esophageal ulcer (white arrow) was observed with small metal staples (white arrowheads) indicating the anastomotic site. In the right-sided figure, the gap between the staples might have indicated a dehiscence of the anastomosis (yellow arrows)
Respiratory condition deteriorated within a week of hospitalization, and the patient died 2013 days after diagnosis. An autopsy was not performed in accordance with the family’s decisions.
Discussion
The incidence of GCN has been reported to be 2% in a series of 1000 patients [2] who underwent esophagectomies at the University of Pittsburgh Medical Center. Peripheral arterial disease, impaired cardiac function, poor nutritional status, and diabetes mellitus are presumed risk factors for this devastating condition [3]. However, no reliable preoperative risk assessment has yet been established [4]. Recently, indocyanine green staining has been recommended for the intraoperative evaluation of the blood flow of the conduit [5], and delayed reconstruction is recommended if ischemic conditions are suspected in the conduit [6]. In our case, moderate to severe chronic kidney disease (glomerular filtration rate 39.1 mL/min) and old age were listed as risk factors. GCN was classified by Veeramootoo et al., and for massive necrosis graded as grade 3 in this classification, emergency surgical removal of the gangrenous portion of the conduit has been strongly recommended [7]. Delay in re-intervention may lead to devastating events such as fistulation of the trachea, lung, or thoracic wall [8,9,10]. Only a small number of patients have been reported to have undergone conservative treatment [11]. In our case, the anastomotic leakage showed no prolonged course, and no drainage was required within 2 weeks after the esophagectomy. In addition, endoscopic evaluation of the gastric conduit was unintentionally postponed because of additional adverse events, namely, rupture of the gallbladder and a hemorrhagic jejunal ulcer.
The GCN was not evident until POD 22 when the patient was stable and showed no sustained elevation of serum inflammatory markers. Follow-up endoscopy showed improved findings at every subsequent re-evaluation, and there were no cues to reconsider our strategy during the entire 9-month clinical course before the cure of conduit necrosis. However, the patient developed a lethal esophagopulmonary fistula more than 5 years after surgery. Delayed perforation of gastric conduit ulcer has been reported so far and associated with radiation therapy, NSAID use, or Helicobacter pylori infection [12,13,14]. The case presented here was free from such known risk factors. The endoscopic image of his anastomotic site ulcer is speculated as an ischemic one. His old age and deteriorating renal function would be listed as strong risk factors accounting for this rare condition.
Treatment of the GCN ultimately failed; however, his initial complication was managed after an in-hospital course of approximately 6 months.
Accurate and timely diagnosis of conduit necrosis is possible with routine endoscopic evaluation during the early postoperative course, which is recommended by several experts [15,16,17]. However, whether the early discovery of massive necrosis promises improved outcomes remains unclear because the success rate of radical surgery is unknown. Interestingly, Page et al. detected gastric conduit ischemia in 16 of 84 patients with an uneventful postoperative course, while 12 necrotic cases had no anastomotic leakage [17]. Three patients were considered to be doing well despite the endoscopic diagnosis of both necrosis and leakage and underwent surgery immediately after diagnosis. One patient died after re-operation. Several other retrospective studies compared the surgical or non-surgical strategy for anastomotic leakage and concluded controversial interpretations [18,19,20]. These studies included cases with less than severe gastric conduits, and one report [18] illustrated two cases of massive conduit necrosis necessitating esophageal diversion; one died before reconstruction surgery, and the other required kidney transplantation.
Conclusions
Although our experience casts doubt on the classical belief that urgent surgery to remove the necrotic conduit is definitively safer than conservative treatment, we nonetheless believe that emergency radical surgery should be recommended for massive GCN if discovered early. Our clinical experience would be worth reporting, as the endoscopic images demonstrate the curative process of such massive conduit necrosis.
Availability of data and materials
Not applicable.
Abbreviations
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- BUN:
-
Blood–urea–nitrogen
- CT:
-
Computed tomography
- CEA:
-
Carcinoembryonic antigen
- CA19-9:
-
Carbohydrate antigen 19-9
- ESCC:
-
Esophageal squamous cell carcinoma
- GCN:
-
Gastric conduit necrosis
- POD:
-
Postoperative day
- T-bil:
-
Total bilirubin
References
Japan Esophageal Society. Japanese classification of esophageal cancer: part I. Esophagus. 2017;14:1–36. https://doi.org/10.1007/s10388-016-0551-7.
Luketich JD, Pennathur A, Awais O, Levy RM, Keeley S, Shende M, et al. Outcomes after minimally invasive esophagectomy: review of over 1000 patients. Ann Surg. 2012;256:95–103. https://doi.org/10.1097/SLA.0b013e3182590603.
Athanasiou A, Hennessy M, Spartalis E, Tan BHL, Griffiths EA. Conduit necrosis following esophagectomy: an up-to-date literature review. World J Gastrointest Surg. 2019;11:155–68. https://doi.org/10.4240/wjgs.v11.i3.155.
Jefferies BJ, Evans E, Bundred J, Hodson J, Whiting JL, Forde C, et al. Vascular calcification does not predict anastomotic leak or conduit necrosis following oesophagectomy. World J Gastrointest Surg. 2019;11:308–21. https://doi.org/10.4240/wjgs.v11.i7.308.
