Abstract
Background
Liposarcomas represent ~9.8–16% of soft tissue sarcomas, with the extremities and retroperitoneum being the primary sites of occurrence. While liposarcoma in the inguinal region is uncommon, few reported cases originate from the retroperitoneum and protrude into the scrotum through the inguinal canal. Here, we present a case of a retroperitoneal liposarcoma with prolapse from the left inguinal canal into the scrotum following hernia repair with a mesh plug.
Case presentation
A 55-year-old male patient underwent a CT scan for a suspected recurrent inguinal hernia, which revealed a sizeable adipose-dense tumor by the left kidney extruded through the left inguinal canal surrounding the scrotum. The patient had undergone mesh plug repair for a left inguinal hernia at another hospital one year ago and noticed ipsilateral inguinal swelling after the hernia repair. The patient was referred to our hospital. The tumor resection was completed with combined resection of potentially involved organs: left side colon, left kidney, and left adrenal gland. Also, complete excision of the tumor was accomplished through surgical resection of the posterior wall of the inguinal canal, the mesh plug, and the tumor extending into the scrotum. Given the nearly complete absence of the inguinal canal's posterior wall and the anterior wall’s torn state, sutures were employed to close the external obturator tenosynovitis. Additionally, the inguinal ligament was closed using a tension-free incision technique. Only a mesh was subsequently placed. The resected tumor measured 47 × 30 × 15 cm and 7.5 kg in weight. After surgical resection, a retroperitoneal liposarcoma diagnosis was established. After 2 years and 6 months following the surgical resection, no recurrence has been observed for either liposarcoma or inguinal hernia.
Conclusion
The previous inguinal hernia in this case must be a prolapse of retroperitoneal liposarcoma. Thus, it is recommended to conduct a preoperative examination, which should include a CT scan, since the presence of a fatty mass within the hernia may indicate the presence of a retroperitoneal liposarcoma. Even if a preoperative diagnosis cannot be made, a long-term prognosis can be expected if the retroperitoneal liposarcoma can be completely resected at reoperation.
Similar content being viewed by others
Background
Spermatic cord lipomas are often identified intraoperatively during inguinal hernia repair procedures. However, liposarcomas originating from the spermatic cord are relatively uncommon. Liposarcomas constitute ~9.8–16% of soft tissue sarcomas [1, 2] and are frequently found in the extremities and retroperitoneum [3]. Instances of retroperitoneal liposarcomas extending from the inguinal canal are exceedingly uncommon. This report details a case involving an exceptionally enormous retroperitoneal liposarcoma that had descended from the left inguinal canal into the scrotum. Notably, no recurrence was observed following surgical intervention.
Case presentation
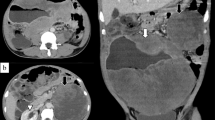
A 55-year-old male patient presented to our hospital with a significant bulge in the left inguinal region; he had undergone mesh plug repair of a left inguinal hernia at another hospital one year ago. Contrast-enhanced computed tomography (CT) revealed an enormous fat-dense tumor originating from the caudal side of the left kidney and extending through the left inguinal canal, eventually reaching the scrotum (Fig. 1a, b). The implanted mesh plug was bulging due to the presence of the tumor (Fig. 1c). The diagnosis was suspected of an enormous retroperitoneal liposarcoma that had prolapsed through the inguinal canal and extended into the scrotum. Surgery was executed to resect the retroperitoneal liposarcoma, accompanied by resection of the left-sided colon and left kidney (Fig. 2a). Concurrently, repair of the left inguinal hernia was undertaken. The tumor showed significant involvement of the left colon and left kidney, necessitating simultaneous resection of both organs. Complete tumor excision was accomplished by removing the mesh plug, which had become integrated with the tumor, extending from the posterior wall of the inguinal canal to the scrotum (Fig. 2b, c). The posterior wall of the inguinal canal displayed significant structural compromise, while the anterior wall showed evidence of tearing. Meticulous suturing of the external oblique aponeurosis to the inguinal ligament was performed, along with a reflexing incision to optimize closure. Only mesh was employed for the repair. The total operative duration was 7 h and 47 min, accompanied by a blood loss of 1489 ml. The resected tumor measured 47 × 30 × 15 cm and 7.5 kg in weight (Fig. 3). Pathological examination confirmed the tumor's identity as a well-differentiated liposarcoma (Fig. 4).