Slooter MD, Mansvelders MSE, Bloemen PR, Gisbertz SS, Bemelman WA, Tanis PJ, et al. Defining indocyanine green fluorescence to assess anastomotic perfusion during gastrointestinal surgery: systematic review. BJS Open. 2021;5:074. https://doi.org/10.1093/bjsopen/zraa074.
Oezcelik A, Banki F, DeMeester SR, Leers JM, Ayazi S, Abate E, et al. Delayed esophagogastrostomy: a safe strategy for management of patients with ischemic gastric conduit at time of esophagectomy. J Am Coll Surg. 2009;208:1030–4. https://doi.org/10.1016/j.jamcollsurg.2009.02.055.
Veeramootoo D, Parameswaran R, Krishnadas R, Froeschle P, Cooper M, Berrisford RG, et al. Classification and early recognition of gastric conduit failure after minimally invasive esophagectomy. Surg Endosc. 2009;23:2110–6. https://doi.org/10.1007/s00464-008-0233-1.
Balakrishnan A, Tapias L, Wright CD, Lanuti MX, Gaissert HA, Mathisen DJ, et al. Surgical management of post-esophagectomy tracheo-bronchial-esophageal fistula. Ann Thorac Surg. 2018;106:1640–6. https://doi.org/10.1016/j.athoracsur.2018.06.076.
Yasuda T, Sugimura K, Yamasaki M, Miyata H, Motoori M, Yano M, et al. Ten cases of gastro-tracheobronchial fistula: a serious complication after esophagectomy and reconstruction using posterior mediastinal gastric tube. Dis Esophagus. 2012;25:687–93. https://doi.org/10.1111/j.1442-2050.2011.01309.x.
Ishikawa S, Sato S, Oshima T, Hazama H, Nagai E, Taki Y, et al. A case of reconstructed gastric tube ulcer penetrated through to the chest wall. J Abd Emerg Med. 2015;35:885–9. https://doi.org/10.11231/jaem.35.885.
Fukuda C, Ide H, Sato Y, Nozaki M, Moriyama T, Narumiya K. A new device of jejunum interposition in a case of necrosed gastric tube after retrosternal gastric tube reconstruction. J Jpn Surg Assoc. 2006;67:2388–91. https://doi.org/10.3919/jjsa.67.2388.
Mizuta N, Suganuma T, Nakatani K, Okada S, Iida M, Tsujimoto S. Gastric tube ulcer perforation into the pericardial space after esophagectomy for esophageal cancer managed successfully by emergency surgery. Jpn J Gastroenterol Surg. 2019;52:137–45. https://doi.org/10.5833/jjgs.2017.0210.
Ubukata H, Nakachi T, Tabuchi T, Nagata H, Takemura A, Shimazaki J, et al. Gastric tube perforation after esophagectomy for esophageal cancer. Surg Today. 2011;41:612–9. https://doi.org/10.1007/s00595-010-4476-9.
Patil N, Kaushal A, Jain A, Saluja SS, Mishra PK. Gastric conduit perforation. World J Clin Cases. 2014;2:398–401. https://doi.org/10.12998/wjcc.v2.i8.398.
Nishikawa K, Fujita T, Yuda M, Yamamoto S, Tanaka Y, Matsumoto A, et al. Early postoperative endoscopy for targeted management of patients at risks of anastomotic complications after esophagectomy. Surgery. 2016;160:1294–301. https://doi.org/10.1016/j.surg.2016.06.022.
Lin TH, Huang PM. Early postoperative endoscopy for evaluation of the anastomosis after esophageal reconstruction. Thorac Cardiovasc Surg. 2018;66:376–83. https://doi.org/10.1055/s-0037-1602829.
Page RD, Asmat A, McShane J, Russell GN, Pennefather SH. Routine endoscopy to detect anastomotic leakage after esophagectomy. Ann Thorac Surg. 2013;95:292–8. https://doi.org/10.1016/j.athoracsur.2012.09.048.
Crestanello JA, Deschamps C, Cassivi SD, Nichols FC, Allen MS, Schleck C, et al. Selective management of intrathoracic anastomotic leak after esophagectomy. J Thorac Cardiovasc Surg. 2005;129:254–60. https://doi.org/10.1016/j.jtcvs.2004.10.024.
Guo J, Chu X, Liu Y, Zhou N, Ma Y, Liang C. Choice of therapeutic strategies in intrathoracic anastomotic leak following esophagectomy. World J Surg Oncol. 2014;12:402. https://doi.org/10.1186/1477-7819-12-402.
Page RD, Shackcloth MJ, Russell GN, Pennefather SH. Surgical treatment of anastomotic leaks after oesophagectomy. Eur J Cardiothorac Surg. 2005;27:337–43. https://doi.org/10.1016/j.ejcts.2004.10.053.
Acknowledgements
The authors would like to thank Editage (www.editage.jp) for the English language editing.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Hiroshi Takeuchi wrote the first draft of the manuscript, and all the authors commented on previous versions of the manuscript. All the authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Informed consent was obtained from the patient for the publication of this case report.
Competing interests
All authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Takeuchi, H., Yoshimura, S., Daimon, M. et al. Late-onset lethal complication of non-surgically managed massive gastric conduit necrosis after esophagectomy: a case report. surg case rep 10, 148 (2024). https://doi.org/10.1186/s40792-024-01955-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-024-01955-1