a. Contrast-enhanced CT imaging exhibited a substantial adipose-dense tumor originating from the caudal aspect of the left kidney. b. The tumor has been extending through the left inguinal canal, and reaching the scrotum (indicated by arrows). c. Notably, the mesh plug that had been implanted one year earlier was visibly protruding due to the presence of the tumor (indicated by arrowheads)
a1,2. The tumor was visibly exerting pressure on the left colon and left kidney. b1,2. Given the extensive involvement, a combined resection of the left colon and left kidney was undertaken. c1,2. The tumor was entirely excised through the resection of the posterior wall of the inguinal canal, the mesh plug, and the tumor's extension into the scrotum
The patient was subsequently discharged on postoperative day 33. Impressively, no recurrence has been observed over 2 years and 6 months post-surgery for either liposarcoma or inguinal hernia.
Discussion
We reviewed reported cases of retroperitoneal liposarcoma escaping the inguinal canal, including one autopsy case, and made two findings. The first is the condition under which retroperitoneal liposarcomas can escape from the inguinal canal. The second is how to deal with a retroperitoneal liposarcoma that has prolapsed from the inguinal canal and has been operated on as an inguinal hernia.
Retroperitoneal liposarcoma prolapsing through the inguinal canal remains an infrequent phenomenon. A PubMed search utilizing the keywords "retroperitoneal liposarcoma" and "inguinal" yielded 14 case reports. Inclusive of our case, Table 1 compiles 15 such instances [4,5,6,7,8,9,10,11,12,13,14,15,16]. Notably, all identified cases involved male patients aged between 40 and 86 years, with a mean age of 58.9. The dimensions of the tumors exhibited significant variability, spanning from 17 to 70 cm, with an average of 36.2 cm. Laterality presented no notable asymmetry, as eight cases occurred on the right side and seven on the left. Postoperative histopathological evaluations revealed that well-differentiated liposarcomas characterized 12 cases, while the remaining three exhibited pleomorphic features. Retroperitoneal liposarcomas are recognized for their elevated malignant potential, with Enterline et al. reporting distant metastases in 31% of liposarcoma patients [17]. In contrast, well-differentiated liposarcomas inherently possess lower malignant potential [18]. The emergence of retroperitoneal liposarcomas protruding through the inguinal canal appears contingent on two conditions: the presence of an indirect inguinal hernia and a low-grade malignant tumor capable of asymptomatic growth until it extends from the inguinal canal.
Table 2 offers a comprehensive overview of the initial diagnoses, treatments, and outcomes from the 15 documented cases. Among these cases, seven were diagnosed as inguinal hernias, subsequently undergoing inguinal hernia repair procedures. Significantly, two laparoscopic inguinal hernia repair cases led to intraoperative identification of retroperitoneal liposarcoma, prompting immediate cessation of hernia repair and transition to radical surgery. In five instances, an anterior open technique was employed for inguinal hernia repair; however, postoperative diagnoses of retroperitoneal liposarcoma necessitated re-operation. The authors highlight challenges in the intraoperative diagnosis of retroperitoneal liposarcoma during inguinal hernia repair using anterior open techniques. Postoperative recurrence has been documented in two cases involving re-operations following initial hernia repair. Leão et al. chronicled described a patient who, after refusing routine follow-up, exhibited recurrence nine years postoperatively. The patient subsequently underwent tumor resection, but unfortunately passed away postoperatively [9]. Similarly, Tardur et al. reported recurrence five months postoperatively, followed by tumor resection and a subsequent 20-month period without recurrence [11]. Curative surgical resection remains the optimal approach for liposarcoma treatment. In the present case, the inguinal hernia stemmed from retroperitoneal liposarcoma. Even within instances of hernia repair, long-term survival, and radical intervention are attainable when accurate postoperative diagnosis guides a subsequent radical tumor resection through re-operation. Cheng et al. presented a case wherein tumor resection followed neoadjuvant radiotherapy, yielding positive margins. Subsequent adjuvant chemotherapy resulted in no recurrence at the 26-month postoperative mark [16].
When excising large retroperitoneal liposarcomas prolapsing through the inguinal canal, the inguinal repair is often necessary. However, a question arises regarding the appropriateness of using artificial materials such as mesh during surgery for malignant tumors. Among the 15 cases listed in Table 2, inguinal repair was performed in 8 cases, with mesh being used for repair in only 2 cases, including our case. Although International guidelines for groin hernia management [19] do not specifically address simultaneous surgery for malignant tumors and inguinal hernia repair using mesh, the safety of simultaneous surgery for malignant tumors, such as prostate cancer, and inguinal hernia repair with mesh has been reported in multiple studies [20,21,22]. In the two cases that experienced recurrence in our study, inguinal repair was performed, but mesh was not used, and tumor residue was considered the cause of recurrence. Based on these findings, we believe that the use of mesh for repair is acceptable when achieving R0 resection. Additionally, recent reports suggest that repair with mesh may also be acceptable during inguinal hernia repair following bowel resection, provided there is no contamination of the inguinal region. However, if the inguinal region is contaminated, we recommend choosing either repair using tissue suturing or staged repair using mesh.
While a preoperative confirmation of the diagnosis is ideal, specific circumstances, such as hernia incarceration, might prompt the need for inguinal hernia repair. In laparoscopic surgery, encountering adipose tissue protrusion instead of an inguinal hernia necessitates an immediate decision to halt the procedure and initiate a comprehensive systemic assessment. Conversely, the anterior open technique poses challenges for intraoperative diagnosis. Consequently, surgically excised adipose tissue should be treated as a spermatic cord lipoma, prompting the need for pathological examination.
Conclusions
While spermatic cord lipomas are frequently encountered intraoperatively during inguinal hernia repairs, it is imperative to acknowledge the potential for retroperitoneal liposarcomas to prolapse through the inguinal canal. The challenge of intraoperative diagnosis becomes particularly pronounced when utilizing the anterior open technique, which lacks the advantage of preoperative diagnosis. It is important that intraoperative fat tissue is sent to pathology. If a retroperitoneal liposarcoma is diagnosed postoperatively and a complete resection can be achieved at reoperation, a long-term prognosis can be expected. Furthermore, it is worth noting that repair of the inguinal region may involve the use of mesh, a practice that should be considered permissible in appropriate cases.
In this case, the previous inguinal hernia likely originated from the prolapse of a retroperitoneal liposarcoma. Therefore, recommending a preoperative evaluation, including a CT scan, is prudent. This approach gains significance, as the presence of a fatty mass within the hernia serves as an indicator that warrants consideration of a possible retroperitoneal lipoma or tumor.
Availability of data and materials
The data supporting the findings of this study are available within the article.
References
Antinori A, Antonacci V, Magistrelli P. Giant retroperitoneal liposarcoma. Am J Surg. 2002;184:56–7.
Enjoji M, Hashimoto H. Diagnosis of soft tissue sarcomas. Pathol Res Pract. 1984;178:215–26.
Treadwell T, Treadwell MA, Owen M, McConnell TH, Ashworth CT. Giant liposarcoma of the spermatic cord. South Med J. 1981;74:753–5.
Noguchi H, Naomoto Y, Haisa M, Yamatsuji T, Shigemitsu K, Uetsuka H, et al. Retroperitoneal liposarcoma presenting a indirect inguinal hernia. Acta Med Okayama. 2001;55(1):51–4.
Mizuno Y, Sumi Y, Nachi S, Ito Y, Marui T, Saji S, et al. A case of a large retroperitoneal liposarcoma presenting as an incarcerated inguinal hernia. Hernia. 2006;10:439–42.
Baldassarre E, Santacroce C, Barone M, Torino G, Siani A, Valenti G. Retroperitoneal well-differentiated liposarcoma presenting as an incarcerated inguinal hernia. G Chir. 2007;28:315–7.
Ghimire P, Wu GY, Zhu L. Rare synchronous primary large B-cell gastric lymphoma and huge retroperitoneal liposarcoma with inguinal hernia in chronic hepatitis B patient. Curr Oncol. 2011;18:e103–8.
Bhandarwar AH, Bakhshi GD, Borisa AD, Shenoy SS, Kori CG, Vora S. Giant recurrent retroperitoneal liposarcoma presenting as a recurrent inguinal hernia. Clin Pract. 2011;1: e130.
Leão P, Vilac S, Oliveira M, Falcão J. Giant recurrent retroperitoneal liposarcoma initially presenting as inguinal hernia: review of literature. Int J Surg Case Rep. 2012;3:103–6.
McKinley SK, Abreu N, Patalas E, Chang A. Large retroperitoneal liposarcoma diagnosed upon radiological evaluation of mild right-sided inguinal hernia. Case Rep Radiol. 2013;2013: 187957.
Tardu A, Yagci MA, Karagul S, Ertugrul I, Kayaalp C. Retroperitoneal mass presenting as recurrent inguinal hernia: a case report. Int J Surg Case Rep. 2016;20:46–8.
Fiaschetti V, Castellani F, Croce G, Mondillo M, Amico A, De Majo A, et al. Incidentally discovered well-differentiated retroperitoneal liposarcoma with inguinal canal herniation: report of 2 cases. Radiol Case Rep. 2017;12:308–12.
Lechner M, Borhanian K, Mitterwallner S, Bittner R, Klieser E, Köhler G, et al. Retroperitoneal liposarcoma: a concern in inguinal hernia repair. JSLS. 2019;23: e2018.00064. https://doi.org/10.4293/JSLS.2018.00064.
Matsumoto T, Mima K, Ono A, Miyanari N, Morito A, Yumoto S, et al. Usefulness of laparoscopy in the management of incidentally discovered retroperitoneal liposarcoma mimicking inguinal hernia: a case report and literature review. Int J Surg Case Rep. 2020;72:79–84.
Lieto E, Cardella F, Erario S, Del Sorbo G, Reginelli A, Galizia G, et al. Giant retroperitoneal liposarcoma treated with radical conservative surgery: a case report and review of literature. World J Clin Cases. 2022;10(19):6636–46.
Cheng SH, Huang YS, Lee HH, Yen HH, Jhong YP, Chao TY. Case report and literature review: conversion surgery for initially unresectable huge retroperitoneal liposarcoma after preoperative radiotherapy. Front Oncol. 2023;12:1096411.
Enterline HT, Culberson JD, Rochlin DB, Brady LW. Liposarcoma. A clinical and pathological study of 53 cases. Cancer. 1960;13:932–50.
Longbotham JH, Joyce RP. Retroperitoneal liposarcoma presenting as spermatic cord tumor. Urology. 1987;30(3):276–80.
Hernia Surge Group. International guidelines for groin hernia management. Hernia. 2018;22:1–165.
Chiacchio G, Beltrami M, Cicconofri A, Nedbal C, Pitoni L, Fuligni D, et al. Simultaneous inguinal hernia repair with monofilament polypropylene mesh during robot-assisted radical prostatectomy: results from a single institute series. Medicina (Kaunas). 2023;59(5):820.
Carr WR, O’Dair G. A laparoscopic high anterior resection for sigmoid cancer with extraction through incarcerated left inguinal hernia repaired with Permacol mesh. BMJ Case Rep. 2012;2012:bcr0220125788.
David SF, Dominic S, Esequiel RJ, Adam K, Thomas EA. Transperitoneal robotic-assisted laparoscopic radical prostatectomy and inguinal herniorrhaphy. J Robotic Surg. 2008;1:269–72.
Acknowledgements
The authors thank all colleagues in the Department of Gastroenterological Surgery, Aichi Medical University, Japan, for their helpful contribution to the treatment.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
SU drafted the manuscript. TS, YF, SK, KK, and TS supervised the writing of the manuscript. SU provided management of the patient. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ueda, S., Saito, T., Fukami, Y. et al. A case of enormous retroperitoneal liposarcoma with prolapse from the left inguinal canal following hernia repair. surg case rep 10, 101 (2024). https://doi.org/10.1186/s40792-024-01891-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-024-01891-0